Abstract
Pelvic osteotomy for middle-aged patients with hip dysplasia remains controversial. We asked whether pelvic osteotomy would yield lower Harris hip scores and survivorship in older patients than in younger patients. We compared patients younger than 50 years (n = 123) with patients 50 years or older (n = 41). At last followup, the mean Harris hip scores improved similarly in both groups: from 60 to 89 points in the older group and from 63 to 92 points in the younger group. However, in patients with bilateral surgery, the older group tended to have lower mean scores than the younger group (86 versus 93 points, respectively). Fifteen-year survivorship with a Harris hip score less than 80 points as the end point was similar in the two groups (71% in older patients and 81% in younger patients). In patients with bilateral surgery, the 15-year survivorship was lower in the older group (66% in older patients and 83% in younger patients). The data suggest eccentric rotational osteotomy for older patients can provide lasting function in most patients. However, prudent selection of patients is required for older patients with bilateral osteoarthritis.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
THA markedly improves pain, gait, and activities of daily living for most patients with osteoarthritis. However, pelvic osteotomy has been recommended for young and active patients with hip dysplasia, because THA in that population has been associated with high rates of revision THA [20]. McAuley et al. [18] reported the survivorships of THA in patients 50 years and younger were 89% at 10 years followup and 60% at 15 years followup. Wagner spherical acetabular osteotomy (survivorship 86.4% at 20 years) [22, 23], the rotational acetabular osteotomy of Ninomiya and Tagawa (excellent and good based on the Merle d’Aubigné and Postel score for 80% at 13 years) [19, 20], Ganz’ periacetabular osteotomy (excellent and good based on the Merle d’Aubigné and Postel score for 73% at 11.3 years) [5], and the eccentric rotational acetabular osteotomy of Hasegawa for hip dysplasia (final followup Harris hip score 89.0 at 7.5 years) [8] reportedly are successful in young and active patients. Osteotomy should be considered for young patients (younger than 50 years) and middle-aged patients (between 50 and 60 years) because of the high rates of revision THA needed owing to prolongation of the average lifespan.
The senior author (YH) previously reported the mean Harris hip score improved from 71 to 89 points at a mean of 7.5 years’ followup after pelvic osteotomy for 126 patients with hip dysplasia who were younger than 60 years with or without joint space narrowing [8]. Risk factors for lower survivorship were high body mass index (BMI) (≥ 24 kg/m2), concomitant valgus osteotomy, operative year between 1989 and 1992, and postoperative subluxation [9]. However, pelvic osteotomy for middle-aged patients remains controversial even in the absence of these four risk factors [20, 24, 26]. In patients having unilateral disease, the unaffected side potentially can protect or reduce the load on the affected side. However, in patients with bilateral disease, one affected side with moderate or severe pain cannot protect the other side. Clinical outcomes in patients with bilateral disease therefore may be different from those of patients with unilateral disease. If this is true, we may have to pay particular attention to the indications in patients with bilateral disease [11].
We asked (1) whether eccentric rotational acetabular osteotomy would yield lower Harris hip scores and survivorship in patients 50 years or older than in patients younger than 50 years and (2) whether hip scores and survivorship would be lower with bilateral surgery than with unilateral surgery.
Materials and Methods
We retrospectively reviewed 238 patients (279 hips) treated by eccentric rotational acetabular osteotomy between 1992 and 2002. We excluded 26 male patients (28 hips) and two patients (three hips) with neuromuscular disorders. This left 210 female patients (248 hips). We then selected 123 patients younger than 50 years who were matched to 41 patients 50 years or older with respect to BMI, preoperative joint space width, followup, ratio of bilateral/unilateral involvement, joint congruency in maximum abduction, and volume of perioperative and postoperative bleeding. We chose three control examples for one case example to raise statistical power. Matching was accomplished by creating database queries, which meant patients could be matched for a larger number of variables than would be possible with other methods. At the time of surgery, the overall mean age of the patients was 40.8 years (range, 14–59 years); the mean ages of the older and younger patients were 53 years (range, 50–59 years) and 36.7 years (range, 14–49 years), respectively (Table 1). The patients were similar in all considered factors other than age. The minimum followup was 5 years (mean, 9.2 years; range, 5–15 years). Of the 210 patients, we lost eight to followup. The study did not receive Institutional Review Board approval because our institution does not require such approval for retrospective studies.
Table 1.
