Abstract
The Ponseti method of treatment for congenital clubfeet has gained widespread clinical acceptance. We have used manipulation, serial casting, and surgery to treat congenital clubfeet for almost 3 decades. Considering the Ponseti method of treatment to replace our traditional treatment method, we conducted a randomized, controlled trial evaluating the short-term outcome of the two treatment protocols. We evaluated foot function and applied a standardized measure of health status for children with orthopaedic problems. Nineteen patients (28 feet) were included in the trial. Nine infants (12 feet) were assigned to the Ponseti treatment group, and 10 (16 feet) were assigned to a group with initial casting and posteromedial release at the age of 6 to 8 months. The minimum followup was 3.3 years (mean, 3.5 years; range 3.3–3.8 years). Outcome measures included the Functional Rating System of Laaveg and Ponseti, the Pediatric Outcomes Data Collection Instrument (PODCI), and standardized radiographic measurements. At last followup the mean Functional Rating score was higher in the Ponseti group. Passive dorsiflexion and passive inversion-eversion were better in the Ponseti group. PODCI scales were comparable and radiographic outcome measures were similar in both groups. This trial has documented a favorable short-term outcome for the Ponseti method when compared with a traditional treatment protocol.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
In the last 2 decades, the Ponseti method of treatment for congenital clubfoot has gained widespread acceptance as a conservative way to address this complex deformity [24]. One report on the long-term outcome of the Ponseti method particularly inspired pediatric orthopaedic surgeons to adopt this treatment [7]. The authors reported in detail on the simplicity of the method to achieve and maintain a flexible, plantigrade, and painless foot. However, because there are no data on the worldwide use of different methods for clubfoot management, one could assume numerous centers still treat congenital clubfoot by initial casting followed by surgical correction of residual deformities. Outcome of treatment is rated differently in the literature with some authors presenting success rates of as much as 80% excellent or good short- to mid-term outcomes for Ponseti management and for surgical treatment [7, 31]. In light of seemingly comparable outcomes, the much less invasive treatment pioneered by Ignacio V. Ponseti is repeatedly cited as the preferred treatment [19, 22, 27, 29]. The evidence to support this estimation is based on retrospective trials and a few studies with historical control groups [19, 20, 29]. Larger groups of patients with followup have been reported only by a couple centers worldwide [20, 26].
For almost 3 decades, we treated congenital clubfoot with manipulation (following the guidelines of Johann Bösch from the 1950s [3], whose approach was remarkably similar to that of Ponseti) and casting up to the age of 6 months followed by posteromedial release. The less invasive character, the straightforward biomechanical concepts, and the favorable reports on the Ponseti method motivated us to organize a prospective, randomized trial to compare it with our traditional treatment method before changing the treatment protocol at our institution.
To compare the Ponseti method of treatment with our traditional treatment protocol to correct congenital clubfeet, we formulated two questions: (1) Is foot function different for the two methods in children at 3.5 years of age? (2) Is the health status for children with orthopaedic problems different at the age of 3.5 years?
Materials and Methods
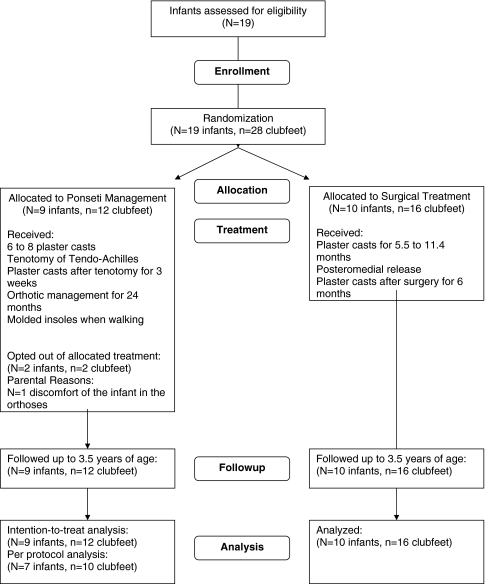
In 2001, we began a single-center, randomized, unblinded controlled trial with a parallel design. The trial was set up as an intention-to-treat analysis (Fig. 1). We included only otherwise healthy infants younger than 2 weeks born with clubfoot/clubfeet and without any other congenital anomalies. Parents were informed about the intention of the trial and it was made clear that the two treatment concepts were explicitly different. We indicated the traditional treatment was the current standard at our clinic for congenital clubfeet and that this institution had long-time experience in providing such treatment. Parents also were informed that the Ponseti method was much less invasive and successfully performed at institutions abroad but that we could not provide data on outcome for the Ponseti treatment when applied to our local setting. When parents gave written informed consent to participate in the study, infants were randomly assigned to one of two study groups using a randomization table according to a uniform distribution. In the case of bilateral clubfeet, both feet received the same treatment.
