Abstract
Objectives
The current study evaluated if the effectiveness of brief alcohol intervention in reducing 6- and 12-month risk of injuries in a large level 1 urban trauma center varies based on trauma patients’ ethnicity.
Methods
Eligible White, Hispanic and Black trauma patients ≥ 18 years old were randomized to brief alcohol intervention, or treatment as usual. The intervention, implemented by trained health educators, was a “non-confrontational, patient centered conversation” focused on patients’ drinking pattern with the purpose of encouraging them to change risky drinking. Study outcomes were patient-reported 6 and 12 month incidence of all-type injuries, alcohol-related injuries and serious injuries (i.e. injuries requiring emergency department visit or hospital admission).
Results
A total of 1,493 trauma patients (668 Whites, 537 Hispanics, 288 Blacks) participated in this study. After one year of follow-up, we were not able to detect any important association between brief intervention and the risk of all-type injuries, alcohol-related injuries or, serious injuries among study participants. In addition, the association between brief intervention and the outcomes of interest was not modified by patients’ ethnicity.
Conclusions
Our study, congruent with some recent publications, implies that there are some patient- and provider-related impediments that could restrict the effectiveness of brief intervention programs in trauma centers, regardless of patient ethnicity. Unless those impediments are identified and eliminated, assuming that brief intervention will be an effective strategy for controlling future alcohol-related injuries among trauma patients and should be provided under any circumstances, might not be reasonable.
INTRODUCTION
Numerous strategies have been proposed to control the undesirable consequences of alcohol over-consumption. One of the proposed strategies is motivational interviewing and related practices such as brief intervention 1, 2. Motivational interviewing is a client-based, semi-directive intervention that attempts to increase patients’ awareness of their problematic behaviors, the undesirable consequences of those behaviors, and the potential benefits that patients might experience if they change their behavior. Several studies have presented compelling evidence to support the effectiveness of MI and BI in reducing alcohol intake in primary care clinics, hospitals, and clinical research settings2-7. Injury requiring emergency care or hospital admission is an emotionally salient event that may constitute a unique opportunity to use brief intervention and motivate patients to change their drinking behavior8, 9. However, in comparison to other medical settings, patients in emergency departments and trauma centers are in acute need for medical care in an environment that might not be the best for interaction between a brief intervention provider and patient. As a result of this difficulty in implementing brief intervention in such environments, only a few randomized clinical trials have addressed the issue.
In addition, studies have demonstrated that alcohol consumption pattern varies substantially based on ethnicity 10, 11, which can explain why certain subgroups of the population are at higher risk for the detrimental consequences of alcohol12-19. For example, young Hispanic males are at highest risk for drunk driver death, while alcohol-related intentional injuries are more common in young Black males17. Unfortunately, none of the previous studies have evaluated the potential influence of ethnicity on the association between BI and alcohol-related injuries.
The current randomized clinical trial is the first study that has evaluated the effectiveness of BI in reducing 6- and 12-month risk of all-type injuries, alcohol-related injuries, and serious injuries (i.e., injuries that required emergency department visits or hospital admissions) among White, Hispanic, and Black trauma patients aged 18 years and older hospitalized in a large level 1 urban trauma center.
METHODS
Study Design
This randomized clinical trial was conducted after approval of the relevant institutional review boards (IRBs).
