Abstract
Rationale
Families of ICU patients may be at risk for increased psychological morbidity due to end-of-life decision-making. Identification of chart-based quality indicators of palliative care that predict family satisfaction with decision-making may help guide interventions to improve decision-making and family outcomes.
Objective
To determine patient and family characteristics and chart documentation of processes of care that are associated with increased family satisfaction with end-of-life decision-making for ICU patients.
Methods
We conducted a cohort study of ICU patients dying in 10 Seattle-Tacoma area medical centers.
Measurement
Outcomes from family surveys included summary scores for family satisfaction with decision-making and a single item score that indicated feeling supported during decision-making. Predictor variables were obtained from surveys and chart abstraction.
Main Results
Survey response rate was 41% (442/1074). Analyses were conducted on 356 families with questionnaire and chart abstraction data. Family satisfaction with decision-making was associated with withdrawal of life-support and chart documentation of: physician recommendations to withdraw life-support; discussions of patients’ wishes; and discussions of families’ spiritual needs. Feeling supported during decision-making was associated with withdrawal of life-support, spiritual care involvement and chart documentation of: physician recommendations to withdraw life-support; expressions of families’ wishes to withdraw life-support; and discussions of families’ spiritual needs.
Conclusions
Increased family satisfaction with decision-making is associated with withdrawing life-support and documentation of palliative care indicators including: physician recommendations to withdraw life-support, expressions of patients’ wishes and discussions of families’ spiritual needs. These findings provide direction for future intervention studies to improve family satisfaction in end-of-life decision-making.
Keywords: end-of-life, palliative care, decision-making, Post Traumatic Stress Disorder, family satisfaction
INTRODUCTION
Approximately 20% of all deaths in the United States occur in the intensive care unit (ICU)1 and the majority of ICU deaths involves decisions to withdraw life-support.2,3 Because patients in the ICU are usually too ill or sedated to express their treatment preferences and values, a surrogate decision maker is often involved. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment demonstrated that many physicians were unaware of their patients’ preferences for end-of-life treatment and did not follow these preferences in the care that they delivered.4 Therefore, family members play an important role in decision-making in the ICU setting.
There is growing recognition of the importance of developing a model that describes shared decision-making in the ICU. However, there is considerable variability in approaches to accomplish this.5 Research has demonstrated that communication between physicians and surrogate decision makers is often poor.6, 7 For example, one study found that 35% of surrogate decision makers did not understand the physician’s explanation about the diagnosis or options for further care of the patient.7 Similarly, another study found that almost half of surrogate decision makers reported that physician-family communication was incomplete in the ICU.8
Dissatisfaction with decision-making among family members in the ICU may not only affect patients’ care, but also the psychological health of the decision makers. Pochard reported that 73% of surrogate decision makers experienced anxiety and 35% experienced depression during their loved one’s ICU stay.9 Another study suggested that 33% of family members had a high burden of symptoms of Post Traumatic Stress Disorder (PTSD) and that family members had a higher burden of symptoms if they were involved in end-of-life decision-making.8 More recently, a randomized trial from France suggested that providing a bereavement packet and standardizing “end-of-life family conferences” to encourage family participation significantly decreased family symptoms of depression, anxiety, and PTSD three months after the patient’s death.10 Therefore, understanding and improving the satisfaction of family members with decision-making about end-of-life care in the ICU may be important not only for better patient-and family-centered care, but also as a way of reducing families’ risks for symptoms of anxiety, depression, and PTSD after the death of a loved one in the ICU.
There is increasing interest in using the medical chart to identify indicators of high quality palliative and end-of-life care in order to assess and improve the quality of care provided to patients and family members in the ICU. A recent consensus document proposed 18 chart-based indicators11 and others have proposed a “palliative care bundle” based on chart documentation of palliative care in the ICU.12
In this exploratory study, we identify factors documented in the medical chart that are associated with family members feeling more satisfied with and more supported during end-of-life decision-making. We hypothesize that there may be certain patient characteristics, family member characteristics and end-of-life care processes that are associated with increased satisfaction in decision-making and these may help guide the development of future interventions to improve shared decision-making in the ICU. In addition, we believe that understanding approaches that may improve satisfaction with decision-making in the ICU may be essential to reducing the risk of psychological disease in family members of patients that die in the ICU.
METHODS
Design
We are currently performing a cluster randomized trial of an interdisciplinary, quality improvement intervention to enhance palliative care in the ICUs of 15 Seattle-Tacoma area hospitals. For the current analyses, we used baseline survey and medical record abstraction data from 10 of these hospitals (data collected 8/09/03 to 11/27/05). Hospitals included a university-affiliated county hospital (65 ICU beds), two community-based teaching hospitals (44 and 45 ICU beds) and seven community-based non-teaching hospitals (ranging in size from 15 to 45 ICU beds).
