Abstract
Background
Menopausal hormone therapy increases mammographic density. We determined whether increases in serum estrone sulfate (E1S) levels during menopausal hormone therapy predict increased mammographic density.
Methods
We measured percent mammographic density and serum E1S levels in 428 participants of the Postmenopausal Estrogen/Progestin Interventions study who were randomly assigned to daily conjugated equine estrogen (CEE) 0.625 mg alone, CEE + daily medroxyprogesterone acetate (MPA) 2.5 mg, CEE + cyclical MPA (10 mg days 1-12 per 28-day cycle), or CEE + cyclical micronized progesterone (10 mg days 1-12). Serum E1S levels were determined by RIA. Information about covariates was determined by annual questionnaire. Using linear regression, we determined the association between change in E1S level from baseline to 12 months and change in percent mammographic density (by semiquantitative interactive threshold method).
Results
After controlling for baseline mammographic density, age, body mass index, alcohol intake, parity, smoking, ethnicity, physical activity, and age at first pregnancy, mammographic density increased by 1.3% for every 1 ng/mL increase in E1S level (P < 0.0001). The association between change in E1S level and change in mammographic density differed by treatment group (greater effect in CEE + cyclical MPA group versus CEE group; P = 0.05). After controlling for treatment group, change in the ratio of E1S to E1 was also positively associated with change in mammographic density.
Conclusions
Increases in serum E1S levels during menopausal hormone therapy are associated with increases in mammographic density. The relative contribution of E1S and E1 to stimulation of breast tissue awaits further elucidation.
Introduction
High mammographic density is a risk factor for breast cancer (1, 2). Dense tissue in >50% of the breast could account for up to one third of breast cancer cases (1). The increase in mammographic density (3) with use of menopausal hormone therapy may be related to elevated breast cancer risk among hormone therapy users. Moreover, the presence of dense tissue decreases the cancer-detecting sensitivity of mammography (4). Therefore, factors that predict the magnitude of increase in mammographic density among menopausal hormone therapy users are of interest and are largely unexplored.
Our group has previously shown that greater increases in serum estrone (E1) levels during menopausal hormone therapy with conjugated equine estrogens (CEE) plus a progestogen predict greater increases in mammographic density (5). However, E1 sulfate (E1S) is quantitatively the most important component of CEE (6), and circulating E1S may have effects on breast tissue. For example, the breast is rich in the steroid sulfatase enzyme necessary for conversion of E1S to E1 and estradiol (7). In addition, serum E1S levels are associated with breast cancer risk in postmenopausal women. In a meta-analysis, women with serum E1S levels in the highest quintile had a 2-fold greater risk of breast cancer relative to women with E1S levels in the lowest quintile (8). Therefore, we hypothesized that greater increases in serum E1S level among women assigned to CEE-containing hormone therapy would predict greater increases in mammographic density. We also posited that increase in E1S levels would more strongly predict increases in mammographic density among women treated with CEE plus a progestogen than among women treated with CEE alone. Prior studies have not addressed this hypothesis.
With the goal of enhancing the understanding of the biological effects of estrogens on breast tissue, and how these effects relate to mammographic density, we analyzed the association between changes in serum E1S levels and changes in mammographic density using data from the Postmenopausal Estrogen/Progestin Interventions Trial, a randomized controlled trial of CEE, with or without a progestogen, in postmenopausal women.
Materials and Methods
Participants
We analyzed data from the Postmenopausal Estrogen/Progestins Intervention Study-Mammographic Density Substudy (PEPI-MDS), a study initiated after completion of the PEPI randomized controlled trial. The PEPI trial design has been described in detail (9). In brief, the PEPI trial was a randomized controlled trial designed to compare the effects of placebo and several menopausal hormone therapy regimens on cardiovascular risk factors in postmenopausal women. Participants were recruited between December 27, 1989 and February 8, 1991 at seven centers: George Washington University, Washington, DC; The Johns Hopkins University, Baltimore, MD; Stanford University, Stanford, CA; University of California, Los Angeles, CA; University of California, San Diego, CA; University of Iowa, Iowa City, IA; and University of Texas Health Science Center, San Antonio, TX. Inclusion criteria required participants to be between 45 and 64 y of age and to be at least 1 y postmenopausal. Women with any major contraindication to the use of estrogen or progestin therapy (e.g., breast cancer) were excluded (9).
Of the 1,557 women screened for inclusion in the PEPI randomized controlled trial, 875 met the inclusion criteria and were randomized to one of the five treatment regimens. The five treatment regimens were as follows: placebo, 0.625 mg/d CEE, daily CEE plus medroxyprogesterone acetate (MPA) 10 mg/d for 12 d/mo (CEE + cyclical MPA), daily CEE plus MPA 2.5 mg/d continuously (CEE + MPA continuous), and daily CEE plus micronized progesterone (microP) 200 mg/d for 12 d/mo (CEE + microP). The PEPI trial was approved by the human research review boards at each study site, and informed consent was obtained from all participants.
