Abstract
Objectives
There is a dearth of information on the experience of pain in persons living with HIV and co-occurring psychological and substance use problems. This study examined the prevalence and correlates of pain in 162 HIV+ persons diagnosed with mood and/or anxiety disorders as well as substance use disorders.
Methods
Bodily pain scores in the current sample were compared to pain scores in the United States (US) general population and HIV+ persons who screened negative for psychological and substance use problems. Bivariate analyses were used to identify significant correlates of pain scores in the current sample which were then subjected to multiple regression analysis.
Results
Pain scores in the current sample were significantly lower (indicating more pain) than the general population and HIV+ persons who screened negative for psychological and substance use problems. Multivariate analysis indicated that the presence of mood disorder, older age and lower CD4 cell counts (below 200) were associated with increased pain. Presence of mood disorder accounted for the largest amount of unique variance in pain scores.
Discussion
HIV+ persons with diagnosed mood/anxiety and substance use disorders reported substantially higher levels of pain than the general population and HIV+ persons without these comorbid conditions. The presence of mood disorder emerged as an important marker for pain in the current sample. Given that individuals living with HIV and comorbid psychological and substance use disorders are at increased risk for pain, concerted efforts should be directed at identifying and treating pain in this population.
Keywords: Pain, human immunodeficiency virus, anxiety, depression, drug abuse
Introduction
Pain is recognized as a source of considerable distress and disability among persons living with HIV (1–7). Pain in the context of HIV may derive from multiple sources (3), including the effects of HIV disease on the nervous system, immune suppression, iatrogenic treatment effects (e.g., antiretroviral medications), various disorders associated with HIV (8), as well as factors unrelated to HIV (e.g., pre-existing conditions) or its treatment (8, 9). In convenience samples of HIV infected persons, the prevalence of pain has been estimated at between 25% to 80% (1, 4, 10, 11). In the HIV Cost and Services Utilization Study (HCSUS), the first nationally representative sample of HIV+ persons in the United States (US), our prior research indicated that 67% reported experiencing pain during the previous month (12).
Recent models have conceptualized pain as a multidimensional construct incorporating biological, psychological and social aspects (13). Consistent with this biopsychosocial model, investigators have begun to focus on the impact of co-existing psychological and substance use disorders on the experience of pain among HIV infected persons (2, 3). Mood and anxiety disorders are the most common Axis I psychological disorders among HIV+ persons. In the HCSUS, approximately 48% screened positive for a mood or anxiety disorder, and roughly 12% screened positive for substance dependence (14). In HIV, the presence of pain has been strongly linked with mood and anxiety disorders. One study found that HIV+ individuals with posttraumatic stress disorder (PTSD) reported greater pain intensity and pain-related interference than those without PTSD (15). In the HCSUS, we previously found that pain demonstrated strong concurrent associations with panic disorder, major depression and PTSD (16). Longitudinal analyses however, revealed that increasing pain over a time was associated with the presence of panic disorder, but not with major depression or PTSD.
The literature on the relationship between substance abuse and pain in HIV is more mixed. Although research in convenience samples indicates that HIV+ individuals who are injection drug users (IDUs) report increased pain compared to non-IDUs (7, 9, 17, 18), at least two studies did not find differences in pain report between these groups (1, 19). In the HCSUS, our earlier work indicated that screening positive for drug dependence in relation to a broad range of substances (not just IDU), was associated with increased pain (6). In addition, drug dependence was predictive of increased pain over time, even after controlling for prior pain. Notably, in the studies which found no differences in pain report among IDUs vs. non-IDUs approximately 70% met criteria for AIDS. In contrast, in the HCSUS, only about 36% met AIDS criteria. Thus, it is possible that at more advanced stages of HIV disease, differences in pain report based on substance abuse history may be less prominent.
Despite the high prevalence of comorbid psychological and substance use disorders in HIV, there a paucity of research on the experience of pain in HIV+ individuals with both comorbid substance use disorders and psychological disorders. Such “triply diagnosed” HIV+ persons are reported to have poorer health outcomes, lower medication adherence rates, and lower treatment and retention rates compared to the general HIV population (20, 21). To the authors’ knowledge no prior work has focused on identifying the correlates of pain among triply diagnosed HIV+ persons. Thus, the purpose of this study was to determine the prevalence of pain in a sample of triply diagnosed HIV+ persons and to identify key sociodemographic and clinical characteristics associated with pain in these individuals. In contrast to previous work that relied on diagnostic screeners, the current sample was determined to meet full criteria for both psychological and substance use disorders using the gold standard for clinical diagnostic interviews (i.e. The Structured Clinical Interview for DSM-IV (SCID) (22, 23)(described fully below).
