Abstract
Rationale and Objectives
We sought to examine heart rate and heart rate variability during cardiac computed tomography (CT).
Materials and Methods
Ninety patients (59.0 ± 13.5 years) underwent coronary CT angiography (CTA), with 52 patients also undergoing coronary artery calcium scanning (CAC). Forty-two patients with heart rate greater than 70 bpm were pretreated with oral β-blockers (in five patients, use of β-blocker was not known). Sixty-four patients were given sublingual nitroglycerin. Mean heart rate and percentage of beats outside a ±5 bpm region about the mean were compared between baseline (free breathing), prescan hyperventilation, and scan acquisition (breath-hold).
Results
Mean scan acquisition time was 13.1 ± 1.5 seconds for CAC scanning and 14.2 ± 2.9 seconds for coronary CTA. Mean heart rate during scan acquisition was significantly lower than at baseline (CAC 58.2 ± 8.5 bpm; CTA 59.2 ± 8.8 bpm; baseline 62.8 ± 8.9 bpm; P < .001). The percentage of beats outside a ±5 bpm about the mean were not different between baseline and CTA scanning (3.5% versus 3.3%, P = .87). The injection of contrast had no significant effect on heart rate (58.2 bpm versus 59.2 bpm, P = .24) or percentage of beats outside a ±5 bpm about the mean (3.0% versus 3.3%, P = .64). No significant difference was found between gender and age groups (P > .05).
Conclusions
Breath-holding during cardiac CT scan acquisition significantly lowers the mean heart rate by approximately 4 bpm, but heart rate variability is the same or less compared with normal breathing.
Keywords: Heart rate, computed tomography, coronary angiography
The patient's heart rate and heart rate variation play a very important role in cardiac computed tomography (CT) examinations, e.g., CT coronary artery calcium (CAC) and coronary CT angiography (CTA) (1-4), due to the limit of temporal resolution available in current CT systems (for single segment image reconstruction, this is as fast as 0.165 second using single-source CT or 0.85 second using dual-source CT) (5,6). A study to evaluate the effect of heart rate on the quality of CT angiography exams obtained with 16-channel multidetector row CT (MDCT) demonstrated a significant negative correlation between mean heart rate and image quality (7). Besides mean heart rate, significant variations in heart rate (e.g., from 41 to 100 bpm [beats per minute] during scanning, equivalent to an R-R interval ranging from 1463 to 600 msec), result in misregistration of ECG-gated data and severe discontinuities in the reconstructed cardiac images (Fig. 1). Thus, most vendors offer an ECG editor that allows the operator to modify the synchronization and thereby reduce artifacts caused by short-term variations of the patient's heart rate (8).
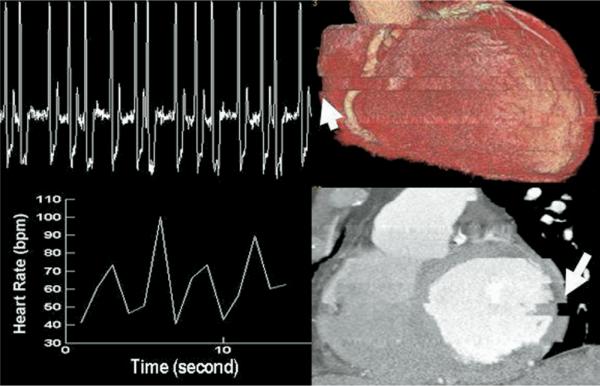
Figure 1.
An example of an erratic heart rate and the resultant CT images in a patient with atrial fibrillation or other arrhythmia. The heart rate changed from 40 bpm to 100 bpm during CT scan acquisitions. This variation in the heart rate resulted in significant discontinuities in the CT images (arrows).
Although underlying disease is the most important factor influencing individual patient's heart rate and its variability, heart rate and heart rate variability may be influenced by many other factors under the clinical conditions that exist during a cardiac CT exam. These include breath-holding during the scan, the injection of intravenous contrast media, the use of β-blockers or nitroglycerin, and patient demographics (age, gender). Typical exam times for 16-channel MDCT range from 20 to 25 seconds (9). With the introduction of 64-channel MDCT, the time required to image the heart has decreased to approximately 5 to 15 seconds, depending on the scanner model used. While some have reported an increase in heart rate with lengthy breath-holding during scan acquisition (10), the magnitude of heart rate and heart rate variation within a 5- to 15-second time frame have not been previously evaluated.
