Abstract
Background
Improved quality of life (QOL) is a purported benefit of exercise despite few randomized controlled trials (RCTs) and no dose-response trials.
Methods
The effect of 50%, 100%, and 150% of the NIH Consensus Development Panel physical activity dose on QOL was examined in a six-month RCT. Participants were 430 sedentary postmenopausal women (BMI 25.0-43.0 kg/m2) with elevated systolic blood pressure randomized to a non-exercise control group (n=92) or 1 of 3 exercise groups: exercise energy expenditure of 4 (n=147), 8 (n=96), or 12 (n=95) kcal/kg/week. Eight aspects of physical and mental QOL were measured at baseline and month 6 with the SF-36.
Results
Change in all mental and physical aspects of QOL, except body pain, was dose-dependent (trend analyses were significant and exercise dose was a significant predictor of QOL change; p-values<0.05). Change (95% confidence interval) in QOL for the control, 4, 8, and 12 kcal/kg/week groups, respectively, were: physical functioning 2.5 (-0.1-5.1), 4.7 (2.7-6.8), 6.3 (3.7-8.8), 8.2 (5.6-10.7); role physical 2.6 (-2.7-7.9), 8.9 (4.8-13.1), 9.7 (4.5-14.8), 13.1 (7.8-18.3); bodily pain 2.6 (-1.0-6.3), 4.1 (1.3-7.0). 2.4 (-1.1-6.0), 6.8 (3.3-10.4); general health 1.5 (-0.8-3.9), 5.5 (3.6-7.4), 4.7 (2.4-7.1), 7.8 (5.4-10.1); mental health 0.6 (-1.4-2.6), 4.4 (2.8-6.0), 3.6 (1.6-5.5), 4.2 (2.2-6.2); role emotional 4.2 (-0.5-8.9), 8.6 (4.9-12.3), 9.4 (4.8-14.0), 14.6 (9.9-19.2); social functioning -0.4 (-3.3-2.5), 4.5 (2.2-6.8), 5.0 (2.1-7.9), 8.7 (5.9-11.6); vitality 4.6 (1.6-7.6), 9.8 (7.5-12.2), 9.1 (6.1-12.0), 11.7 (8.8-14.7). Controlling for weight change did not attenuate the exercise-QOL association.
Conclusion
Exercise-induced QOL improvements were dose-dependent and independent of weight change.
Keywords: Quality of Life, physical activity, dose-response, exercise training, SF-36
A sedentary lifestyle is a risk factor for many chronic conditions including diabetes, heart disease, stroke, and certain types of cancers.1-6 Regular physical activity and higher levels of cardiorespiratory fitness are associated with lower risk for premature mortality, and exercise training has been demonstrated to improve a number of important risk factors such as cardiorespiratory fitness,7 weight, HDL cholesterol, and fasting insulin.8 Though mood, level of functioning, energy level, and other measures of quality of life (QOL) are purported to be improved by regular exercise, this claim is largely unsubstantiated in populations without significant morbidities. There is strong evidence that regular exercise substantially improves QOL in populations with serious diseases such as cancer9 or chronic obstructive pulmonary disease,10 but the data are not as supportive in populations without disease. Although many, but not all, epidemiology studies have found an association between exercise and QOL, the available data from intervention trials fail to consistently find a strong effect of exercise training on QOL.11, 12 Further, the data from intervention trials are difficult to interpret due to small sample sizes, inadequate control groups, poor exercise compliance, and many studies included a weight loss component making it difficult to separate the benefits of weight loss from increased exercise.
To our knowledge, there are no well-controlled, properly powered randomized controlled trials (RCTs) examining the role of exercise at improving QOL among individuals without significant comorbidities. The Dose-Response to Exercise in postmenopausal Women (DREW) study was designed to examine the health benefits of 50%, 100%, and 150% of the NIH Consensus Panel13 physical activity recommendation in 464 sedentary, overweight or obese, postmenopausal women with elevated blood pressure. The primary outcomes of cardiorespiratory fitness and blood pressure have been reported,7 but data on a number of important secondary outcomes also were included a priori in the study design, and these included a QOL survey.14 Given the relatively large sample size, very high compliance to a tightly controlled exercise intervention, and the high participant retention rate, DREW provides an excellent opportunity to examine the effects of exercise on QOL. Identifying a dose-response relation between exercise and QOL could not only help determine minimum exercise thresholds for promoting QOL, but increase assurance that the exercise-induced benefits are not spurious or the result of chance alone. Thus, the primary aim of this study was to examine changes in QOL across different doses of supervised exercise. We hypothesized that six-months of structured moderate intensity exercise would significantly improve QOL in a dose dependent manner.
METHODS
Study Design
A complete description of the DREW study design and methods has been published elsewhere.7, 14 In brief, the study was a randomized dose-response exercise trial with a non-exercise control group and three exercise groups with incrementally higher doses of energy expenditure. The non-exercise control group was asked to maintain their baseline level of activity during the six-month study period. The research protocol was reviewed and approved annually by The Cooper Institute Institutional Review Board. Written informed consent was obtained from all participants prior to their participation.
Study Participants
Thorough descriptions of the recruiting, screening process, and methods have been published.7, 14 Briefly, the study was limited to postmenopausal women age 45 to 75 years who were sedentary (not exercising more than 20 minutes on 3 or more days a week, and < 8000 steps per day assessed over the course of one week), overweight or obese (BMI 25.0 to 43.0 kg/m2), and who had a systolic blood pressure of 120.0 to 159.9 mm Hg. Exclusion criteria included history of stroke, heart attack, diabetes, or any medical condition that prevented participants from adhering to the protocol or exercising safely. Women with a score ≥10 on the Center for Epidemiological Studies Depression scale (CES-D)15 were excluded based data from our laboratory indicating that these women have a greater probability of attrition and other studies demonstrating that depressed mood is associated with attrition from exercise programs that are part of weight loss programs 16 and cardiac rehabilitation 17. Participants were recruited from the Dallas, Texas area from April 2001 to June 2005.
Outcomes
Change in QOL was measured with the Medical Outcomes Study Short-Form 36 Health Survey (SF-36).18, 19 The SF-36 is a self-administered 36-item questionnaire that measures physical and mental QOL. Physical QOL is measured with the following four scales: physical functioning (PF), role limitations due to physical problems (Role-Physical or RP), bodily pain (BP), and general health perception (GH). Mental QOL also is measured with four scales: role limitations due to emotional problems (Role-Emotional or RE), social functioning (SF), vitality (VT), and mental health (MH). The validity and reliability of the SF-36 have been established and there are standardized norms available for comparative purposes.18, 19 Participants’ raw scores were converted into scale scores ranging from 0 to 100, with higher scores representing better QOL or higher functioning for all scales.