Materials and Methods
Participants
This study analyzed data from a cohort of 162 HIV infected patients with current DSM-IV psychological and substance use disorders. These data were derived from a larger study (described below). The 162 participants were recruited from May 2000- July 2003, at the CORE center, Chicago; a public urban ambulatory care facility serving mostly socio-economically disadvantaged HIV infected patients. The current sample was originally recruited as part of the larger HIV/AIDS Treatment Adherence, Health Outcomes and Cost Study, a multi-year cooperative agreement involving 8 study sites and jointly funded by agencies within the Substance Abuse and Mental Health Services Administration (SAMHSA), the Health Resources and Services Administration (HRSA) and National Institutes of Health (NIH). This multi-site study examined the effectiveness of integrated care for HIV infected persons with co-occurring psychological and substance abuse disorders (24). All participants included in this study signed informed consent forms, and the study was approved by the hospital’s institutional review board. Demographic information for the 162 patients in the current study is displayed in Table 1.
Table 1.
Demographic and clinical characteristics of 162 HIV infected persons with comorbid psychological and substance use disorders
| Total (N = 162) |
|
|---|---|
| Age, mean years (SD) (Range: 24 – 60 years) | 39.7 (7.3) |
| Sexa | |
| Male | 107 (66.1%) |
| Female | 55 (33.9%) |
| Race | |
| African-American | 133 (82.1%) |
| White | 21 (13.0%) |
| Asian | 1 (0.6%) |
| Native American/Alaska native | 1(0.6%) |
| Other | 6 (3.7%) |
| Educational level, mean yrs (SD) | 10.5 (1.5) |
| Insurance | |
| Uninsured | 88 (54.7%) |
| Private | 5 (3.1%) |
| Medicaid | 50 (30.9%) |
| Medicare | 19 (11.8%) |
| VA/CHAMPUS | 3 (1.9%) |
| HIV transmission factorb | |
| MSM | 48 (29.6%) |
| Heterosexual contact | 106 (65.4%) |
| IDU | 58 (35.8%) |
| Alcohol & Substance Use Disorders | |
| Alcohol Abuse/Dependence | 49 (30.2%) |
| Substance Abuse/Dependence (not alcohol) | 16 (9.9%) |
| Both Alcohol and Substance Abuse/Dependence | 97 (59.9%) |
| Psychological Disorders | |
| Mood Disorderc | 71 (43.8%) |
| Anxiety Disorderd | 8 (4.9%) |
| Both Anxiety and Mood Disorders | 21 (13.0%) |
Note: Sex: Female group includes one male-to-female transgendered individual
Frequencies sum to more than 162 due to patients with multiple HIV transmission risk factors
Includes major depression, bipolar disorder and dysthymia
Includes generalized anxiety disorder, post-traumatic stress disorder and panic disorder/agoraphobia; VA = Veterans’ Affairs, Department of; CHAMPUS = Civilian Health and Medical Program of the Uniformed Services; MSM = Men who have sex with men; IDU = Intravenous drug use.
Procedure
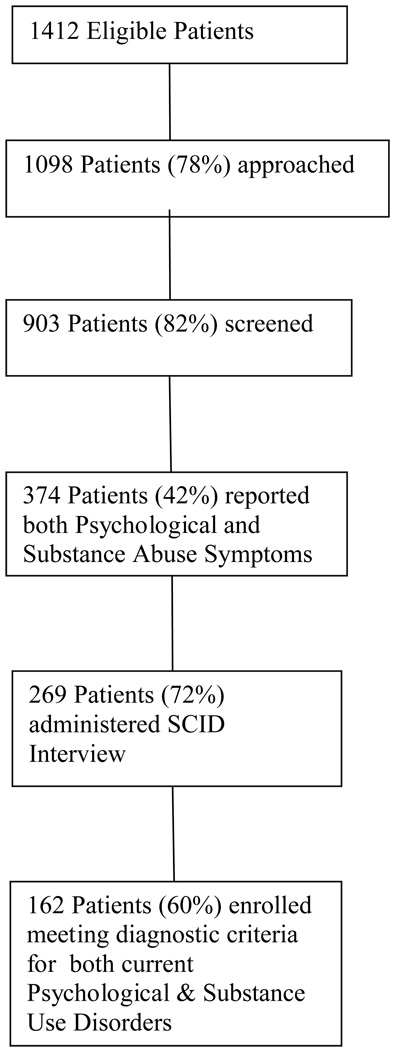
A flow chart illustrating participant enrollment for the current sample is shown in Figure 1. Briefly, from May 2000 to August 2002, 1176 adult HIV patients were screened using items from standardized instruments [Composite International Diagnostic Interview (CIDI) (25), Structured Clinical Interview for DSM-IV (SCID)(22), Alcohol Use Disorders Identification Test (AUDIT) (26) and Clinical Diagnostic Questionnaire (CDQ)(27)]. Only those who screened positive, i.e., reported symptoms associated with psychological and substance use disorders were eligible for diagnostic interview using selected diagnostic modules of the SCID. Trained interviewers administered the initial screener, conducted the diagnostic interview and collected additional patient self-report data. The full baseline assessment was conducted over two sessions. The SCID interview was given in session 1 to determine diagnostic study eligibility. Patients who met diagnostic eligibility were then scheduled for session 2. The session 2 assessment included sociodemographics, physical and mental health functioning, as well as substance use severity. Only those measures relevant to the current study are discussed below. Each session averaged 1.5 hours in length. Patients were paid $20 for these assessments.
