Abstract
Symptomatic intraspinal lumbar facet joint synovial cysts can be managed both conservatively and surgically. Diagnosis of the lumbar facet joint cyst is made through cross-sectional imaging of the spine, either by computerized tomography (CT) scan, myelography, or most commonly magnetic resonance imaging. Conservative treatment by facet joint injection can be performed under fluoroscopic or CT guidance, although only CT guidance provides direct visualization of the cyst confirming accurate needle placement. This case report illustrates the use of percutaneous CT-guided facet joint cyst treatment as a temporizing measure or alternative to surgical treatment in the proper clinical scenario.
Keywords: CT-guided injections, lumbar facet joint cysts
Introduction
Intraspinal ganglion cysts were first reported in the late 1800s with the first surgery for nerve root decompression for juxta facet cysts performed in 1950 [1]. The distinguishing factor between spinal synovial cysts and ganglion cysts is the presence or absence of the synovial lining found within synovial cysts. Synovial cysts are thought to be relatively uncommon causes of lumbar back pain with symptoms including radiculopathy, neurogenic claudication, neurologic deficit, and less commonly, cauda equina syndrome. The pathognomonic imaging finding for a facet joint cyst is direct communication of the cyst with the facet joint. Lumbar facet joint synovial cysts are most commonly seen in the setting of facet joint osteoarthrosis and, to a lesser extent, spondylolisthesis. Although anterior, intraspinal facet joint cysts are most likely to require surgical treatment due to radiculopathy or neurologic deficit, posterior or extra-canalicular synovial cysts are reported to be more common by a ratio of 4:1 [2]. We present a case of a patient with severe radicular symptoms with an intraspinal lumbar facet joint cyst diagnosed by magnetic resonance imaging and treated by computerized tomography (CT)-guided injection, aspiration, and rupture.
Case report
The patient is a 63-year-old woman with increasing left-sided radicular symptoms. Magnetic resonance imaging (MRI) of the lumbar spine revealed severe left-sided facet joint arthrosis with only mild disc degeneration. Immediately adjacent to the degenerated left L5–S1 facet joint was a 7-mm cyst compressing the left S1 nerve root in the left lateral recess (Figs. 1 and 2). Despite oral medications, the patient experienced no relief of her symptoms. Due to a complex medical history, it was decided that conservative management be employed, and percutaneous cyst aspiration, injection, and rupture was performed.
Fig. 1.
Axial T2 weighted image demonstrating a fluid intensity cyst (white arrow) just anteromedial to the degenerated left L5–S1 facet joint compressing the left S1 nerve root in the lateral recess
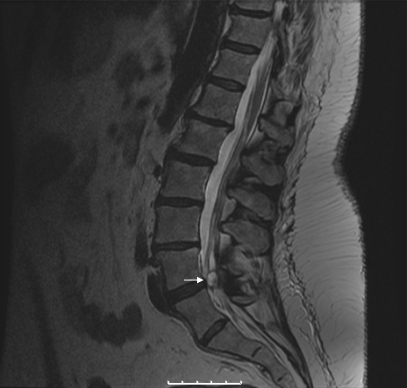
Fig. 2.
Sagittal T2 weighted image demonstrating a fluid intensity cyst (white arrow) within the spinal canal
A computerized axial tomography scan-guided approach was chosen over fluoroscopically guided facet joint injection given the more reliable placement of the needle directly into the cyst under CT guidance. Under intermittent CT guidance, a 20 gauge long spinal needle was placed into the left facet joint utilizing a posterior approach and initial aspiration was attempted (Fig. 3a, b). A small amount of radiographic contrast material was injected to confirm communication with the facet joint, and attempts to rupture the cyst by distending the cyst through the degenerated facet joint were made and unsuccessful. A second 20 gauge long spinal needle was then directed under intermittent CT guidance directly into the cyst via an angled translaminar approach while avoiding the thecal sac (Fig. 4). The cyst was mechanically perforated and aspirated, yielding only a trace amount of thick viscous fluid. In hopes of preventing recurrence of the cyst and inflammation related to the release of synovial fluid into the epidural space, a mixture of cortisone and 1% lidocaine was injected into both the facet joint and cyst with medication re-distributing into the epidural space (Figs. 5 and 6). Short-term follow-up with the referring physician revealed satisfactory relief of radicular symptoms.]