Setting and Selection of Participants
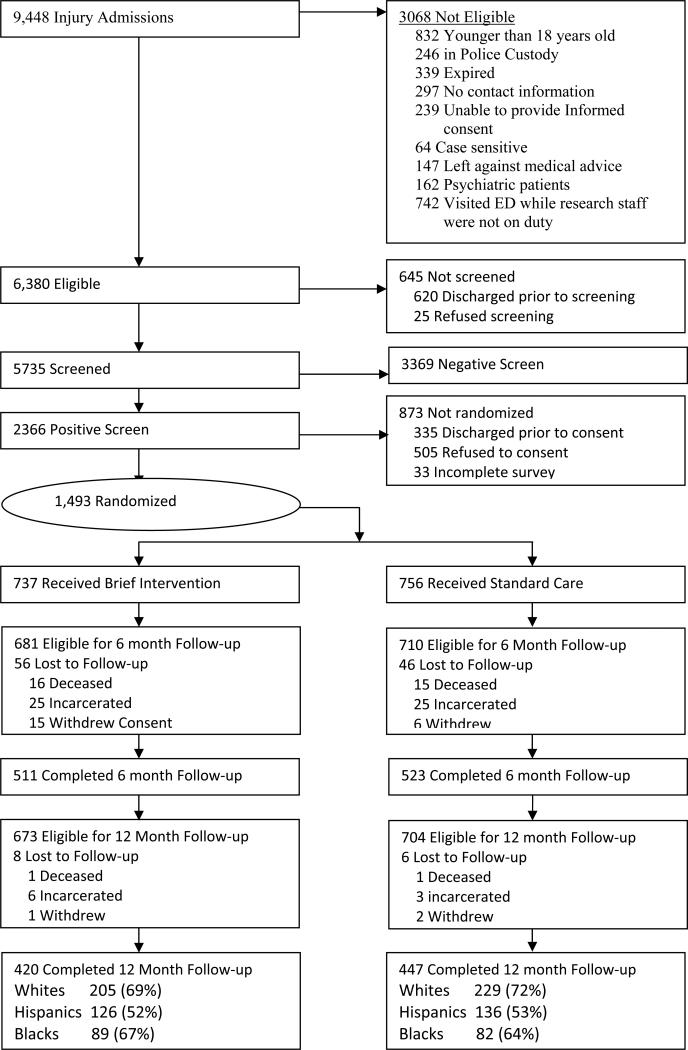
Between May 2003 and May 2005, 9,448 trauma activations were seen in the trauma center. Figure 1 depicts the flow chart of the patients. As presented, only 67% of the patients were eligible to be included in the study. Patients were considered ineligible for the following reasons: 1) they were less than 18 years of age, 2) they spoke neither English nor Spanish, 3) they had no identifiable residence, 4) they were under arrest or in police custody at the time of admission or during their hospital stay, 5) they were judged by the trauma care or research staff to be actively suicidal or psychotic, 6) they were victims of sexual assault, or 7) they had a medical condition that precluded a face-to-face interview. Patients who were intoxicated at the time of their injury or presented with a Glasgow Coma Scale (GCS) < 14 were monitored by research staff for inclusion in the study. Patients with a GCS < 14 that did not resolve prior to discharge were not eligible for screening or enrollment. In order to evaluate if a person was sober enough to be screened, clinicians evaluated the patient's orientation to person, place and time.
Figure 1.
Of the 6,380 eligible patients, 90% were screened by the research team based on the following four criteria: a) positive blood alcohol content at ED, b) self-reported drinking within 6 hours prior to injury, c) positive on one or more items of the CAGE questionnaire that occurred in the past year 20, and d) drinking pattern beyond the National Institute on Alcohol Abuse and Alcoholism standards 21 (≥ 5 drinks per occasion for men and ≥ 4 drinks per occasion for women). Patients who screened positive for a potential alcohol-related injury using the above criteria were eligible for inclusion in the randomized clinical trial.
Sixty-three percent of the screened positive patients provided written informed consent and were compensated for their participation in the study. Patients were interviewed within 24 hours of enrollment by three bilingual trained health educators. Interviews took place between May 2003 and May 2005 with a total of 1,493 trauma patients. Interviews lasted 40 minutes on average and were conducted in the ED (20%) or in the trauma unit (80%) with the use of a structured interview by trained clinicians.
Training and Supervision
Clinicians were master's level students or degreed and were certified in brief intervention following the successful completion of training. This training took 5 full days and was administered by a certified trainer from the Motivational Interviewing Network of Trainers. The first 3 days focused on general principles of motivational interviewing. The other 2 days focused on the application of motivational interviewing principles in the trauma care setting. Training consisted of a mix of didactic lectures, video examples and role play. Clinicians read the first eleven chapters of the Second Edition of Motivational Interviewing:, “Preparing People for Change” by Miller and Rollnick 1, and watched the training videos with the Study Supervisor. Successful completion of the certification process required submission of three audio taped interventions with clients. If a patient refused to be audio taped the following patient was audio taped. Clinicians were required to submit an audio tape at least once per month.
Data collection
Data collected covered demographic characteristics, risk perception, history of risky behaviors, history of alcohol- and non-alcohol-related injuries, alcohol consumption, and physical, social, and legal problems associated with alcohol use, including indicators of alcohol abuse and dependence.
Sampling was limited to patients who identified themselves as Black, White, or Hispanic. Randomization was conducted within each ethnic group. As a result, the final sample of patients randomized to brief intervention or assessment consisted of 668 Whites (45%), 537 Hispanics (36%), and 288 (19%) Blacks. While screening rates did not vary by ethnicity (Whites=91%, Blacks=89% and Hispanics=89%), participation rates did vary by ethnicity with 66% of Whites, 75% of Blacks and 56% of Hispanics agreeing to participate in the study and subsequently being randomized.