The purpose of our study was to examine heart rate and heart rate variability during cardiac CT examinations, and to investigate the potential influence of breath-holding, iodinated contrast media, age, gender, β-blockade, and nitroglycerin on heart rate and heart rate variability.
MATERIALS AND METHODS
Following institutional review board approval of this retrospective data analysis, HIPAA (Health Insurance Portability and Accountability Act)-compliant study, we examined ECG data from patients who had undergone coronary CT angiography on a 64-channel CT system during the study period and who had consented to the use of medical records for research purposes. Patients who had declined authorization for use of their medical records in research were excluded from participation.
Data Acquisition
For routine cardiac CT examinations, three ECG leads are placed on the patient to record ECG signals for prospective triggering or retrospective gating. For the CT scanner used by our institution for cardiac CT, ECG data are recorded by the CT scanner and were stored in a DICOM file on an external hard drive for further analysis.
Inclusion Criteria
We examined ECG data from 101 consecutive patients undergoing coronary CTA examination between March 2, 2005, and September 15, 2005, using 64-channel MDCT (Sensation-64; Siemens Medical Solutions, Forchheim, Germany). When patients underwent a non—contrast-enhanced CAC scan, these data were also stored and analyzed.
Exclusion Criteria
Data from patients having atrial fibrillation, not consenting to the use of their medical records for research purposes, having beat-to-beat variability exceeding 20 bpm during baseline breathing, or with corrupted archived ECG data were excluded from data analysis.
Scanning Protocol
Per clinical protocol, patients with heart rate greater than 70 bpm were pretreated with oral β-blockers (n = 42), 50 or 100 mg, depending on patient's heart rate (50 mg for heart rate less than 80 bpm, 100 mg for heart rate equal to or greater than 80 bpm). When administered, β-blocker was given approximately 1 hour before CT examination.
For the coronary CTA examinations, a dual-injection technique was used to inject intravenous contrast media. A test bolus of 20 ml of iodinated contrast material (Visipaque 320; Amersham Health) followed by 30 ml of NaCl (0.9%) was injected, with monitoring scans performed at 1.5-second intervals to determine the time of peak enhancement in the ascending aorta. Following the test bolus procedure, sublingual nitroglycerin (0.4 mg) was given to dilate the coronary vessels for the purpose of improving CTA image quality (n = 64). Nitroglycerin was not given when contraindicated (systolic blood pressure below 100 mm Hg, aortic stenosis, obstructive hypertrophic cardiomyopathy, use of medications for erectile dysfunction within 48 hours) or at patient's request or physician's discretion. Approximately 60 seconds later, 80 ml of iodinated contrast material (Visipaque 320; Amersham Health) followed by 70 ml of contrast medium and NaCl was injected at 4 ml/sec.
Both CAC and CTA examinations were performed using retrospective ECG-gated spiral scanning with a pitch value of 0.2, where pitch is defined as the ratio of the table increment per tube rotation to the total nominal beam width. Scanning was performed using an x-ray tube potential of 120 kVp and an effective tube current-time product (mAseff = tube current-time product/pitch) of 850 mAseff for the CTA exams or 220 mAseff for the CAC exams. The detector collimation was 32 × 0.6 mm, and the z-flying focal spot technique was used, resulting in 64 overlapping projections per angular sample (5). Images were reconstructed using a single segment image reconstruction algorithm.
Data Analysis
Using the archived digital ECG data recorded from the scanner, an automated program written by one of the authors (J.Z.) (MATLAB; The MathWorks, Natick, MA) was used to locate the peaks of each R wave and determine, on a beat-by-beat basis, the heart rate (in bpm) that corresponded to each RR interval.
The mean heart rate, standard deviation, percentage of heartbeats with a variable rate (defined as the percentage of beats outside a ±5 bpm range about a patient's mean heart rate for the scan period), and the minimum to maximum range of heart rates for each patients were computed for three time segments: baseline (during normal breathing), hyperventilation (following instruction to take in a deep breath), and during CT scan acquisition (breath-holding) (Fig. 2).