Figure 1.
Study enrollment flow chart
Measures
1. Addiction Severity Index (ASI-Lite) (28)
assessed alcohol and drug use severity. The ASI is a structured interview instrument with good psychometric properties that measures alcohol and illicit drug related behaviors and quantifies the status of use over time (29). Discriminant and concurrent validity of the ASI has been established in previous samples (30–32). The ASI provides summary scores for each domain. For the current study, summary scores were used for the following two domains: alcohol use, illicit drug use. For each domain the ASI provides a severity rating based on subjective and objective data (scores range from 0–9; larger values indicate greater severity), and a mathematically derived composite score of current behavior (i.e., past 30 days). Information on the frequency of drug use (all drugs) and alcohol use in the past 30 days collected in the ASI was used to derive the average number of days in the past month that patients used drugs and alcohol.
2. Structured Clinical Interview for DSM-IV
(SCID) (22, 23) was used to diagnose psychological and substance use disorders. The SCID is viewed as the gold standard for clinical diagnosis in adults (22, 23). Test-retest reliabilities of reliability coefficients for schizophrenia, mood, alcohol, and substance abuse disorder diagnoses exceed .60 (23, 33). Based on the SCID, participants were classified into two categories: mood disorders (major depression, dysthymia, bipolar disorder) and anxiety disorders (generalized anxiety disorder or GAD, panic disorder/agoraphobia, PTSD). Substance use diagnostic categories included alcohol abuse/dependence and non-alcohol substance abuse/dependence.
3. Short-Form 36 (SF-36) (34–36) Bodily Pain (BP) scale
was used to assess pain. The SF-36 is an extensively used and psychometrically sound survey instrument. Normative data for the SF-36 in the general US population are available (37). The BP scale of the SF-36 consists of two items: 1) How much bodily pain have you had during the past four weeks? Responses range from “none” = 1 to “very severe” = 6; 2) “During the past four weeks, how much did pain interfere with your normal work (including work outside the house and housework)?” Responses range from “Not at all” = 1, to “extremely” = 5. Raw scores for the BP items are linearly transformed to a 0 to 100 scale. Lower scores on the BP scale indicate greater pain.
4. CD4+ (T − helper lymphocyte) cell counts
were abstracted from the patients’ medical charts. Absolute values of CD4 cell counts were available for all but six participants. For three of these participants, self-reported CD4 values, assessed at the baseline interview were included. Prior work has demonstrated strong correlations between self-reported and actual CD4 cell counts, supporting the validity and reliability of self-report data (38, 39). CD4 cell counts were dichotomized into two categories: counts above and counts below 200 (200 × 103 cells/cubic mm). CD4 cell counts below 200 are sufficient for diagnosis of AIDS, even in the absence of AIDS-defining illnesses (40). The three participants without self-report or actual CD4 cell count data were excluded from analyses involving CD4 data.
5. Demographic and clinical characteristics
were assessed during the baseline interviews. Information on age, sex, race, education, insurance status, HIV transmission, and use of HIV medications was gathered. Adherence to HIV medication use in the past 3 days was assessed and the extent of adherence was categorized according to algorithms established for this study using a 1–6 scale ranging from “not at all adherent” to “completely adherent.”
