Abstract
Previous projections of total joint replacement (TJR) volume have not quantified demand for TJR surgery in young patients (< 65 years old). We developed projections for demand of TJR for the young patient population in the United States. The Nationwide Inpatient Sample was used to identify primary and revision TJRs between 1993 and 2006, as a function of age, gender, race, and census region. Surgery prevalence was modeled using Poisson regression, allowing for different rates for each population subgroup over time. If the historical growth trajectory of joint replacement surgeries continues, demand for primary THA and TKA among patients less than 65 years old was projected to exceed 50% of THA and TKA patients of all ages by 2011 and 2016, respectively. Patients less than 65 years old were projected to exceed 50% of the revision TKA patient population by 2011. This study underscores the major contribution that young patients may play in the future demand for primary and revision TJR surgery.
Level of Evidence: Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The aging of the Baby Boom generation, who will start reaching 65 years old in 2011, is a factor in the increased future demand for joint replacement surgery in the United States. Total hip arthroplasty was originally conceived by Sir John Charnley as a procedure for elderly patients of low activity levels [2]. Over time, the indications for lower extremity joint arthroplasty have expanded to include both younger and more active patients. Indeed, over the past decade, the incidence of total joint replacement (TJR) has increased not only in older (> 65 years) but also in younger patients (< 65 years) [7]. The implication of patient age-related differences in future demand for TJR has remained unexplored. Since TJR was primarily intended to treat the elderly patient population, it is unclear if the incidence of these procedures in younger patients would exceed that in older patients in the future.
Historically, young patients have been considered at higher risk for revision due to their higher activity level relative to elderly patients [8]. “Premium” implant technologies, such as hard-on-hard bearings and hip resurfacing, have been introduced to address the increased activity and need for improved implant longevity in younger patients. However, these bearings are associated with higher costs and questions regarding their cost-effectiveness for the elderly patient population have been raised [1]. Previous projections by our group focused on estimating the total nationwide demand for primary and revision TJR [6], and not quantified the relative future size of the young TJR population in the United States that may benefit from premium implants. Due to the likelihood that the young patient population will utilize more costly premium bearings, the future size of this patient group could have a substantial impact on the healthcare costs associated with TJR.
We therefore developed nationwide projections for primary and revision TJR for the young patient population in the United States. First, we evaluated the historical changes in demand for primary and revision TJR in the younger and older patient populations. We also tested the hypothesis that patients younger than 65 years will represent the majority (> 50%) of the anticipated demand for primary and revision TJR in the United States between 2010 and 2030. We also asked whether current trends are advancing according to earlier expectations.
Methods and Materials
We used the Nationwide Inpatient Sample (NIS) to identify primary and revision arthroplasty procedures performed between 1993 and 2006. The NIS is an annual, statistically valid survey of ~ 1000 hospitals conducted by the Federal Healthcare Cost and Utilization Project (HCUP). HCUP recommends using 1993 and later years for longitudinal analyses, that being the period in the NIS program with a consistent sampling design. NIS contains approximately 20% of the inpatient hospitalizations performed in the United States, regardless of payment source. Because of the large size of the database, the NIS is particularly well-suited for epidemiological studies of procedures primary and revision TJR in the national population. We also employed statistical trend files, recently published by HCUP [3], to standardize the treatment of the data for longitudinal analysis of historical trends for inpatient healthcare utilization in the United States.
Patient demographics (eg, age, gender, race/ethnicity) are captured in the NIS. Disease diagnoses and surgical procedures performed (if any) were recorded using the 9th Revision of the International Classification of Diseases (ICD-9-CM). We used ICD-9-CM codes 81.51 and 81.53 for primary and revision total hip arthroplasty (THA); 81.54 and 81.55 were used for primary and revision total knee arthroplasty (TKA). In October 2005, new ICD-9-CM codes were introduced for revisions (00.70–00.73 for revision THA and 00.80–00.84 for revision TKA), which were incorporated into our analysis.