Other Measures
Maximal fitness testing was conducted using a Lode Excalibur Sport cycle ergometer (Groningen, Netherlands) with respiratory gases measured using a Parvomedics True Max 2400 Metabolic Measurement Cart. Weight was measured on an electronic scale (Siemens Medical Solutions, Malvern, PA) and height was measured using a stadiometer. Body mass index (BMI) was calculated as weight in kilograms, divided by height in meters squared. Smoking history, medical history and medication use were assessed by detailed questionnaires. Blood pressure was measured a using a Colin STBP-780 automated blood pressure unit with participants in the recumbent position. Detailed descriptions of the testing procedures are provided elsewhere.7, 14
Exercise Training
Women were assigned to either a non-exercise control group or to groups that expended 4, 8, or 12 kilocalories per kilogram body weight per week (KKW), which corresponds to 50%, 100% and 150%, respectively, of current public health physical activity recommendations.13 Smaller changes in study endpoints were expected in the 4 KKW group; therefore, randomization procedures were created to assign more participants to that group based on the recommendation of the study biostatistician. Exercising women participated in 3 or 4 training sessions each week for 6 months with training intensity at the heart rate associated with 50% of each woman’s peak VO2. All exercise sessions were performed under observation and supervision in an exercise laboratory with standardized prescriptions for exercise dose and strict monitoring of the amount of exercise completed in each session. Participants were weighed each week and their weight was multiplied by their exercise dosage to determine the number of calories to be expended for the week. Women in the exercise groups alternated training sessions on semi-recumbent cycle ergometers and treadmills. Adherence to exercise training over the entire 6-month period was calculated for each individual by dividing the kcal expended during the exercise training by the kcal prescribed for the training period multiplied by 100.
Participant Retention, Adherence, Blinding, and Randomization
A detailed description of procedures for participant retention, adherence, blinding, and random assignment are provided elsewhere.7, 14 To facilitate retention and adherence, participants completed a two-week pre-randomization run-in period and they signed behavioral contracts in which they agreed to adhere to the study protocol. Participants were compensated $150 (total) for completion of baseline ($75) and follow-up ($75) assessments. An additional $350 in incentives was available based on adherence. Assessment personnel were blind to treatment assignment, although blinding was not possible for intervention personnel. Participants were reminded not to discuss their group assignment with the assessment team. Randomization assignment was computer generated and conducted by the statistician.14
Statistical Analysis
Descriptive baseline characteristics of groups were tabulated as means and standard deviations (SD) or as percentages. Differences on baseline SF-36 scale scores among specific subgroups (ethnicity/race, age group, smoking status, marital status, antidepressant use, employment status, and BMI range) were evaluated with analysis of variance (ANOVA), with post-hoc tests when appropriate.
Dose-response effects were evaluated with regression analysis to test for trends in QOL change across groups with adjustment for pre-specified covariates that were identified with the subgroup analysis mentioned above (ethnicity, age group, smoking status, marital status, antidepressant use, employment status, and BMI range). Differences in QOL change across groups were tested by analysis of covariance (ANCOVA) with adjustment. For statistically significant ANCOVAs (p<.05), pair-wise comparisons between exercise groups and the control group were made using the Bonferroni correction for multiple testing. An alpha level of 0.0167 (.05/3 = 0.0167) was utilized because it was our a priori intention to compare only the differences between the exercise groups and the control group; hence, p-values were multiplied by three and reported using the following notations: *p<.05, **p<.01, ***p<.001. Results are presented as adjusted least-squares means with 95% confidence intervals.
Analyses were limited to participants with baseline data. If the outcome value was missing for the participant, we inserted the baseline value for that outcome (i.e., last observation carried forward). Any QOL values > 3 standard deviations from the mean were defined as outliers and eliminated. For exploratory purposes, all QOL outcomes were tested using only available data, without using baseline values carried forward for missing follow-up data. The results from these analyses did not differ substantially from the analyses with baseline values carried forward (the primary analyses); therefore, only the primary analyses are presented. All reported p-values are two-sided. All analyses were performed using SAS version 9.1 (Cary, NC).
RESULTS
A total of 4545 telephone screens were conducted and 4081 potential participants were ineligible based on inclusion and exclusion criteria (Figure 1). After giving informed consent, 464 were randomized, of which 432 had complete QOL data at baseline and 398 of these participants completed the study with 356 usable follow-up QOL surveys. Baseline values were carried forward for missing data/drop-outs, resulting in 430 participants’ data included in the primary analyses. Two participants’ data in the 4 KKW group were eliminated due to being outliers.
Figure 1.
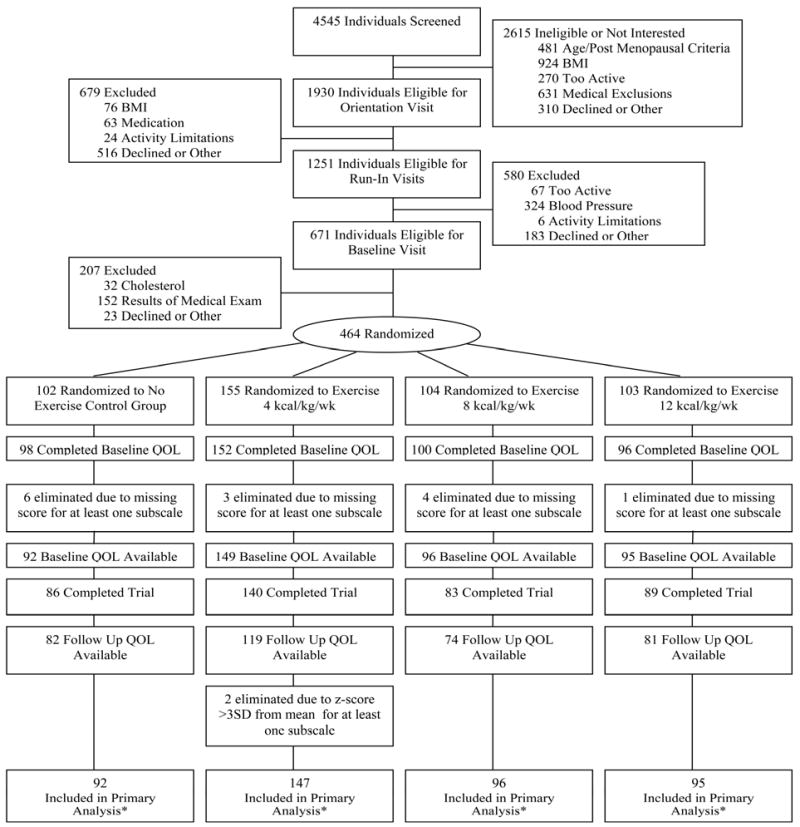
CONSORT diagram describing recruitment and retention of participants. *Baseline values were carried forward if follow-up QOL scores were missing.