Statistical Analysis
One sample t-tests were used to compare bodily pain scores in the current sample with scores reported for the general US population (37) and a national sample of HIV+ persons using data drawn from the HIV Cost and Services Utilization Study (HCSUS)(16, 41) [for information on the HCSUS see (42)]. The HCSUS did not conduct formal diagnostic interviews; instead brief screeners were used to screen for mental health problems. Scores in the present sample were compared to HCSUS participants who screened negative for anxiety disorders, depressive disorders, or substance dependence in the past year.
To examine correlates of pain, bivariate analyses were used to quantify the relationships among the variables prior to multivariate modeling. Bivariate analyses involved independent t-tests to test for differences in bodily pain scores based on sex (male vs. female), race (African-American vs. non-African American), CD4 counts (above vs. below 200), use of HIV medications (yes/no) and presence of psychological (anxiety; depression) and substance use (alcohol; non-alcohol) disorders. In addition, a one-way ANOVA tested for differences in bodily pain scores based on educational level (< high school diploma; high school diploma; some college/associate’s degree; college degree and higher), and Pearson product moment correlation coefficients were generated to characterize the association between bodily pain scores and age (years), ASI drug and alcohol severity scores, average days of drug use (all drugs), alcohol use in the past 30 days and HIV medication adherence. Significant bivariate correlates of bodily pain scores were then subjected to multivariate analysis. Multiple linear regression was used to evaluate the relationship between the independent variable (bodily pain scores), and the dependent variables identified in the bivariate analyses. All dependent variables were entered simultaneously into the multiple regression model. A standard probability level of .05 was used to evaluate the results.
Results
Comparison of pain scores with normative data
The mean bodily pain score in the current sample was 55.1 (SD = 28.6). The mean score for the US general population is 75.2 (SD = 23.7). Pain scores in the present sample were significantly lower than normative values indicating higher levels of pain (t = − 8.92, p < .001). The current sample also scored significantly lower than HCSUS participants who did not screen positive for anxiety disorders, depressive disorders, or substance dependence in the past year (Mean = 76.7;SD =24.7) (t = −9.61 , p<.001).
Bivariate correlates of pain scores
Bivariate analyses indicated that bodily pain scores were significantly related to CD4 cell counts. Persons with CD4 counts below 200 reported greater pain (n = 50; 31.4 %) (M = 48.48; SD = 28.55), compared to persons with CD4 counts above 200 (n = 109; 68.6 %) (M = 58.28; SD = 28.33) (t(157) = −2.02, p < .05). Persons with a mood disorder reported greater pain (M = 49.97; SD = 28.07), relative to persons without a mood disorder (M = 61.81; SD = 28.14) (t(160) = 2.66, p < .01). Bodily pain scores were inversely associated with age (r = −.21, p < .01), indicating that younger age was associated with less pain. Average days of drug use (all drugs) in the past 30 days was positively associated with bodily pain (r = −.17, p < .05). Bodily pain scores were not associated with sex, race, education, use of HIV medications, presence of anxiety disorder, ASI drug or alcohol severity scores, average days of alcohol use in the past 30 days, presence of alcohol or non-alcohol substance use disorders or adherence to HIV medications.
Multivariate analyses of pain scores
Based on the bivariate findings, the following dependent variables were examined in multivariate analyses of pain scores: age, CD4 counts, presence of mood disorder, and average days of drug use. Results of the multiple linear regression analysis are shown in Table 3. As displayed in the table, the beta coefficients for the following independent variables were significantly different from zero: age, CD4 counts, and presence of mood disorder. The beta coefficient for average days of drug use did not differ significantly from zero. Presence of mood disorder accounted for the largest share of unique variance in bodily pain scores (4%), followed by age (3% of unique variance) and CD4 counts (2% of unique variance). The complete model including all predictors explained 12% (10% adjusted) of the variance in pain scores.
Discussion
This sample HIV+ persons with diagnosed comorbid psychological and substance use disorders reported high levels of bodily pain that were substantially greater than the general US population. Bodily pain scores were on average, 20 points lower (indicating more pain) in the current sample compared to normative values and scores among HIV+ persons who screened negative for anxiety disorders, depressive disorders or substance dependence. This difference greatly exceeds the 5 point difference in SF-36 scores generally considered to be clinically significant (37). Bivariate analyses indicated that the presence of mood disorder, low CD4 cell counts (below 200), older age, and more days of drug use (all drugs) in the past month were associated with increased pain. All of these correlates except for days of drug use were significantly associated with pain in multivariate analyses (see Table 3). Notably, the presence of mood disorder explained the largest share of unique variance in bodily pain scores, followed by age and CD4 counts. Pain scores were on average were nearly 12 points lower among persons with a current mood disorder compared to those without mood disorder—a difference that is a clinically significant. These findings are consistent with prior work indicating a strong relationship between pain and depressive symptoms in HIV+ persons (5, 43–45).