Initiated after completion of the original PEPI randomized controlled trial, the PEPI-MDS was intended to elucidate hormonal, genetic, and lifestyle determinants of mammographic density. Mammograms were retrievable from 603 of the 875 PEPI trial participants. Because 7 women had breast implants and mammograms for 2 women were technically inadequate, mammograms from 594 women (67.9% of the 875 women in the PEPI trial) were examined in the PEPI-MDS (3, 5, 10, 11). Because the goal was to consider hormone therapy–associated changes in E1S level, data from the 105 participants assigned to placebo were not considered in this study. Fifty-one of the 489 women assigned to active therapy were missing baseline or 12-mo information about mammographic density and/or E1S level. A further 10 women had extreme outlying values of E1S {i.e., greater than [upper quartile + 3*(upper quartile-lower quartile)] or less than [lower quartile − 3*(upper quartile-lower quartile)]; ref. 12}. Thus, we analyzed data from the 428 active hormone therapy participants for whom we had complete E1S and mammographic density information at both baseline and 12-mo follow-up.
Questionnaire Measurements
We obtained information about age, ethnicity, cigarette smoking, alcohol use, physical activity level, parity, ethnicity, prior hysterectomy, age at menopause, and prior use of menopausal hormone therapy from standardized self-report questionnaires (9). At the baseline visit, using a standardized algorithm, weight and height were measured for calculation of body mass index (BMI; kg/m2; ref. 13). Adherence to treatment assignment was defined as taking at least 80% of study medication at both 6- and 12-mo follow-up visits (verified by pill count).
E1S and E1 Measurements
Fasting morning blood samples were obtained at baseline and 12-mo follow-up within 24 to 48 h of the study mammograms. Serum samples were stored at −70°C until assay. One of the authors (F.Z.S.) analyzed serum E1S levels using direct RIA (DSL-5400, Diagnostic Systems Laboratories, Inc.), as described previously (14). Laboratory assays for baseline and 12-mo values of E1S were done at the same time. Interassay and intraassay coefficients of variation for serum E1S were 4.6% and 5.5%, respectively, and the lower limit of detection was 0.05 ng/mL. Serum E1 was analyzed by an in-house RIA after organic solvent extraction and celite column chromatography in the laboratory of B.R. Hopper (University of California, San Diego, CA). For the E1 assay, the interassay coefficient of variation was 15%, the intraassay coefficient of variation was 16%, and the lower limit of detection was 3 pg/mL.
Mammographic Density Measurement
Baseline and 12-mo conventional craniocaudal mammograms obtained between 1989 and 1994 (during the original PEPI study) were retrieved from the seven participating PEPI clinical centers. Breast density was read by a single expert reader (G.U.) who was masked to treatment assignment. Using a validated method described previously (15), mammograms were digitized at a resolution of 150 pixels per square inch. Breast tissue was outlined on the digitized mammogram image by the reader. Next, for each image, the reader established a threshold above which breast tissue would be considered dense and a density threshold below which breast tissue would be considered nondense. The software calculated percent mammographic density as the ratio of the total area of dense breast tissue in the image to the total area of breast tissue. The intrarater reliability for percent mammographic density was high: intraclass correlation coefficients were >0.95 for the 104 mammograms that were rated as not difficult to read or as slightly difficult to read and 0.91 for the 16 mammograms that were difficult to read or very difficult to read (as judged by the expert reader; ref. 3).
Statistical Analysis
We compared E1S levels at baseline and 12 mo, and change in E1S levels at 12 mo, for each of the estrogen + progestogen treatment groups with those of the CEE-only group using two-sample t tests. Change in E1S, change in E1S + E1, and change in E1S/E1 were symmetrically distributed. Simple (unadjusted) Spearman correlations between change in E1S level (12 mo minus baseline) and change in mammographic density were calculated.
Multivariable linear regression was used to examine the adjusted association between change in E1S level (main exposure) and change in mammographic density (outcome). Because the residual plot showed increasing residual values with increasing predicted Y values, we used a weighted regression procedure. We regressed the absolute values of the residuals from the ordinary least-squares regression on the independent variables to generate predicted residual values on which to base weights. The weight for each sample record was calculated as 1/(predicted residual)2. Weighted multivariable linear regression models were done with and without data from women with extreme outlying values of E1S change (12). Because inclusion of outliers yielded similar results to exclusion of outliers, we excluded outliers from our final models. Models were adjusted for baseline mammographic density (continuous log transformed), age (continuous), BMI (tertile), change in BMI (12 mo minus baseline, continuous), daily alcohol intake (log transformed), parity (none versus 1-2 versus ≥3 pregnancies), cigarette smoking (current versus not current), ethnicity (Caucasian versus not Caucasian), physical activity tertile, hormone therapy arm (CEE, CEE + MPA continuous, CEE + cyclical MPA, CEE + microP), and age at first pregnancy based on prior publications (3, 16-21). Because the association between BMI and change in mammographic density was nonlinear, we adjusted for BMI in tertiles. To avoid excluding nulliparous women while maintaining the ability to adjust for parity-related information, we created scaled variables for the multivariable linear regression models. Each parous woman was assigned the value of her own age at first pregnancy minus the mean age at first pregnancy for all parous women; thus, each nulliparous woman was assigned a value of zero for age at first pregnancy. To assess whether the association between change in E1S and change in mammographic density change varied by treatment group, interaction terms for treatment arm*change in E1S level were included in the regression models.