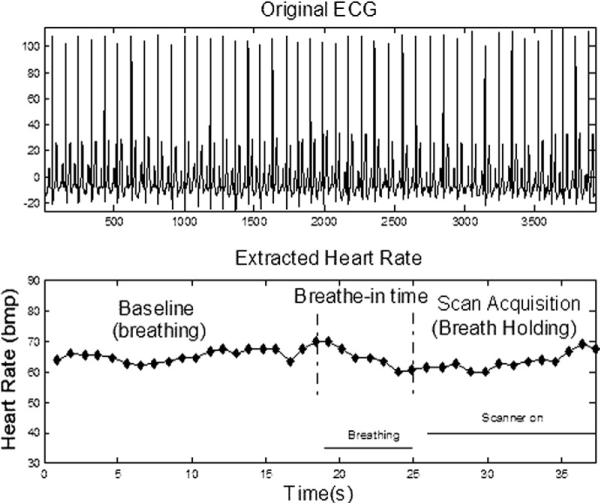
Figure 2.
Original ECG data and corresponding extracted heart rates using a MATLAB-based program during three time segments of CT acquisition: baseline breathing, breath-in time (hyperventilation), and scan acquisition.
The three time segments were identified based on the time information recorded by the CT scanner. For all patients, the baseline breathing data were obtained in the time just before coronary CTA scan hyperventilation— after the small amount of contrast injection (i.e., the “test bolus”) used for the determination of circulation time but before the start of the intravenous contrast injection for the CTA acquisition. The hyperventilation period was the 6 seconds immediately before scan acquisition. The start of this time period was initiated by the use of the automated operator instructions, which directed the patient to take in a deep breath and hold it. These instructions were initiated 6 seconds before the start of CT data acquisition. The scan acquisition time (i.e., breath-holding time) varied according to the length of anatomy scanned. ECG data before the CAC acquisition were not recorded by the system; hence, baseline (during normal breathing) data for the CAC examinations could not be examined.
Statistical Analysis
For each patient, the mean heart rates were calculated separately for each of the five scan periods (CAC hyperventilation, CAC scanning, baseline breathing, CTA hyperventilation, and CTA scanning). Heart rate variability was measured by calculating the percentage of heartbeats either 5 or more beats below or 5 or more beats above the mean heart rate for any given period and was estimated for each of the three periods of time around the CTA scan (before breath-holding, during hyperventilation, during CT acquisition), as well as the two periods around the CAC scan (during hyperventilation and during CT acquisition). These estimates of mean heart rate and heart rate variation are reported as a mean and standard deviation for each of the five scan periods. A paired t-test was used to compare estimates (both the mean rate and percentage outside ±5 bpm of the mean rate) between five different pairs of time periods (baseline breathing to CTA hyperventilation, baseline breathing to CTA scan acquisition, CTA hyperventilation to CTA scan acquisition, CAC hyperventilation to CTA hyperventilation, and CAC scan acquisition versus CTA scan acquisition).
A two-sample t-test was used to test for a significant difference in the mean heart rate between genders and age groups and for patients with (n = 42) and without (n = 43) the use of β-blockers (definitive use information unavailable in five patients) and with (n = 64) and without (n = 26) the use of sublingual nitroglycerin during each of the five time periods. The same comparisons were done for the estimates of heart rate variation.
Finally, to compare for potential changes in heart rate over the duration of the breath-holding (e.g., due to mild hypoxia), a paired t-test was used to compare the first and last three heartbeats recorded during CAC and CTA examinations.
Note that for comparisons solely within the CTA examination, a total of 90 patients were included in analyses, while for comparisons within the CAC examination, or across the CTA and CAC examinations, a total of 52 patients were included in analyses.
RESULTS
Of the 101 patients who underwent coronary CT angiography 57 also underwent CAC scanning. Eleven patients were excluded from analysis (atrial fibrillation/flutter, n = 4; not consenting to the use of their medical records for research purposes, n = 2; beat-to-beat variability exceeding 20 bpm during baseline breathing, n = 3; corrupted archived ECG data, n = 2). These 11 patients (8 men and 3 women) included 5 patients who underwent both CAC and CTA. The resultant amount of ECG data represented 90 patients undergoing coronary CT angiography, with 52 of these patients also undergoing precontrast CAC scanning.