On the other hand, the current results are somewhat at odds with our previous research in the HCSUS which indicated that increasing pain over time was associated with panic disorder but not major depression or PTSD (16). In fact, the present study did not find a significant relationship between presence of anxiety disorder and pain. A possible explanation for these divergent findings is that there were many more HIV+ persons in the current sample diagnosed with a mood disorder (44%) than an anxiety disorder (> 5%). In contrast, the prevalence of major depression, panic disorder and PTSD were all fairly similar in the HCSUS and ranged between 5 – 9% (16). The present findings indicate that the presence of clinical depression may be a stronger marker of concurrent pain than clinical anxiety among HIV+ persons with co-occurring psychological and substance use disorders.
As discussed above, multivariate analyses also revealed a significant association between increased pain and lower CD4 counts. Pain scores were on average almost 10 points lower among those with low CD4 counts (less than 200) relative to those with high CD4 counts, a clinically meaningful difference. These findings concur with prior studies supporting an association between increased pain and more advanced HIV disease (8, 12, 43, 45–47). Similarly, we previously reported that in the HCSUS, drug dependence was directly related to increased HIV illness burden (i.e., more advanced HIV clinical stage and presence of wasting syndrome) which in turn predicted greater pain over time (6). However, it should be noted that some studies have not found a relationship between more advanced HIV disease and increased pain (11, 48). Differences in the assessment of pain and/or the extent of HIV disease progression across samples may account for these discrepant results.
The finding that older age was associated with increased pain in multivariate analyses is consistent with findings in the general population (36). On the other hand, we found no association between age and reported pain in our prior research in the HCSUS (12). The divergence between these findings is somewhat surprising given that the mean age of the current sample and the HCSUS sample are quite similar (i.e., 39.7 and 38.8 years, respectively). However, the age range in the HCSUS sample was much broader (i.e., 18 –77 years) than the current sample (i.e., 24–60 years). Reasons for the different age-based findings in the two samples are unclear, although it should be noted that the age-related results in both samples held after accounting for HIV disease status.
Perhaps the most unexpected finding in the current sample was the lack of association between drug or alcohol use and reported pain. Although the bivariate analyses revealed that more days of drug use over the past 30 days was associated with greater pain, this relationship was not significant in the multivariate analyses. Pain was not correlated with drug or alcohol severity scores, days of alcohol use in the past month, or with the presence of alcohol or non-alcohol substance use disorders. These findings are inconsistent with our previous research in the HCSUS which found an association between use of a broad range of illicit substances, and increased pain (6). On the other hand, the current results agree with at least two prior studies indicating no differences in pain report between IDUs and non-IDUs (1, 19). It is possible that in the current sample, there was insufficient variation in the extent of drug/alcohol use which may have attenuated any potential association with pain.
In the current sample, pain scores did not vary based on sex, race, education, or use of HIV medications (yes/no). These findings diverge somewhat from prior reports. In the HCSUS, we found that bodily pain scores were lower, indicating more pain, among IV-drug using women (compared to men who have sex with men), the unemployed, and the less educated(12). On the other hand, bodily pain scores were higher (indicating less pain) among African Americans relative to whites (12). An earlier study in a convenience sample of HIV+ persons found that not only did women report more pain than men, non-whites reported more pain compared to whites (1). It is possible that variations in pain assessment and/or in sample characteristics may account for these discrepant findings. Additional investigations on racial/ethnic and sex differences in pain among HIV+ persons are warranted.
Although this study is the first to the authors’ knowledge to specifically examine the prevalence and correlates of pain in HIV+ persons with comorbid psychological and substance use disorders, limitations should be noted. First, the high patient volume during clinic hours made it difficult to locate, recruit and screen all eligible study participants. Thus, of the 1,412 eligible participants contacted, 78% were screened (see Figure 1). Second, the multi-step enrollment process impacted study attrition rates. For example, after participants were screened eligible, the baseline assessment was administered over two sessions; both sessions were to be administered within a one month time frame. As a result, 16% (62/374) of the participants that were eligible for SCID interview missed their initial baseline interview and 6% missed session two of their baseline assessment.