Patient characteristics
| Characteristic | Group O (n = 41) | Group Y (n = 123) | p Value |
|---|---|---|---|
| Age (years) | 53.0 ± 10.3 | 36.7 ± 2.7 | < 0.0001* |
| Height (cm) | 155.1 ± 3.7 | 155.8 ± 4.9 | 0.357* |
| Weight (kg) | 55.2 ± 6.9 | 54.0 ± 7.1 | 0.341* |
| Body mass index (kg/m2) | 22.9 ± 2.5 | 22.3 ± 2.9 | 0.171* |
| Followup (years) | 8.8 ± 2.6 | 9.3 ± 2.9 | 0.295* |
| Bilateral/unilateral | 23/18 | 59/64 | 0.367† |
| Perioperative hemorrhage (mL) | 322.7 ± 141.6 | 364.6 ± 211.0 | 0.238* |
| Postoperative hemorrhage (mL) | 228.5 ± 66.4 | 251.3 ± 85.1 | 0.119* |
| Preoperative joint space (mm) | 2.9 ± 1.4 | 3.2 ± 1.3 | 0.221* |
| Center-edge angle (degrees) | 4.2 ± 6.9 | 1.1 ± 9.8 | 0.065* |
| Acetabular head index | 53.9 ± 8.9 | 51.3 ± 7.0 | 0.061* |
| Joint congruency (good/poor) | 19/22 | 66/57 | 0.417† |
Values are expressed as mean ± standard deviation; *statistically analyzed by Student’s t test; †statistically analyzed by chi square test; Group O = patient 50 years or older; Group Y = patients younger than 50 years.
The indications for eccentric rotational acetabular osteotomy were (1) acetabular dysplasia with a center-edge angle less than 10° and discontinuity of Shenton’s line, (2) 30 minutes’ walk without rest dependent on hip pain, (3) unsuccessful nonoperative treatment for 6 months, (4) age between 15 and 50 years, and (5) joint congruency and femoral head coverage in maximum abduction. Contraindications for this osteotomy were a severely deformed femoral head in an advanced stage and age older than 60 years [9].
All surgeries were performed by one surgeon (YH). The operative techniques were described previously [8, 9]. Briefly, we made a 20-cm curved skin incision 3 cm proximal to the tip of the greater trochanter. The greater trochanter was detached with a bone saw and reflected proximally. The gluteus muscles were reflected proximally from the acetabular rim. The osteotomy site was located approximately 20 mm from the joint space according to preoperative planning. After osteotomy of the ilium and pubis, the acetabular fragment rotated in the lateral direction easily. We verified coverage of the femoral head by the rotated acetabular fragment on an anteroposterior (AP) projection with an image intensifier before fixation of the acetabular fragment with three polylactide screws. The fragment could be seen directly. We did not rotate the fragment anterior or posterior. The greater trochanter then was fixed with two AO cancellous screws or a cerclage wire (Fig. 1). Our eccentric rotational acetabular osteotomy was modified from the typical rotational acetabular osteotomy in which the greater trochanter is not detached; when the greater trochanter is detached the added exposure makes the surgery easy to perform.
Fig. 1A–C.
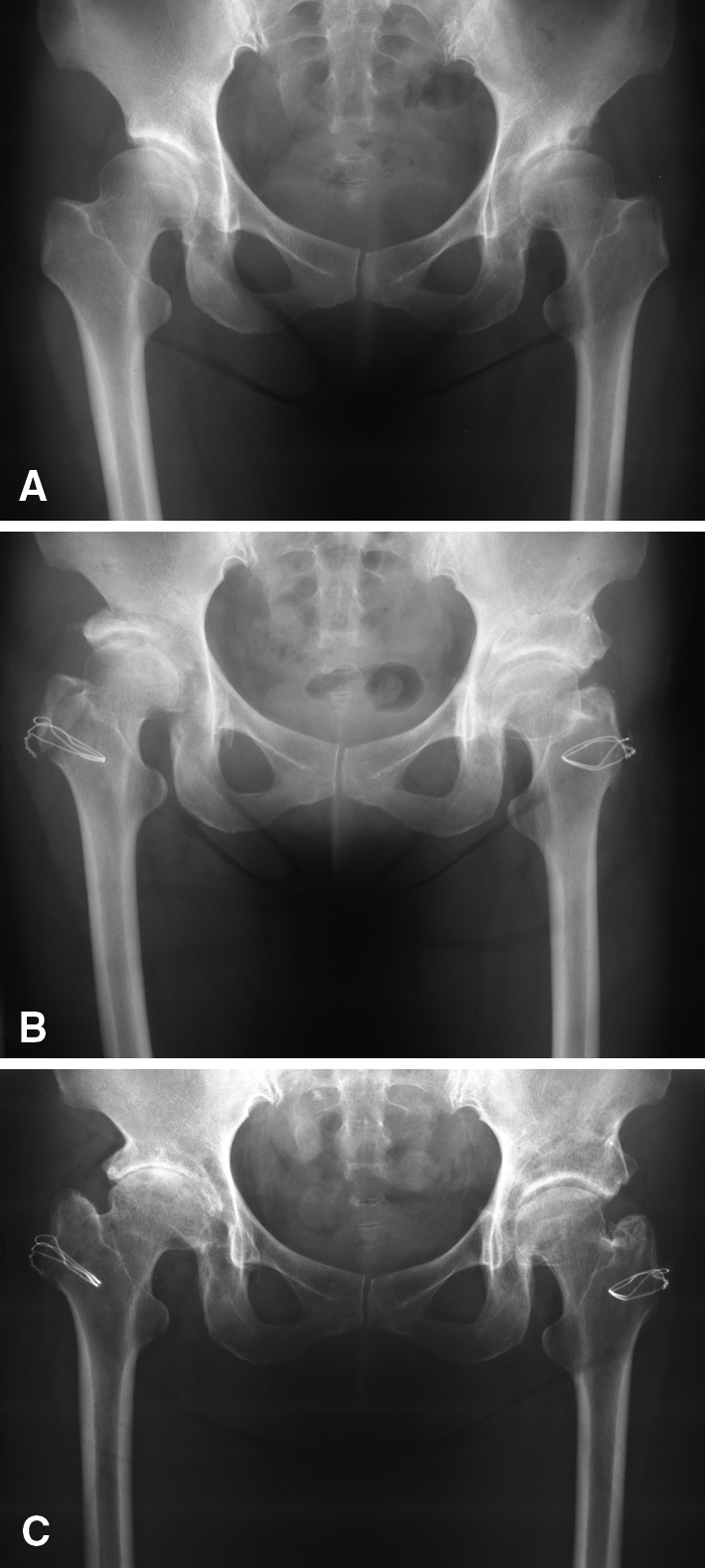
(A) An AP radiograph of the pelvis shows marked bilateral hip dysplasia of a symptomatic 53-year-old woman who had previous acetabular osteotomies. (B) A postoperative AP radiograph of the patient’s right hip at 1 month and of the left hip at 1 year shows marked improvement in femoral head coverage. The patient had marked improvement in function. (C) Fifteen years after surgery, the patient’s postoperative AP radiograph shows substantial deterioration of the joint space of the right hip but preservation of the joint space of the left hip.