Fig. 1.
A summary of the trial is shown.
The outcome measure used to assess foot function was the Functional Rating System (FRS) of Laaveg and Ponseti (FRS) [21]. A successful treatment was defined by FRS 75 or greater of 100 points. Assuming group proportions of 25% or 75%, respectively, a sample size of 23 clubfeet per treatment group was calculated to exceed a statistical power of 0.90 under the null hypothesis stating that there was no difference in the treatment effect on the primary outcome measure for the two treatments under investigation (significance level 0.05, two-sided exact Fisher test, nQuery Advisor® 3.0; Statistical Solutions, Saugus, MA). The local ethics committee required an interim evaluation of the extent of surgery required to achieve correction of the deformity after a minimum of 12 feet was assigned to each group. This number resulted in a power of 0.60 under the assumptions mentioned. Recruitment of new patients stopped in 2003 when that interim evaluation indicated a higher number of surgical procedures other than simple tenotomies were being performed in the traditional treatment group. In accordance with the judgment of the local ethics committee, it was considered unethical to use this method with new patients. (Although enrollment was stopped, we continue to follow the patients to document long-term outcome.) Nine patients were assigned to the Ponseti group (N = 9, six females, three males; n = 12 clubfeet). The traditional therapy group consisted of 10 patients (N = 10, three females, seven males; n = 16 clubfeet). None of the clubfeet in either group fell into the category Ponseti et al. termed “complex” [26]. Clubfeet in both groups were of comparable severity at the start of the treatment as documented by the scores of Pirani et al. [23].
Treatment of patients in the Ponseti group followed the regimen described by Ponseti [24]. Manipulative therapy and cast applications were performed on an outpatient basis with weekly changes of toe to groin plaster casts. In all cases, a persistent hindfoot equinus made a tenotomy of the tendo-Achilles necessary. For the tenotomies, patients and their caregivers were admitted to the hospital for 3 days. Tenotomies were performed with the patients under general anesthesia. This is a deviation from the original description of the Ponseti method in which tenotomies are performed as an outpatient under local anesthesia. Treatment guidelines at our institution require any surgical intervention, including percutaneous tenotomies, in infants younger than 18 weeks to be performed under general anesthesia. The local pediatric anesthesiologist required the infants to be admitted the day before surgery and to be discharged the day after surgery. The tenotomies were performed according to the method described by Ponseti using a No. 15 blade, and no neurovascular compromise was experienced. After tenotomy of the tendo-Achilles, plaster casts were applied for 3 weeks. Orthotic management for abduction and external rotation of the feet started once correction of the deformity was achieved and consisted of a Tibax bar (Basko Healthcare, Vienna, Austria) with GloboPed shoes (Bauernfeind, Remscheid, Germany). The rotation was set to 70° external rotation for clubfeet and to 45° external rotation for the normal foot in unilateral cases. At the beginning, the splint was applied 24 hours a day. When the patient was 6 months old, the splint was removed in the morning and in the afternoon for 3 hours to allow for unrestricted sitting and crawling. Once the patients began to stand up and walk, the splint was applied at night only. The orthotic device was discontinued when the patient was 24 months old. The duration of 24 months represents the lower range for the duration of orthotic treatment, which originally was described to vary between 2 and 4 years [24]. Until this time, none of the patients experienced pressure sores. At the time the devices were discontinued, all patients were prescribed custom molded foot shoes for daytime use. The shoes had soft insoles with a heel counter, a moderate flange at the lateral aspect of the cuboid, and another flange at the medial aspect of the first metatarsal head. These insoles were intended to apply a 3-point-force to maintain correction.