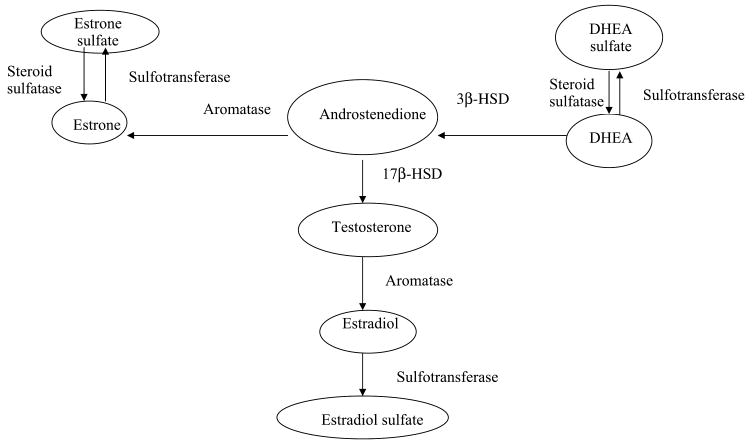
In an attempt to take into account the biological interconversion between E1S and E1 by the steroid sulfatase enzyme (Fig. 1), we ran a second set of multivariable models. These models added change in E1 levels (12 mo minus baseline) to the model containing the covariates listed above. There was a statistically significant correlation between change in E1 levels and change in E1S levels (Spearman correlation = 0.69; P < 0.0001). The variance inflation factor [1/(1-squared multiple correlation between E1S and the remainder of the covariates); ref. 22] indicated no appreciable multicollinearity.
Figure 1.
Estrogen metabolism in postmenopausal women. DHEA, dehydroepiandrosterone; 3β-HSD, 3β-hydroxysteroid dehydrogenase; 17β-HSD, β-hydroxysteroid dehydrogenase; ER, estrogen receptor; Sulfotransferase, estrogen sulfotransferase and phenolsulfotransferase (31, 32).
Because the change in the ratio of E1S to E1 could indicate hormone therapy–associated changes in the balance of E1S and E1, we created a third set of multivariable linear regression models to further jointly explore overall serum E1S and E1 status. Maintaining change in mammographic density as the outcome, and adjusting for the same covariates as the previous multivariable linear regression models, we did multivariable linear regression with the change in the ratio of E1S to E1 (12 mo minus baseline) as the main exposure.
Results
Baseline Characteristics
Baseline characteristics of the participants comprising the analytic sample are displayed in Table 1. On average, participants were 56.2 ± 4.2 years old and 5.7 ± 2.7 years postmenopausal at baseline. Participants were primarily Caucasian and nonsmokers, and 90% were adherent to treatment assignment at both 6- and 12-month follow-up. Mean baseline BMI was 26 kg/m2. Characteristics of the analytic sample did not differ notably from the excluded PEPI-MDS participants or from the remainder of the PEPI participants. Because we excluded women assigned to placebo from the current analysis, mammographic density change and E1S change were higher in the participants of the current study than in the remainder of the PEPI-MDS participants.
Table 1. Baseline characteristics of the analytic sample, excluded PEPI participants, and excluded PEPI-MDS participants.
| Characteristic | Analytic sample (complete baseline and 12-mo mammographic density and serum E1S information), n = 428 | Excluded PEPI-MDS participants (incomplete E1S or mammographic density or assignment to placebo arm), n = 166* | ||
|---|---|---|---|---|
| Mean (SD) | n (frequency) | Mean (SD) | n (frequency) | |
| Age (y) | 56.2 (4.2) | 55.6 (4.6) | ||
| Years since menopause (mean)† | 5.7 (2.7) | 5.5 (2.6) | ||
| BMI (kg/m2) | 25.9 (4.4) | 26.7 (4.6) | ||
| Prior use of hormone therapy‡ | 244 (57.0) | 85 (51.2) | ||
| Recency of hormone therapy use (mo)§ | 23.4 (43.7) | 28.4 (50.8) | ||
| No. pregnancies resulting in live births | 3.2 (1.7) | 3.1 (1.8) | ||
| Smoking | ||||
| Current | 51 (11.9) | 26 (15.7) | ||
| Former | 155 (36.2) | 70 (42.2) | ||
| Never | 222 (51.9) | 70 (42.2) | ||
| Alcohol use (g/d) | 6.3 (12.6) | 6.5 (12.0) | ||
| Level of physical activity‖ | ||||
| Low | 282 (65.9) | 118 (71.1) | ||
| Medium | 143 (33.4) | 46 (27.7) | ||
| High | 3 (0.7) | 2 (1.2) | ||
| Nonwhite ethnicity | 45 (10.5) | 27 (16.3) | ||
| Adherence to treatment assignment¶ | 385 (90.0) | 134 (80.7) | ||
| Hysterectomy** | 129 (30.1) | 50 (30.1) | ||
| Baseline mammographic density (median %, interquartile range)†† | 24 (27) | 24 (30) | ||
| Baseline E1S level nmol/L, mean (SD) | 1.80 (0.84) | 2.45 (2.11) | ||
We excluded data from 51 PEPI-MDS participants who did not have complete baseline and follow-up information on mammographic density and E1S level, 105 participants assigned to placebo, and 10 participants with extreme outlying values for baseline E1S or 12-mo change in E1S.
The last menstrual period for women who reported having a hysterectomy with bilateral oophorectomy was the date of the hysterectomy.