Questionnaires
The Family Satisfaction in the ICU (FS-ICU) survey is a valid and reliable instrument designed to measure family satisfaction with ICU care. Details of the questionnaire’s original development and validation are presented elsewhere.13, 14 Recently, Wall and colleagues developed a validated scoring method for the FS-ICU and empirically demonstrated two domains within the instrument: satisfaction with care (FS-ICU Care) and satisfaction with decision-making (FS-ICU Decision-making).15
In the current study, our objective was to identify factors associated with family satisfaction with decision-making. Therefore, we used the FS-ICU Decision-making subscale as our primary outcome variable. The subscale score was the mean of all valid responses on 10 relevant items and transformed to range from 0 to 100, with higher scores indicating more satisfaction. Examples of the questionnaire items included “Did you feel included in the decision-making process?” and “Did you receive an appropriate amount of information to participate in the decision-making process?.” Total scores were calculated using a minimum of 1 valid response. Additionally, we included as a second outcome variable the single item, “Did you feel supported during the decision-making process?” (FS-Support). This item which is included in the FS-ICU Decision-making score was also arithmetically transformed to a 0 to 100 score from a 1 to 5 scale to provide a score directly comparable to the FS-ICU Decision-making subscale. This item was of interest because of its potential utility as a single item outcome for measuring the effect of interventions designed to enhance the family’s decision-making experience.
Study Participants
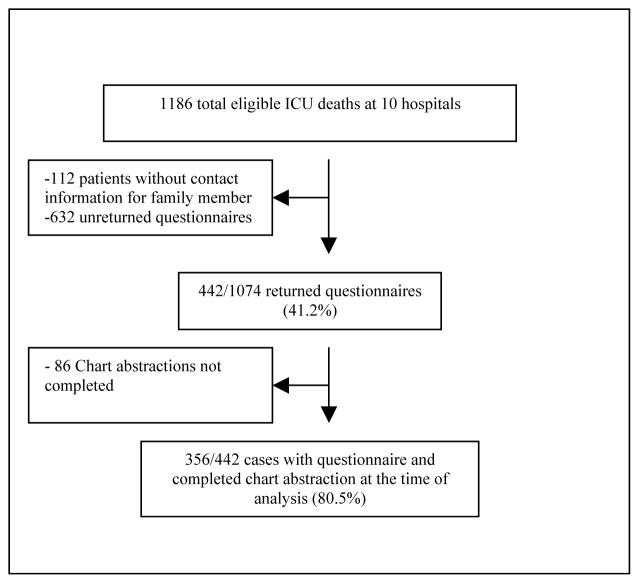
Figure 1 shows the development of the sample of study subjects. Subjects included all patients dying in the ICU or within 24 hours of transfer from the ICU and their family members. ICU decedents were identified using hospital admission, discharge and transfer records. Patients who died within 24 hours of being transferred from the ICU were included in order to capture patients that were transferred after life-support withdrawal. Family members were identified using two approaches. At one site, the legal next of kin was identified from electronic medical records. At the other nine sites, the questionnaire was sent to the patient’s home and addressed to the “Family of [patient’s name]”. All study procedures were approved by the Institutional Review Boards of all participating hospitals.
Figure 1.
Identification of cases for analysis.
Data Collection
Surveys with $10 incentives were mailed to the family member one to two months after the patient’s death and included a cover letter expressing condolences and explaining the purpose of the study. An option was offered to the recipient to defer to another individual (family or friend) who was involved in the patient’s care, if they preferred. Family members could refuse participation by returning a self-addressed stamped refusal card, calling a toll free number and leaving a message requesting no further mailings, or returning a blank questionnaire. A reminder/thank-you card was mailed 1 week after the initial mailing. If the questionnaire packet was not received within the following three weeks, a final mailing with a second copy of the survey was sent. These methods were used to enhance response rates.16
Patients’ medical records were reviewed by trained chart abstractors using a standardized chart abstraction protocol. Chart abstractor training included 80–120 hours (2–3 weeks) of formal training. Training included instruction on the protocol, guided practice charts and independent chart review with reconciliation with the research abstractor trainer. Abstractors were required to reach 90% agreement with the trainer before being able to code independently. After initial training, 5% of the charts were co-reviewed to ensure 95% agreement on the 440 abstracted data elements.
Data analysis
Our primary goal was to identify predictors of family satisfaction with decision-making when a loved one died in the ICU. We used two separate methods to assess family satisfaction with decision-making. First, we used the 10-item FS-ICU Decision-making subscale (FS-ICU Decision-making). Second, we examined a single FS-ICU item: “Did you feel supported during the decision-making process?” (FS-Support).
The predictor variables included patient characteristics (e.g., age, race and ethnicity, diagnosis), family member/friend characteristics (e.g., age, race, and ethnicity, education, relationship to patient) and processes of care that were documented in the medical record (e.g., withdrawing life-support, use of spiritual care services, documentation of discussions in family conferences) (Appendix 1). Kruskal-Wallis tests were calculated for categorical predictor variables and Mann-Whitney tests were performed for dichotomous predictor variables. Significance was reported at p≤0.05.
Appendix 1.