Patients in the traditional group underwent similar manipulative therapy as those in the Ponseti group and wore plaster casts with weekly changes until the age of 6 to 8 months. In all cases, we corrected residual deformities by posteromedial release. Through a Cincinnati-type skin incision [8], a posteromedial release was performed following the technique described by Carroll et al. to correct residual deformities (average age at the time of surgery, 7.6 months; range, 5.5–11.4 months [4]; surgery was delayed in four patients as a result of respiratory infections). After correction, the talonavicular and the talocalcaneal joints were pinned using smooth Kirschner wires, which were not buried, and toe to groin plaster casts were applied. Prophylactic antibiotics were given intravenously for 5 days. The average hospital stay was 6 days (range, 5–8 days). There were no neurovascular complications or skin problems in any of the cases. Kirschner wires were removed 4 weeks after surgery. Six weeks after surgery, the plaster casts were removed and rigid knee-ankle-foot orthoses were provided for nighttime splinting up to the age of 36 months. Molded foot orthoses were prescribed once the patients were able to stand and walk.
One senior consultant orthopaedic surgeon (EBZ) applied all plaster casts, another senior consultant (WEL) performed all surgical interventions other than the simple tenotomies, and a third senior consultant (GS) evaluated the patients at 6 months for the necessity of surgical intervention and for the final assessment. After removal of the final cast (3 weeks after the tenotomy for the Ponseti group and 6 weeks after surgery for the traditional treatment group), patients were seen every 3 months. At this time, the fit of the orthotic device was evaluated and the clubfeet were examined by one of the authors (EBZ) for any sign of relapse.
Two patients were not treated per protocol. In the first case, the parents opted out of the Ponseti treatment 5 weeks after tenotomy of the tendo-Achilles and 2 weeks after fitting the orthosis, owing to the baby’s considerable discomfort wearing the orthosis during the night. In this case, the initial Pirani score for the foot was 6. When the final cast after tenotomy of the tendo-Achilles was removed, the midfoot and hindfoot contractures were corrected. Two weeks later, we observed a relapse of the midfoot and hindfoot contractures. At this time, the parents opted out of the Ponseti treatment. For a second infant in the Ponseti group, a clubfoot with an initial score of 6 according to Pirani et al. [23] was improved by casting and tenotomy of the tendo-Achilles. Again, after removal of the final cast after tenotomy of the tendo-Achilles, the midfoot and hindfoot contractures were corrected. Seven weeks after the tenotomy, a relapse of the hindfoot contracture was evident. As a consequence, three more casts were applied and the passive dorsiflexion of the ankle was improved to neutral position. Because of a relapse of the equinus in this foot, we recommended performing a second tenotomy of the tendo-Achilles. At this time, the parents decided to change the treatment plan to the traditional treatment protocol with posteromedial release. Both patients were treated with plaster casts to the age of 7.7 and 8.5 months, respectively, when posteromedial release was performed. According to the intention-to-treat protocol, these two patients (two feet) remained assigned to the Ponseti group for further assessments and analysis.
The FRS of Laaveg and Ponseti was chosen as the primary outcome measure to assess foot function [21]. Angular motion measurements were obtained using a plastic handheld goniometer. To evaluate the health status of the children at an average age of 3.5 years, the parent-reported Pediatric Health Assessment was used (PODCI, Pediatric Outcomes Data Collection Instrument, Pediatric Orthopaedic Society of North America) [10]. The FRS and PODCI were evaluated at a mean of 3.5 years of age (range, 3.3–3.8 years). From the PODCI, we selected four core scales (transfer and basic mobility, sports and physical functioning, pain and comfort, happiness) and the global function scale, which combines all the different dimensions of the instrument. A physician (GS) not involved in the treatment of these patients performed the assessments.
Additional data recorded were the Pirani scores and selected angles measured from plain radiographs using a handheld goniometer [23]. The Pirani score was used to document severity of the clubfeet at the start of the treatments and after six to eight plaster casts to provide information on the condition of the feet after the first weeks of treatment. Radiographs of the feet were taken after 6 to 8 weeks of treatment and at the last evaluation and were evaluated for the lateral tibiocalcaneal angle at maximum dorsiflexion, anteroposterior talocalcaneal angle, and lateral talocalcaneal angle by one of the authors (GS).