Women were allowed to enroll in PEPI-MDS if they discontinued menopausal hormone therapy for at least 2 mo before the first screening visit.
Months elapsed since menopausal hormone therapy use (based on self-reported date of last use) in those participants who reported prior use of hormone therapy.
Self-reported activity was scored as 1 (inactive), 2 (light), 3 (moderate), or 4 (heavy) for each domain of exercise (leisure and home), and the overall score was calculated as 1/2 of leisure plus home scores minus 1. Categorized as low (≤1.5), medium (≥1.5 and <3), or high (≥3).
Adherence with at least 80% of study medication at both 6- and 12-mo follow-up visits.
Surgical removal of the uterus, with or without oophorectomy.
Percentage of the breast area that is dense, determined using the semiautomated interactive threshold method of Ursin and colleagues (15).
Change in E1S, E1, Their Sum, and Their Ratio
All E1 and E1S values were above the assay detection limits and mean baseline E1S and E1 levels did not vary significantly among treatment groups (Table 2A and B). Compared with women assigned to CEE, in whom mean change in serum E1S level (12 months minus baseline) was 1.93 ng/mL, the change in E1S was more pronounced among women assigned to the combination therapy arms (2.24 ng/mL; P = 0.06 for pooled CEE + progestogen groups versus CEE alone). This difference between unopposed CEE and combination therapy was especially notable among women assigned to CEE + microP therapy (2.49 ng/mL; P = 0.01 versus CEE). Change in E1S level was significantly higher among women assigned to CEE + microP than among women assigned to CEE + MPA continuous (P = 0.02). In contrast, as previously reported (5), the change in serum E1 levels was not significantly different in any combination therapy group compared with CEE alone (Table 2B).
Table 2. Changes in serum estrone (E1), estrone sulfate (E1S), and the ratio of E1S/E1 by treatment arm.
| A. Baseline, 12 mo, and change in serum E1S (ng/mL) by treatment arm | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Baseline | 12 mo | Change (12 mo − baseline) | |||||||
| Mean | 95% CI | P | Mean | 95% CI | P | Mean | 95% CI | P | ||
| CEE only (reference) | 105 | 0.65 | 0.59-0.71 | — | 2.58 | 2.29-2.86 | — | 1.93 | 1.65-2.20 | — |
| CEE + MPA cyclic | 103 | 0.59 | 0.53-0.64 | 0.14 | 2.86 | 2.53-3.19 | 0.20 | 2.27 | 1.95-2.60 | 0.11 |
| CEE + MPA continuous | 113 | 0.60 | 0.55-0.65 | 0.21 | 2.58 | 2.30-2.86 | 0.99 | 1.98 | 1.71-2.25 | 0.79 |
| CEE + microP | 107 | 0.69 | 0.63-0.74 | 0.37 | 3.18 | 2.80-3.55 | 0.01 | 2.49 | 2.13-2.85 | 0.01 |
| Estrogen + progestogen groups combined | 323 | 0.62 | 0.59-0.66 | 0.45 | 2.87 | 2.68-3.06 | 0.09 | 2.24 | 2.06-2.43 | 0.06 |
| B. Baseline, 12 mo, and change in E1 (pg/mL) by treatment arm | ||||||||||
| n | Baseline | 12 mo | Change (12 mo − baseline) | |||||||
| Mean | 95% CI | P | Mean | 95% CI | P | Mean | 95% CI | P | ||
| CEE only (reference) | 105 | 15.8 | 14.3-17.3 | — | 118 | 105-130 | — | 102 | 89.0-115 | — |
| CEE + MPA cyclic | 103 | 15.3 | 14.1-16.6 | 0.65 | 111 | 98.3-124 | 0.46 | 95.6 | 83.0-108 | 0.49 |
| CEE + MPA continuous | 113 | 16.1 | 14.6-17.6 | 0.75 | 110 | 98.4-121 | 0.37 | 93.8 | 82.5-105 | 0.35 |
| CEE + microP | 107 | 17.4 | 15.3-19.6 | 0.21 | 103 | 92.6-114 | 0.08 | 86.0 | 75.5-96.5 | 0.06 |
| Estrogen + progestogen groups combined | 323 | 16.3 | 15.3-17.3 | 0.58 | 108 | 101-115 | 0.17 | 91.8 | 85.2-98.4 | 0.15 |
| C. Baseline, 12 mo, and change in E1S/E1 [nmol/L]/[nmol/L] by treatment arm | ||||||||||
| n | Baseline | 12 mo | Change (12 mo − baseline) | |||||||
| Mean | 95% CI | P | Mean | 95% CI | P | Mean | 95% CI | P | ||
| CEE only (reference) | 105 | 35.9 | 32.0-39.9 | — | 18.5 | 17.0-20.0 | — | −17.4 | −21.7 to −13.1 | — |
| CEE + MPA cyclic | 103 | 31.7 | 26.9-36.6 | 0.19 | 21.9 | 20.0-23.8 | 0.01 | −9.9 | −15.0 to −4.8 | 0.03 |
| CEE + MPA continuous | 113 | 32.9 | 29.9-35.9 | 0.22 | 20.2 | 18.2-22.2 | 0.19 | −12.7 | −16.0 to −9.5 | 0.09 |
| CEE + microP | 107 | 36.3 | 32.6-40.0 | 0.89 | 25.4 | 23.1-27.8 | 0.0000 | −11.2 | −14.9 to −7.5 | 0.03 |
| Estrogen + progestogen groups combined | 323 | 33.6 | 31.4-35.9 | 0.32 | 22.5 | 21.2-23.7 | 0.0001 | −11.3 | −13.6 to −9.0 | 0.01 |
NOTE: P value is for the two-sample t test for the null hypothesis that the mean value for the listed treatment group is equal to the mean value of the CEE-alone treatment group.