As summarized in Table 1, the study population had a mean (SD) age of 57.4 (6.5), a mean BMI of 31.8 (3.8) kg/m2, and 34.9% were non-Caucasian. Almost 30% of the study population reported a history of depression with 18.2% taking anti-depressant medication at baseline. Only 4.4% of the participants were current smokers and 76.5% were employed. Almost half of the participants were using hormone therapy and 15.2% were taking thyroid medication. With the exception of blood pressure, as a group the cardiovascular risk factors were in normal ranges. The mean baseline peak VO2 was very low at 15.4 (2.9) ml/kg/min (see Table 2). Adherence to exercise was 95.4%, 88.1%, and 93.7% across the 4, 8 and 12 KKW groups and each group spent 73.9, 138.3, and 183.6 minutes per week exercising, respectively (Table 2).
Table 1.
Baseline characteristics of the study sample.
| Randomization Groups |
|||||
|---|---|---|---|---|---|
| Characteristics | All participants (n= 430) | Control (n=92) | 4 kcal/kg/wk (n= 147) | 8 kcal/kg/wk (n=96) | 12 kcal/kg/wk (n=95) |
| Demographics | |||||
| Age, y | 57.4 (6.5) | 57.1 (6.0) | 57.9 (6.6) | 57.7 (6.6) | 56.5 (6.7) |
| Education, No. (%) | |||||
| <12 yrs | 12 (2.8) | 3 (3.3) | 4 (2.7) | 3 (3.1) | 2 (2.1) |
| 12-16 yrs | 295 (68.6) | 66 (71.7) | 103 (70.1) | 63 (65.6) | 63 (66.3) |
| >16 yrs | 123 (28.6) | 23 (25.0) | 40 (27.2) | 30 (31.3) | 30 (31.6) |
| Married, No. (%) | 393 (91.4) | 86 (93.5) | 138 (93.9) | 85 (88.5) | 84 (88.4) |
| Ethnicity, No. (%) | |||||
| Caucasian | 280 (65.1) | 62 (67.4) | 90 (61.2) | 60 (62.5) | 68 (71.6) |
| African American | 122 (28.4) | 20 (21.7) | 48 (32.7) | 30 (31.3) | 24 (25.3) |
| Hispanic/other | 28 (6.5) | 10 (10.9) | 9 (6.1) | 6 (6.3) | 3 (3.2) |
| Employed, No. (%) | 329 (76.5) | 78 (73.9) | 109 (74.2) | 75 (78.1) | 77 (81.0) |
| Cigarette smoker, No. (%) | 19 (4.4) | 3 (3.3) | 8 (5.4) | 2 (2.1) | 6 (6.3) |
| History of Depression, No.(%) | 128 (29.8) | 27 (29.4) | 41 (27.9) | 24 (25.0) | 36 (37.9) |
| Anti-depressant medication, No. (%) | 78 (18.2) | 17 (18.5) | 27 (18.4) | 18 (18.8) | 16 (16.8) |
| Thyroid medication, No. (%) | 65 (15.2) | 13 (14.1) | 18 (12.2) | 16 (16.7) | 18 (19.0) |
| Hormone therapy, No. (%) | 196 (47.2) | 48 (52.2) | 62 (42.2) | 42 (43.8) | 44 (46.3) |
| Cardiovascular disease factors | |||||
| LDL-C, mg/dL | 118.4 (26.4) | 118.3 (26.4) | 117.6 (27.2) | 118.2 (25.3) | 120.2 (26.7) |
| HDL-C, mg/dL | 57.4 (14.3) | 56.4 (13.3) | 58.1 (14.5) | 57.0 (15.2) | 57.8 (14.0) |
| Triglycerides, mg/dL | 129.2 (64.0) | 133.9 (67.7) | 130.0 (60.1) | 127.8 (58.2) | 124.9 (71.8) |
| Fasting glucose, mg/dL | 94.7 (9.6) | 95.1 (13.2) | 94.4 (8.6) | 94.6 (8.3) | 95.1 (8.3) |
| Blood pressure, mm Hg | |||||
| Systolic | 139.8 (13.0) | 141.6 (12.2) | 139.4 (13.2) | 140.2 (13.5) | 138.2 (12.9) |
| Diastolic | 81.0 (8.5) | 80.9 (7.8) | 80.9 (9.0) | 80.9 (8.0) | 81.0 (8.9) |
| Anthropometrics | |||||
| Weight, kg | 84.6 (6.5) | 86.4 (12.3) | 83.4 (11.5) | 85.2 (12.8) | 84.3 (11.2) |
| Body mass index (kg/m2) | 31.8 (3.8) | 31.4 (3.6) | 32.1 (4.1) | 31.5 (3.7) | 32.4 (3.9) |
| Quality of Life (SF-36) | |||||
| Physical QOL | |||||
| Physical Functioning | 78.2 (18.6) | 78.9 (16.6) | 78.0 (19.3) | 75.4 (21.0) | 80.8 (16.6) |
| Role Physical | 75.5 (34.1) | 78.8 (31.2) | 72.8 (37.0) | 77.6 (33.5) | 74.5 (32.8) |
| Bodily Pain | 70.7 (19.5) | 69.8 (17.0) | 71.4 (20.3) | 72.0 (20.9) | 69.2 (19.2) |
| General Health | 72.0 (16.2) | 70.9 (16.2) | 72.9 (16.1) | 70.5 (17.3) | 73.3 (16.4) |
| Mental QOL | |||||
| Role Emotional | 78.3 (33.9) | 77.2 (36.3) | 78.2 (34.6) | 84.0 (29.8) | 73.7 (34.0) |
| Social Functioning | 84.8 (19.4) | 83.4 (20.3) | 85.7 (18.4) | 87.6 (16.3) | 81.8 (22.4) |
| Vitality | 54.2 (20.3) | 52.7(19.7) | 54.5 (21.0) | 56.3 (20.1) | 53.1 (20.3) |
| Mental Health | 77.7 (13.8) | 76.6 (14.6) | 78.1 (13.5) | 78.5 (13.1) | 77.3 (14.3) |
Continuous variables presented as means (SD) and dichotomous variables presented as count (percentage). Abbreviations: LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol.