For both groups, descriptive statistics were calculated for the FRS total scores and all FRS categories, the PODCI and its subscales, the Pirani scores and its items, and the radiographic measures mentioned. We compared the FRS total scores and its categories, the PODCI and its subscales, the Pirani scores and its items, and the radiographic measures mentioned between the two groups using nonparametric tests (Mann-Whitney U-tests). After a Bonferroni adjustment for multiple testing, the significance level was defined to be < 0.0004 for single outcome measures. Statistical analysis was performed using Statistica 6.0 for Windows (StatSoft, Tulsa, OK).
Results
Pirani scores taken to document initial severity of the clubfeet showed no group differences at the start of the trial (Table 1). All 19 patients were followed up until the final evaluation.
Table 1.
Pirani scores before and after six to eight plaster casts
| Items | Start of the treatment | After the sixth to eighth plaster cast | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Traditional treatment group | Ponseti group | p Value | Traditional treatment group | Ponseti group | p Value | |||||
| (n = 16) | (n = 12) | (n = 16) | (n = 12) | |||||||
| Median | 10th/90th percentile | Median | 10th/90th percentile | Median | 10th/90th percentile | Median | 10th/90th percentile | |||
| Clinical sign | ||||||||||
| Severity of the posterior crease (PC) | 0.5 | 0.5/1.0 | 1.0 | 0.5/1.0 | 0.4862 | 0.5 | 0.1/1.0 | 0.5 | 0.0/1.0 | 0.8526 |
| Emptiness of the heel (EH) | 1.0 | 0.5/1.0 | 1.0 | 0.5/1.0 | 0.9260 | 0.5 | 0.5/1.0 | 0.5 | 0.0/1.0 | 0.4165 |
| Rigidity of the equinus (RE) | 1.0 | 0.5/1.0 | 0.8 | 0.5/1.0 | 0.7805 | 0.5 | 0.0/1.0 | 0.5 | 0.0/1.0 | 0.9629 |
| Curvature of the lateral border of the foot (CLB) | 0.8 | 0.5/1.0 | 1.0 | 0.5/1.0 | 0.7103 | 0.0 | 0.0/0.5 | 0.0 | 0.0/0.5 | 0.3531 |
| Severity of the medial crease (MC) | 0.5 | 0.0/1.0 | 0.8 | 0.0/1.0 | 0.4576 | 0.0 | 0.0/0.5 | 0.0 | 0.0/0.0 | 0.5774 |
| Position of the lateral part of the head of the talus (LHT) | 1.0 | 0.5/1.0 | 1.0 | 0.5/1.0 | 0.5157 | 0.0 | 0.0/0.5 | 0.0 | 0.0/0.5 | 0.8892 |
| Contracture scores | ||||||||||
| Hindfoot contracture score (HFCS) | 2.0 | 1.5/3.0 | 2.3 | 1.5/3.0 | 0.8164 | 1.5 | 0.5/3.0 | 1.3 | 0.0/3.0 | 0.7628 |
| Midfoot contracture score (MFCS) | 2.0 | 1.5/3.0 | 2.8 | 1.0/3.0 | 0.7452 | 0.0 | 0.0/1.5 | 0.0 | 0.0/0.5 | 0.5661 |
| Total score (TS) | 4.0 | 3.5/6.0 | 5.0 | 2.5/6.0 | 0.7805 | 1.5 | 0.5/3.5 | 1.3 | 0.0/3.5 | 0.4862 |
HFCS = the hind foot contracture score is the sum of the clinical signs PC, EH, and RE; MFCS = the midfoot contracture score is the sum of the clinical signs CLB, MC, and LHT; TS = the total score is the sum of the contracture scores HFCS and MFCS.
When foot function was evaluated at the age of 3.5 years, patients in the Ponseti group scored higher in the FRS total score (Table 2). None of the patients experienced foot pain, and all feet had a plantigrade position when standing. The FRS category for gait was comparable in both groups. For the passive motion category of the FRS, passive maximal dorsiflexion and total anterior inversion-eversion mobility scores were higher (p = 0.0061; p = 0.0258, respectively) in the Ponseti group.
Table 2.