Patients were randomized to receive either an assessment-only or an assessment-with-BI using a permuted block (block size 6) design to ensure approximately equal distribution of patients according to their ethnicity. Treatment assignment was generated offsite and was provided to study clinicians in sealed opaque envelopes. Study clinicians were blinded to patient randomization prior to completion of the baseline assessment.
Brief intervention with injured patients has been described elsewhere 22, 23. The intervention, implemented by bilingual trained health educators, was a “non-confrontational, patient centered conversation” focused on patients’ drinking pattern with the purpose of encouraging them to change risky drinking 22, 23. In the assessment-only group, patients completed a questionnaire that generally took 30 to 40 minutes to complete. Following assessments, patients were referred to a drug and alcohol counselor and other appropriate hospital services. This was consistent with general practice for treating patients with alcohol problems at the level 1 trauma center where the clinical trial was conducted. Patients who qualified for the study and consented to participate were interviewed at the beginning of the study, and followed-up at 6 and 12 months via phone interviews. Patients were reimbursed for their participation in the study at the base line ($25) and at 6 and 12 month follow up ($50). Figure 1 demonstrates the proportion of patients who were not interviewed at 6 and at 12 months, and the plausible reasons for withdrawal from the study.
The following information was obtained from the patients at baseline. Socio-demographic characteristics included age, gender, ethnicity, acculturation, education, and employment status. Ethnicity was obtained by three pre-determined survey questions: “Are you Spanish, Hispanic, or Latino/a?” (yes/no); “What is your race?” (White, Black or African American, Asian, Native Hawaiian or other Pacific Islander American Indian or Alaskan native, some other origin, mixed or more than one race). If respondents indicated more than one race, they were then asked about the race group that described them best. For the purpose of this study, race was limited to White or Black and classified as non-Hispanic White, non-Hispanic Black and Hispanic. Alcohol and drug variables included alcohol abuse or dependence, drug use or dependence, frequency of drinking, typical number of standard drinks consumed, maximum amount consumed in last year, frequency of binge drinking, readiness to change, impulsivity, risk perception, engagement in injury-related risk behaviors and history of prior injury. At 6 and 12 months, study participants were asked about their drinking pattern, drug use, type and mechanism of injury, the underlying cause of injury, and role of alcohol in the injury during the past 6 months.
Outcome Measures
Injury outcomes were the dependent variables in all analyses. Patients were asked about their all-type injuries, alcohol-related injuries (i.e., injuries that happened while the patient was under the influence of alcohol), and injuries that required emergency department or hospital visits during the past 6 months. We treated each injury outcome as a binary variable. Therefore, the number of the injuries was not taken into consideration.
Data Analysis
We adopted two approaches in order to evaluate the association between brief intervention and each of the three injury outcomes in multivariable analysis. In approach 1, we compared the risk of injuries at 6 months relative to the risk of injury at the beginning of the study. We repeated the same approach to compare the risk of injuries between month 12 and month 6. This approach allowed us to evaluate if the association between BI and the three injury outcomes was influenced by the time since intervention. Since all-type injury was found to be a common outcome in our study (with more than 10% prevalence 24, 25) we used a log-binomial model to calculate the risk ratio (RR) rather than using logistic regression model and calculating odds ratio 24-26. Studies have shown that the estimated odds ratios based on logistic regression models could result in biased estimates in cohort or clinical trials with common outcomes 24-26.
We tested the significance of interaction between ethnicity and brief intervention on injury outcomes.
We adjusted our estimates for the following potential confounding variables: age, gender, education status (less than high school, some high school education, more than high school), employment status (employed for wages, unemployed), frequency of binge drinking during the past year, drinking volume per week, maximum number of drinks during the past month, injury intention (intentional vs. unintentional), mechanism and severity of injury. The selection of covariates for multivariate analysis was based on a priori hypothesis.
In approach 2, we evaluated the 12-month influence of BI on the risk of all-type, alcohol-related and emergency department-required injuries, using the Generalized Estimating Equation method 27, which allowed us to evaluate the marginal influence 28 of the intervention on the outcomes, taking into consideration the longitudinal design of the study. Similar to log-binomial model, we adjusted our estimates for the same potential confounding variables and added the interaction terms between intervention and ethnicity to evaluate if the associations between brief intervention and the three injury outcomes were influenced by patients’ ethnicity. We used Stata (Stata SE 10.0, StataCorp, College Station, TX) for all analyses.
RESULTS
A total of 1,493 patients were randomized to intervention or control group. Table 1 summarizes the demographic, injury-related, and drinking-related characteristics of the patients in the intervention and control group for Whites, Hispanics and Blacks.
Table 1.