Predictor variables assessed.
| Patient |
|---|
| Demographics |
| Age at time of death |
| Gender |
| Race |
| Ethnicity |
| Insurance Status |
| Consults |
| Palliative Care Consult |
| Social Work Consult |
| Spiritual Care Consult |
| Orders |
| DNR order in place |
| Died in the setting of full support |
| Support withdrawn |
| CPR was ordered/performed in the last hour of life |
| Status |
| On the ventilator in the last week of life |
| On non-invasive positive pressure ventilator in the last week of life |
| Mental status in the last day of life |
| Comorbidities: |
| Renal disease, arthritis, COPD, peptic ulcer, HIV, heart disease/hypertension/peripheral vascular disease, liver disease, stroke, drug/alcohol abuse, history of psychological disease, history of trauma |
| Family member |
| Demographics |
| Age |
| Gender |
| Race |
| Ethnicity |
| Education status |
| Family Relationship |
| Relationship to patient |
| Years that the family member knew the patient |
| Lived with patient |
| Family conference from 1st and last 72 hours of ICU stay |
| Family conference occurred |
| Prognosis discussed |
| Withdrawal of support recommended by physician |
| Family Wishes to withdraw life support discussed |
| Patient’s Wishes discussed |
| Spiritual care needs discussed |
| Family discord with other family member/doctor/nurses |
In order to assess whether respondents were significantly different from non-respondents, we compared demographic characteristics including age, gender, race and ethnicity, insurance, admission diagnosis, co-morbidities and ICU length of stay. We used t-tests for continuous variables that approximated a normal distribution, Mann-Whitney tests for non-normally distributed continuous variables (i.e., ICU length of stay) and chi square tests for categorical variables. All analyses were performed in SPSS 13.0 (2004).
RESULTS
After excluding patients for whom there was no contact information, survey packets were sent to 1074 family members. Among the 442 family members that returned survey packets (41.2% response rate), chart abstraction data were available for 356 patients (Figure 1).
Baseline demographics of family members that returned questionnaires and patients, both with and without family questionnaires, are reported in Tables 1 and 2, respectively. Demographic characteristics for patients for whom questionnaires were not returned, as compared with patients with returned questionnaires, did not vary significantly by age, gender, or insurance. Patients with family member respondents were more likely to be white and had longer ICU stays. A lower proportion of patients with neurologic or psychiatric co-morbidities had family members who responded to the survey.
Table 1.
Demographics of respondents
| Characteristics (n=356) | Total N (%) |
|---|---|
| Age (mean +/−SD) | 58.56 (14.54) |
| Female (%) | 233 (65.4) |
| Race (%)¶ | |
| Caucasian | 305 (85.7) |
| Black | 14 (3.9) |
| Asian | 16 (4.5) |
| Pacific Islander | 3 (0.8) |
| Native American | 16 (4.5) |
| Hispanic | 7 (2.0) |
| Other | 8 (2.2) |
| Respondent relationship (%) | |
| Spouse | 153 (43.0) |
| Adult Child | 122 (34.3) |
| Sibling | 23 (6.5) |
| Parent | 17 (4.8) |
| Other | 32 (9.0) |
| Unknown | 9 (2.5) |
| Education (%) | |
| Less than High School | 11 (3.1) |
| High School | 73 (20.5) |
| Some College or Trade School | 159 (44.7) |
| 4-year college degree | 50 (14.0) |
| Graduate or Professional School | 52 (14.6) |
| Unknown | 11 (3.1) |
Respondents were allowed to enter more than one race/ethnicity.
Table 2.
Demographics for patients for whom family members responded to the survey and those patients for whom family members did not respond
| Patient Characteristics | Patients with a family survey returned (n=356) | Patients without a family survey returned (n=484) | P |
|---|---|---|---|
| Age (mean +/−SD) | 70.1 (15.9) | 68.1 (16.2) | 0.072 |
| # Female (%) | 147 (41.3) | 229 (47.3) | 0.083 |
| # Race (%)¶ | |||
| Caucasian | 278 (78.1) | 288 (59.5) | <0.001 |
| Black | 8 (2.2) | 42 (8.7) | <0.001 |
| Asian | 13 (3.7) | 46 (9.5) | 0.001 |
| Pacific Islander | 0 (0) | 12 (2.5) | <0.01 |
| Native American | 2 (0.6) | 6 (1.2) | 0.195 |
| Hispanic (%) | 4 (1.1) | 4 (0.8) | 0.05 |
| Other | 1 (0.3) | 5 (1.0) | 0.148 |
| # Insurance (%) | 0.514 | ||
| Private/commercial | 33 (9.3) | 38 (7.9) | |
| Government/public | 252 (70.8) | 346 (71.5) | |
| None, unknown | 71 (19.1) | 100 (20.7) | |
| # Admission Diagnosis (%)¶ | 0.02 | ||
| Cardiovascular events, illness | 69 (19.4) | 69 (14.3) | |
| Trauma | 41 (11.5) | 29 (6.0) | |
| Sepsis | 37 (10.4) | 53 (11.0) | |
| Respiratory failure/pulmonary disease | 33 (9.3) | 65 (13.4) | |
| Pneumonia | 27 (7.6) | 30 (6.2) | |
| #Comorbidities (%)¶ | |||
| Cardiovascular | 145 (40.7) | 191 (39.5) | 0.152 |
| Respiratory | 99 (27.8) | 149 (31.2) | 0.293 |
| Oncologic | 94 (26.4) | 110 (22.7) | 0.057 |
| Neurologic | 56 (15.7) | 86 (17.8) | <0.001 |
| Hepatic | 29 (8.1) | 44 (9.1) | 0.137 |
| Renal | 22 (6.2) | 44 (9.2) | 0.109 |
| Psychiatric | 110 (30.9) | 197 (40.7) | 0.001 |
| Length of ICU stay in days (median, IQR) | 2.79 (0.89, 7.06) | 2.38 (0.75, 5.8) | 0.0221 |
More than one response could be entered per patient.