Functional Rating System scores
| Category | Traditional treatment group | Ponseti group | |||
|---|---|---|---|---|---|
| (n = 16) | (n = 12) | ||||
| Median | 10th/90th percentile | Median | 10th/90th percentile | p Value | |
| Satisfaction (best at 20 points) | 16 | 16/20 | 20 | 16/20 | 0.0327 |
| Function (best at 20 points) | 20 | 20/20 | 20 | 20/20 | 0.7143 |
| Pain (best at 30 points) | 30 | 24/30 | 30 | 24/30 | 0.3797 |
| Position of the heel when standing (best at 10 points) | 10 | 5/10 | 10 | 10/10 | 0.6424 |
| Passive motion | |||||
| Dorsiflexion (best at 5 points) | 2 | 1/3 | 4 | 1/5 | 0.0061 |
| Varus-valgus motion of the heel (best at 3 points) | 1 | 1/2 | 2 | 1/2 | 0.1144 |
| Anterior inversion-eversion of foot (best at 2 points) | 1 | 1/1 | 1.5 | 1/2 | 0.0258 |
| Gait (best at 10 points) | 8 | 0/10 | 9 | 8/10 | 0.2854 |
| Total score (best at 100 points) | 84 | 74/93 | 94.5 | 76/98 | 0.0021 |
Satisfaction was scored from “very satisfied” to “very unsatisfied” in five intervals; function of the foot in daily living was scored from no limitation of activities to limitation of walking in five intervals; pain was scored from “never painful” to “painful during walking” in five intervals; position of the heel scored the amount of varus of the heel from “0° to some heel valgus” to “heel varus greater than 10°” in four intervals; dorsiflexion scored one point per 5°; varus-valgus motion of the heel scored one point per 10°; anterior inversion-eversion of foot scored one point per 25°; gait was evaluated for normal appearance, the ability to to-walk and heel-walk, and for limping.
When the health status for children with orthopaedic problems was assessed at the age of 3.5 years using the PODCI, core scales for transfer and basic mobility, sports and physical functioning, pain and comfort, happiness, and the global function scale showed scores between 92 and 100 in which a score of 100 represents best mobility, function and least pain, etc (Table 3). The radiographic variables were similar between the groups (Table 4).
Table 3.
The Pediatric Outcomes Data Collection Instrument (PODCI) subscales
| PODCI scales | Traditional treatment group | Ponseti group | p Value | ||
|---|---|---|---|---|---|
| (n = 16) | (n = 12) | ||||
| Median | 10th/90th percentile | Median | 10th/90th percentile | ||
| Transfer and basic mobility | 98.5 | 84.8/100 | 93.9 | 78.8/100 | 0.1858 |
| Sports and physical functioning | 93.8 | 81.7/100 | 92.6 | 74.0/100 | 0.8164 |
| Pain and comfort | 100.0 | 41.1/100 | 100.0 | 77.8/100 | 0.8892 |
| Happiness | 91.7 | 62.5/100 | 100.0 | 83.3/100 | 0.2941 |
| Global function | 94.8 | 80.4/97.9 | 94.4 | 79.9/99.2 | 0.9629 |
PODCI scores of 0 represent the most disability, scores of 100 represent least disability; transfer and basic mobility scale: measures difficulty experienced in performing routine motion and motor activities in daily activities; sports and physical functioning scale: measures difficulty or limitations encountered in participating in more active activities or sports; pain and comfort scale: measures the level of pain experienced during the past week; happiness scale: measures overall satisfaction with personal looks and sense of similarity to friends and others of own age; global functioning scale: a general combined scale calculated from the first four scales listed above.
Table 4.
Radiographic outcome measures*
| Angles | Traditional treatment group | Ponseti group | |||
|---|---|---|---|---|---|
| (n = 16) | (n = 12) | ||||
| Median* | 10th/90th percentile | Median* | 10th/90th percentile | p Value | |
| Lateral tibiocalcaneal angle | |||||
| at 6 to 8 weeks | 101 | 74/120 | 100 | 84/116 | 0.8501 |
| at followup (3.5 years of age) | 83 | 70/92 | 79 | 68/86 | 0.0946 |
| Anteroposterior talocalcaneal angle | |||||
| at 6 to 8 weeks | 28 | 12/40 | 24 | 10/28 | 0.1858 |
| at followup (3.5 years of age) | 30 | 24/40 | 28 | 18/42 | 0.1896 |
| Lateral talocalcaneal angle | |||||
| at 6 to 8 weeks | 26 | 2/46 | 36 | 15/48 | 0.1858 |
| at followup (3.5 years of age) | 29 | 19/38 | 31 | 24/42 | 0.4105 |
* In degrees.