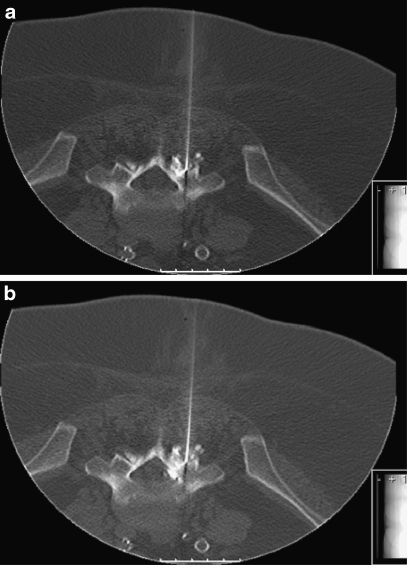
Fig. 3.
Axial CT image demonstrating a needle and contrast material injected in the facet joint (a) with subsequent filling of facet joint cyst (b)
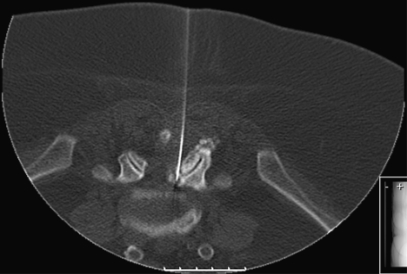
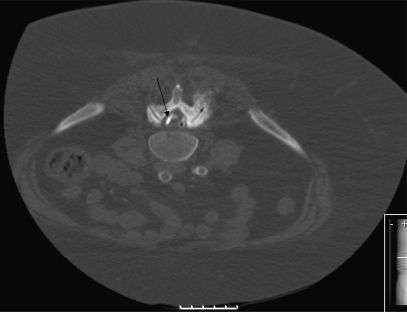
Fig. 4.
Axial CT image demonstrating a separate needle inserted directly into the facet joint cyst after attempted rupture by facet joint injection
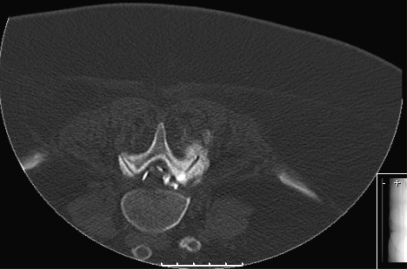
Fig. 5.
Axial CT image demonstrating contrast material outside the cyst and facet joint in the epidural space from successful rupture
Fig. 6.
Axial CT image demonstrating contrast material (black arrow) outside the cyst and facet joint in the epidural space from successful rupture
Discussion
Synovial cysts arise from the facet joint and, if they extend anteriorly, are typically located posterolateral to the thecal sac contributing to central canal or lateral recess stenosis with nerve root compression [3]. These cysts are exceedingly rare in the thoracic and cervical spine. Speculation concerning the increased prevalence of posterior extra-canalicular cysts is thought to be related to the presence of the ligamentum flavum as a mechanical barrier to anterior cyst formation. In addition, supine positioning may provide a gravitational factor by increasing the intra-articular pressure at the posterior aspect of the joint relative to the anterior intra-articular aspect of the joint [2].
Lumbar facet joint synovial cysts are found most commonly at the L4–5 motion segment, the least stable of the lumbar levels and where spondylolisthesis is also most prevalent. This suggests that underlying micro instability of the motion segment and chronic hypermobility are in part related to facet joint synovial cyst formation [1]. Regardless of the presence of facet joint osteoarthrosis and micro-instability, facet joint cysts are relatively rare with a reported prevalence in symptomatic patients of 0.65–2.3% [1, 2]. The next most common level for synovial cyst occurrence is L5–S1 followed by L3–4, followed by L2–3 [4].
The imaging appearance of facet joint cysts can be variable on both MRI and CT. Synovial cysts are typically defined as round or ovoid collections composed of varying types of fluid arising from the facet joint and projecting beyond the margins of the joint [2]. On CT scan, they may have varying densities depending on the composition of the cyst. Simple fluid density suggests a serous type of synovial fluid with increasing density suggestive of inspissation, hemorrhage, or increased protein or calcium content. Air density within the cyst can result from a negative pressure void allowing for dissolved nitrogen in fluid to sublimate into a gaseous state [5]. Similarly, the appearance on MRI can also vary with a predominantly serous fluid containing cyst demonstrating a well-defined hypo-intense rim with characteristic hyper-intense fluid signal on T2 weighted imaging and hypo-intensity on T1 weighted imaging. Increased signal on T1 weighted sequences may herald the presence of hemorrhage or increased protein content, while markedly diminished signal intensity on all pulse sequences may reflect the presence of hemosiderin, calcification, or nitrogen gas within the cyst [5].