Postoperatively, patients were allowed out of bed and began 10-kg partial weightbearing with a walker the day after surgery. Six weeks after surgery, full weightbearing was permitted with two crutches. Full weightbearing without crutches was permitted 4 months after surgery.
We followed patients clinically and radiographically 3 months postoperatively and annually thereafter. One surgeon (YH) evaluated the hips clinically using the Harris hip score [6].
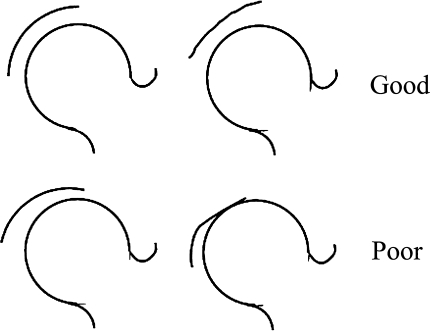
We obtained AP radiographs with the patient in the supine position, centered on the pubic symphysis at a 1.1-m distance. One of us (JY) measured the joint space width, center-edge angle, and acetabular-head index preoperatively, 6 weeks postoperatively, and at the last followup [8, 10]. The radiographic measurements were performed using calipers (Mitsutoyo, Tokyo, Japan) by one physician (JY) blinded to the clinical scores. The minimum joint space width (perpendicular distance between acetabular and femoral head subchondral bone) of the weightbearing region was measured on an AP radiographic image obtained with the patient in the supine position. We made no correction for magnification. The measurement was made three times and the mean value was used. The measurement interobserver variability (kappa statistic) between the two authors (JY, TK) was 0.83. The intraobserver variability after a 3-month interval was 0.88. Preoperative joint congruency in maximum abduction was evaluated. We classified joint congruency as good if the curvature of the acetabular and femoral head subchondral bone were almost identical and if the joint space became wide or was adequately maintained and as poor if the curvature was not identical and if partial narrowing or disappearance of the joint space occurred (Fig. 2) [26]. The interobserver variability of joint congruency categorization (kappa statistic) among the three authors (JY, TK, TS) was 0.82 [4].
Fig. 2.
The diagrams illustrate the classification of joint congruency in maximum abduction. We classified joint congruency as good if the curvature of the acetabulum and femoral head were almost identical and if the joint space became wide or was adequately maintained and as poor if the curvature was not identical and if partial narrowing or disappearance of the joint space occurred.
We determined differences in age, BMI, followup, perioperative hemorrhage, postoperative hemorrhage, preoperative joint space, center-edge angle, and acetabular-head index between older and younger patient groups using Student’s t test. Differences in bilateral/unilateral and joint congruency between the two groups were determined using the chi square test. Harris hip score at the final followup between the two groups was compared using one-way analysis of variance adjusted for BMI, followup, preoperative joint space width, and joint congruency. Kaplan-Meier survivorship analysis was performed with a Harris hip score less than 80 points as one end point and THA as a second end point (patients awaiting THA were not considered in this analysis). Survival between the two groups was determined by log-rank test. The statistical software used was StatView® Version 5.0 (SAS Institute Inc, Cary, NC).