The incidence of primary and revision THA/TKA surgeries was calculated using NIS between 1993 and 2006 for population subgroups in the United States as a function of age, gender, race, and census region. The size of the population subgroups was determined from the Census Bureau’s census data in 1990 and 2000 and intracensus estimates [9]. The prevalence of surgery was modeled using Poisson regression allowing for different rates for each population subgroup, as reported previously [6]. Briefly, the multivariate Poisson model allows differences in prevalence between population subgroups, as well as changes over time, to be assessed. The future size of each population subgroup was obtained from the population projection data reported by the Census Bureau. These population projections take into account the future mortality and increased life expectancy for the oldest population groups. National TJR projections were obtained by summing the projections for each subgroup, for which both the population and the prevalence of surgery were modeled to vary over time (“variable rate” approach). A conservative estimate of the TJR projections was also determined by assuming a constant prevalence of surgery, while accounting only for population changes over time (“constant rate” approach). Unlike the variable rate approach where the future prevalence of surgery was modeled to change with time, the constant rate approach assumed that the future prevalence of surgery (i.e., number of procedures per 100,000 population in each demographic subgroup) did not change and remained constant based on the average historical prevalence between 2004 and 2006. Independent models were used for primary and revision hip and knee arthroplasty. To evaluate the nationwide projections for primary and revision TJR for the young patient population, the number and proportion of procedures, along with 95% confidence intervals, were further stratified by patients aged under and over 65 years. The confidence intervals for the proportion of procedures was estimated from the ratio of the confidence intervals for the procedure counts stratified by the specific age group and the entire population.
To evaluate whether TJR trends are advancing according to earlier estimates [6], which were derived from 1990 to 2003 data, we compared the previous projections against TJR utilization data obtained from the NIS within the three most recent years (2004 to 2006). The previous projections were also compared against the current projections to assess changes in the estimated trends.
Results
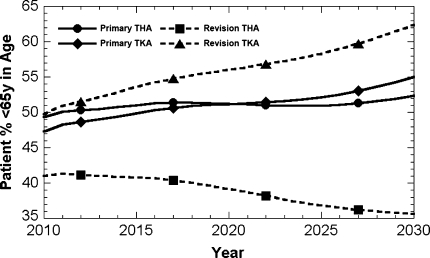
The relative size of the younger patient population grew between 1993 and 2006, especially for TKA. In 1993, 32% of primary or revision THAs and 25% to 27% of primary or revision TKAs were performed in patients less than 65 years old. In 2006, the most recent year of NIS data available, the relative size of the young patient population had increased to 40% to 46% of primary and revision TJR recipients (Table 1). Substantial increases in the utilization of primary hip as well as primary and revision knee replacement surgery among patients under 65 years old were predicted over time based on the variable rate approach (Fig. 1) (Tables 1–3). A similar trend was not projected for revision THA, for which younger patients were not modeled to increase substantially in relative prevalence over time.
Table 1.
Number of primary and revision TJR procedures in patients younger than 65 years old in 2006 (NIS Data)
| Procedure | Age | Total | Percentage younger than 65 years | ||
|---|---|---|---|---|---|
| < 45 years | 45 to 54 years | 55 to 64 years | |||
| Primary THA | 14,300 (12,800–15,900) | 34,300 (31,100–37,600) | 56,300 (51,100–61,500) | 229,900 (211,000–248,800) | 46% (45%–46.3%) |
| Revision THA | 2,400 (2,000–2,700) | 5,000 (4,300–5,700) | 7,500 (6,500–8,400) | 37,200 (33,300–41,200) | 40% (34.3%–41%) |
| Primary TKA | 9,900 (8,900–11,000) | 59,100 (54,100–64,100) | 147,100 (135,100–159,100) | 524,600 (484,000–565,100) | 41% (40.9%–41.5%) |
| Revision TKA | 1,800 (1,400–2,100) | 6,400 (5,600–7,200) | 12,100 (10,700–13,500) | 46,400 (41,600–51,300) | 44% (42.5%–44.4%) |
Fig. 1.
The projected relative proportion of the younger patient population (< 65 y) for primary and revision total joint replacement between 2010 and 2030 is shown.
Table 3.