Facet joint injection demonstrating communication of the facet joint with the cyst is pathognomonic for the presence of a synovial cyst. The differential diagnosis includes ganglion cysts, posterior longitudinal ligament cysts, and ligamentum flavum cysts; however, these cysts do not communicate with the facet joint and are not lined with epithelium [1]. Confounding the problem is the theory that synovial and ganglion cysts may be the same entity at different points of the disease process, with ganglion cysts occurring as a result of degeneration of a synovial cyst [1]. One study reviewing the surgical excision and histopathological evaluation of facet joint cysts showed no synovial lining in their samples [6]. The process is thought to begin with synovial herniation through a defective joint capsule [6]. Anantomical differences in the consistency of the ligamentum flavum, with increased collagen rather than elastic fibers, contribute to inherent weaknesses at the capsular portion of the ligamentum as opposed to the interlaminar portion predisposing the capsular portion to injury and cyst formation [6].
Treatment for lumbar facet joint synovial cysts includes both conservative and surgical treatments with reports of spontaneous resolution if left untreated [1]. While surgery is the gold standard for the treatment for symptomatic facet joint cysts, conservative options include bed rest, physical therapy, acupuncture, oral analgesics and anti-inflammatories, and percutaneous injection and aspiration [4, 7]. Surgical treatment is most effective, with very rare instances of recurrence when the entire cyst is excised but is not without inherent risks. Typically, surgical treatment requires laminectomy and/or facetectomy and now includes a minimally invasive endoscopic/microscopic approach [4, 7]. Common surgical risks include spinal instability, dural tear, neurologic injury, epidural hemorrhage and hematoma, seroma, and cyst recurrence [4]. In some instances, spinal fusion is performed, especially if there is concurrent spinal instability [7]. Typically, the procedure of choice is tailored depending on cyst size, adherence of the cyst to the dura, and concomitant disease. Cyst size has been reported to increase the risk of dural adhesion resulting in subtotal resection of the cyst to prevent the risk of dural tear [7]. Surgical treatment is typically recommended as soon as conservative measures fail to alleviate symptoms [7]. Percutaneous interventions are usually indicated in elderly or high-risk patients.
Under image-guided assistance, transforaminal or interlaminar epidural corticosteroid and anesthetic injection can be performed pre-emptively or concurrently to reduce the risk of procedure-related pain [4]. The advantage of CT over fluoroscopy is the direct treatment of synovial cysts as well as ganglion, posterior longitudinal ligament, and ligamentum flavum cysts that do not communicate with the facet joint, therefore allowing direct, safe, and reliable puncture of the cyst without dural violation. As reported by one study, percutaneous intervention has a 70% probability of long-term success with a 37.5% risk of recurrence and 45% chance of success after repeat cyst rupture [4].
In conclusion, percutaneous CT-guided lumbar facet joint cyst treatment is a safe, reliable, and nonsurgical method of treating symptomatic lumbar spine facet cysts.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ayberk G, Ozveren F, Gok B, Yazgan A, Tosun H, Seckin Z et al (2008) Lumbar synovial cysts: Experience with nine cases. Neurol. Med.-Chir. 48(7):298–303 discussion 303 [DOI] [PubMed]
- 2.Doyle AJ, Merrilees M (2004) Synovial cysts of the lumbar facet joints in a symptomatic population: Prevalence on magnetic resonance imaging. Spine 29(8):874–878 [DOI] [PubMed]
- 3.Epstein NE (2004) Lumbar synovial cysts: A review of diagnosis, surgical management, and outcome assessment. J. Spinal Disord. Tech. 17(4):321–325 [DOI] [PubMed]
- 4.Allen TL, Tayli Y, Lutz GE (2008) Fluoroscpoic percutaneous lumbar zygapophyseal joint cyst rupture: A clinical outcome study. Spine J. 8(Issue 5, Supplement 1):68S [DOI] [PubMed]
- 5.Marichal DA, Bertozzi JC, Rechtine G, Murtagh FR (2006) Case 101: Lumbar facet synovial cyst. Radiology 241(2):618–621 [DOI] [PubMed]
- 6.Kusakabe T, Kasama F, Aizawa T, Sato T, Kokubun S (2006) Facet cyst in the lumbar spine: Radiological and histopathological findings and possible pathogenesis. J. Neurosurg. Spine 5(5):398–403 [DOI] [PubMed]
- 7.Boviatsis EJ, Staurinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M et al (2008) Spinal synovial cysts: Pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur. Spine J. 17(6):831–837 [DOI] [PMC free article] [PubMed]