SI conversions: To convert LDL-C and HDL-C to mmol/L multiply by 0.0259. To convert triglycerides to mmol/L multiply by 0.0113. To convert glucose to mmol/L multiply by 0.0555
Table 2.
Mean (SD) exercise-related variables at baseline and change in exercise-related variables after exercise training.
| Randomization Groups |
|||||
|---|---|---|---|---|---|
| All (n= 430) | Control (n=92) | 4 kcal/kg/wk (n= 147) | 8 kcal/kg/wk (n=96) | 12 kcal/kg/wk (n=95) | |
| Exercise-related variables | |||||
| Baseline Peak relative VO2, ml/kg/min | 15.4 (2.9) | 15.5 (3.1) | 15.5 (3.0) | 14.7 (2.5) | 15.7 (3.0) |
| Change in Peak relative VO2, ml/kg/min | 0.78 (1.9) | -0.30 (1.9) | 0.65 (1.9) | 1.33 (1.6) | 1.52 (1.80) |
| 6-mo Adherence (%)a | 92.8 (20.4) | N/A | 95.4 (15.5) | 88.1 (26.4) | 93.7(19.5) |
| Mean Number of Sessions per week | 2.9 | N/A | 2.7 | 2.9 | 3.1 |
| Time spent exercising (min/week) b | 113.8 (61.3) | N/A | 73.9 (15.5) | 138.3 (25.3) | 183.6 (43.3) |
Abbreviations: VO2, volume of oxygen consumed.
Adherence was calculated for each individual by dividing the kilocalories expended during the 6-month exercise training by the kilocalories prescribed for the training period *100.
Data for individuals who completed the intervention. Data are for exercise training period excluding the initial ramping period, which represents 6 months of data for the 4-kcal/kg, 5 months for the 8-kcal/kg, and 4 months for the 12-kcal/kg/wk groups.
The mean baseline scores for QOL scales for the total population and by group are presented in Table 1. As illustrated in Figure 2, the DREW sample at baseline had scores similar to the general United States (U.S.) population20. The mean QOL scores for the DREW sample differed from the national mean by only 0.02 to 0.22 standard deviation units, which are considered differences of small magnitude 21. The mean baseline scores for QOL scales across specific subgroups are presented in Table 3, and, although some comparisons had small sample size, these data demonstrate that we observed many of the expected QOL differences among groups. For example, QOL at baseline was lower on all scales among participants taking antidepressant medication compared to participants not taking such medication. Additionally, employed participants reported better QOL on the PF, RP, and BP scales.
Figure 2.
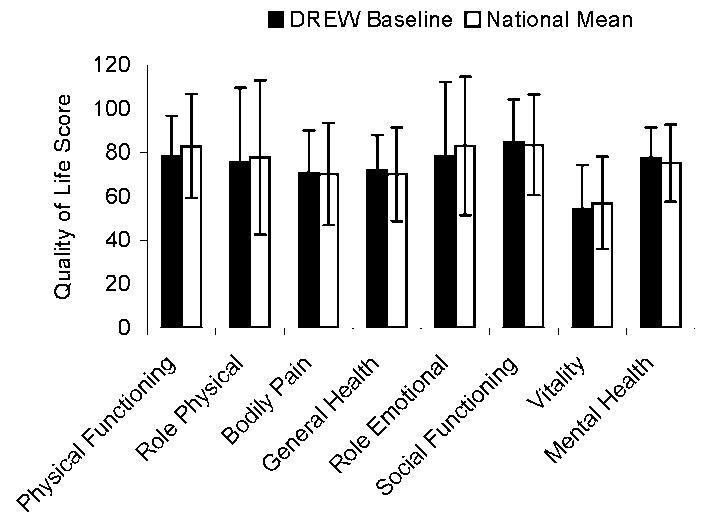
Mean (± SD) baseline SF-36 scores for the DREW sample and the national mean for the United States. The mean QOL scores for the DREW sample differed from the national mean by only 0.02 to 0.22 standard deviation units, which are considered differences of small magnitude 21.
Table 3.
Unadjusted fitted mean (SD) baseline quality of life (SF-36) scores by subgroups.