Demographic, injury-related, and drinking characteristics of study participants by intervention group and ethnicity
| White | Hispanic | Black | ||||
|---|---|---|---|---|---|---|
| Control (n=342) | Intervention (n=326) | Control (n=274) | Intervention (n=263) | Control (n=140) | Intervention (n=148) | |
| Age category % | ||||||
| 18−24 |
29 |
24 |
40 |
39 |
13 |
23 |
| 25−34 |
25 |
27 |
36 |
38 |
24 |
19 |
| 35−44 |
25 |
26 |
16 |
17 |
30 |
30 |
| 45+ |
20 |
24 |
08 |
06 |
33 |
28 |
| Male % |
74 |
83 |
88 |
89 |
76 |
85 |
| Marital Status % | ||||||
| Single, never married |
44 |
41 |
49 |
46 |
43 |
51 |
| Married or living with life time partner |
25 |
28 |
32 |
35 |
26 |
22 |
| Separated, divorced, widowed or married not living with spouse |
30 |
31 |
19 |
20 |
31 |
27 |
| Education level % | ||||||
| > High school |
39 |
40 |
12 |
13 |
22 |
20 |
| High school diploma |
36 |
38 |
21 |
24 |
54 |
51 |
| Some high school |
25 |
21 |
67 |
63 |
24 |
28 |
| Employment status % | ||||||
| Employed for wages |
70 |
69 |
78 |
77 |
58 |
50 |
| Not employed for wages |
29 |
31 |
23 |
23 |
42 |
50 |
| Income level ($) % | ||||||
| No income |
7 |
2 |
6 |
5 |
7 |
11 |
| < 10,000 |
12 |
11 |
23 |
25 |
26 |
33 |
| 10,000 to < 30,000 |
31 |
37 |
52 |
52 |
39 |
41 |
| 30,000 to < 50,000 |
24 |
22 |
12 |
12 |
21 |
10 |
| ≥ 50,000 |
25 |
27 |
7 |
7 |
7 |
5 |
| Intentional injuries % |
12 |
12 |
28 |
27 |
33 |
30 |
| Binge drinking/week % | ||||||
| Every/nearly every day |
11 |
8 |
7 |
6 |
13 |
11 |
| 1 to 4 times a week |
28 |
32 |
32 |
41 |
29 |
31 |
| 1 to three times a month |
29 |
24 |
40 |
31 |
23 |
24 |
| Once a year or less |
32 |
37 |
22 |
21 |
35 |
34 |
| Number of drinks per drinking day, mean (median) |
5.7 (5) |
5.6 (5) |
7.2 (6) |
7.8 (6) |
4.5 (3) |
4.3 (3) |
| Number of binge drinking per year, mean (median) |
71 (30) |
68 (30) |
64 (30) |
73 (30) |
81 (30) |
80 (30) |
| Maximum number of drinks per drinking day, mean (median) | 13 (10) | 15 (12) | 14 (12) | 15 (12) | 10 (7) | 9 (7) |
In all, 113 of the 736 intervention were taped and coded using the Motivational Interviewing Skill Code v1.0. The mean of the Global Therapist Rating (M=5.8, SE=.08), Reflection to Question Ratio (M=1.6, SE=.13), percent Open Questions (M=.55, SE=..02), percent Complex Reflections (M=.41, SE=..02) and percent MI Consistent (M=.97, SE=1.3) behaviors counts were determined from the MISC ratings. With the exception of the percent of complex reflections in which some audio tapes were below threshold proficiency (>40%), the means and 95% CI indicated that therapist behaviors were at or above the threshold or expert proficiency levels.
The reported frequency of at least one all-type, alcohol-related or emergency department-required injury at 6- and 12-month follow-up for intervention and control groups is reflected in Table 2. Except during the second 6 months where Blacks receiving brief intervention reported more all-type injuries than the control group, the observed differences between the intervention and the control group were not statistically significant for injury outcomes.
Table 2.