Results
Improvements in the Harris hip score were similar for both groups (Tables 2, 3). In patients with unilateral surgery, the mean Harris hip scores at last followup were similar (p = 0.789) in older and younger patients (92.2 ± 10.4 versus 91.5 ± 10.6, respectively) (Table 3). However, in patients with bilateral surgery, the mean Harris hip score was lower (p = 0.046) in the older group (Table 3).
Table 2.
Preoperative Harris hip scores in the two groups
| Harris hip score | Group O | Group Y | p Value* |
|---|---|---|---|
| Total cases (n = 164) | n = 41 | n = 123 | |
| Total | 60.2 ± 8.3 | 63.1 ± 8.8 | 0.040 |
| Pain | 20.7 ± 4.1 | 22.2 ± 4.7 | 0.084 |
| Gait | 18.9 ± 4.6 | 19.7 ± 5.2 | 0.343 |
| Range of motion | 4.9 ± 0.3 | 5.3 ± 2.5 | 0.339 |
| Daily activity | 11.7 ± 3.0 | 12.4 ± 2.8 | 0.134 |
| Unilateral cases (n = 82) | n = 18 | n = 64 | |
| Total | 61.9 ± 7.9 | 62.2 ± 8.7 | 0.900 |
| Pain | 21.1 ± 4.7 | 21.1 ± 4.0 | 0.988 |
| Gait | 19.2 ± 4.8 | 19.7 ± 5.4 | 0.706 |
| Range of motion | 4.9 ± 0.1 | 5.3 ± 2.7 | 0.546 |
| Daily activity | 12.7 ± 2.0 | 12.4 ± 2.9 | 0.745 |
| Bilateral cases (n = 82) | n = 23 | n = 59 | |
| Total | 58.9 ± 8.6 | 64.2 ± 8.9 | 0.005 |
| Pain | 20.4 ± 3.7 | 23.3 ± 5.2 | 0.016 |
| Gait | 18.7 ± 4.4 | 19.7 ± 5.1 | 0.347 |
| Range of motion | 4.9 ± 0.4 | 5.2 ± 2.2 | 0.531 |
| Daily activity | 11.0 ± 3.5 | 12.4 ± 2.8 | 0.024 |
Values are expressed as mean ± standard deviation; *one-way analysis of variance adjusted for body mass index, followup duration, preoperative joint space width, and joint congruency; Group O = patient 50 years or older; Group Y = patients younger than 50 years.
Table 3.
Harris hip scores in the two groups at final followup
| Harris hip score | Group O | Group Y | p Value* |
|---|---|---|---|
| Total cases (n = 164) | n = 41 | n = 123 | |
| Total | 88.7 ± 13.0 | 92.0 ± 11.7 | 0.084 |
| Pain | 42.2 ± 5.2 | 41.9 ± 4.9 | 0.773 |
| Gait | 26.6 ± 7.1 | 27.8 ± 6.5 | 0.246 |
| Range of motion | 4.8 ± 0.4 | 5.2 ± 2.3 | 0.314 |
| Daily activity | 11.7 ± 2.6 | 13.0 ± 2.4 | 0.0008 |
| Unilateral cases (n = 82) | n = 18 | n = 64 | |
| Total | 92.2 ± 10.4 | 91.5 ± 10.6 | 0.789 |
| Pain | 43.2 ± 3.3 | 41.9 ± 4.4 | 0.245 |
| Gait | 28.8 ± 5.2 | 27.4 ± 6.2 | 0.383 |
| Range of motion | 4.9 ± 0.2 | 5.2 ± 2.6 | 0.610 |
| Daily activity | 11.6 ± 3.0 | 13.0 ± 2.4 | 0.012 |
| Bilateral cases (n = 82) | n = 23 | n = 59 | |
| Total | 86.0 ± 14.4 | 92.6 ± 12.9 | 0.016 |
| Pain | 41.4 ± 6.2 | 42.0 ± 5.4 | 0.653 |
| Gait | 24.8 ± 7.9 | 28.3 ± 6.9 | 0.032 |
| Range of motion | 4.8 ± 0.5 | 5.2 ± 1.9 | 0.406 |
| Daily activity | 11.7 ± 2.3 | 12.9 ± 2.3 | 0.007 |
Values are expressed as mean ± standard deviation; *one-way analysis of variance adjusted for body mass index, followup duration, preoperative joint space width, and joint congruency; Group O = patient 50 years or older; Group Y = patients younger than 50 years.