The subjects were 52 men (mean age ± standard deviation: 57.7 ± 14.0 years; age range: 27-87 years) and 38 women (mean age ± standard deviation: 60.8 ± 14.6 years; age range: 26-90 years). The patients were divided into two different age groups as less than or equal to the median versus above the median (63.6 years), to investigate the possible influence of age on heart rate variability. There were no significant differences in age distribution between male and female patients of the group of 90 patients (P > .05). Mean scan acquisition time (i.e., time required for the breath-hold) was 13.1 ± 1.5 seconds for CAC scanning and 14.2 ± 2.9 seconds for coronary CTA.
Table 1 shows the mean heart rate and percentage of heartbeats with a variable rate during baseline breathing, CAC hyperventilation, CAC scan acquisition, coronary CTA hyperventilation, and coronary CTA scan acquisition. Table 2 shows the difference in mean heart rates across all patients between time periods. There was a slight but significant reduction in mean heart rate from baseline breathing to CTA scan acquisition (mean heart rate difference = 3.6 bpm, P <.001). The mean heart rate during baseline breathing was 62.8 ± 8.9 bpm, decreasing to 59.2 ± 8.8 bpm during CTA scan acquisition. Similar reductions in heart rate were observed between hyperventilation periods and scanning (P <.01). There was no difference in mean heart rate during CAC scan acquisition and CTA scan acquisition (mean heart rate difference = 0.9 bpm, P = .24).
Table 1.
Mean heart rate and percentage of heartbeats with a variable rate* for each of the five time periods shown
| CAC (n = 52) |
CTA (n = 90) |
||||
|---|---|---|---|---|---|
| Parameter | Baseline | Hyperventilation | Scan Acquisition | Hyperventilation | Scan Acquisition |
| Heart rate (bpm; mean ± SD) | 62.8 ± 8.9 | 61.4 ± 7.8 | 58.2 ± 8.5 | 63.9 ± 9.5 | 59.2 ± 8.8 |
| Heart rate range (bpm) | 46.9-92.0 | 48.2-85.6 | 41.9-88.4 | 41.6-95.7 | 40.6-88.3 |
| Percentage of beats with variable heart rate* | 3.5 ± 11.0 | 12.7 ± 22.3 | 3.0 ± 8.4 | 14.5 ± 24.8 | 3.3 ± 10.2 |
Defined as the percentage of beats during the time period outside a ±5 bpm range about the mean heart rate.
Table 2.
Comparison of mean heart rates during five time periods
| Time Period 1 | Time Period 2 | No. of Patients | Mean Difference (SD) in Heart Rates (Across All Patients)* | Significance (Paired t-Test) |
|---|---|---|---|---|
| CTA baseline breathing | CTA hyperventilation | 90 | -1.2(3.3) | <.001 |
| CTA baseline breathing | CTA scanning | 90 | 3.6 (4.4) | <.001 |
| CTA hyperventilation | CTA scanning | 90 | 4.8 (5.0) | <.001 |
| CAC scanning | CAC scanning | 52 | -0.9 (5.1) | .24 |
| CAC hyperventilation | CAC scanning | 52 | 3.2 (3.4) | <.001 |
A positive value means that the value for time period 1 is bigger than for time period 2, and a negative value means the estimate for time period 2 is larger.
Table 3 compares the heart rate variability between these five time periods, showing the mean difference in percentage of heartbeats with a variable rate between pairs of time periods. Importantly, there was no difference in percentage of heartbeats with a variable rate between baseline breathing and CTA scanning (difference in percentage of variable beats between baseline breathing and CTA scan acquisition =+0.3%; P = .87). Additionally, relating to the effect of intravenous contrast media administration on heart rate, there was no difference in heart rate variability during CAC scan acquisition and coronary CTA scan acquisition (difference in percentage of variable beats between CAC and CTA scan acquisition = -1.0%; P = .64). Matched mean testing demonstrated no change in the mean heart rate between the first three and last three beats of each scan acquisition (P >.05).
Table 3.
Comparison of heart rate variability during time periods
| Time Period 1 | Time Period 2 | No. of Patients | Mean Difference (SD) in Percentage of Variable Beats (Across All Patients)* | Significance (Paired t-Test) |
|---|---|---|---|---|
| CTA baseline breathing | CTA hyperventilation | 90 | -11.0 (25.3) | <.001 |
| CTA baseline breathing | CTA scanning | 90 | 0.3 (15.5) | .87 |
| CAC scanning | CTA scanning | 52 | -1.0 (15.4) | .64 |
| CAC hyperventilation | CTA hyperventilation | 52 | -2.3 (23.2) | .47 |
| CAC scanning | CAC scanning | 52 | -1.0 (15.4) | .64 |
| CAC hyperventilation | CAC scanning | 52 | 9.7 (23.5) | .004 |
The percentage of beats more than 5 bpm different from the mean heart rate were compared for each patient between the time periods shown.