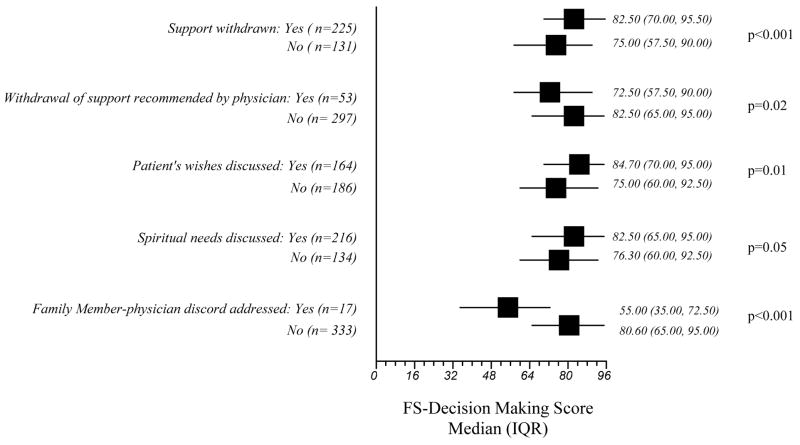
The median (IQR) FS-ICU Decision-making score was 80 (62.5, 92.5). No significant associations with the FS-ICU Decision-making subscale score were found for patient or family member demographic characteristics or patient diagnoses (data not shown). Processes of care that were significantly associated with higher FS-ICU Decision-making subscale scores included medical record documentation of: 1) having life-support withdrawn (p≤0.001); 2) having a physician recommend withdrawal of life-support therapies during a family conference (p=0.02); 3) discussing the patient’s end-of-life wishes during the family conference (p=0.01); and 4) discussing spiritual needs during a family conference (p=0.05). Lower scores were significantly associated with having documentation of family-physician discord during a family conference (p<0.001). (Figure 2)
Figure 2.
Significant associations between the “Satisfaction with Decision-making” (FS-Decision-making) subscale score and processes of care variables.
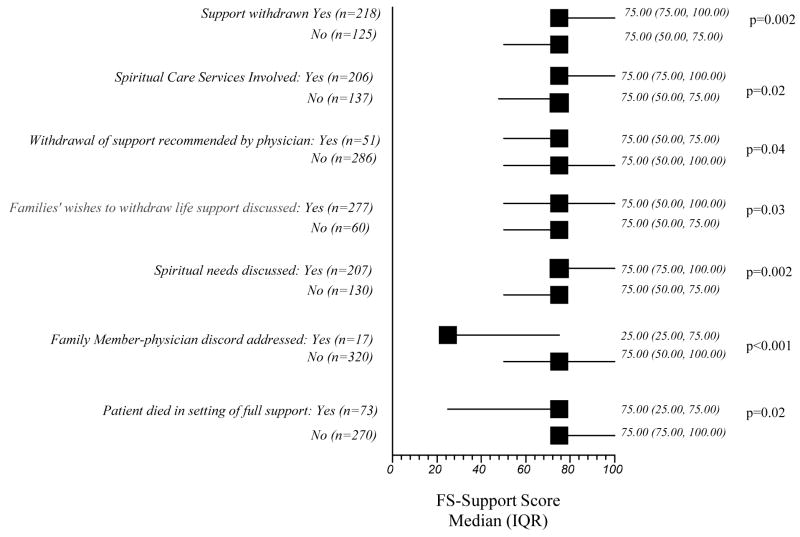
The median (IQR) score for the single item, “Did you feel supported during the decision-making process” (FS-Support), was 75 (50, 100). Significant associations with the single item FS-Support are shown in Figure 3. No patient or family demographic characteristics or patient diagnoses were associated with this item (data not shown). Medical record documentation of the following processes of care was associated with higher scores on this item: 1) having life-support withdrawn (p = 0.002); 2) involvement of spiritual care services (p=0.02) 3) having a physician recommend withdrawal of life-support therapies during a family conference (p=0.04); 3) having family express wishes to withdraw life-support during the family conference (p=0.03) and 4) having spiritual needs discussed at a family conference (p=0.002). A lower FS-Support item score was associated family-physician discord occurring during the family conference and documented in the chart (p<0.001) and with the patient dying in the setting of full support (p=0.02).