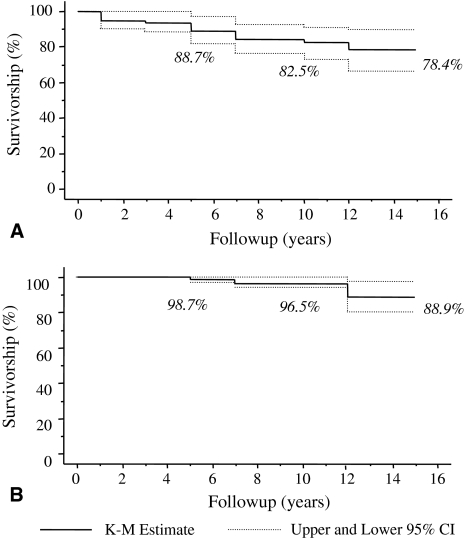
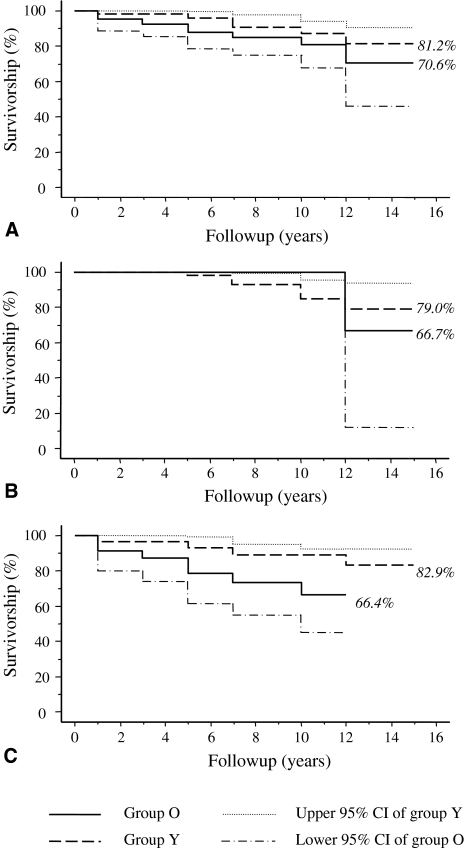
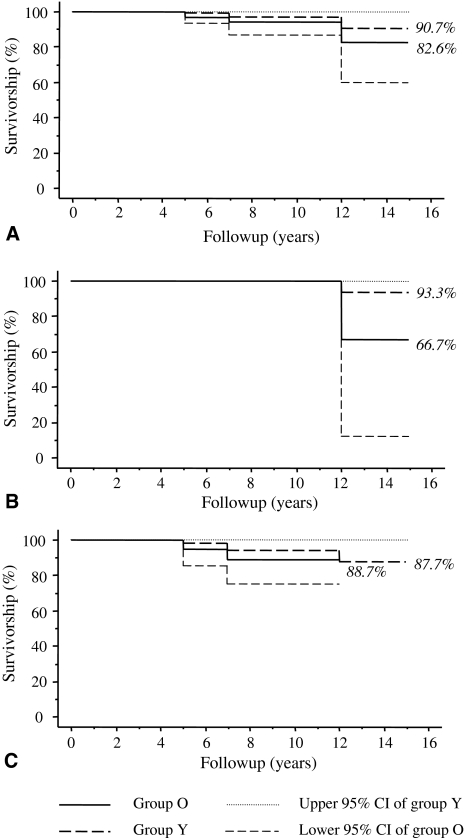
Using a Harris hip score less than 80 points as the end point, we found a 10-year survival rate of 87.3% (95% confidence interval [CI], 83.0%–91.6%) and a 15-year survival rate of 75.2% (95% CI, 61.1%–89.3%) (Fig. 3A). With conversion to THA as the end point, we found a 10-year survival rate of 96.5% (95% CI, 93.5%–99.5%) and a 15-year survival rate of 88.9% (95% CI, 80.2%–97.6%) (Fig. 3B). We observed no differences in survivorship with a Harris hip score less than 80 points as the end point between the younger and older groups (Fig. 4A). In the patients with unilateral disease, we also found no differences between the older and younger groups (Fig. 4B). However, in patients with bilateral disease, we found a lower survivorship in the older patients compared with the younger patients (Fig. 4C). Survivorship with conversion to THA as the end point was similar in the younger and older groups (Fig. 5A), as was survivorship in the patients with unilateral and bilateral osteotomies (Fig. 5B–C).
Fig. 3A–B.
Kaplan-Meier (K-M) survivorship curves with 95% CIs for each 5-year interval (n = 164) are shown: (A) with the end point defined as a Harris hip score less than 80 and (B) with the end point defined as conversion to THA.
Fig. 4A–C.
Kaplan-Meier survivorship curves of eccentric rotational acetabular osteotomy with the end point defined as a Harris hip score less than 80 are shown for older patients (Group O) and younger patients (Group Y). The 95% CIs are shown on only one side of each curve. Survivorship is shown for (A) all patients, (B) patients with unilateral surgery only, and (C) patients with bilateral surgery only. The 10- and 15-year survivorship rates were similar in Groups O and Y in patients with unilateral surgery but lower (p = 0.017) for Group O in patients with bilateral surgery.
Fig. 5A–C.