The reported incidence of all-type, alcohol-related, and ED-required injuries by intervention and control groups, for Whites, Hispanics and Blacks1
| Control n (%) | Intervention n (%) | Total n (%) | |
|---|---|---|---|
| Whites | |||
| All-type injury, 1st 6 months | 67 (25) | 57 (23) | 124 (24) |
| All-type alcohol-related injury, 1st 6 months | 17 (6) | 24 (10) | 41 (8) |
| All-type ED required injury, 1st 6 months | 10 (4) | 14 (6) | 24 (5) |
| All-type injury, 2nd 6 months | 50 (16) | 56 (19) | 106 (18) |
| All-type alcohol-related injury, 2nd 6 months | 12 (4) | 16 (6) | 28 (5) |
| All-type ED required injury, 2nd 6 months |
14 (5) |
9 (3) |
23 (4) |
| Hispanics | |||
| All-type injury, 1st 6 months | 25 (15) | 36 (14) | 61 (19) |
| All-type alcohol-related injury, 1st 6 months | 9 (5) | 9 (6) | 18 (6) |
| All-type ED required injury, 1st 6 months | 6 (4) | 9 (6) | 15 (5) |
| All-type injury, 2nd 6 months | 24 (10) | 27 (12) | 51 (11) |
| All-type alcohol-related injury, 2nd 6 months | 8 (3) | 5 (2) | 13 (3) |
| All-type ED required injury, 2nd 6 months |
6 (2) |
11 (5) |
17 (4) |
| Blacks | |||
| All-type injury, 1st 6 months | 18 (20) | 22 (20) | 40 (20) |
| All-type alcohol-related injury, 1st 6 months | 4 (4) | 11 (10) | 15 (8) |
| All-type ED required injury, 1st 6 months | 3 (3) | 5 (5) | 8 (4) |
| All-type injury, 2nd 6 months * | 14 (11) | 28 (22) | 42 (16) |
| All-type alcohol-related injury, 2nd 6 months | 6 (5) | 5 (4) | 11 (4) |
| All-type ED required injury, 2nd 6 months | 4 (3) | 5 (4) | 9 (3) |
Not adjusted for any covariate
Table 3 reflects the results of log-binomial analysis that evaluated the association between the three injury-related outcomes and brief intervention adjusted for age, gender, number of drinking binges drinking in the past month, mean number of drinks per drinking day, maximum number of drinks in the past month, and alcohol dependency status. Other variables did not change the results materially and were excluded from the model: education status (less than high school, some high school education, more than high school), marital status employment status (employed for wages, unemployed), intention of injury (intentional vs. unintentional), mechanism of injury, severity of injury. As presented, we were not able to detect any statistically significant association between the intervention and injury outcomes at 6- and 12-months, if in reality such associations exist. In addition, the associations between BI and injury outcomes were not influenced by ethnicity of the trauma patients.
Table 3.
Log-binomial analysis comparing the risk of having at least one injury, one alcohol-related injury, or one ED-required injury for the intervention group relative to the control group1,2
| White |
Hispanic |
Black |
|
|---|---|---|---|
| Injury Type | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| |
1st 6 months |
||
| All-type | 0.96 (0.70−1.32) | 1.57 (0.99−2.48) | 0.89 (0.49−1.59) |
| Alcohol-related | 1.62 (0.89−2.96) | 1.03 (0.42−2.54) | 2.07 (0.67−6.37) |
| ED required |
1.46 (0.65−3.26) |
1.81 (0.62−5.25) |
1.58 (0.39−6.39) |
| |
2nd 6 months |
||
| All-type | 1.18 (0.83−1.68) | 1.26 (0.74−2.17) | 1.92 (1.05−3.53) |
| Alcohol-related | 1.42 (0.68−2.97) | 0.71 (0.23−2.21) | 1.00 (0.32−3.17) |
| ED required | 0.72 (0.31−1.63) | 2.06 (0.75−5.62) | 1.11 (0.28−4.33) |
Adjusted for age, gender, number of binge drinking during the past month, mean number of drinks per drinking day, maximum number of drinks during the past month and alcohol dependency status
Adjustment for education, marital and employment status, injury intention, mechanism of injury and severity of injury did not change the results materially
The Generalized Estimating Equation analyses resulted in the same conclusions (Table 4). In other words, the intervention was not found to be associated with reduction in the risk of all-type injuries, alcohol-related injuries or emergency department-required injuries for any one of the ethnic groups. The beta coefficients for interactions terms were also not statistically significant.
Table 4.
GEE analysis, comparing the relative risk (RR) of having at least one injury, one alcohol-related injury or one ED-required injury, for the intervention group relative to the corresponding risks for the controls1, 2 during 12 months of follow up
| White |
Hispanic |
Black |
|
|---|---|---|---|
| Injury Type | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| All-type | 1.07 (0.75−1.53) | 1.49 (0.90−2.46) | 1.56 (0.84−2.88) |
| Alcohol-related | 1.53 (0.84−2.78) | 1.25 (0.49−3.16) | 2.08 (0.75−5.74) |
| ED required | 1.05 (0.54−2.07) | 2.16 (0.87−5.35) | 1.17 (0.36−3.84) |
Adjusted for age, gender, number of binge drinking during the past month, mean volume of drinking per week, maximum number of drinks during the past month and alcohol dependency status
Adjustment for education, marital and employment status, type and severity of injury did not change the results materially
In order to evaluate the potential influence of loss to follow up on the results of the study, we conducted two sensitivity analyses, using two scenarios. Under the first one, we assumed that all of the missing individuals experienced at least one injury, one alcohol-related injury or one ED-required injury. Adopting the same analytical approach mentioned above, we were not able to detect any significant association between BI and injury recidivism and ethnicity did not have a modification effect (results not presented). Under the second scenario, we assumed that none of the missing individuals experienced an injury. The results of the study did not change materially and the conclusion remained the same. Since there was no evidence that the intervention was associated with missing status within each ethnic group, we did not expand the sensitivity analyses to scenarios to consider different proportions of patients in intervention and control group experiencing injury events.