When we compared the per protocol analysis (traditional treatment group: N = 10 patients; n = 16 clubfeet; Ponseti group: N = 7 patients; n = 10 clubfeet) with the intention-to-treat analysis, only some results changed. For the per protocol analysis, the score for passive dorsiflexion of the heel (FRS) was higher (p = 0.0001) in the Ponseti group than in the traditional treatment group (median, 4.0; percentiles, 10th 3.0 and 90th 5.0 versus median, 2.0; percentiles, 10th 1.0 and 90th 3.0, respectively). Also, the FRS total score was higher (p = 0.0001) in the Ponseti group than in the traditional treatment group (median, 95; percentiles, 10th 92 and 90th 98 versus median, 84; percentiles, 10th 74 and 90th 93, respectively). Group comparisons for all other FRS categories and for the PODCI scales revealed similar results as the comparisons performed in the intention-to-treat analysis (traditional treatment group: n = 10 patients, n = 16 clubfeet; Ponseti group N = 9 patients, n = 12 clubfeet).
Discussion
The Ponseti technique has become the standard for treatment of congenital clubfoot in the last 2 decades [12]. For almost 3 decades at our institution, the deformity was treated by initial casting and posteromedial release to correct residual deformities at the age of 6 to 8 months. Before changing treatment standards at our institution, we decided to perform a prospective, controlled trial to compare the Ponseti method with our traditional treatment method. We intended to evaluate foot function and health status of children with orthopaedic problems at the age of 3.5 years.
This study has several limitations. Because the rate of surgery was higher for the traditional therapy group, patient acquisition was terminated after the preliminary evaluation. This led to small collectives and to interventions at rates that might not reflect the rates observable in larger cohorts. In the Ponseti group, tenotomies of the tendo-Achilles were performed more frequently than reported so far (100% versus 78% to 98%) [21, 29]. Also, when treated per protocol, none of the patients in the Ponseti group required surgery. This rate was reported to vary from 2% to greater than 23% [2, 6, 15, 18, 22, 29]. Because two of our parents opted out of the Ponseti group and favored surgical treatment, one could argue that 17% of the patients in the Ponseti group required a posteromedial release. In contrast, Herzenberg et al. reported that 97% of the clubfeet could be managed with manipulation, casting, and tenotomy of the tendo-Achilles [19]. The wide range of surgery rates indicates modifications to the original technique and local factors might have a considerable impact on the success of the Ponseti method. The aim of the trial was to evaluate the Ponseti method when used in our specific local setting. Splinting in patients in the Ponseti group was terminated at 24 months, which is the shortest duration of splint application reported by Ponseti [24]. Similar to a report by Dobbs et al. we performed tenotomies of the tendo-Achilles with the patients under general anesthesia, which was required to comply with our local treatment guidelines [13]. Treatment under general anesthesia and short duration of orthotic management are deviations from the Ponseti protocol [24]. All patients in the traditional treatment group required surgery at the age of 6 to 8 months. Before the start of this trial, the traditional treatment protocol led to surgery in 72% of the cases at our institution (unpublished data). This supports previous reports regarding the importance of tenotomy of the tendo-Achilles for short-term success of the Ponseti method when a residual equinus is present after the first weeks of manipulation and casting [14, 28].