Kaplan-Meier survivorship curves of eccentric acetabular osteotomy with the end point defined as conversion to THA are shown for older patients (Group O) and younger patients (Group Y). The 95% CIs are shown on only one side of each curve. Survivorship is shown for (A) all patients, (B) patients with unilateral surgery only, and (C) patients with bilateral surgery only. Survivorship was similar (p = 0.644) in both groups regardless of age and whether the osteotomy was unilateral or bilateral.
Four patients in the older patient group and four in the younger patient group were converted to THA during followup. No patient had a superior gluteal nerve palsy; there was one older patient with insufficiency of gluteal muscle recovery because of severe pain postoperatively. One younger patient had nonunion of the trochanter.
Discussion
Pelvic osteotomy has been recommended for young and active patients with hip dysplasia because THA in that population has been associated with high rates of revision THA [20]. However, it remains controversial for middle-aged patients [20, 24, 26]. We can select operative methods for middle-aged patients if the outcomes of osteotomy for them are as good as for young patients. Clinical outcomes between bilaterally affected and unilaterally affected cases may differ. We therefore asked whether (1) eccentric rotational acetabular osteotomy would yield lower Harris hip scores and survivorship in patients 50 years or older than in patients younger than 50 years, and (2) hip scores and survivorship would be lower with bilateral surgery than with unilateral surgery.
We note certain limitations to our study. First, it included a relatively small number of patients, which limits the statistical power. However, the number of patients is relatively large compared with many published studies and we found some differences. Second, the Harris hip score may decrease with age in normal people, and the scores in this study are not age-adjusted. Brinker et al. [2] evaluated 200 patients (age range, 50–100 years) and noted older patients (age > 85 years) had lower hip scores [2]. But in patients younger than 85 years, hip score did not decrease with age substantially. Lieberman et al. [16] reported, in three age groups (58–64 years, 65–74 years, > 75 years), there were no correlations between WOMAC score or Harris hip score and age of the patients. Individuals without hip and knee disorders maintain fairly stable function as they grow older [16]. Third, we did not compare survival of our patients with pelvic osteotomy with that of patients not treated surgically or that of patients with THA. Using any revision as an end point, McAuley et al. [18] reported survival of 89% at 10 years followup and 60% at 15 years followup of THA in patients 50 years and younger. Also, using any revision as an end point, Hartofilakidis et al. [7] reported survivorship of 90% at 10 years followup and 73.3% at 18 years followup of Charnley THA in patients 55 years and younger. Our survivorships are comparable with theirs (Table 4). One surgeon operated on all hips and we excluded patients on whom we operated from 1989 to 1991, thus eliminating potentially inferior outcomes from a learning curve.
Table 4.
Study results of survival of THAs and pelvic osteotomy
| Study | Age (years) | Femoral type of THA/type of pelvic osteotomy | Overall survival for revision/conversion to THA after osteotomy |
|---|---|---|---|
| Mäkelä et al. [17] | 55–64 | Cementless, straight, porous-coated stem with a modular, porous-coated press-fit cup | 95%/80% at 10/15 years |
| Cementless, anatomic, porous-coated and/or hydroxyapatite-coated stem with a modular, porous-coated and/or hydroxyapatite-coated press-fit cup | 92%/78% at 10/15 years | ||
| Hybrid | 90% at 10 years | ||
| Cemented | 85%/71% at 10/15 years | ||
| Hartofilakidis et al. [7] | < 55 | Cemented Charnley | 90%/73% at 10/18 years |
| McAuley et al. [18] | < 50 | Cementless, straight, porous-coated stem with a modular, porous-coated press-fit cup | 89%/60% at 10/15 years |
| Allami et al. [1] | 69.1 (21–103) | Cemented Charnley | 95% at 10 years |
| Kerboull et al. [14] | < 50 | Cemented Charnley-Kerboull | 85.4% at 20 years |
| Yasunaga et al. [26] | < 46 | Rotational acetabular osteotomy | 93.7% at 10 years* |
| 46–58 | 70.0% at 10 years* | ||
| Peters et al. [21] | 15–47 | Bernese periacetabular osteotomy | 92% at 36 months |
| Schramm et al. [22] | mean 24.4 | Wagner spherical osteotomy | 65.1% at 25 years |
| Current study | < 50 | Eccentric rotational acetabular osteotomy | 90.7% at 15 years |
| 50–60 | 82.6% at 15 years |
* Radiographic progression of osteoarthritis was defined as the end point.