LIMITATIONS
First, similar to any other BI clinical trial, the study population was comprised of a group of risky drinkers who volunteered to participate in the study. As a result, the results may be applicable to these type of drinkers only. Second, assessment of the outcome (i.e. injury) was based on self-reported data, while some other studies have used medical and legal records for outcome ascertainment 29. Third, it is possible that a longer follow-up interval might be necessary to demonstrate reduced injuries as a result of the interventions. However, in spite of these limitations, our study was the first that had enough power to detect ethnicity-specific effect of brief alcohol intervention in emergency departments.
DISCUSSION
We did not find a clinically important or statistically significant association between brief intervention and injury recidivism after 12 months of follow-up, regardless of the ethnicity of the patients. Few studies have evaluated the effectiveness of brief intervention in the emergency department setting and those that have produced inconsistent results.
Monti et al. evaluated the efficacy of an emergency department-based brief intervention program among adolescents and demonstrated that the intervention was effective in reducing alcohol-related problems, including injuries 30. In Spirito's study, teenagers 13 to 17 years old were randomized to brief intervention or standard care. These authors found that the intervention significantly reduced alcohol consumption and risk of future injuries31. Gentilello targeted adult trauma patients (≥ 18 years old) in a large urban level 1 trauma center and found that brief intervention compared to standard care was associated with substantial reduction in injury recidivism during three years of follow up29. However, such significant associations between brief intervention and alcohol-related injuries have not been reported in some more recent studies. Longabaugh et al. found that brief intervention with a booster session of brief intervention was effective in preventing future alcohol-related injuries during 12 months of follow up, while brief intervention alone (without the booster intervention) was not32. Daeppen and colleagues screened 5,136 trauma patients in the emergency department of a large university hospital in Switzerland33. Approximately 29% of the patients were considered risky drinkers based on the National Institute on Alcohol Abuse and Alcoholism standards34. After randomizing 1,489 risky drinkers to brief intervention and control treatment, reduction in drinking consumption and the incidence of all-type and alcohol-related injuries was similar after 12 months of follow up33. In the most recently published randomized clinical trial, D'Onofrio randomized 494 hazardous/harmful drinkers to BI which lasted 10−15 minutes or discharge instructions for hazardous and harmful drinking35. After 12 months of follow up, both groups demonstrated substantial decrease in alcohol consumption and ED visits, but the difference between the groups was not statistically significant 35.
In order to summarize the results of the published literature, Havard and colleagues reviewed studies published between January 1996 and July 2007 to evaluate the efficacy of emergency department-based brief intervention programs in decreasing alcohol consumption and injury recidivism among trauma patients36. They found only 11 randomized clinical trials with robust methodology to include in their meta-analysis 36 (D'Onofrio's study was not included in this meta analysis). The type of intervention varied from providing a handout comprised of general advice with personalized feedback to one-on-one counseling lasting more than an hour36. While almost all trials have considered drinking behaviors as one of the main outcomes of interest, only a few studies have focused on injury recidivism 29-33, 37. The authors concluded that “meta-analyses revealed that interventions did not significantly reduce subsequent alcohol consumption, but were associated with approximately half the odds of experiencing an alcohol-related injury”36.
While this conclusion could be valid, to us, the most important part of Havard's study was highlighting some of the methodological challenges that exist in the design and conduction of emergency department-based BI studies. These methodological challenges complicate the comparison of the results from the different studies. Therefore, interpretation of the results of the meta-analyses studies based on very heterogeneous studies could be difficult. Some of those challenges also affected our study.