When evaluating foot function 3.5 years after treatment, we observed differences for several categories of the FRS of Laaveg and Ponseti [21]. The category “satisfaction” describing the level of caregiver contentment suggested parents of patients in the Ponseti group were “very satisfied” with the short-term outcome, whereas parents of patients in the traditional treatment group were “satisfied.” Laaveg and Ponseti evaluated 104 clubfeet and reported 72% “very satisfied” patients, 19% “satisfied,” and 4% “not satisfied” with the long-term outcome [21]. Because the FRS scores are described to correlate with age, the initial high scores for the level of contentment in our study must be interpreted with caution [17]. However, the less invasive character of Ponseti management without the need for wound management and the shorter hospital stay seem to contribute to parental satisfaction. Brace intolerance, a contributing cause to limited parent compliance and possibly early recurrence, was not a substantial source of concern for the caregivers [18]. The passive mobility category of the FRS revealed better mobility of the feet in dorsiflexion and in inversion-eversion for the Ponseti group with scores similar to those reported by Laaveg and Ponseti [21]. This finding was accentuated even more when groups were evaluated per protocol. When interpreting the FRS total scores according to the classification described by Laaveg and Ponseti [21], feet function could be classified as “good” for the traditional treatment group (84 of 100) and “excellent” for the Ponseti group, respectively (94 of 100). In a study evaluating two sequential cohorts of patients with clubfeet [20], a more conservative treatment protocol also led to better results for the FRS of Laaveg and Ponseti when compared with the outcome of posteromedial release. In addition to the retrospective design of the study, it provides only fair evidence for the quality of the Ponseti method because limited posterior release was performed at the time of the tenotomy of the tendo-Achilles.
Evaluating the health status of children with orthopaedic problems, PODCI core scales were similar for both groups at 3.5 years of age. Although this instrument has not been used regularly to assess outcome of clubfoot treatment, we believe it provides a feasible tool for continued evaluation of our cohorts. Regarding the short-term evaluation, there were high values in all dimensions for both study groups. Radiographic measures documented changes toward normal at followup and were comparable for both groups. Angular measurements were within the range reported by other groups [16, 25, 30].
The data presented here compare short-term outcomes of the Ponseti method with a traditional treatment regimen for congenital clubfeet in a prospective, randomized trial. The results reveal good to excellent outcomes for both groups. The Ponseti method resulted in better parental satisfaction and better passive mobility of the clubfeet. The number of cases included in this trial is small and therefore its external validity must be interpreted with caution. However, at our clinic, we now follow up our participants in an open trial to evaluate midterm and long-term outcomes. Considering all aspects of the Ponseti method, particularly the more conservative approach and lower complication rate as reported in the literature [1, 5, 9, 11, 32], we changed the standard treatment of congenital clubfeet at our institution to the Ponseti method of treatment.
Acknowledgments
We thank Lutz Leistritz, PhD, from the Institute of Medical Statistics, Computer Sciences and Documentation, University of Jena, for statistical advice.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Atar D, Lehman WB, Grant AD. Complications in clubfoot surgery. Orthop Rev. 1991;20:233–239. [PubMed]
- 2.Bor N, Herzenberg JE, Frick SL. Ponseti management of clubfoot in older infants. Clin Orthop Relat Res. 2006;444:224–228. [DOI] [PubMed]
- 3.Bösch J. [Biological fundamentals of conservative therapy of clubfoot] [in German]. Z Orthop Ihre Grenzgeb. 1954;85:429–448. [PubMed]
- 4.Carroll NC, McMurtry R, Leete SF. The pathoanatomy of congenital clubfoot. Orthop Clin North Am. 1978;9:225–232. [PubMed]
- 5.Changulani M, Garg N, Bruce CE. Neurovascular complications following percutaneous tendoachillis tenotomy for congenital idiopathic clubfoot. Arch Orthop Trauma Surg. 2007;127:429–430. [DOI] [PubMed]