| Physical Health Measures | Mental Health Measures | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline Category | N | Physical Functioning | Role Physical | Bodily Pain | General Health | Role Emotional | Social Functioning | Vitality | Mental Health |
| Ethnicity/Race | |||||||||
| Caucasian | 280 | 76.4 (18.6) a | 74.7 (33.7) | 70.3 (18.9) | 72.3 (15.6) | 78.0 (33.4) | 84.9 (19.5) | 52.3 (19.7) a | 77.4 (13.4) |
| African American | 122 | 81.5 (18.9) b | 77.5 (35.0) | 71.3 (20.7) | 70.8 (17.3) | 77.9 (35.5) | 83.3 (20.3) | 57.9 (21.0) b | 77.8 (14.9) |
| Hispanic or Other | 28 | 83.1 (15.1) ab | 75.0 (35.4) | 72.0 (20.9) | 74.5 (17.7) | 83.3 (32.1) | 89.7 (12.3) | 57.1 (21.4) ab | 79.6 (12.5) |
| Age Group | |||||||||
| 45-54 years | 175 | 81.6 (17.2) a | 79.3 (31.2) | 71.6 (19.5) | 69.1 (17.1) a | 77.7 (33.0) | 81.8 (20.8) a | 54.3 (21.0) | 76.3 (14.0) |
| 55-64 years | 195 | 77.8 (18.7) a | 74.7 (34.6) | 70.0 (19.6) | 73.2 (15.0) b | 78.1 (34.8) | 87.2 (17.3) b | 54.1 (20.0) | 78.2 (13.5) |
| >65 years | 60 | 70.0 (19.8) b | 67.1 (39.2) | 70.4 (19.3) | 76.7 (16.1) b | 80.6 (33.8) | 85.8 (20.5) ab | 54.1 (19.7) | 79.6 (13.7) |
| Smoking Habits | |||||||||
| Never | 307 | 78.0 (19.3) | 76.0 (33.4) | 70.6 (19.4) ab | 71.7 (16.0) | 77.6 (34.7) | 85.1 (19.6) | 54.1 (20.7) | 77.7 (14.1) |
| Former | 104 | 79.9 (16.1) | 76.4 (35.0) | 73.1 (18.2) a | 73.9 (16.6) | 79.2 (32.6) | 84.2 (19.2) | 55.0 (20.0) | 78.6 (12.5) |
| Current | 19 | 72.9 (19.2) | 63.1 (40.3) | 59.7 (24.9) b | 66.6 (18.0) | 84.2 (28.0) | 82.9 (17.3) | 50.8 (17.3) | 72.0 (14.0) |
| Marital Status | |||||||||
| Not Married | 37 | 81.9 (14.3) | 81.8 (30.4) | 74.6 (18.7) | 68.9 (17.7) | 75.7 (32.1) | 78.4 (22.6) | 48.1 (23.4) | 75.5 (16.2) |
| Married | 393 | 77.9 (18.9) | 74.9 (34.4) | 70.3 (19.6) | 72.3 (16.1) | 78.5 (34.1) | 85.4 (19.0) | 54.8 (20.0) | 77.9 (13.5) |
| Antidepressant Use | |||||||||
| No | 351 | 79.1 (18.0) a | 77.2 (33.0) a | 71.7 (18.9) a | 73.4 (15.9) a | 80.8 (32.2) a | 86.1 (18.9) a | 56.4 (20.0) a | 78.6 (13.7) a |
| Yes | 78 | 74.6 (20.7) b | 67.9 (38.0) b | 66.4 (21.5) b | 65.7 (16.3) b | 67.1 (38.9) b | 78.8 (20.7) b | 44.4 (19.2) b | 73.3 (13.3) b |
| Employed | |||||||||
| No | 101 | 72.8 (21.5) a | 67.8 (40.5) a | 65.2 (20.9) a | 71.9 (16.4) | 76.2 (38.4) | 84.0 (20.8) | 54.1 (21.1) | 76.8 (14.2) |
| Yes | 329 | 79.9 (17.3) b | 77.9 (31.6) b | 72.4 (18.8) b | 72.1 (16.2) | 78.9 (32.4) | 85.0 (18.9) | 54.2 (20.1) | 77.9 (13.6) |
| BMI Range | |||||||||
| Overweight | 151 | 83.1 (16.3) a | 79.0 (31.6) a | 72.3 (19.5) a | 75.1 (15.6) a | 75.1 (35.9) | 86.8 (18.6) | 55.8 (20.6) | 77.3 (15.3) |
| Obese Class I | 177 | 77.8 (18.4) b | 77.1 (33.2) ab | 72.0 (19.2) ab | 71.1 (16.0) ab | 82.3 (30.4) | 84.6 (20.5) | 54.5 (20.8) | 78.3 (12.5) |
| Obese Class II | 102 | 71.9 (20.2) c | 67.6 (38.1) b | 66.1 (19.6) b | 69.1 (16.9) b | 76.1 (36.1) | 82.2 (18.4) | 51.2 (18.9) | 77.0 (13.6) |
Values are expressed as unadjusted fitted means (SD). P values for group differences were assessed by analysis of variance using Bonferroni correction. For pairwise comparisons within subgroups and SF-36 scales, means that differ significantly (p<.05) are noted with different superscripts. For example, employed participants reported significantly better physical functioning, role physical, and bodily pain aspects of QOL at baseline compared to participants who were not working. Employed participants did not differ significantly from participants who were not working on any other SF-36 scales.
Figure 3 summarizes the mean change in SF-36 measures across the control and exercise groups. The positive linear trend across groups was statistically significant for all physical and mental QOL scales (all p-values < 0.0001), with exercise dose being a significant independent predictor of change in all QOL scales (p-values ranged from < 0.0001 to 0.04), except bodily pain (p=0.19). Thus, a dose-response effect of exercise on QOL was noted for all aspects of QOL except bodily pain. The ANCOVAs indicated that for all physical and mental QOL scales, except BP (p=0.32), the 12 KKW group significantly improved QOL compared to the control (p-values ranged from <0.001 to 0.04). Additionally, the 4 KKW group significantly improved GH, VT, and MH compared to control (p-values 0.01 to 0.04). All three exercise groups significantly improved SF compared to control (p-values < 0.0001 to 0.03). The analyses were conducted without the aforementioned covariates and the results were virtually identical.
Figure 3.