In sum, the present study found that HIV+ persons with comorbid psychological and substance use disorders reported more pain than the US general population. The differences in reported pain were substantial and clinically meaningful. The key correlates of increased pain in the current sample were the presence of mood disorder, older age and CD4 counts below 200. Notably, the presence of mood disorder accounted for the largest share of unique variance associated with pain, suggesting that mood disorders may be a key marker for pain among triply diagnosed HIV+ individuals. The current findings support the need for an enhanced focus on the identification and treatment of pain among HIV+ persons. As the present investigation and others (1, 5, 11, 12, 18, 19, 46–48) have noted, pain remains a considerable problem in HIV despite advances in treatment approaches. Moreover, several reports suggest that pain is undertreated in HIV+ persons (1, 4, 10, 11, 45, 49), and this undertreatment of pain is especially prominent among women, the less educated, and IDUs (49). Future research should examine the extent to which pain among HIV+ persons with co-occurring psychological and substance use disorders is adequately addressed, particularly as the current analysis indicates that this population is especially vulnerable to the experience of pain.
Table 2.
Multiple linear regression analysis of age, CD4 counts, presence of mood disorder, and average days of drug use on SF-36 bodily pain subscale scores
| Variables Entered | β | sr2 (unique) | Model R2 |
|---|---|---|---|
| Age | −.18* | .03 | |
| CD4 counts | .15* | .02 | |
| Mood Disorder | −.20* | .04 | |
| Drug use | −.10 | .01 | |
| .12 |
Note: β = Standardized regression coefficient; sr2 (unique) = unique contribution of an independent variable to R2 in the total set of independent variables; Model R2 = Coefficient of determination (goodness of fit) for overall regression model after entry of each independent variable
p < .05.
Acknowledgements
Sources of support: This work was supported by a cooperative agreement for the "HIV/AIDS Treatment Adherence, Health Outcomes and Cost Study," a collaboration of six Federal entities within the U.S. Department of Health and Human Services (DHHS): The Center for Mental Health Services (CMHS), which had the lead administrative responsibility, and the Center for Substance Abuse Treatment (CSAT), both components of the Substance Abuse and Mental Health Services Administration (SAMHSA); the HIV/AIDS Bureau of the Health Resources and Services Administration (HRSA); the National Institute of Mental Health (NIMH), the National Institute on Drug Abuse (NIDA), and the National Institute on Alcohol Abuse and Alcoholism (NIAAA), all parts of the National Institutes of Health (NIH).
Footnotes
Disclaimer footnote: The views expressed are those of the author(s) and are not to be construed as official or as reflecting the views or policies of the Substance Abuse and Mental Health Services Administration (SAMHSA), the Health Resources and Services Administration (HRSA), the National Institutes of Health (NIH) or any other agencies of the U.S. Department of Health and Human Services (DHHS).
References
- 1.Breitbart W, McDonald MV, Rosenfeld B, et al. Pain in ambulatory AIDS patients. I: Pain characteristics and medical correlates. Pain. 1996;68:315–321. doi: 10.1016/s0304-3959(96)03215-0. [DOI] [PubMed] [Google Scholar]
- 2.Douaihy AB, Stowell KR, Kohnen S, et al. Psychiatric aspects of comorbid HIV/AIDS and pain, Part 2. AIDS Read. 2007;17:350–352. 7–61. [PubMed] [Google Scholar]
- 3.Douaihy AB, Stowell KR, Kohnen S, et al. Psychiatric aspects of comorbid HIV/AIDS and pain, Part 1. AIDS Read. 2007;17:310–314. [PubMed] [Google Scholar]
- 4.Frich LM, Borgbjerg FM. Pain and pain treatment in AIDS patients: a longitudinal study. J Pain Symptom Manage. 2000;19:339–347. doi: 10.1016/s0885-3924(00)00140-8. [DOI] [PubMed] [Google Scholar]
- 5.Rosenfeld B, Breitbart W, McDonald MV, et al. Pain in ambulatory AIDS patients. II: Impact of pain on psychological functioning and quality of life. Pain. 1996;68:323–328. doi: 10.1016/s0304-3959(96)03220-4. [DOI] [PubMed] [Google Scholar]