Abbreviation: 95% CI, 95% confidence interval.
We evaluated an indicator of the balance of serum E1S to serum E1, expressed as E1S (nmol/L)/E1 (nmol/L). The ratio of E1S to E1 decreased significantly less by 12-month follow-up in participants assigned to combination therapy (decrease 11.3) compared with CEE alone (decrease 17.4; P = 0.01 for pooled CEE + progestogen groups versus CEE alone; Table 2C). In examining the change in E1S to E1 ratio separately for each treatment arm, we found that (a) the decline in the ratio was significantly less with administration of CEE alone than with administration of CEE + cyclical MPA (P = 0.03 versus CEE) or CEE + microP (P = 0.03 versus CEE; Table 2C) and (b) the ratio decreased significantly more in women assigned to CEE + microP than in women assigned to CEE + MPA continuous (P < 0.001).
Change in Mammographic Density
Mean change in percent mammographic density (12 months minus baseline) was 3.5% overall (SD, 9.3%). The increase in percent mammographic density was 0.5% (SD, 5.1%) among placebo group participants, 1.2% (SD, 7.5%) among CEE alone participants, 4.9% (SD, 8.7%) among CEE + cyclical MPA participants, 4.7% (SD, 10.4%) among CEE + MPA continuous participants, and 3.0% (SD, 9.8%) among CEE + microP participants. Change in mammographic density was significantly more pronounced among combination therapy recipients than among recipients of CEE alone, as described in detail in a prior publication (3).
Associations between Change in Serum E1S Level and Change in Percent Mammographic Density
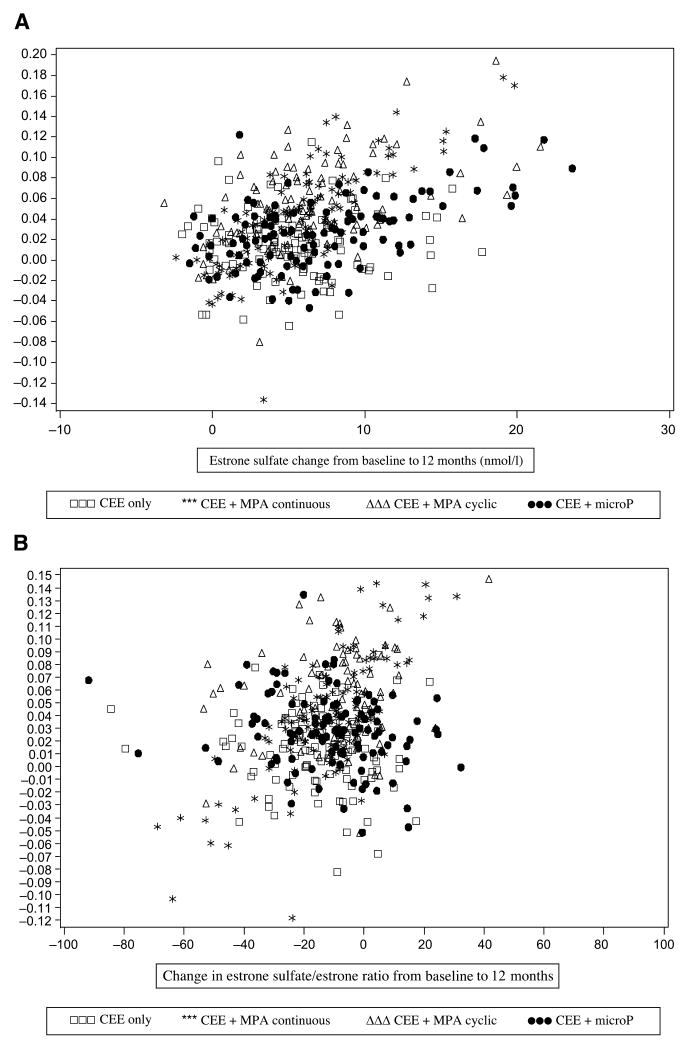
Change in E1S level and change in mammographic density (12 months minus baseline) were significantly positively correlated (Pearson r = 0.19; P < 0.0001). After adjustment for baseline mammographic density, age, BMI, change in BMI, alcohol intake, parity, cigarette smoking, physical activity, ethnicity, and age at first pregnancy, change in E1S was positively associated with increase in percent mammographic density (β = 1.3%; SE, 0.3%; P < 0.0001). That is, for every 1 nmol/L increase in E1S level at 12-month follow-up, percent mammographic density was 1.3% higher. Change in E1S remained significantly positively associated with change in percent mammographic density (β = 0.5%; SE, 0.2%; P = 0.006) after further adjustment for treatment assignment and treatment arm *Δ E1S interaction (Fig. 2A).
Figure 2.