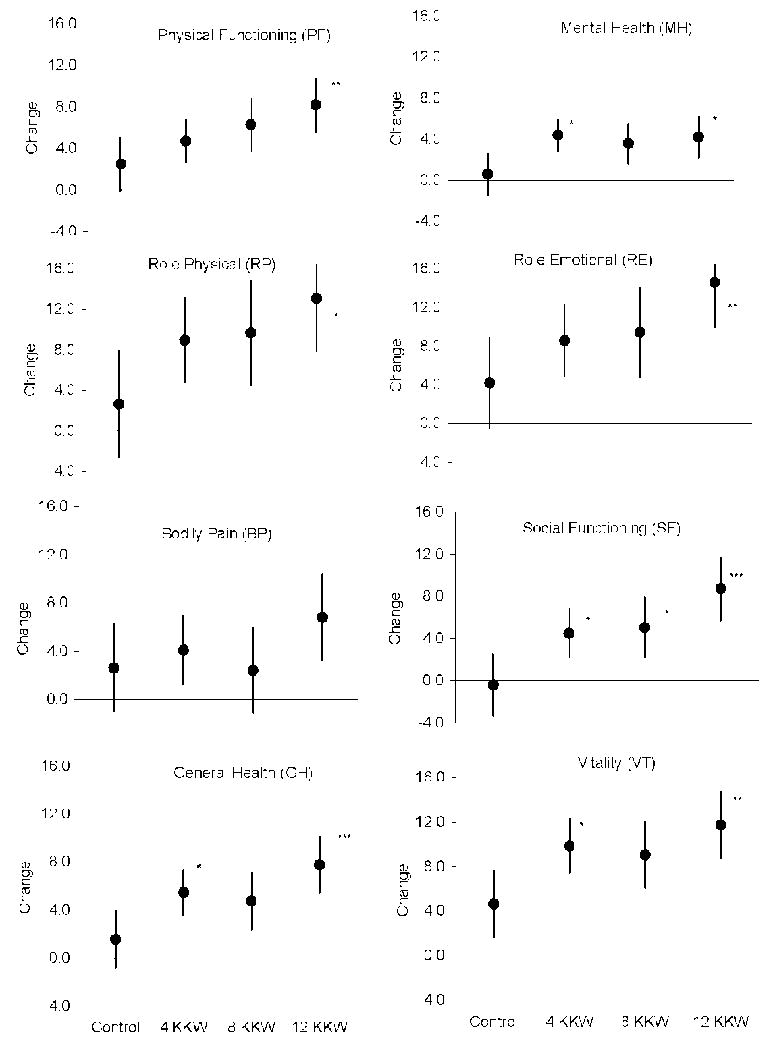
Mean change (Least-squares means ± 95% confidence interval) on SF-36 measures across the control and exercise groups. The dose-response relations between exercise dose and change in QOL were evaluated with regression analysis to test for trends in QOL change across groups. Significant trends were found for all QOL scales (all p-values < 0.0001), with exercise dose being an independent predictor of change in PF, t(1) = 3.19, p=0.002; RP, t(1) = 2.62, p=0.009; GH, t(1) = 3.21, p=0.001; MH, t(1) = 2.03, p=0.044; RE, t(1) = 3.00, p=0.003; SF, t(1) = 4.17, p<0.0001; and VT, t(1) = 2.88, p=0.004; but not BP, t(1) = 1.31, p=0.192. Differences in QOL change across groups were tested by analysis of covariance (ANCOVA) with adjustment for pre-specified covariates (age, antidepressant use, BMI, employment status, ethnicity, marital status, and smoking status at baseline). Significant ANCOVAs (p < .05) were followed by pair-wise comparisons to test if the exercise groups differed significantly from the control group. The alpha level was set a 0.0167 (.05/3=0.0167) and all p-values were multiplied by three; hence, the following notation was used to depict statistical significance: *p < .05, **p < .01, ***p < .001. For significant comparisons, the LS mean differences (95% confidence intervals) between the 12 KKW and control group follow: PF 5.7 (1.2-10.2), RP 10.4 (1.3-19.5), GH 6.2 (2.1-10.4), MH 3.6 (0.2-7.1), RE 10.4 (2.3-18.4), SF 9.1 (4.1-14.2), and VT 7.1 (1.9-12.2). Similarly, significant LS mean differences (95% CI) between the 4 KKW and control group were: GH 3.9 (0.2-7.6), VT 5.2 (0.5-9.9), SF 4.9 (0.3-9.4), and MH 3.8 (0.7-6.9). The 8 KKW significantly improved SF compared to control 5.4 (0.4-10.4).
The mean change in weight across the control, 4 KKW, 8 KKW and 12 KKW groups was -0.94 (4.0), -1.34 (3.5), -1.86 (3.4), and -1.34 (2.9) kg, respectively, with no between group differences. To examine the effect of weight loss on improvement in SF-36 measures, all analyses were repeated with additional adjustment for change in body weight. Weight change was a significant covariate in only two of the eight comparisons and inclusion of this covariate did not have a meaningful effect on any of the mean values, significance, nor trends across exercise groups. To further assure that weight loss was not responsible for the observed results, change in SF-36 scores across the exercise groups was examined with participants sub-grouped into those who lost weight and those who maintained or gained weight. Figure 4 summarizes the change in SF-36 scores across exercise groups for these subgroups. The p-values for the treatment-by-subgroup interactions for the SF-36 scales ranged from 0.07 to 0.95. These non-significant interactions indicate that the pattern of change in each of the SF-36 measures across the exercise groups was similar for those who did and did not lose weight.
Figure 4.
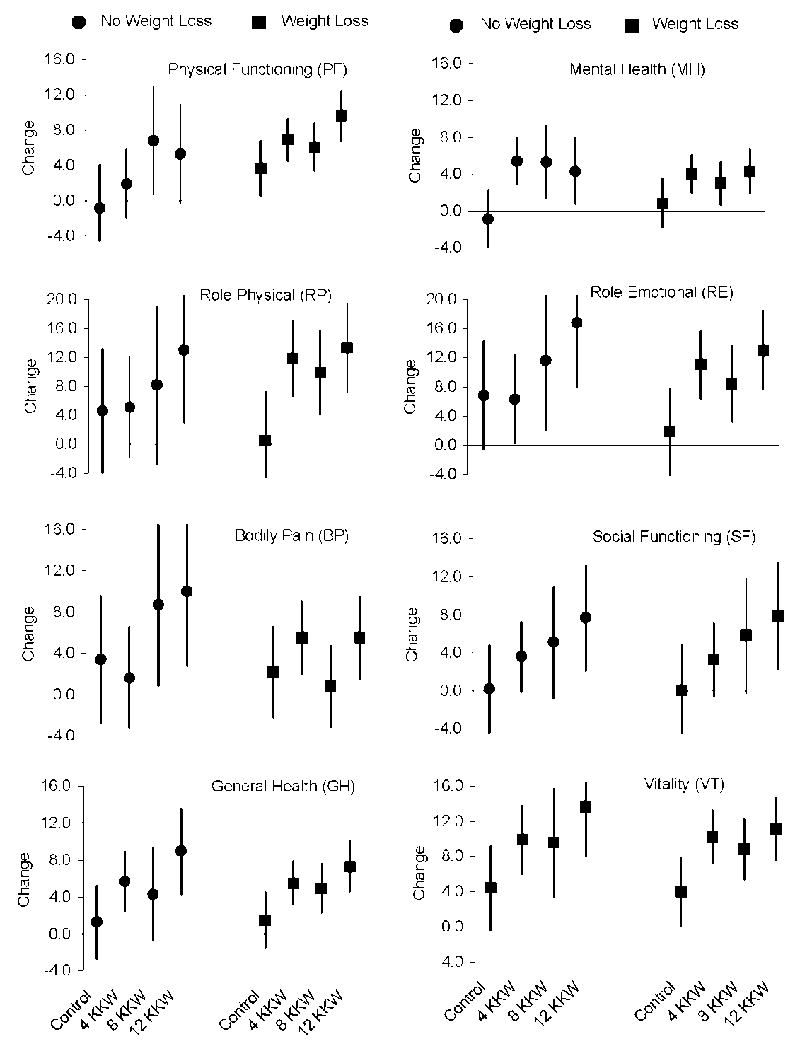
Change in SF-36 scores across the exercise groups was examined for two subgroups of participants: 1) those who lost weight vs. 2) those who maintained or gained weight, using analysis of covariance (ANCOVA) with baseline age, antidepressant use, employment status, ethnicity, marital status, and smoking status as covariates. Mean change (Least-squares means ± 95% confidence interval) on SF-36 scales across the control and exercise groups for participants who did and did not lose weight are depicted. The results from the ANCOVAs follow: PF, F(3, 416) = 0.12, p=0.95; RP, F(3, 416) = 1.00, p=0.39; BP, F(3, 416) = 1.41, p=0.24; GH, F(3, 416) = 0.28, p=0.84; MH (3, 416) = 0.18, p=0.91; RE, F(3, 416) = 2.41, p=0.07; SF, F(3, 416) = 0.87, p=0.46; and VT, F(3, 416) = 0.11, p=0.95. These non-significant interactions indicate that the pattern of change in each of the SF-36 measures across the exercise groups was similar for those who did and did not lose weight.