- 6.Tsao JCI, Dobalian A, Stein JA. Illness burden mediates the relationship between pain and illicit drug use in persons living with HIV. Pain. 2005;119:124–132. doi: 10.1016/j.pain.2005.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vogl D, Rosenfeld B, Breitbart W, et al. Symptom prevalence, characteristics, and distress in AIDS outpatients. J Pain Symptom Manage. 1999;18:253–262. doi: 10.1016/s0885-3924(99)00066-4. [DOI] [PubMed] [Google Scholar]
- 8.Hewitt DJ, McDonald M, Portenoy RK, et al. Pain syndromes and etiologies in ambulatory AIDS patients. Pain. 1997;70:117–123. doi: 10.1016/s0304-3959(96)03281-2. [DOI] [PubMed] [Google Scholar]
- 9.Del Borgo C, Izzi I, Chiarotti F, et al. Multidimensional aspects of pain in HIV-infected individuals. AIDS Patient Care STDS. 2001;15:95–102. doi: 10.1089/108729101300003690. [DOI] [PubMed] [Google Scholar]
- 10.Larue F, Fontaine A, Colleau SM. Underestimation and undertreatment of pain in HIV disease: multicentre study. BMJ. 1997;314:23–28. doi: 10.1136/bmj.314.7073.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCormack JP, Li R, Zarowny D, et al. Inadequate treatment of pain in ambulatory HIV patients. Clin J Pain. 1993;9:279–283. doi: 10.1097/00002508-199312000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Dobalian A, Tsao JCI, Duncan RP. Pain and the use of outpatient services among persons with HIV: results from a nationally representative survey. Med Care. 2004;42:129–138. doi: 10.1097/01.mlr.0000108744.45327.d4. [DOI] [PubMed] [Google Scholar]
- 13.Gatchel RJ, Turk DC, editors. Psychosocial factors in pain: critical perspectives. New York: The Guilford Press; 1999. [Google Scholar]
- 14.Bing EG, Burnam A, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 15.Smith MY, Egert J, Winkel G, et al. The impact of PTSD on pain experience in persons with HIV/AIDS. Pain. 2002;98:9–17. doi: 10.1016/s0304-3959(01)00431-6. [DOI] [PubMed] [Google Scholar]
- 16.Tsao JCI, Dobalian A, Naliboff BD. Panic disorder and pain in a national sample of persons living with HIV. Pain. 2004;109:172–180. doi: 10.1016/j.pain.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Fantoni M, Ricci F, Del Borgo C, et al. Multicentre study on the prevalence of symptoms and symptomatic treatment in HIV infection. J Pallitat Care. 1997;13:9–13. [PubMed] [Google Scholar]
- 18.Martin C, Pehrsson P, Osterberg A, et al. Pain in ambulatory HIV-infected patients with and without intravenous drug use. Eur J Pain. 1999;3:157–164. doi: 10.1053/eujp.1999.0111. [DOI] [PubMed] [Google Scholar]
- 19.Breitbart W, Rosenfeld B, Passik S, et al. A comparison of pain report and adequacy of analgesic therapy in ambulatory AIDS patients with and without a history of substance abuse. Pain. 1997;72:235–243. doi: 10.1016/s0304-3959(97)00039-0. [DOI] [PubMed] [Google Scholar]
- 20.Mellins CA, Havens JF, McCaskill E, et al. Mental health, substance use and disclosure are significantly associated with the medical treatment adherence of HIV- infected mothers. Psychology, Health and Medicine. 2002;7:451–460. [Google Scholar]
- 21.Sherbourne CD, Hays RD, Fleishman JA, et al. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. Am J Psychiatry. 2000;157:248–254. doi: 10.1176/appi.ajp.157.2.248. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Williams JB, Gibbon M, et al. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 23.Williams JB, Gibbon M, First MB, et al. The Structured Clinical Interview for DSM-III-R (SCID). II. Multisite test-retest reliability. Arch Gen Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 24.HIV/AIDS Treatment Adherence Health Outcomes and Cost Study Group. The HIV/AIDS Treatment Adherence, Health Outcomes and Cost Study: Conceptual foundations and overview. AIDS Care. 2004;16:S6–S21. doi: 10.1080/09540120412331315312. [DOI] [PubMed] [Google Scholar]
- 25.Kessler R, Andrews G, Mroczek D, et al. The World Health Organization Composite International Diagnostic Short-Form (CIDI-SF) Geneva: WHO; 1998. [Google Scholar]
- 26.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 27.Aidala A. Training guide: Client Diagnostic Questionnaire. Evaluations and Technical Assistance Center: Columbia University of Public Health; 1999. [Google Scholar]