A positive value means that the estimate for time period 1 had a greater percentage of variable beats than for time period 2, and a negative value means the estimate for time period 2 is larger.
Table 4 describes the mean heart rate and heart rate variation by patient age, gender, β-blockade, and nitroglycerin administration. There was no significant difference in mean heart rate or heart rate variability between patients greater than or less than 63.6 years (i.e., the median age), or between males and females, during any of the five time periods (P <.05).
Table 4.
Heart rate and heart rate variation during CT scan acquisition by age, gender, β-blockade, and nitroglycerin administration
| Age (yr) |
Gender |
β-Blockade† |
Nitroglycerin |
|||||
|---|---|---|---|---|---|---|---|---|
| Parameter | <63.6 (n = 45) | >63.6 (n = 45) | Male (n = 52) | Female (n = 38) | With (n = 42) | Without (n = 43) | With (n = 64) | Without (n = 26) |
| Heart rate (bpm) | ||||||||
| Mean ± SD | 59.8 ± 10.2 | 58.5 ± 7.2 | 59.4 ± 10.2 | 58.8 ± 6.6 | 59.2 ± 7.6 | 59.0 ± 10.2 | 58.9 ± 18.8 | 59.9 ± 9.4 |
| rcentage | 40.6-88.3 | 46.0-75.5 | 40.6-88.3 | 46.9-74.4 | 45.3-79.3 | 40.6-88.3 | 40.6-88.3 | 46.0-75.5 |
| Percentage beats with variable heart rate* | ||||||||
| Mean ± SD | 3.7 ± 9.9 | 2.9 ± 10.6 | 4.3 ± 13.0 | 1.9 ± 3.8 | 2.9 ± 8.3 | 3.7 ± 12.2 | 2.8 ± 8.6 | 5.0 ± 14.8 |
| Range | 0-50 | 0-68 | 0-68 | 0-13 | 0-50 | 0-68 | 0-50 | 0-68 |
Defined as the percentage of beats during the study period outside a ±5 bpm range about the mean heart rate.
β-Blockade information was not available in five patients.
Additionally, there was no significant difference between mean heart rate or heart rate variability between any of the time periods, when comparing patients who received with those who did not receive nitroglycerin. Similarly, there was no significant difference between heart rate variability between any of the time periods, when comparing patients who received β-blockade and those who did not (for five patients, β-blockade use was not available). Those patients who received β-blockade tended to lower their heart rates more during breath-holding for CTA scan acquisition (-1.8 bpm versus 0.5 bpm), but this trend did not reach statistical significance (P = .06).
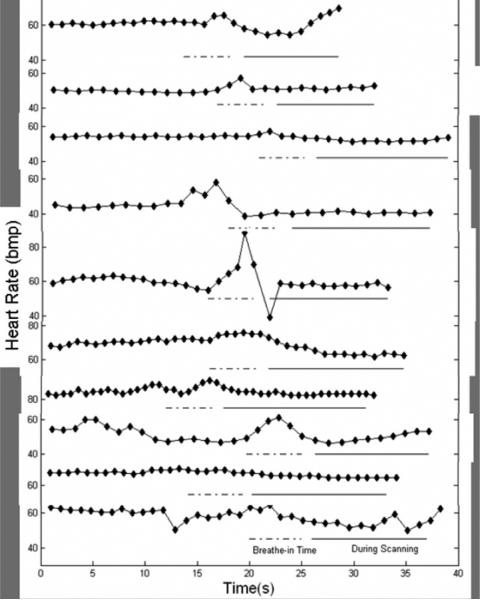
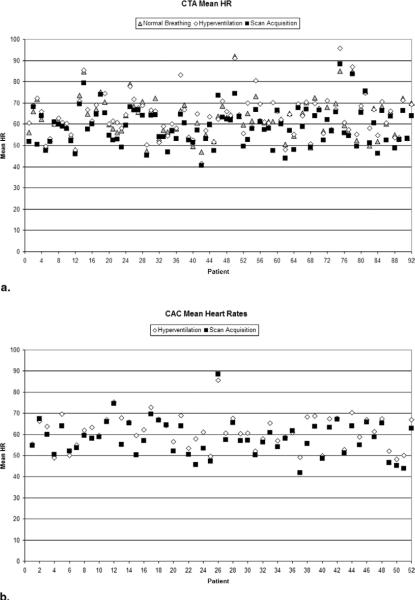
Figure 3 shows sample ECG profiles for the first 10 patients (when sorted according to alphabetic order). Figure 4 shows a scatterplot of mean heart rate (bpm) for 90 patients who underwent CTA examinations and demonstrates that during CT scan acquisition, mean heart rate was generally lower than during baseline breathing.