All analyses were repeated with change in fitness as a covariate, and the conclusions from these analyses were not meaningfully affected. Change in fitness was also correlated with change in QOL and only two of the eight correlation coefficients differed significantly from zero and the size of the coefficients was small (Physical Functioning, r=.11, p=.02; Role Physical, r=.12, p=.02). These findings suggest that changes in fitness are not necessary to improve QOL when individuals increase physical activity.
To explore the effect of antidepressant use on the results, participants were sub-grouped by antidepressant use (yes/no), and change in QOL among exercise groups was tested with an exercise group by sub-group interaction. The interaction term was not significant for all four physical measures of QOL (p-values > .11), but it was significant for the Role Emotional, Social Functioning, and Vitality scales (the p-value for the Mental Health scale approached significance; p=.06). These findings and examination of group means indicated that participants in the non-exercise control condition who took antidepressant medication experienced no increase in QOL during the trial, and for some mental QOL measures they experienced decreased QOL. Conversely, control participants who were not taking antidepressant medication experienced small increases in QOL during the trial.
COMMENT
The primary finding from this randomized controlled exercise trial was a significant, positive dose-response relation between the amount of exercise performed and improvements in measures of both physical and mental QOL. While improved quality life is routinely cited as a benefit of regular exercise, data to support this claim are limited to conflicting epidemiology reports or from studies in persons diagnosed with major chronic diseases such as cancer. Though not observed for all measures, it is of interest that even 4 KKW of exercise (approximately 74 min per week) was associated with a significant improvement in QOL for several of the QOL scales as compared with women in the non-exercise control group. It is noteworthy that the improvements in QOL occurred at a modest training intensity (heart rate at 50% peak VO2) and, as demonstrated by our low dropout rate and excellent adherence in all exercise groups to the six-month caloric expenditure target, the exercise prescriptions were well-tolerated by participants. As a consequence of randomizing more participants to the 4 KKW group, statistical power was sufficient to detect differences in QOL change between the control and 4 KKW group, but not the control and 8 KKW group, despite very similar effect sizes. The significant trend (regression) analyses confirm the dose-response effect, however.
Most cross-sectional studies have observed higher levels of activity to be associated with higher QOL scores,12 particularly for physical aspects of QOL.22 However, in one cross-sectional study, extended bouts of exercise were associated with poor QOL.23 Prospective observational studies suggest that people who report higher levels of exercise also report higher QOL scores, at least among women.24 Nonetheless, as in all observational studies, causation cannot be implied from these findings and it is easy to hypothesize that people with a higher perceived QOL are more like to be physically active or more likely to increase their level of exercise. To our knowledge, we are the first to demonstrate in an RCT that instituting a regular exercise program results in significant improvements in both mental and physical QOL and that these improvements are sensitive to exercise dose; i.e., dose-dependent. The robust effect of exercise on mental QOL in the present study is of interest, since cross-sectional studies find an association primarily between physical aspects of QOL and exercise. It is also of interest that physical activity induced changes in QOL were independent of changes in fitness, suggesting that changes in fitness are not requisite for physical activity induced improvements in QOL.
In an uncontrolled weight loss study, which included exercise, weight loss and/or exercise was associated with improved QOL,25 and a prospective observational study supports the hypothesis that weight loss among overweight women is associated with improved QOL.26 The findings from DREW provide insight into the relative importance of weight loss in exercise-induced changes in QOL, as weight loss in DREW was small and did not differ significantly among the groups. Moreover, exercise induced improvements in QOL were independent of weight loss and the magnitude of change in QOL was similar among those that did and did not lose weight. These results support the hypothesis that exercise in the absence of substantial weight loss can significantly improve both physical and mental QOL.
The public health implications of our findings are significant. We are in the midst of a large shift in the demographics of the U.S. with the proportion of Americans over age 65 growing dramatically over the next few decades. While maximizing longevity is of great importance, maximizing QOL should also be a priority. Our findings suggest that increasing physical activity is an effective tool to improve QOL. Increasing exercise, particularly as individuals age, has many health benefits, e.g., cardiovascular disease (CVD) risk factors are reduced,7,8 and our results indicate that improved QOL can be added to the list of benefits of exercise, and that these improvements are dose-dependent and independent of weight loss, at lease in people similar to this study sample.
Limitations and Strengths
The study has limitations because its sample was limited to sedentary, overweight or obese, postmenopausal women at risk for CVD. Thus, we do not know if the results will apply to other women or men. Nonetheless, the study sample was a group that would likely benefit from exercise training and represents a sizeable proportion, probably a majority, of U.S. women in the age range of 45 to 75 years. Further, although baseline SF-36 scores were similar to the national mean, baseline QOL scores were high, yet we were able to detect significant improvements in QOL. Because participants assigned to incrementally higher doses of exercise spent more time exercising at the center, they had more contact with study personnel and this contact could have influenced QOL. However, in the only other RCTs testing if exercise affects QOL11, the amount of contact between study personnel and participants varied systematically among the study groups, yet no consistent effect of exercise on QOL was found, suggesting that contact with study personnel has little effect on QOL. Lastly, the DREW study was not designed specifically to evaluate the effect of exercise on QOL, however, QOL measures were pre-planned secondary outcomes and this RCT provides compelling evidence of the dose-response relation between exercise and improved QOL.