Figure 3.
Significant associations between the “Feeling supported during decision-making” (FS-Support) item score, and processes of care variables.
CONCLUSIONS
Our findings suggest that family members with a loved one dying in the ICU report more satisfaction with decision-making and report feeling more supported during the decision-making process in situations where life support is withdrawn, when there is more complete chart documentation of communication during the family conference, and in circumstances where there is chart documentation of an assessment of the spiritual care needs of family members. Of interest, family or patient demographics such as age; race and ethnicity; education level; gender; and number and type of patient co-morbidities were not associated with family member satisfaction in end-of-life decision-making in our study. Other studies have shown an association between satisfaction with care and demographics such as race, ethnicity, and education.17, 18, 19
Family members who made a decision to withdraw life sustaining efforts reported greater feelings of support during end-of-life decision-making and higher satisfaction with end-of-life decision-making. This finding suggests that being involved in this decision may be an important aspect for satisfaction with the decision-making process. These results could be related to the family accepting the inevitable, preparing for their loved one’s death and having some sort of control in this situation. For example, these findings are supported by a recent study showing that most ICU family members do not want to keep their loved one “alive on life-support when there is little hope for a meaningful recovery.”20 Similarly, another study showed that family members of a dying patient needed adequate time to prepare for the death of their loved one.21 Cumulatively, these findings suggest that supporting family members through the decision to withdraw life support when survival is unlikely could be an important target for improving satisfaction with decision-making in the ICU.
However, although supporting family members in their decision to withdraw life support may be an important intervention, it is important to note that not all decisions to withdraw life support are under the control of ICU clinicians. First, family members may not be ready to withdraw life support even if death is inevitable because they have not come to terms with their loved one’s illness and impending death.22 Second, the details and trajectory of the illness or injury may incorporate a high level of uncertainty about the outcome. Uncertainty about the outcome may result in unclear recommendations from the physician about end-of-life decisions23, 24 and could also possibly lead to worse family satisfaction in decision-making and feelings of support. In contrast, if the physician makes recommendations to withdraw life support when the outcome is uncertain, family members could lose trust in the physician or may feel as if they have to make the decision on their own.25 These two situations might potentially be associated with family dissatisfaction with decision-making and be difficult for clinicians to address. Nonetheless, since the majority of deaths are preceded by a decision to withdraw life-sustaining treatment, we believe that our findings suggest that the process of supporting family members through a decision to withdraw life-support when survival is unlikely may be important for improving the care we deliver in the ICU.
Recently, several studies have suggested that reducing the number of days in the ICU prior to death by implementing proactive ethics consultation,26 proactive palliative care consultation,27,28,29 and routine ICU family conferences30 can lead to improved quality of care. Although these studies demonstrated a “reduction in the prolongation of dying” in the ICU, they did not examine family satisfaction with decision-making or family outcomes such as symptoms of depression, anxiety, or PTSD. Our findings suggest that proactive identification of circumstances in which withdrawal of life support is indicated may also be associated with increased family satisfaction with decision-making. Furthermore, a recent randomized trial found that an intervention including a standardized end-of-life family conference focused on supporting family member’s involvement, in addition to administration of a bereavement pamphlet, resulted in a dramatic decrease in symptoms of depression, anxiety and PTSD in family members.10 Our study provides specific suggestions for other components of care for family members that may be useful for interventions to improve satisfaction with decision-making and psychological outcomes. Future studies should examine the effect of improving communication and reducing the prolongation of dying in the ICU on family satisfaction with decision-making.
Our results also suggest that family members felt more support and were more satisfied with the decision-making process when spirituality was addressed during a family conference. A previous report of family members of pediatric patients similarly showed that families were more satisfied and felt more supported with their end-of-life decisions when spiritual care was offered.31 Spirituality may provide a platform for family members to express themselves and feel comforted. Families may be able to use spiritual care to cope with death and the guilt of “letting their loved one go.”32 The association between documentation of discussion of spiritual needs and increased satisfaction with end-of-life decision-making suggests that the involvement of spiritual care at the end-of-life is an important aspect for future investigation.
Our finding that family-physician disagreements are significantly associated with less family satisfaction with decision-making and decreased feelings of support during the process suggests that effective communication and conflict resolution between the physician and family member are important. Although family-physician disagreement was documented in medical records in only 5% of the cases, other studies have suggested that, when specifically asked about conflict, family members report family-physician conflict in 40% of the cases.33 Abbott and colleagues reported that family-physician conflict was most commonly attributed to poor communication (33%) or unprofessional behavior of the staff (15%).33 Therefore, we believe that improving communication strategies and reducing clinician-family discord may also be crucial to improving family member satisfaction with decision-making.