Figure 3.
ECG profiles of 10 patients chosen according to alphabetic order. Heart rate during hyperventilation is designated by the dotted line, while heart rate during scan acquisition is designated by the solid line
Figure 4.
a, Scatterplot of mean heart rate (bpm) for 90 patients who underwent CTA examinations (shaded triangle, baseline during normal breathing; open diamond, during hyperventilation; filled box, during CTA scan acquisition with breathhold). For a given patient, mean heart rate during CTA acquisition was generally lower than during baseline breathing or hyperventilation in the same patient. b, Scatterplot of mean heart rate (bpm) for 52 patients who underwent CAC examinations (open diamond, during hyperventilation; filled box, during CAC scan acquisition with breath-hold). For a given patient, mean heart rate during CAC scanning was generally lower than during hyperventilation in the same patient.
DISCUSSION
Previous studies have shown that reducing average heart rate and heart rate variability is beneficial for reducing cardiac imaging artifacts (1,2). Despite these findings, little quantitative information is available about how heart rate and heart rate variation if affected by a cardiac CT scan acquisition. We studied the heart rate and heart rate variation during cardiac CT exams in three time periods relating to cardiac CT: baseline breathing, prescan hyperventilation, and scan acquisition (during breath-holding).
We found that heart rate was slightly but significantly lowered during cardiac CT acquisition (by about 4 bpm, P < .01), compared to prescan baseline breathing. These results were true regardless of the use of intravenous contrast for the coronary CTA exams, during which heart rate did not vary significantly from the heart rate during non-contrast CAC scanning (P = .24). More important, however, we found there was no difference in the percentage of heartbeats with a variable rate (defined as more than 5 bpm deviation from the mean) between baseline breathing and CTA acquisition (P = .87). There was also no difference in heartbeat variability between contrast-enhanced coronary CTA and noncontrast CAC acquisitions (P = .64). Additionally, heart rate variability did not differ between scan periods when multiple potential confounding factors were taken into account, including gender, age, nitroglycerin, and β-blocker use.
In the absence of cardiac arrhythmias, there are two possible factors that may influence beat-to-beat variability during CT acquisition: physiological factors such as apneic bradycardia during breath-holding and random events such as the occasional premature ventricular contraction (PVC). To examine the physiological effect of breathholding on heart rate during the apneic scan acquisition period, we compared the mean heart rate between the first three heartbeats and the last three heartbeats during CT acquisition. No significant difference was observed (P > .05). Therefore, apnea for scan periods of 12 to 15 seconds appears to have no influence on heart rates.
Reducing scan time, however, may reduce the possibility of random events such as a PVC. Most current CT scanners have software that permits editing of ECG data with retrospective ECG-gating to address small heart rate variations, that is, a single premature beat, to yield acceptable image quality. If there is greater variability, such as multiple random events, shorter scan times may help reduce image degradation due to the use of a shorter scan acquisition window. This can be achieved using a wider detector (e.g., 64 detector rows instead of 32), which allows the system to scan the heart in fewer gantry rotations. However, in this case, each premature heartbeat affects larger portions of the data set, which may also compromise the exam quality. While a wider detector decreases overall scan time, it does not improve the temporal resolution of a given image, which is dependent on the gantry rotation time, reconstruction algorithm, and source geometry (5). Alternatively, a larger pitch value can be used, which increases the table speed. However, the maximum pitch value is limited by the patient's heart rate, and a significant pitch increase cannot be achieved if multisector reconstructions are to be used for high heart rates (>70 bpm), which is necessary for current single-source CT technology with temporal resolutions of approximately 165 to 200 msec.