A. Association between change in E1S level (main exposure, nmol/L) and absolute change in percent mammographic density (outcome), adjusted for baseline mammographic density, age, BMI (tertile), change in BMI (kg/m2), log alcohol intake (g/d), parity, cigarette smoking (current versus not current), physical activity tertile, age at first pregnancy, ethnicity, treatment arm, and treatment arm*Δ E1S. Outliers excluded, n = 428. B. Association between change in ratio of E1S to E1 (main exposure, E1S and E1 in nmol/L) and absolute change in percent mammographic density (outcome), adjusted for baseline mammographic density, age, BMI (tertile), change in BMI (kg/m2), log alcohol intake (g/d), parity, cigarette smoking (current versus not current), physical activity tertile, age at first pregnancy, ethnicity, treatment arm, and treatment arm*Δ [E1S/E1]. Outliers excluded, n = 426 (due to 2 missing E1 values).
Previously, our group reported that 12-month increase in serum E1 levels increase was significantly associated with increased mammographic density in PEPI (5). For this reason, and because of the significant statistical and biological interrelation between E1S and E1, we examined the joint influence of change in E1S and E1 during hormone therapy on change in mammographic density (same covariates as above). In the model including both E1S and E1, change in E1S level remained positively associated with change in percent mammographic density (β = 0.4%; SE, 0.2%; P = 0.03) and change in E1 was no longer a statistically significant predictor of change in mammographic density.
After adjustment for the same covariates listed above, change in the ratio of E1S to E1 (12 months minus baseline, E1S and E1 in nmol/L) was significantly positively associated with increase in percent mammographic density (β = 0.0003; SE, 0.0001; P = 0.002; Fig. 2B).
Treatment Arm Modification of the E1S-Mammographic Density Association
After adjustment for baseline mammographic density, age, BMI, change in BMI, alcohol intake, parity, cigarette smoking, physical activity, age at first pregnancy, ethnicity, and hormone treatment arm, there was a significant interaction between treatment assignment and change in E1S. The effect of E1S on change in mammographic density was weaker in women assigned to CEE alone than in women assigned to CEE + cyclical MPA. For every 10 nmol/L increase in E1S, the increase in percent mammographic density was 0.33% in women assigned to CEE alone and 5.1% for women assigned to CEE + cyclical MPA (P = 0.05 for interaction term; data not shown). For each of the remainder of the progestogen-containing arms, the Δ E1S-Δ mammographic density association was not statistically significantly different from that of participants assigned to CEE alone. A similar statistically significant interaction by treatment arm was observed in models examining change in E1S to E1 ratio (data not shown).
Discussion
In this longitudinal study, we found that increase in E1S levels during 12 months of CEE-containing menopausal hormone therapy was significantly positively associated with increase in percent mammographic density. For every 1 nmol/L increase in E1S level, percent mammographic density was 1.3% higher. The association was weaker in women assigned to CEE alone than in women assigned to CEE + cyclical MPA and was not altered in magnitude after adjustment for change in serum E1 level. Whether increases in mammographic density measured longitudinally predict increased breast cancer risk is not yet proven, but a 1% increment in mammographic density predicts a 2% higher relative risk of breast cancer (23).
To our knowledge, this is the first study to examine the E1S-mammographic density association during CEE-containing therapy. One prior study has examined change in E1S level as a predictor of mammographic density change during estradiol + norethindrone acetate therapy (24). After 6 months of estradiol + norethindrone acetate therapy, change in E1S level and mammographic density was significantly positively associated.
We found that the E1S-mammographic density association was more pronounced in women taking CEE + cyclical MPA compared with CEE alone. In addition, the increase in E1S level was greater with CEE + microP therapy than with administration of CEE alone. The explanation for both of these findings may be that progestogens prolong the clearance of E1S. Among postmenopausal women treated with a 24-h constant infusion of E1S (18 mg in normal saline), the subsequent i.m. administration of progesterone (100 mg in oil) significantly lowered the metabolic clearance rate of E1S and elevated E1S levels (25).
Our results are congruent with prior literature about sex steroid influences on breast tissue. Infusion of E1S to rats with mammary tumors significantly increases tumor volume, and local conversion (at the breast) of E1S to E1 is documented as one underlying mechanism (26). Human breast tissue expresses all necessary enzymes for estradiol synthesis, including steroid sulfatase, CYP17, CYP11a, CYP19, hydroxysteroid dehydrogenase, CYP1A1, CYP3A4, and CYP1B1 (27). Steroid sulfatase, previously referred to as E1 sulfatase, cleaves all steroid sulfates, including E1S (28). Normal breast tissue contains steroid sulfatase activity (i.e., the capacity to convert E1S to E1; ref. 29). It is feasible that local conversion of E1S into E1 at the breast by steroid sulfatase, and possibly further conversion to estradiol, may explain the increase in mammographic density. Our data do not permit us to directly test this theory. Our findings of hormone therapy–associated decline in the E1S to E1 ratio, suggesting increased sulfatase activity, are consistent with this hypothesis.
Our work has several implications. First, these results may partly explain why endogenous E1S level has been associated with both breast cancer risk (8) and with risk of breast cancer relapse (30) in postmenopausal women. That is, if circulating serum E1S is causatively linked with breast cancer, then the effects of E1S at the breast may be signaled by, or may act via, increasing mammographic density. Second, this research may help explain interindividual variability among women's mammographic density responses to menopausal hormone therapy. Not all women experience increases in mammographic density as a result of menopausal hormone therapy (10), perhaps because of differing degrees of sex steroid level changes, and/or because of variations in sex steroid metabolism, among individuals. Thus, our study enhances the understanding of the biological effects of estrogens on breast tissue.