First and foremost, it is difficult, if not impossible, to have a control group that does not receive any intervention or screening. In our study, both groups took part in an extensive assessment of drinking and other injury related risk behaviors. Assessment took approximately 30 to 40 minutes and was sequenced in a way that may have approximated a brief motivational intervention. Some researchers have suggested that simply asking a control group about their drinking behavior could increase awareness and affect their drinking behavior 5, 38. Daeppen and colleagues evaluated this hypothesis by including a control group that was not assessed at the baseline33. However, they were not able to show any “assessment effect” 33. Second, there is no standardized protocol for implementing brief intervention in the emergency departments. For example, in Blow's study, researchers considered different formats of tailored message booklets and brief advice as interventions39. Third, different studies have used different interventionists for screening and providing the intervention. For example, D'Onofrio used physicians and physician assistants for this purpose. Although there are training courses for alcohol screening and brief intervention counseling, not all these courses are the same and not all studies train interventionists through these courses. As mentioned before, interventionists in our study went through strict training programs. In addition, experienced BI researchers monitored their performance. Therefore, we strongly believe that our lack of ability to find significant intervention effect was not the result of differences in implementation of the study between the intervention and control groups. Fourth, studies select different study populations. For example, D'Onofrio excluded alcohol dependents from their study 35. However, alcohol dependents were included in our study and our results were adjusted for alcohol dependence status.
In conclusion, while studies have presented convincing evidence to support the effectiveness of BI in reducing alcohol intake in primary care clinics 2-7, emergency department-based BI programs have resulted in inconsistent conclusions 36. Our study revealed no association between lack of effectiveness and patient ethnicity. Additional evaluations of factors that may limit the effectiveness of BI in emergency departments are warranted before emergency department-based BI can be advocated as a general approach for reducing alcohol use and alcohol-related injury.
Acknowledgments
This study was supported by grant R01-AA015439 from the National Institute on Alcohol Abuse and Alcoholism and National Institutes of Health and registered at ClinicalTrials.gov. Registration ID #NCT00132262. http://clinicaltrials.gov/
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change. Guilford Press; NY: 2002. [Google Scholar]
- 2.Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH post treatment outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 3.Fleming MF, Barry KL, Manwell LB, et al. Brief physician advice for problem alcohol drinkers - A randomized controlled trial in community-based primary care practices. Jama-Journal of the American Medical Association. 1997 Apr;277(13):1039–1045. [PubMed] [Google Scholar]
- 4.Israel Y, Hollander O, Sanchez-Craig M, et al. Screening for problem drinking and counseling by the primary care physician-nurse team. Alcoholism,Clinical and Experimental Research. 1996;20:1443–1450. doi: 10.1111/j.1530-0277.1996.tb01147.x. [DOI] [PubMed] [Google Scholar]
- 5.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 6.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. Journal of General Internal Medicine. 1997 May;12(5):274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chick J, Ritson B, Connuaghton J, et al. Advice versus extended treatment for alcoholism: A controlled study. British Journal of Addiction. 1988;83:159–170. doi: 10.1111/j.1360-0443.1988.tb03977.x. [DOI] [PubMed] [Google Scholar]
- 8.Gentilello LM, Dugan P, Drummond D, et al. Major injury as a unique opportunity to initiate treatment in the alcoholic. American Journal of Surgery. 1988;156:558–561. doi: 10.1016/s0002-9610(88)80553-1. [DOI] [PubMed] [Google Scholar]
- 9.Soderstrom CA, Cowley RA. A national alcohol and trauma center survey: Missed opportunities, failures of responsibility. Archives of Surgery. 1987;122:1067–1071. doi: 10.1001/archsurg.1987.01400210105016. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert MJ, Cervantes RC. Patterns and practices of alcohol-use among Mexican-Americans - A comprehensive review. Hispanic Journal of Behavioral Sciences. 1986 Mar;8(1):1–60. [Google Scholar]
- 11.Markides K, Ray LA, Stroup-Benham CA, et al. Acculturation and alcohol consumption in the Mexican American population of the southwestern United States: Findings from HHANES 1982−1984. American Journal of Public Health. 1990;80(Supplement):42–46. doi: 10.2105/ajph.80.suppl.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borges G, Cherpitel C, Mittleman M. Risk of injury after alcohol consumption: a case-crossover study in the emergency department. Social Science and Medicine. 2004 Mar;58(6):1191–1200. doi: 10.1016/s0277-9536(03)00290-9. [DOI] [PubMed] [Google Scholar]