The study reported herein has many strengths, including being an RCT with three different exercise doses and with all exercise completed in the laboratory. Our study had a large proportion of non-Caucasian participants (primarily African-American), and exercise energy expenditure, heart rate, and steps taken during exercise on the treadmill were extensively monitored. Exercise adherence was excellent, the dropout rate was low, and baseline SF-36 values were similar to the national mean for the U.S. Additionally, expected differences on baseline QOL scores were observed among subgroups, including BMI category and employment status. The exercise doses, including intensity, are easily obtainable and were well tolerated by sedentary women, resulting in confidence that the exercise doses utilized in this study can be achieved by women in the community.
CONCLUSIONS
In this study of previously sedentary, overweight or obese, postmenopausal women, exercise improved both physical and mental QOL in a dose dependent fashion, and the improvements in QOL were independent of weight loss.
Acknowledgments
This work was performed at The Cooper Institute, and the staff is especially commended for their efforts. We thank The Cooper Institute Scientific Advisory Board and the DREW participants.
Footnotes
Preliminary results from this study were presented at the American Heart Association’s Nutrition, Physical Activity and Metabolism Conference, Colorado Springs, CO (March 13, 2008).
References
- 1.Blair SN, Kohl HW, 3rd, Barlow CE, Paffenbarger RS, Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273:1093–1098. [PubMed] [Google Scholar]
- 2.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262:2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 3.Gulati M, Pandey DK, Arnsdorf MF, et al. Exercise capacity and the risk of death in women: The St James Women Take Heart Project. Circulation. 2003;108:1554–1559. doi: 10.1161/01.CIR.0000091080.57509.E9. [DOI] [PubMed] [Google Scholar]
- 4.Mora S, Redberg RF, Cui Y, et al. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: A 20-year follow-up of the lipid research clinics prevalence study. JAMA. 2003;290:1600–1607. doi: 10.1001/jama.290.12.1600. [DOI] [PubMed] [Google Scholar]
- 5.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 6.Stevens J, Evenson KR, Thomas O, Cai J, Thomas R. Associations of fitness and fatness with mortality in Russian and American men in the lipids research clinics study. Int J Obes Relat Metab Disord. 2004;28:1463–1470. doi: 10.1038/sj.ijo.0802770. [DOI] [PubMed] [Google Scholar]
- 7.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: A randomized controlled trial. JAMA. 2007;297:2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 8.Cornelissen VA, Fagard RH. Effects of endurance training on blood pressure, blood pressure-regulating mechanisms, and cardiovascular risk factors. Hypertension. 2005;46:667–675. doi: 10.1161/01.HYP.0000184225.05629.51. [DOI] [PubMed] [Google Scholar]
- 9.Burnham TR, Wilcox A. Effects of exercise on physiological and psychological variables in cancer survivors. Med Sci Sports Exerc. 2002;34:1863–1867. doi: 10.1097/00005768-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Emery CF, Schein RL, Hauck ER, MacIntyre NR. Psychological and cognitive outcomes of a randomized trial of exercise among patients with chronic obstructive pulmonary disease. Health Psychol. 1998;17:232–240. doi: 10.1037//0278-6133.17.3.232. [DOI] [PubMed] [Google Scholar]
- 11.de Vreede PL, van Meeteren NL, Samson MM, Wittink HM, Duursma SA, Verhaar HJ. The effect of functional tasks exercise and resistance exercise on health-related quality of life and physical activity. A randomised controlled trial. Gerontology. 2007;53:12–20. doi: 10.1159/000095387. [DOI] [PubMed] [Google Scholar]
- 12.Spirduso WW, Cronin DL. Exercise dose-response effects on quality of life and independent living in older adults. Med Sci Sports Exerc. 2001;33:S598–608. doi: 10.1097/00005768-200106001-00028. discussion S609-510. [DOI] [PubMed] [Google Scholar]
- 13.Physical activity and cardiovascular health. NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. JAMA. 1996;276:241–246. [PubMed] [Google Scholar]
- 14.Morss GM, Jordan AN, Skinner JS, et al. Dose Response to Exercise in Women aged 45-75 yr (DREW): design and rationale. Med Sci Sports Exerc. 2004;36:336–344. doi: 10.1249/01.MSS.0000113738.06267.E5. [DOI] [PubMed] [Google Scholar]
- 15.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 16.Clark MM, Niaura R, King TK, Pera V. Depression, smoking, activity level, and health status: pretreatment predictors of attrition in obesity treatment. Addict Behav. 1996;21:509–513. doi: 10.1016/0306-4603(95)00081-x. [DOI] [PubMed] [Google Scholar]
- 17.Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000;160:1818–1823. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]
- 18.Ware JE, Jr, Kosinski M, Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: QualityMetric Inc; 1993. p. 2002. [Google Scholar]
- 19.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 20.Ware JE, Jr, Kosinski M. SF-36 Physical & Mental Health Summary Scales: A Manual for Users of Version 1. Second Edition. Lincoln, RI: QualityMetric Incorporated; 2001. [Google Scholar]
- 21.Cohen J. Statistical power analysis for the behavioral sciences. 2. New Jersey: Lawrence Erlbaum; 1988. [Google Scholar]
- 22.Wendel-Vos GC, Schuit AJ, Tijhuis MA, Kromhout D. Leisure time physical activity and health-related quality of life: cross-sectional and longitudinal associations. Qual Life Res. 2004;13:667–677. doi: 10.1023/B:QURE.0000021313.51397.33. [DOI] [PubMed] [Google Scholar]
- 23.Brown DW, Brown DR, Heath GW, et al. Associations between physical activity dose and health-related quality of life. Med Sci Sports Exerc. 2004;36:890–896. doi: 10.1249/01.mss.0000126778.77049.76. [DOI] [PubMed] [Google Scholar]
- 24.Wolin KY, Glynn RJ, Colditz GA, Lee IM, Kawachi I. Long-term physical activity patterns and health-related quality of life in U.S. women. Am J Prev Med. 2007;32:490–499. doi: 10.1016/j.amepre.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fontaine KR, Barofsky I, Andersen RE, et al. Impact of weight loss on health-related quality of life. Qual Life Res. 1999;8:275–277. doi: 10.1023/a:1008835602894. [DOI] [PubMed] [Google Scholar]
- 26.Fine JT, Colditz GA, Coakley EH, et al. A prospective study of weight change and health-related quality of life in women. JAMA. 1999;282:2136–2142. doi: 10.1001/jama.282.22.2136. [DOI] [PubMed] [Google Scholar]