Our study has several limitations. First, although we designed this study as an exploratory analysis, multiple comparisons could have led to spurious associations. Therefore, our results should be considered hypothesis-generating. Second, our study had a relatively low response rate of 41%. Despite this low response rate, it is typical in this type of survey research that contacts families of patients who have died.34, 35, 36, 14 Third, we found that patients of non-responding family members were less likely to be white and had shorter ICU stays, suggesting that there may be some response bias. These results have been demonstrated elsewhere and suggest that further research is needed to improve response rates of minorities.37 However, it is important to note that there is no ethical alternative to allowing family members to opt out of participation. Fourth, the validity of using chart documentation of processes of care as a surrogate marker for quality of care is limited by the comprehensiveness of documentation in the medical record.38 In addition, we did not survey the family members about their perceptions of family conferences and it is unclear if family perceptions would be a better predictor of satisfaction than chart documentation. Also, the physician who documents family conference discussions may have other characteristics or skills which may lead to higher family member satisfaction with decision-making. Although the family conference documentation in the medical record is likely to be incomplete, the fact that we found positive associations between satisfaction with making and chart-assessed processes of care suggests that chart documentation of these aspects of care are potential markers for improved family experience. Finally, this study took place in 10 hospitals in the Seattle-Tacoma area and findings may not generalize to other areas.
In order to develop or refine ICU-based strategies that may increase family member satisfaction with decision-making and may lead to improved quality of end-of-life care in the ICU, we will need to fully understand potential predictors associated with family member satisfaction with end-of-life decision-making. Our findings suggest that family members feel more satisfied and supported in the decision-making process in circumstances when life support is withdrawn. They also report feeling more satisfied and supported in circumstances where there is chart documentation of family conference discussions about patient’s end-of-life wishes, physician recommendations for withdrawing life support, and attention to families’ spiritual needs. A recent randomized trial demonstrated that a focus on communication can improve family outcomes and our findings complement this prior study by providing some specific guidance for the development of future interventions to support families during decision-making regarding end-of-life care.10 Future studies are warranted to further investigate novel interventions to improve communication about withdrawal of life support and to increase involvement of spiritual care services
Abbreviation List
- FS-ICU Care
Family Satisfaction with Care
- FS-ICU Decision-making
Family Satisfaction with Decision-making
- FS-ICU
Family Satisfaction in the Intensive Care Unit
- FS-Support
“Did you feel supported during the decision-making process?” item
- ICU
Intensive Care Unit
- PTSD
Post Traumatic Stress Disorder
- SD
Standard deviation
Footnotes
Disclosure: Dr. Gries, Dr. Wall, Dr. Curtis and Dr. Engelberg do not receive any personal or financial support from organizations with financial interest in the subject matter nor do they have any conflicts of interest.
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD. Robert Wood Johnson Foundation ICU End-Of-Life Peer Group. Use of intensive care at the end-of-life in the United States: an epidemiologic study. Crit Care Med. 2004 Mar;32(3):638–43. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 2.Curtis RJ, Park DR, Krone MR, Pearlman RA. Use of the medical futility rationale in do-not-attempt resuscitation orders. JAMA. 1995 Jan 11;273(2):124–8. [PubMed] [Google Scholar]
- 3.Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life-support from the critically ill. Am J Respir Crit Care Med. 1997 Jan;155(1):15–20. doi: 10.1164/ajrccm.155.1.9001282. [DOI] [PubMed] [Google Scholar]
- 4.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995 Nov 22–29;;274(20):1591–8. [PubMed] [Google Scholar]
- 5.Carlet J, Thijs LG, Antonelli M, Cassell J, Cox P, Hill N, Hinds C, Pimentel JM, Reinhart K, Thompson BT. Challenges in end-of-life care in the ICU. Statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003. Intensive Care Med. 2004 May;30(5):770–84. doi: 10.1007/s00134-004-2241-5. Epub 2004 Apr 20. [DOI] [PubMed] [Google Scholar]