- 13.Caetano R, M C. Driving under the influence (DUI) among U.S. ethnic groups. Accident: analysis and prevention. 2005 Mar;37(2):217–224. doi: 10.1016/j.aap.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Kon AA, Pretzlaff RK, Marcin JP. The association of race and ethnicity with rates of drug and alcohol testing among US trauma patients. Health Policy. 2004;69(2):159. doi: 10.1016/j.healthpol.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Caetano R, Ramisetty-Mikler S, Floyd LR, et al. The epidemiology of drinking among women of child-bearing age. Alcohol Clin Exp Res. 2006 Jun;30(6):1023–1030. doi: 10.1111/j.1530-0277.2006.00116.x. [DOI] [PubMed] [Google Scholar]
- 16.Caetano R. Prevalence, incidence and stability of drinking problems among whites, blacks and Hispanics: 1984−1992. J Stud Alcohol. 1997 Nov;58(6):565–572. doi: 10.15288/jsa.1997.58.565. [DOI] [PubMed] [Google Scholar]
- 17.Caetano R. Alcohol-related health disparities and treatment-related epidemiological findings among whites, blacks, and Hispanics in the United States. Alcoholism, clinical and experimental research. 2003 Aug;27(8):1337–1339. doi: 10.1097/01.ALC.0000080342.05229.86. [DOI] [PubMed] [Google Scholar]
- 18.Caetano R, Babor TF. Diagnosis of alcohol dependence in epidemiological surveys: an epidemic of youthful alcohol dependence or a case of measurement error? Addiction. 2006 Sep;101(Suppl 1):111–114. doi: 10.1111/j.1360-0443.2006.01599.x. [DOI] [PubMed] [Google Scholar]
- 19.Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: an update using 1996 data. Journal of Studies of Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]
- 20.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA : the journal of the American Medical Association. 1984 Oct 12;252(14):1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 21.NIAAA . The physician's guide to helping patients with alcohol problems (NIH Publication No.953769) National Institute on Alcohol Abuse and Alcoholism, National Institute of Health; Washington, DC: 1995. [Google Scholar]
- 22.Field C, Hungerford DW, Dunn C. Brief motivational interventions: an introduction. J Trauma. 2005;59:S21–26. doi: 10.1097/01.ta.0000179899.37332.8a. [DOI] [PubMed] [Google Scholar]
- 23.Dunn C, Hungerford DW, Field C, et al. The stages of change: when are trauma patients truly ready to change? J Trauma. 2005;59:S27–32. doi: 10.1097/01.ta.0000185298.24593.56. [DOI] [PubMed] [Google Scholar]
- 24.McNutt LA, Wu C, Xue X, et al. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003 May 15;157(10):940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 25.Robbins AS, Chao SY, Fonseca VP. What's the relative risk? A method to directly estimate risk ratios in cohort studies of common outcomes. Ann Epidemiol. 2002 Oct;12(7):452–454. doi: 10.1016/s1047-2797(01)00278-2. [DOI] [PubMed] [Google Scholar]
- 26.Greenland S. Interpretation and choice of effect measures in epidemiologic analyses. Am J Epidemiol. 1987;125:761–768. doi: 10.1093/oxfordjournals.aje.a114593. [DOI] [PubMed] [Google Scholar]
- 27.Liang KY, Zeger SL. Longitudinal data analysis using general linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 28.Localio AR, Berlin JA, Ten Have TR, et al. Adjustments for Center in Multicenter Studies: An Overview. Ann Intern Med. 2001;135:112–123. doi: 10.7326/0003-4819-135-2-200107170-00012. [DOI] [PubMed] [Google Scholar]
- 29.Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Annals of Surgery. 1999 Oct;230(4):473–480. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999 Dec;67(6):989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 31.Spirito A, Monti PM, Barnett NP, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. Journal of Pediatrics. 2004 Sep;145(3):396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 32.Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62(6):806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- 33.Daeppen JB, Gaume J, Bady P, et al. Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: a randomized controlled clinical trial. Addiction. 2007 Aug;102(8):1224–1233. doi: 10.1111/j.1360-0443.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 34.National Institute on Alcohol Abuse and Alcoholism . Helping Patients Who Drink Too Much. A CLINICIAN'S GUIDE. Updated 2005 Edition. U.S. DEPARTMENT OF HEALTH & HUMAN SERVICES, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- 35.D'Onofrio G, Pantalon MV, Degutis LC, et al. Brief Intervention for Hazardous and Harmful Drinkers in the Emergency Department. Ann Emerg Med. 2008 doi: 10.1016/j.annemergmed.2007.11.028. Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103(3):368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- 37.Rodriguez-Martos A, Castellano Y, Salmeron JM, et al. Simple advice for injured hazardous drinkers: an implementation study. Alcohol & Alcoholism. 2007 Sep-Oct;42(5):430–435. doi: 10.1093/alcalc/agm052. [DOI] [PubMed] [Google Scholar]
- 38.Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH post treatment outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 39.Blow FC, Barry KL, Walton MA, et al. The efficacy of two brief intervention strategies among injured, at-risk drinkers in the emergency department: impact of tailored messaging and brief advice. Journal of Studies on Alcohol. 2006 Jul;67(4):568–578. doi: 10.15288/jsa.2006.67.568. [DOI] [PubMed] [Google Scholar]