- 6.Changulani M, Garg NK, Rajagopal TS, Bass A, Nayagam SN, Sampath J, Bruce CE. Treatment of idiopathic club foot using the Ponseti method: initial experience. J Bone Joint Surg Br. 2006;88:1385–1387. [DOI] [PubMed]
- 7.Cooper DM, Dietz FR. Treatment of idiopathic clubfoot: a thirty-year follow-up note. J Bone Joint Surg Am. 1995;77:1477–1489. [DOI] [PubMed]
- 8.Crawford AH, Marxen JL, Osterfeld DL. The Cincinnati incision: a comprehensive approach for surgical-procedures of the foot and ankle in childhood. J Bone Joint Surg Am. 1982;64:1355–1358. [PubMed]
- 9.Cummings RJ, Bashore CJ, Bookout CB, Elliott MJ. Avascular necrosis of the talus after McKay clubfoot release for idiopathic congenital clubfoot. J Pediatr Orthop. 2001;21:221–224. [DOI] [PubMed]
- 10.Daltroy LH, Liang MH, Fossel AH, Goldberg MJ. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. Pediatric Outcomes Instrument Development Group. Pediatric Orthopaedic Society of North America. J Pediatr Orthop. 1998;18:561–571. [DOI] [PubMed]
- 11.Dobbs MB, Gordon JE, Walton T, Schoenecker PL. Bleeding complications following percutaneous tendoachilles tenotomy in the treatment of clubfoot deformity. J Pediatr Orthop. 2004;24:353–357. [DOI] [PubMed]
- 12.Dobbs MB, Nunley R, Schoenecker PL. Long-term follow-up of patients with clubfeet treated with extensive soft-tissue release. J Bone Joint Surg Am. 2006;88:986–996. [DOI] [PubMed]
- 13.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86:22–27. [DOI] [PubMed]
- 14.Dyer PJ, Davis N. The role of the Pirani scoring system in the management of club foot by the Ponseti method. J Bone Joint Surg Br. 2006;88:1082–1084. [DOI] [PubMed]
- 15.Eberhardt O, Schelling K, Parsch K, Wirth T. [Treatment of congenital clubfoot with the Ponseti method] [in German]. Zeitschrift fur Orthopadie und Ihre Grenzgebiete. 2006;144:497–501. [DOI] [PubMed]
- 16.Fridman MW, de Almeida Fialho HS. The role of radiographic measurements in the evaluation of congenital clubfoot surgical results. Skeletal Radiol. 2007;36:129–138. [DOI] [PubMed]
- 17.Haasbeek JF, Wright JG. A comparison of the long-term results of posterior and comprehensive release in the treatment of clubfoot. J Pediatr Orthop. 1997;17:29–35. [DOI] [PubMed]
- 18.Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007;89:487–493. [DOI] [PubMed]
- 19.Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop. 2002;22:517–521. [DOI] [PubMed]
- 20.Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am. 2003;85:1286–1294. [DOI] [PubMed]
- 21.Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am. 1980;62:23–31. [PubMed]
- 22.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113:376–380. [DOI] [PubMed]
- 23.Pirani S, Outerbridge H, Moran M, Sawatsky B. A method of evaluating the virgin clubfoot with substantial inter-observer reliability. In the Proceedings of the Pediatric Orthopaedic Society of North America (POSNA), Vol. 71. Miami, FL: April 30–May 4, 1995.
- 24.Ponseti IV. Congenital Clubfoot. Fundamentals of Treatment. 1st Ed. Oxford, United Kingdom: Oxford University Press Inc; 1996.
- 25.Ponseti IV, El-Khoury GY, Ippolito E, Weinstein SL. A radiographic study of skeletal deformities in treated clubfeet. Clin Orthop Relat Res. 1981;160:30–42. [PubMed]
- 26.Ponseti IV, Zhivkov M, Davis N, Sinclair M, Dobbs MB, Morcuende JA. Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res. 2006;451:171–176. [DOI] [PubMed]
- 27.Scher DM. The Ponseti method for treatment of congenital club foot. Curr Opin Pediatr. 2006;18:22–25. [DOI] [PubMed]
- 28.Scher DM, Feldman DS, van Bosse HJ, Sala DA, Lehman WB. Predicting the need for tenotomy in the Ponseti method for correction of clubfeet. J Pediatr Orthop. 2004;24:349–352. [DOI] [PubMed]
- 29.Segev E, Keret D, Lokiec F, Yavor A, Wientroub S, Ezra E, Hayek S. Early experience with the Ponseti method for the treatment of congenital idiopathic clubfoot. Isr Med Assoc J. 2005;7:307–310. [PubMed]
- 30.Simons GW. A standardized method for the radiographic evaluation of clubfeet. Clin Orthop Relat Res. 1978;135:107–118. [PubMed]
- 31.Turco VJ. Resistant congenital club foot:one-stage posteromedial release with internal fixation: a follow-up report of a fifteen-year experience. J Bone Joint Surg Am. 1979;61:805–814. [PubMed]
- 32.Weseley MS, Barenfeld PA, Barrett N. Complications of the treatment of clubfoot. Clin Orthop Relat Res. 1972;84:93–96. [DOI] [PubMed]