- 6.Malacrida R, Bettelini CM, Degrate A, Martinez M, Badia F, Piazza J, Vizzardi N, Wullschleger R, Ranpin Ch. Reasons for dissatisfaction: a survey of relatives of intensive care unit patients who died. Crit Care Med. 1998 Jul;26(7):1187–93. doi: 10.1097/00003246-199807000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Azoulay E, Pochard F, Chevret S, Adrie C, Annane D, Bleichner G, Bornstain C, Bouffard Y, Cohen Y, Feissel M, Goldgran-Toledano D, Guitton C, Hayon J, Iglesias E, Joly L, Jourdain M, Laplace C, Lebert C, Pingat J, Poisson C, Renault A, Sanchez O, Selcer D, Timsit J, Le Gall J, Schlemmer B. Half the family members of intensive care unit patients do not want to share in decision-making process: A study in 78 French intensive care units. Crit Care Med. 2004 Sep;32(9):1832–8. doi: 10.1097/01.ccm.0000139693.88931.59. [DOI] [PubMed] [Google Scholar]
- 8.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollarert P, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larche J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B. Risk of Post-traumatic Stress Symptoms in Family Members of Intensive Care Unit Patients. Am J Respir Crit Care Med. 2005 May 1;171(9):987–94. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 9.Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Merouani A, Moulront S, Pigne E, Pingat J, Zahar JR, Schlemmer B, Azoulay E French FAMIREA study group. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care. 2005 Mar;20(1):90–6. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Alexandre Lautrette, MD, Michael Darmon, MD, Bruno Megarbane, MD,PhD, Luc Marie Joly, MD, Sylvie Chevret, MD,PhD, Christophe Adrie, MD, PhD, Didier Barnoud, MD, Gerard Bleichner, MD, Cedric Bruel, MD, Gerald Choukroun, MD, Curtis J Randall, MD,MPH, Fabienne Fieux, MD, Richard Galliot, MD, Maite Garrouste-Orgeas, MD, Hugues Georges, MD, Dany Goldgran-Toledano, MD, Merce Jourdain, MD,PhD, Georges Loubert, MD, Jean Reignier, MD, Faycal Saidi, MD, Bertrand Souweine, MD,PhD, Francois Vincent, MD, Nancy Kentish Barnes, PhD, Frederic Pochard, MD,PhD, Benoit Schlemmer, MD, Elie Azoulay., MD,PhD A Communication Strategy and Brochure for Relatives of Patients Dying in the ICU. NEJM. Feb 1;356(5):469–78. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 11.Mularski RA, Curtis JR, Billings JA, Burt R, Byock I, Fuhrman C, Mosenthal AC, Medina J, Ray DE, Rubenfeld GD, Schneiderman LJ, Treece PD, Truog RD, Levy MM. Proposed quality measures for palliative care in the critically ill: a consensus from the Robert Wood Johnson Foundation Critical Care Workgroup. Crit Care Med. 2006 Nov;34(11 Suppl):S404–11. doi: 10.1097/01.CCM.0000242910.00801.53. [DOI] [PubMed] [Google Scholar]
- 12.Nelson JE, Mulkerin CM, Adams LL, Pronovost PJ. Improving comfort and communication in the ICU: a practical new tool for palliative care performance measurement and feedback. Qual Saf Health Care. 2006 Aug;15(4):264–71. doi: 10.1136/qshc.2005.017707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heyland DK, Tranmer J for the KGH ICU Research Working Group. Measuring family satisfaction with care in the intensive care unit: the development of a questionnaire and preliminary results. J Crit Care. 2001 Dec;16(4):142–9. doi: 10.1053/jcrc.2001.30163. [DOI] [PubMed] [Google Scholar]
- 14.Heyland DK, Rocker GM, Dodek PM, Kutsogiannis DJ, Konopad E, Cook DJ, Peters S, Tranmer JE, O’Callaghan CJ. Family satisfaction with care in the intensive care unit: results of a multiple center study. Crit Care Med. 2002 Jul;30(7):1413–8. doi: 10.1097/00003246-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Wall RJ, Engelberg RA, Downey L, Heyland DK, Curtis JR. Refinement, scoring, and validation of the Family Satisfaction in the Intensive Care Unit (FS-ICU) survey. Crit Care Med. 2007 Jan;35(1):271–9. doi: 10.1097/01.CCM.0000251122.15053.50. [DOI] [PubMed] [Google Scholar]
- 16.Dillman DA. Mail and Internet Surveys: The Tailored Design Methods. 2. New York: John Wiley Co; 2000. p. 464. [Google Scholar]
- 17.Welch LC, Teno JM, Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc. 2005 Jul;53(7):1145–53. doi: 10.1111/j.1532-5415.2005.53357.x. [DOI] [PubMed] [Google Scholar]
- 18.Koffman J, Higginson IJ. Accounts of carers’ satisfaction with health care at the end of life: a comparison of first generation black Caribbeans and white patients with advanced disease. Palliat Med. 2001 Jul;15(4):337–45. doi: 10.1191/026921601678320322. [DOI] [PubMed] [Google Scholar]
- 19.Teno JM, Mor V, Ward N, Roy J, Clarridge B, Wennberg JE, Fisher ES. Bereaved family member perceptions of quality of end-of-life care in U.S. regions with high and low usage of intensive care unit care. J Am Geriatr Soc. 2005 Nov;53(11):1905–11. doi: 10.1111/j.1532-5415.2005.53563.x. [DOI] [PubMed] [Google Scholar]