Projected future demand of primary and revision TJR procedures in patients less than 65 years old by 2030
| Procedure | Variable rate (Poisson regression) | Constant rate (2004–2006 average) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| < 45 y | 45–54 y | 55–64 y | Total | % < 65 y | < 45 y | 45–54 y | 55–64 y | Total | % < 65 y | |
| Primary THA | 46,900 (39,100–56,300) | 202,500 (174,400–235,900) | 217,700 (190,700–249,300) | 891,800 (774,000–1,030,200) | 52% (52.2%–52.6%) | 15,600 (12,200–19,000) | 31,000 (25,100–36,800) | 62,800 (51,500–74,100) | 345,700 (285,300–406,000) | 32% (31.1%–32%) |
| Revision THA | 3,200 (2,200–4,400) | 13,200 (10,100–17,400) | 16,100 (12,500–20,600) | 91,400 (70,800–117,600) | 36% (35.1%–36.1%) | 2,700 (1,800–3,700) | 4,600 (3,300–6,000) | 8,500 (6,200–10,800) | 59,000 (43,600–74,300) | 27% (25.9%–27.5%) |
| Primary TKA | 95,200 (73,900–122,900) | 994,100 (856,000–1,158,800) | 1,300,200 (1,149,400–1,477,500) | 4,344,900 (3,797,600–4,994,900) | 55% (54.8%–55.2%) | 9,800 (7,600–12,000) | 51,500 (42,900–60,100) | 162,300 (137,300–187,400) | 792,200 (668,700–915,700) | 28% (28.1%–28.3%) |
| Revision TKA | 16,300 (11,000–24,200) | 102,300 (77,000–137,700) | 93,000 (72,700–120,800) | 339,000 (258,500–451,100) | 62% (62.2%–62.7%) | 1,700 (1,000–2,400) | 5,300 (3,800–6,800) | 12,500 (9,400–15,600) | 64,600 (47,900–81,100) | 30% (29.7%–30.5%) |
The demand for primary THA and TKA among patients younger than 65 years was projected to exceed 50% of TJR recipients by 2011 and 2016, respectively (Fig. 1). Patients under 65 were projected to exceed 50% of the candidate population for revision TKA by 2011 (Fig. 1). By 2030, the demand for TJA by patients less than 65 years is projected to be 52% of primary THAs and 55% to 62% of primary or revision TKAs (Fig. 1) (Table 3). The future demand was projected to grow the fastest for the 45 to 54 years age category for primary TKA, which was anticipated to grow from 59,077 in 2006 to 994,104 (17 times) by 2030. For primary THA, the demand in the same age category was only projected to grow by a factor of 5.9 (2006–2030).
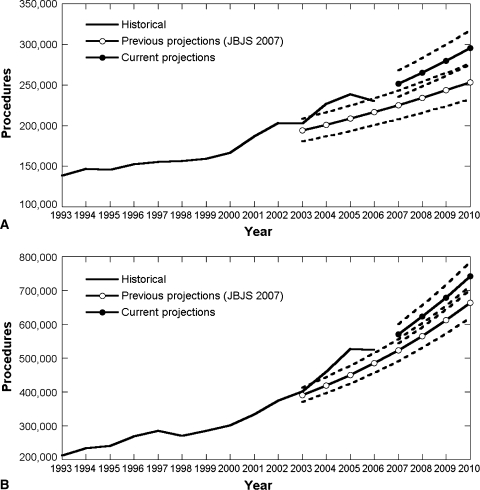
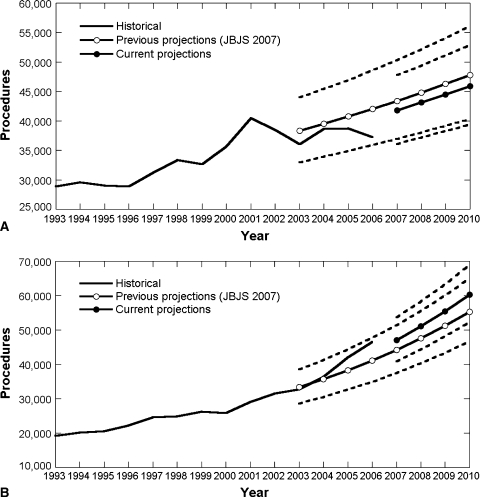
The previous projections, which used a variable rate approach, provided reasonably accurate estimates of the primary (Fig. 2A–B) and revision (Fig. 3A–B) TJR trends between 2004 and 2006, particularly for revision THA (Fig. 3A) and TKA (Fig. 3B) procedures. The historical data for revision TJR were within the 95% confidence intervals of the previous projections (Fig. 3A–B), but the previous projections underestimated the historical number of primary TJR procedures (Fig. 2A–B). As such, the updated projections were greater than the previous projections for primary TJA, but relatively unchanged for revision TJA.
Fig. 2A–B.
Historical incidence of primary total hip arthroplasty (A) and primary total knee arthroplasty (B) from 1993–2006, superimposed with previous projections [6], and the updated projections from the current study. The dotted lines represent the 95% CI for the projections.
Fig. 3A–B.
Historical incidence of revision total hip arthroplasty (A) and revision total knee arthroplasty (B) from 1993–2006, superimposed with previous projections [6], and the updated projections from the current study. The dotted lines represent the 95% CI for the projections.