- 28.McLellan AT, Kushner H, Metzger D, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 29.McLellan AT, Luborsky L, Woody GE, et al. An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. J Nerv Ment Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Zanis DA, McLellan AT, Corse S. Is the Addiction Severity Index a reliable and valid assessment instrument among clients with severe and persistent mental illness and substance abuse disorders? Community Ment Health J. 1997;33:213–227. doi: 10.1023/a:1025085310814. [DOI] [PubMed] [Google Scholar]
- 31.Zanis DA, McLellan AT, Cnaan RA, et al. Reliability and validity of the Addiction Severity Index with a homeless sample. J Subst Abuse Treat. 1994;11:541–548. doi: 10.1016/0740-5472(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 32.Argeriou M, McCarty D, Mulvey K, et al. Use of the Addiction Severity Index with homeless substance abusers. J Subst Abuse Treat. 1994;11:359–365. doi: 10.1016/0740-5472(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 33.Segal DL, Hersen M, Van Hasselt VB. Reliability of the Structured Clinical Interview for DSM-III-R: an evaluative review. Compr Psychiatry. 1994;35:316–327. doi: 10.1016/0010-440x(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 34.Hays R, Cunningham W, Sherbourne C, et al. Health-related quality of life in people with HIV infection: Results from the HIV Cost and Services Utilization Study. Am J Med. 2000;108:714–722. doi: 10.1016/s0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- 35.Stewart AL, Ware JE. Measuring functioning and well-being: the medical outcomes study approach. Durham: Duke University Press; 1992. [Google Scholar]
- 36.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 37.Ware JE, Kosinski M, Gandek B. SF-36 Health Survey: manual and interpretation guide. Lincoln, RI: Quality Metric Inc; 2000. [Google Scholar]
- 38.Cunningham WE, Rana HM, Shapiro MF, et al. Reliability and validity of self-report CD4 counts-in persons hospitalized with HIV disease. J Clin Epidemiol. 1997;50:829–835. doi: 10.1016/s0895-4356(97)00061-9. [DOI] [PubMed] [Google Scholar]
- 39.Kalichman SC, Rompa D, Cage M. Reliability and validity of self-reported CD4 lymphocyte count and viral load test results in people living with HIV/AIDS. Int J STD AIDS. 2000;11:579–585. doi: 10.1258/0956462001916551. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control. 1993 Revised Classification System for HIV Infection and Expanded Surveillance Case Definition for AIDS Among Adolescents and Adults. MMWR. 1992;41(RR17) [PubMed] [Google Scholar]
- 41.Tsao JCI, Dobalian A, Myers CD, et al. Pain and use of complementary and alternative medicine in a national sample of persons living with HIV. J Pain Symptom Manage. 2005;30:418–432. doi: 10.1016/j.jpainsymman.2005.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bozzette S, Berry S, Duan N, et al. The care of HIV-infected adults in the United States. HIV Cost and Services Utilization Study Consortium. N Engl J Med. 1998;339:1897–1904. doi: 10.1056/NEJM199812243392606. [DOI] [PubMed] [Google Scholar]
- 43.Evans S, Ferrando S, Sewell M, et al. Pain and depression in HIV illness. Psychosomatics. 1998;39:528–535. doi: 10.1016/S0033-3182(98)71285-X. [DOI] [PubMed] [Google Scholar]
- 44.Lagana L, Chen XH, Koopman C, et al. Depressive symptomatology in relation to emotional control and chronic pain in persons who are HIV positive. Rehabilitation Psychology. 2002;47:402–414. [Google Scholar]
- 45.Singer EJ, Zorilla C, Fahy-Chandon B, et al. Painful symptoms reported by ambulatory HIV-infected men in a longitudinal study. Pain. 1993;54:15–19. doi: 10.1016/0304-3959(93)90094-6. [DOI] [PubMed] [Google Scholar]
- 46.Breitbart W. Pain management and psychosocial issues in HIV and AIDS. American Journal of Hospice and Palliative Care. 1996;13:20–29. doi: 10.1177/104990919601300108. [DOI] [PubMed] [Google Scholar]
- 47.Schofferman J, Brody R. Pain in far advanced AIDS. In: Chapman R, Foley K, editors. Advances in Pain Research and Therapy. New York: Raven Press; 1990. pp. 379–386. [Google Scholar]
- 48.Lebovits AH, Smith G, Maignan M, et al. Pain in hospitalized patients with AIDS: analgesic and psychotropic medications. Clin J Pain. 1994;10:156–161. doi: 10.1097/00002508-199406000-00010. [DOI] [PubMed] [Google Scholar]
- 49.Breitbart W, Rosenfeld BD, Passik SD, et al. The undertreatment of pain in ambulatory AIDS patients. Pain. 1996;65:243–249. doi: 10.1016/0304-3959(95)00217-0. [DOI] [PubMed] [Google Scholar]