A limitation of this study is the inability to examine the local influence of E1S on the breast. In addition, although we were able to account for concomitant increases in E1 level and explored the E1S-E1 interrelationship, we could not account for all aspects of the complex interplay between E1S, E1, and other estrogen metabolites. Finally, our results cannot be extrapolated to non–CEE-containing hormone therapy regimens. However, our study has many strengths, including its large sample size, prospective design, direct head-to-head comparison of four commonly prescribed hormone therapy regimens, proximate timing of serum sampling and mammogram acquisition, use of a validated reproducible technique for mammographic density quantification, hormone assay quality, and comprehensive data about potentially important confounders.
In conclusion, increases in serum E1S levels are positively associated with increases in mammographic density during CEE-containing menopausal hormone therapy. To reduce the burden of breast cancer associated with menopausal hormone therapy use, future research should more precisely describe the degree to which hormone therapy–associated increases in mammographic density are associated with increased breast cancer risk, and attempt to refine the understanding about which women are at particular risk of increased mammographic density and breast cancer risk during hormone therapy.
Acknowledgments
We thank the women who generously participated in the Postmenopausal Estrogen/Progestin Interventions Trial.
Grant support: NIH research grant 5K12 AG01004-08 from the National Institute on Aging (C.J. Crandall) and NIH grant 5R01 CA077708:08 (G.A. Greendale).
Footnotes
Disclosure of Potential Conflicts of Interest: E. Barrett-Connor: principal investigator of Reloxifene trials over 3 years ago. The other authors disclosed no potential conflicts of interest.
References
- 1.Boyd NF, Lockwood GA, Byng JW, Tritchler DL, Yaffe MJ. Mammographic densities and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 1998;7:1133–44. [PubMed] [Google Scholar]
- 2.American Cancer Society. Breast cancer facts & figures 2005-2006. Atlanta: American Cancer Society; 2005. [Google Scholar]
- 3.Greendale GA, Reboussin BA, Slone S, Wasilauskas C, Pike MC, Ursin G. Postmenopausal hormone therapy and change in mammographic density. J Natl Cancer Inst. 2003;95:30–7. doi: 10.1093/jnci/95.1.30. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg RD, Hunt WC, Williamson MR, et al. Effects of age, breast density, ethnicity, and estrogen replacement therapy on screening mammographic sensitivity and cancer stage at diagnosis: review of 183,134 screening mammograms in Albuquerque, New Mexico. Radiology. 1998;209:511–8. doi: 10.1148/radiology.209.2.9807581. [DOI] [PubMed] [Google Scholar]
- 5.Ursin G, Palla SL, Reboussin BA, et al. Post-treatment change in serum estrone predicts mammographic percent density changes in women who received combination estrogen and progestin in the Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. J Clin Oncol. 2004;22:2842–8. doi: 10.1200/JCO.2004.03.120. [DOI] [PubMed] [Google Scholar]
- 6.Speroff L, Fritz MA. Clinical gynecologic endocrinology and infertility. 7th. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 7.Thijssen JH. Local biosynthesis and metabolism of oestrogens in the human breast. Maturitas. 2004;49:25–33. doi: 10.1016/j.maturitas.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Key T, Appleby P, Barnes I, Reeves G. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst. 2002;94:606–16. doi: 10.1093/jnci/94.8.606. [DOI] [PubMed] [Google Scholar]
- 9.Espeland MA, Bush TL, Mebane-Sims I, et al. Rationale, design, and conduct of the PEPI Trial. Postmenopausal Estrogen/Progestin Interventions Control Clin Trials. 1995;16:3–19S. doi: 10.1016/0197-2456(94)00033-y. [DOI] [PubMed] [Google Scholar]
- 10.Greendale GA, Reboussin BA, Sie A, et al. Effects of estrogen and estrogen-progestin on mammographic parenchymal density. Postmenopausal Estrogen/Progestin Interventions (PEPI) Investigators. Ann Intern Med. 1999;130:262–9. doi: 10.7326/0003-4819-130-4_part_1-199902160-00003. [DOI] [PubMed] [Google Scholar]
- 11.Greendale GA, Palla SL, Ursin G, et al. The association of endogenous sex steroids and sex steroid binding proteins with mammographic density: results from the Postmenopausal Estrogen/Progestin Interventions Mammographic Density Study. Am J Epidemiol. 2005;162:826–34. doi: 10.1093/aje/kwi286. [DOI] [PubMed] [Google Scholar]
- 12.Rosner B. Fundamentals of biostatistics. 5th. Pacific Grove (CA): Duxbury; 2000. [Google Scholar]