- 20.Heyland DK, Dodek P, Rocker G, Groll D, Gafni A, Pichora D, Shortt S, Tranmer J, Lazar N, Kutsogiannis J, Lam M Canadian Researchers End-of-Life Network(CARENET) What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006 Feb 28;174(5):627–33. doi: 10.1503/cmaj.050626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morita T, Ikenaga M, Adachi I, Narabayashi I, Kizawa Y, Honke Y, Kohara H, Mukaiyama T, Akechi T, Kurihara Y, Uchitomi Y Japan Pain, Rehabilitation, Palliative Medicine, and Psycho-Oncology (J-PRPP) Study Group. Concerns of family members of patients receiving palliative sedation therapy. Support Care Cancer. 2004 Dec;12(12):885–9. doi: 10.1007/s00520-004-0678-2. Epub 2004 Sep 15. [DOI] [PubMed] [Google Scholar]
- 22.West HF, Engelberg RA, Wenrich MD, Curtis JR. Expressions of nonabandonment during the intensive care unit family conference. J PAlliat Med. 2005 Aug;8(4):797–807. doi: 10.1089/jpm.2005.8.797. [DOI] [PubMed] [Google Scholar]
- 23.Christakis NA, Asch DA. Biases in how physicians choose to withdraw life support. Lancet. 1993 Sep 11;342(8872):642–6. doi: 10.1016/0140-6736(93)91759-f. [DOI] [PubMed] [Google Scholar]
- 24.Christakis NA, Iwashyna TJ. Attitude and self-reported practice regarding prognostication in a national sample of internists. Arch Intern Med. 1998 Nov 23;158(21):2389–95. doi: 10.1001/archinte.158.21.2389. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds S, Cooper AB, McKneally M. Withdrawing life-sustaining treatment: ethical considerations. Thorac Surg Clin. 2005 Nov;15(4):469–80. doi: 10.1016/j.thorsurg.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Schneiderman LJ, Gilmer T, Teetzel HD, Dugan DO, Blustein J, Cranford R, Briggs KB, Komatsu GI, Goodman-Crews P, Cohn F, Young EW. Effect of ethics consultations on nonbeneficial life-sustaining treatments in the intensive care setting: a randomized controlled trial. JAMA. 2003 Sep 3;290(9):1166–72. doi: 10.1001/jama.290.9.1166. [DOI] [PubMed] [Google Scholar]
- 27.Campbell ML, Guzman JA. Impact of a proactive approach to improve end-of-life care in a medical ICU. Chest. 2003 Jan;123(1):266–71. doi: 10.1378/chest.123.1.266. [DOI] [PubMed] [Google Scholar]
- 28.Campbell ML, Guzman JA. A proactive approach to improve end-of-life care in a medical intensive care unit for patients with terminal dementia. Crit Care Med. 2004 Sep;32(9):1839–43. doi: 10.1097/01.ccm.0000138560.56577.88. [DOI] [PubMed] [Google Scholar]
- 29.Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med. 2007 Jun;35(6):1530–5. doi: 10.1097/01.CCM.0000266533.06543.0C. [DOI] [PubMed] [Google Scholar]
- 30.Lilly CM, De Meo DL, Sonna LA, Haley KJ, Massaro AF, Wallace RF, Cody S. An intensive communication intervention for the critically ill. Am J Med. 2000 Oct 15;109(6):469–75. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 31.Davies B, Brenner P, Orloff S, Worden W. Addressing Spirituality in Pediatric and Palliative Care. J Palliat Care. 2002 Spring;18(1):59–67. [PubMed] [Google Scholar]
- 32.Koenig H. The Role of Religion and Spirituality at the End-of-life. Gerontologist. 2002 Oct;42(Spec No 3):20–3. doi: 10.1093/geront/42.suppl_3.20. [DOI] [PubMed] [Google Scholar]
- 33.Abbott Katherine H, BA, Sago Joni G, MD, Breen Catherine M, MD, Abernethy Amy P, MD, Tulsky James A., MD Families looking back: One year after discussion of withdrawal or withholding of life-sustaining support. CCM. 2001 January;29(1):197–201. doi: 10.1097/00003246-200101000-00040. [DOI] [PubMed] [Google Scholar]
- 34.Heyland DK, Rocker GM, O’Callaghan CJ, Dodek PM, Cook DJ. Dying in the ICU: perspectives of family members. Chest. 2003 Jul;124(1):392–7. doi: 10.1378/chest.124.1.392. [DOI] [PubMed] [Google Scholar]
- 35.Casaarett DJ, Crowley R, Hirschman KB. Surveys to assess satisfaction with end-of-life care. Does timing matter? J Pain Symptom Management. 2003;25( 2):128–32. doi: 10.1016/s0885-3924(02)00636-x. [DOI] [PubMed] [Google Scholar]
- 36.Merrouche Y. Freyer G. Saltel P, Rebattu P. Quality of final care for terminal cancer patients in a comprehensive cancer centre from the point of view of patients’ families. Support Care Cancer. 1996 May;4( 3):163–8. doi: 10.1007/BF01682335. [DOI] [PubMed] [Google Scholar]
- 37.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family perspectives on end-of-life care at the last place of care. JAMA. 2004 Jan 7;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 38.Kirchhoff KT, Anumandla PR, Foth KT, Lues SN, Gilbertson-White SH. Providing end-of-life care to patients: critical care nurses’ perceived obstacles and supportive behaviors. Am J Crit Care. 2005 Sep;14(5):395–403. [PubMed] [Google Scholar]