Discussion
When TJR was first developed, it was primarily intended for treating the elderly patient population. However, with the increasing utilization of TJR [6], the age-related differences in the future incidence of TJR remain unexplored. This is of particular concern because more costly premium hard-on-hard bearings are intended for the younger patient population [1], which could have substantial impact on future healthcare resources. We therefore evaluated the historical changes in demand for primary and revision TJR in the younger and older patient populations. We also tested the hypothesis that patients younger than 65 years will represent the majority (> 50%) of the anticipated demand for primary and revision TJR in the United States between 2010 and 2030. We also asked whether current trends are advancing according to earlier expectations [6].
Our study has several limitations. Our projections are based on the historical growth trajectory of joint replacement surgeries, and do not take into account potential limitations in the availability of surgeons or limited economic resources by private and public payers and hospitals in the future. For example, a shortage in the number of surgeons will have a substantial influence on the actual number of procedures that are performed. We also have not incorporated the potential for future alternative technologies, such as cartilage regeneration or tissue engineering, or drug therapies that limit the progression of joint diseases, which may preempt the need for TJR. We were also unable to account for the potential impact of changes in economy, which may place additional economic burden on patients to pay substantial out-of pocket expenses for these procedures, depending on their insurance coverage. Our study also did not consider potential changes in healthcare policies, such as adoption of volume standards or regionalization of TJR to high volume centers [5], which could limit the access to care and decrease the future demand. The above economic, policy, and scientific factors cannot be readily incorporated in the statistical model. Our study was also focused on the procedural trends in the U.S.; followup research may include an analysis of trends in other countries, though the availability of historical TJR trends in other countries may be limited. Nonetheless, these limitations in no way diminish the importance of conducting and regularly updating surgical projections to help guide future research, surgeon training, and public health policy decisions. Our study also incorporated a more conservative projection, which relied only on the future changes in population growth, while maintaining current rates of adoption of TJR. Despite these limitations, our current findings are expected to have implications in the private coverage and reimbursement of joint replacement procedures in the future, as patients less than 65 years of age are not typically covered by Medicare, which today funds the majority of total joint replacement procedures in the United States.
We found the relative size of the young patient population for TJR has grown between 1993 and 2006. While 25% to 32% of primary or revision TJRs were performed in patients less than 65 years old in 1993, these proportions have increased to 40% to 46% in the most recent NIS data. The increasing trend in younger patients undergoing TJR has also been reported for different, but partly overlapping, historical periods. For example, Jain et al. reported that the proportion of primary TKA patients aged less than 60 years increased from 12.5% to 19.5% (+56%) between 1990–1993 and 1998–2000 [4]. In addition, for patients aged under 70 years, the proportion increased by 9% from 45.6% to 49.6%. Due to the difference in the stratification by age categories, we were unable to make a direct comparison with the data by Jain et al. [4]. However, our findings that the historical volume of TJR procedures in the younger patient population have been increasing is consistent with these previously reported trends.
While we previously forecasted an increase in demand for primary hip and knee replacement in 2030 by 174% and 673% [6], respectively, the current study underscores the contribution that young patients are expected to play in the future utilization of primary TJR surgery, if historical trends in prevalence continue into the future. The statistical modeling approach we have employed in the current and previous study fits a multivariate but linear Poisson regression model to the historical prevalence of TJR procedures. However, because the size of the population subgroups is free to change nonlinearly in the future based on the Census Bureau’s projection, the actual projected incidence of surgical demand is therefore not constrained to be a linear function over time. The demand for primary hip and knee arthroplasty between 2004 and 2006 generally exceeded our previous projections, which employed an identical methodology. However, we are unable to judge, based on the limited window of new data for validation, whether a more complex modeling approach would provide a more reliable forecast of demand for surgical procedures.
Our previous methodology provided a reasonable short-term forecast of the demand for revision hip and knee surgeries between 2004 and 2006. In particular, for 2006, we observed a slight decrease in the estimated number of primary THA and TKA procedures compared to 2005 (Fig. 2), but this decrease fell within the uncertainty of the estimates. Additional years of data will continue to be necessary to determine whether the historical trends will continue to apply in the future. Furthermore, if the future demand for TJR procedures is based only on the population growth with no change in the surgical prevalence (constant rate approach), then the projected increase in demand is not expected be as dramatic as previously predicted for the overall patient population and young patient population (Tables 2, 3). Furthermore, these findings have implications for the economic burden associated with TJR procedures, as younger patients often receive higher demand, more costly “premium” implants (such as hard-on-hard bearings and hip resurfacing implants), which are intended to perform better and improve implant longevity in more active patients.