- 13.Wood PD, Kessler G, Lippel K, Stefanick ML, Wasilauskas CH, Wells HB. Physical and laboratory measurements in the PEPI Trial Postmenopausal Estrogen/Progestin Interventions. Control Clin Trials. 1995;16:36–53S. doi: 10.1016/0197-2456(95)96882-c. [DOI] [PubMed] [Google Scholar]
- 14.Slater CC, Hodis HN, Mack WJ, Shoupe D, Paulson RJ, Stanczyk FZ. Markedly elevated levels of estrone sulfate after long-term oral, but not transdermal, administration of estradiol in postmenopausal women. Menopause. 2001;8:200–3. doi: 10.1097/00042192-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Ursin G, Astrahan MA, Salane M, et al. The detection of changes in mammographic densities. Cancer Epidemiol Biomarkers Prev. 1998;7:43–7. [PubMed] [Google Scholar]
- 16.Vachon CM, Kuni CC, Anderson K, Anderson VE, Sellers TA. Association of mammographically defined percent breast density with epidemiologic risk factors for breast cancer (United States) Cancer Causes Control. 2000;11:653–62. doi: 10.1023/a:1008926607428. [DOI] [PubMed] [Google Scholar]
- 17.Titus-Ernstoff L, Tosteson AN, Kasales C, et al. Breast cancer risk factors in relation to breast density (United States) Cancer Causes Control. 2006;17:1281–90. doi: 10.1007/s10552-006-0071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.El-Bastawissi AY, White E, Mandelson MT, Taplin SH. Reproductive and hormonal factors associated with mammographic breast density by age (United States) Cancer Causes Control. 2000;11:955–63. doi: 10.1023/a:1026514032085. [DOI] [PubMed] [Google Scholar]
- 19.Jeffreys M, Warren R, Gunnell D, McCarron P, Smith GD. Life course breast cancer risk factors and adult breast density (United Kingdom) Cancer Causes Control. 2004;15:947–55. doi: 10.1007/s10522-004-2473-3. [DOI] [PubMed] [Google Scholar]
- 20.Maskarinec G, Pagano I, Chen Z, Nagata C, Gram IT. Ethnic and geographic differences in mammographic density and their association with breast cancer incidence. Breast Cancer Res Treat. 2007;104:47–56. doi: 10.1007/s10549-006-9387-5. [DOI] [PubMed] [Google Scholar]
- 21.Gram IT, Funkhouser E, Tabar L. Moderate physical activity in relation to mammographic patterns. Cancer Epidemiol Biomarkers Prev. 1999;8:117–22. [PubMed] [Google Scholar]
- 22.Afifi AA, Clark V, May S. Computer-aided multivariate analysis. 4th. Boca Raton: Chapman & Hall/CRC; 2004. [Google Scholar]
- 23.Boyd NF, Byng JW, Jong RA, et al. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995;87:670–5. doi: 10.1093/jnci/87.9.670. [DOI] [PubMed] [Google Scholar]
- 24.Hofling M, Carlstrom K, Svane G, Azavedo E, Kloosterboer H, Von Schoultz B. Different effects of tibolone and continuous combined estrogen plus progestogen hormone therapy on sex hormone binding globulin and free testosterone levels—an association with mammographic density. Gynecol Endocrinol. 2005;20:110–5. doi: 10.1080/09513590400021151. [DOI] [PubMed] [Google Scholar]
- 25.Jasonni VM, Bulletti C, Franceschetti F, et al. Preliminary report on progesterone effect on peripheral estrone sulfate metabolism. Acta Eur Fertil. 1983;14:137–40. [PubMed] [Google Scholar]
- 26.Santner SJ, Levin MC, Santen RJ. Estrone sulfate stimulates growth of nitrosomethylurea-induced breast carcinoma in vivo in the rat. Int J Cancer. 1990;46:73–8. doi: 10.1002/ijc.2910460115. [DOI] [PubMed] [Google Scholar]
- 27.Kristensen VN, Borresen-Dale AL. Molecular epidemiology of breast cancer: genetic variation in steroid hormone metabolism. Mutat Res. 2000;462:323–33. doi: 10.1016/s1383-5742(00)00018-1. [DOI] [PubMed] [Google Scholar]
- 28.Nussbaumer P, Billich A. Steroid sulfatase inhibitors. Med Res Rev. 2004;24:529–76. doi: 10.1002/med.20008. [DOI] [PubMed] [Google Scholar]
- 29.Chetrite GS, Thomas JL, Shields-Botella J, Cortes-Prieto J, Philippe JC, Pasqualini JR. Control of sulfatase activity by nomegestrol acetate in normal and cancerous human breast tissues. Anticancer Res. 2005;25:2827–30. [PubMed] [Google Scholar]
- 30.Lonning PE, Helle SI, Johannessen DC, Ekse D, Adlercreutz H. Influence of plasma estrogen levels on the length of the disease-free interval in postmenopausal women with breast cancer. Breast Cancer Res Treat. 1996;39:335–41. doi: 10.1007/BF01806162. [DOI] [PubMed] [Google Scholar]
- 31.Harris RM, Wood DM, Bottomley L, et al. Phytoestrogens are potent inhibitors of estrogen sulfation: implications for breast cancer risk and treatment. J Clin Endocrinol Metab. 2004;89:1779–87. doi: 10.1210/jc.2003-031631. [DOI] [PubMed] [Google Scholar]
- 32.Dunning AM, Dowsett M, Healey CS, et al. Polymorphisms associated with circulating sex hormone levels in postmenopausal women. J Natl Cancer Inst. 2004;96:936–45. doi: 10.1093/jnci/djh167. [DOI] [PubMed] [Google Scholar]