Previously, osteotomy was recommended mostly for younger persons, with the mean age in most earlier osteotomy series between 20 and 40 years [5, 12, 15, 20, 23]. Ninomiya and Tagawa [20] did not recommend osteotomy in elderly patients because of limping owing to weakness of the gluteus medius. However, some reports have described osteotomy in middle-aged subjects as well. Yano et al. [24] obtained an improvement in Japanese Orthopaedic Association hip score from 48.2 to 81.2 at a mean 38 months after rotational acetabular osteotomy in a group with a mean age of 42.3 years (range, 31–62 years). Moreover, Yasunaga et al. noted no major difference in 10-year survivorship after rotational acetabular osteotomy between a group of 24 patients (26 hips) who were 46 years or older (70.0%) and a group of 60 patients (63 hips) who were younger than 46 years (93.7%) [26]. Similarly, we found the Harris hip score at last followup was similar between the younger and older patient groups. Survivorship with the end point defined as a Harris hip score less than 80 points was 80.7% at 10 years and 70.6% at 15 years in older patients. Furthermore, survivorship with conversion to THA as the end point was 94.4% at 10 years and 82.6% at 15 years in older patients (Table 4). Although we have no data, we interpret the survival data to suggest the biomechanical changes induced by osteotomy may reduce the progression of joint cartilage degeneration seen in the normal course.
We found eccentric rotational acetabular osteotomy survivorship with conversion to THA as the end point was 96.5% and 88.9% at 10 and 15 years, respectively. Peters et al. [21] performed Bernese periacetabular osteotomy in 73 patients (83 hips) with a mean age at surgery of 28 years and a mean followup of 46 months and reported a survivorship at 36 months of 92% with THA as the end point. Schramm et al. [22] performed Wagner spherical osteotomy in 22 patients (22 hips) with a mean age of 24.4 years and a mean followup of 23.9 years and reported a survivorship at 25 years of 65.1% with THA as the end point. Thus, the Harris hip score and survivorships obtained in our study with eccentric rotational acetabular osteotomy in patients with a mean age of 40.8 years were favorable. Yasunaga et al. [25] reported a comparative study on the outcomes of curved varus osteotomy for minimal dysplasia of the hip in 15 patients older than 45 years at a mean of 8 years after surgery and on the outcomes of rotational acetabular osteotomy in 16 patients performed during the same period. No difference was observed between the two groups regarding the Merle d’Aubigné and Postel score during followup. Curved varus osteotomy is considered a less invasive operation. However, we choose nonoperative treatment or shelf acetabuloplasty [3] for elderly patients with mild dysplasia because, in failed cases, it is difficult to insert a prosthesis into part of the proximal femur.
In patients with bilateral surgery, the Harris hip score and survivorships of the older patients were inferior to those of the younger patients. At last followup, the mean Harris hip score was 92.6 points in younger patients and 86.0 points in older patients. The 10- and 15-year survivorship rates were 87.3% and 82.9% in younger patients and 66.4% and 66.4% in older patients. The Harris hip score generally decreases with age in normal people. Harris hip scores also were lower in older patients than in younger patients in this study. However, in patients with bilateral osteotomies, the mean Harris hip score in older patients at the final followup was inferior to that in younger patients. Moreover, the survivorship rates with conversion to THA as the end point between the two groups were similar (patients awaiting THA were not considered in this analysis). Although we cannot fully explain why the mean daily activity score of older patients was inferior to that in younger patients (Table 3), it is possible the intervention inhibits postoperative daily activity by physician advice. Because patients with bilateral disease cannot protect the other side, the probability of progression of degenerative arthritis may be greater, and thus the choice of therapy has been difficult in such patients [11]. Kawate et al. [13] reported, at the 25-year followup of patients who had valgus osteotomy for arthritic hips, the mean score of patients with unilateral hip involvement was higher than that of patients with bilateral involvement. Hisatome et al. [11] reported a 10-year survivorship rate of 86.9% in 61 bilaterally affected cases subjected to unilateral rotational acetabular osteotomy in which symptoms on the unoperated side were mild and in which the end point was radiographic evidence of osteoarthritis progression. If symptoms are mild, high survival rates still may be obtained even when there is bilateral involvement. It therefore appears the unoperated side can support the operated side in the younger patients with early osteoarthritis with mild pain on the unoperated side. However, after 50 years, once the disease has progressed, the pain on the unoperated side will likely worsen and the burden on the operated side will be increased. In older patients with bilateral involvement, the surgical indications must be considered carefully, paying special attention to factors such as the disease stage of the unoperated side. In bilaterally affected cases, THA may be the selection for the more severe side.
Even in patients 50 years or older, high survival comparable to that for younger patients can be obtained with an eccentric rotational acetabular osteotomy in patients with unilateral disease. Therefore, we believe osteotomy merits consideration in patients 50 years or older with dysplasia as well. However, surgeons should be careful in considering osteotomy in older patients with bilateral osteoarthritis.