Table 2.
Projected future demand of primary and revision TJR procedures in patients less than 65 years old by 2010
| Procedure | Variable rate (Poisson regression) | Constant rate (2004–2006 average) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| < 45 y | 45–54 y | 55–64 y | Total | % < 65 y | < 45 y | 45–54 y | 55–64 y | Total | % < 65 y | |
| Primary THA | 18,300 (16,500–20,200) | 49,900 (46,500–53,500) | 77,700 (73,400–82,200) | 295,600 (275,500–316,600) | 49% (49.2%–49.5%) | 14,800 (11,600–17,900) | 35,000 (28,700–41,300) | 63,300 (52,600–74,100) | 250,900 (208,500–293,200) | 45% (44.6%–45.4%) |
| Revision THA | 2,800 (2,200–3,400) | 6,500 (5,600–7,600) | 9,500 (8,300–10,700) | 45,900 (39,300–52,900) | 41% (40.9%–41.1%) | 2,600 (1,700–3,400) | 5,100 (3,700–6,500) | 8,400 (6,300–10,400) | 41,200 (30,900–51,400) | 39% (38.1%–39.7%) |
| Primary TKA | 14,900 (13,000–17,000) | 103,400 (97,200–110,000) | 232,200 (222,200–242,700) | 741,400 (701,600–783,100) | 47% (47.2%–47.4%) | 9,400 (7,400–11,500) | 57,800 (48,500–67,100) | 160,800 (137,100–184,400) | 552,600 (469,700–635,600) | 41% (41.1%–41.4%) |
| Revision TKA | 2,500 (1,900–3,200) | 10,200 (8,800–11,700) | 17,200 (15,400–19,200) | 60,300 (52,200–68,900) | 50% (49.4%–50.2%) | 1,700 (1,000–2,300) | 5,900 (4,300–7,500) | 12,200 (9,400–15,000) | 45,500 (34,300–56,600) | 43% (43%–43.7%) |
The NIS data from 2004–2006 provide a basis to judge the validity of our previous projections [6], which were derived from 1990–2003 data. During the most recent 3-year period, the incidences of primary total hip and total knee replacements were higher than the 95% confidence limits of the previous projections. The results of our current study for primary hip and knee replacement are, therefore, higher than those reported previously. On the other hand, the 2004–2006 NIS data for revision hip and knee replacement generally fell within the 95% confidence limits of the previous projections, and little difference was observed between current and previous long-term projections. The latest findings for primary TJRs continue to underscore the importance of routinely monitoring and regularly updating projections based on the latest available national data on procedure volumes.
Based on 1993–2006 NIS data, our current projections update and supercede previous modeling efforts that employed 1990–2003 NIS data [6]. In light of the current and anticipated demand for total joint replacement procedures by patients less than 65 years in age, emphasis on improving the reliability and survivorship of joint replacements continues to be a critical element in meeting future demands for joint replacement. It remains clear from the projected increases in the demand for revision surgery that efforts to minimize the national revision burden will be beneficial, especially in light of the increased resources that we project will be needed to meet the future demand for primary hip and knee arthroplasty procedures. A national TJR registry, which has been credited with decreasing the revision burden in Sweden [8], does not exist in the United States and would provide a mechanism for tracking the longitudinal performance of specific implants of all age groups in this country. Current administrative databases, such as NIS or Medicare, lack this capability. The projected demand for both primary and revision joint replacements provides a basis for cost-effectiveness studies for a United States TJR registry.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Bozic KJ, Morshed S, Silverstein MD, Rubash HE, Kahn JG. Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics. The case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am. 2006;88:706–714. [DOI] [PubMed]
- 2.Charnley J. Arthroplasty of the hip: A new operation. Lancet. 1961;I:1129–1132. [DOI] [PubMed]
- 3.Houchens RL, Elixhauser A. Using the HCUP Nationwide Inpatient Sample to Estimate Trends (Updated for 1988–2004). http://www.hcup-us.ahrq.gov/reports/methods.jsp. Accessed 24 October, 2005.
- 4.Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R, Katz JN. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005;52:3928–3933. [DOI] [PubMed]
- 5.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909–1916. [DOI] [PubMed]
- 6.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. [DOI] [PubMed]
- 7.Kurtz SM, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. [DOI] [PubMed]
- 8.Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84 Suppl 2:2–20. [DOI] [PubMed]
- 9.National Center for Health Statistics. U.S. Population Projections. http://www.census.gov/population/www/projections/stproj.html. Accessed 24 October, 2005.