This study had several limitations. Cardiac CT imaging requires patients to take a breath in and hold their breath in order to eliminate motion artifact caused by respiration. However, it is difficult to control the extent of breathholding between patients. Given the fact that reductions in heart rate during apnea are proportional to initial lung volumes (11), with the greatest reduction in heart rate occurring when apnea is performed at the vital capacity, variations in breath-holding extent will alter the magnitude of the heart rate reductions. Additionally, we only examined heart rate and heart rate variability with respect to acquisition times for 64-channel CT, and not other acquisition protocols or using slower speed scanners. Finally, in this study, patients with heart rates greater than 70 bpm received β-blockers before their CT scans. Further studies will be necessary to determine heart rate variation during cardiac CT scanning for non-β-blocked patients having higher heart rates.
CONCLUSIONS
The results in this study indicate the following for patients presenting for clinically indicated cardiac CT: (1) breath-holding during cardiac CT scan acquisition modestly but significantly lowers the mean heart rate by approximately 4 bpm, (2) for cardiac CTA examinations, heart rate variation during scan acquisition (breath-holding) is not statistically different than during baseline breathing (i.e., before breath-holding), and (3) gender, age, injection of contrast media, β-blockade and nitroglycerin may not significantly influence heart rate or heart rate variation during scan acquisition.
REFERENCES
- 1.Lu B, Zhuang N, Mao SS, Child J, Carson S, Budoff MJ. Baseline heart rate-adjusted electrocardiographic triggering for coronary artery electronbeam CT angiography. Radiology. 2004;233:590–595. doi: 10.1148/radiol.2332030953. [DOI] [PubMed] [Google Scholar]
- 2.Lu B, Mao SS, Zhuang N, et al. Coronary artery motion during the cardiac cycle and optimal ECG triggering for coronary artery imaging. Invest Radiol. 2001;36:250–256. doi: 10.1097/00004424-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Boll DT, Gilkeson RC, Merkle EM, Fleiter TR, Duerk JL, Lewin JS. Functional cardiac CT and MR: Effects of heart rate and software applications on measurement validity. J Thorac Imaging. 2005;20:10–16. doi: 10.1097/01.rti.0000154077.13947.8e. [DOI] [PubMed] [Google Scholar]
- 4.Hong C, Becker CR, Huber A, et al. ECG-gated reconstructed multi-detector row CT coronary angiography: Effect of varying trigger delay on image quality. Radiology. 2001;220:712–717. doi: 10.1148/radiol.2203010055. [DOI] [PubMed] [Google Scholar]
- 5.Flohr TG, Stierstorfer K, Ulzheimer S, Bruder H, Primak AN, McCollough CH. Image reconstruction and image quality evaluation for a 64-slice CT scanner with z-flying focal spot. Med Phys. 2005;32:2536–2547. doi: 10.1118/1.1949787. [DOI] [PubMed] [Google Scholar]
- 6.Flohr TG, McCollough CH, Bruder H, et al. First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol. 2006;16:256–268. doi: 10.1007/s00330-005-2919-2. [DOI] [PubMed] [Google Scholar]
- 7.Hoffmann MH, Shi H, Manzke R, et al. Noninvasive coronary angiography with 16-detector row CT: Effect of heart rate. Radiology. 2005;234:86–97. doi: 10.1148/radiol.2341031408. [DOI] [PubMed] [Google Scholar]
- 8.Cademartiri F, Mollet NR, Runza G, et al. Improving diagnostic accuracy of MDCT coronary angiography in patients with mild heart rhythm irregularities using ecg editing. AJR Am J Roentgenol. 2006;186:634–638. doi: 10.2214/AJR.04.1797. [DOI] [PubMed] [Google Scholar]
- 9.Mollet NR, Cademartiri F, Nieman K, et al. Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol. 2004;43:2265–2270. doi: 10.1016/j.jacc.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 10.Garcia MJ. Tips and tricks to optimize image quality. The 6th International Conference on Cardiac CT; Boston, Massachusetts. 2005. [Google Scholar]
- 11.Song SH, Lee WK, Chung YA, Hong SK. Mechanism of apneic bradycardia in man. J Appl Physiol. 1969;27:323–327. doi: 10.1152/jappl.1969.27.3.323. [DOI] [PubMed] [Google Scholar]