Acknowledgments
We thank Toshiki Iwase, Shinji Kitamura, Ken-ichi Yamauchi, Shinji Sakano, and Hisashi Iwata for assistance and advice concerning eccentric acetabular osteotomy.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Allami MK, Fender D, Khaw FM, Sandher DR, Esler C, Harper WM, Gregg PJ. Outcome of Charnley total hip replacement across a single health region in England: the results at ten years from a regional arthroplasty register. J Bone Joint Surg Br. 2006;88:1293–1298. [DOI] [PubMed]
- 2.Brinker MR, Lund PJ, Cox DD, Barrack RL. Demographic biases found in scoring instruments of total hip arthroplasty. J Arthroplasty. 1996;11:820–830. [DOI] [PubMed]
- 3.Fawzy E, Mandellos G, De Steiger R, Mclardy-Smith P, Benson MK, Murray D. Is there a place for shelf acetabuloplasty in the management of adult acetabular dysplasia? A survivorship study. J Bone Joint Surg Br. 2005;87:1197–1202. [DOI] [PubMed]
- 4.Fleiss JL. Statistical Methods for Rates and Proportions. Ed 2. New York, NY: John Wiley & Sons, Inc; 1981.
- 5.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed]
- 6.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 7.Hartofilakidis G, Karachalios T, Zacharakis N. Charnley low friction arthroplasty in young patients with osteoarthritis: a 12- to 24-year clinical and radiographic followup study of 84 cases. Clin Orthop Relat Res. 1997;341:51–54. [DOI] [PubMed]
- 8.Hasegawa Y, Iwase T, Kitamura S, Yamauchi K, Sakano S, Iwata H. Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years. J Bone Joint Surg Am. 2002;84:404–410. [PubMed]
- 9.Hasegawa Y, Masui T, Yamaguchi J, Kawabe K, Suzuki S. Factors leading to osteoarthritis after eccentric rotational acetabular osteotomy. Clin Orthop Relat Res. 2007;459:207–215. [DOI] [PubMed]
- 10.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed]
- 11.Hisatome T, Yasunaga Y, Tanaka R, Yamasaki T, Ishida O, Ochi M. Natural course of the minimally symptomatic nonoperated hip in patients with bilateral hip dysplasia treated with contralateral rotational acetabular osteotomy. J Orthop Sci. 2005;10:574–580. [DOI] [PubMed]
- 12.Kanai H, Takatori Y, Umeyama T, Nakamura S, Morimoto S, Ninomiya S. Rotational acetabular osteotomy for the treatment of dysplastic hips with end-stage osteoarthrosis: a biological alternative to total hip arthroplasty? Arch Orthop Trauma Surg. 1999;119:376–379. [DOI] [PubMed]
- 13.Kawate K, Tanaka Y, Ohmura T, Hiyoshi N, Yajima H, Tomita Y, Takakura Y. Twenty-five years followup of patients who had valgus osteotomy for arthritic hips. Clin Orthop Relat Res. 2004;426:151–158. [DOI] [PubMed]
- 14.Kerboull L, Hamadouche M, Courpied JP, Kerboull M. Long-term results of Charnley-Kerboull hip arthroplasty in patients younger than 50 years. Clin Orthop Relat Res. 2004;418:112–118. [DOI] [PubMed]
- 15.Lack W, Windhager R, Kutschera HP, Engel A. Chiari pelvic osteotomy for osteoarthritis secondary to hip dysplasia. Indications and long-term results. J Bone Joint Surg Br. 1991;73:229–234. [DOI] [PubMed]
- 16.Lieberman JR, Hawker G, Wright JG. Hip function in patients > 55 years old: population reference values. J Arthroplasty. 2001;16:901–904. [DOI] [PubMed]
- 17.Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older: an analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170. [DOI] [PubMed]
- 18.McAuley JP, Szuszczewicz ES, Young A, Engh CA Sr. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. [DOI] [PubMed]
- 19.Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand. 1998;69:259–265. [DOI] [PubMed]
- 20.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66:430–436. [PubMed]
- 21.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. [DOI] [PubMed]
- 22.Schramm M, Hohmann D, Radespiel-Troger M, Pitto RP. Treatment of the dysplastic acetabulum with Wagner spherical osteotomy: a study of patients followed for a minimum of twenty years. J Bone Joint Surg Am. 2003;85:808–814. [DOI] [PubMed]
- 23.Wagner H. Osteotomies for congenital hip dislocation. The Hip. Proceedings of the Fourth Open Scientific Meeting of the Hip Society. St Louis, MO: CV Mosby; 1976:45–66.
- 24.Yano H, Sano S, Nagata Y, Tabuchi K, Okinaga S, Seki H, Suyama T. Modified rotational acetabular osteotomy (RAO) for advanced osteoarthritis of the hip joint in the middle-aged person: first report. Arch Orthop Trauma Surg. 1990;109:121–125. [DOI] [PubMed]
- 25.Yasunaga Y, Hisatome T, Tanaka R, Yamasaki T, Ochi M. Curved varus osteotomy for minimal dysplastic hip in patients older than 45 years of age: comparison with rotational acetabular osteotomy. J Orthop Sci. 2005;10:264–269. [DOI] [PubMed]
- 26.Yasunaga Y, Takahashi K, Ochi M, Ikuta Y, Hisatome T, Nakashiro J, Yamamoto S. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003;85:266–272. [DOI] [PubMed]