Abstract
Abstract
The number of revision total knee arthroplasties (rev-TKA) is increasing every year. These cases are technically difficult and add considerable burden on the healthcare system. Many patients have concomitant low back pain that may interfere with functional outcome. We asked whether having low back pain at baseline would influence amount and rate of improvement on standardized outcomes measures after rev-TKA. We retrospectively reviewed 308 patients from prospectively collected data in a multicenter study. A minimum 24-month followup was available for 221 patients (71.8%). Patients with low back pain at baseline had worse scores on most instruments than their counterparts at baseline, 12 months postsurgery, and 24 months postsurgery. The data suggest concomitant back pain in patients undergoing rev-TKA affects their outcomes as measured by standardized instruments. Orthopaedic surgeons should counsel their patients with back pain regarding the possibility of slower or less complete recovery.
Level of Evidence: Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA provides pain relief and allows increased physical function in patients with osteoarthritis of the knee, and the positive results from this procedure [5–7, 28, 32] have led to increased demand at an exponential rate during the last 20 years [12, 18, 19]. The corresponding demand for revision of a TKA (rev-TKA) has increased accordingly [1, 4, 18]. The annual demand for primary TKA is expected to increase to 3.48 million procedures by 2030, and the number of annual rev-TKA procedures is expected to double by 2015; an increase in rev-TKAs of 601% has been projected for 2030 [19]. A 2003 National Institutes of Health consensus statement concerning TKA and rev-TKA suggested additional investigation into specific clinical and demographic factors and their influence on outcomes was needed [16]. Since then, the effect of patient characteristics on reported outcomes after TKA was reported [8]. In their investigation into the relationship between failure of primary knee arthroplasty leading to revision surgery and socioeconomic status, Saleh et al. identified numerous comorbidities in their rev-TKA cohort, including back pain (48.3% prevalence) [31].
Back pain reportedly affects eight of 10 people in the United States and prevalence increases with age [27]. By one estimate 59 million people in the United States have experienced low back pain during the past 3 months [26]. A study published in 2007 evaluating the impact of preintervention patient factors on outcomes of primary TKA suggested one such factor was low back pain [8]. Using the Medical Outcomes Study SF-36 and the WOMAC, Escobar et al. reported absence of low back pain was associated with improved health-related quality of life after primary knee arthroplasty [8].
Because of the large percentage of patients reporting low back pain, we first determined the differences in baseline SF-36, WOMAC, Knee Society scores (and their various subscores) in patients without and with back pain; we then determined the improvement in the two groups after revision TKA; and finally we compared the speed and completeness of recovery in the two groups at 12 and 24 months.
Materials and Methods
We retrospectively reviewed prospectively collected data for all patients undergoing revision knee arthroplasty at 17 North American institutions from March 2002 through March 2004. Recruitment followed a strictly managed protocol at each site. After Institutional Review Board approval of the study at each of the participating units, a consecutive series of patients was considered for enrollment once the consulting surgeon identified the need for a revision TKA. Patients had to meet inclusion criteria and not have any exclusion criteria (Table 1), and sign a consent form to be enrolled in the study, therefore, not all patients initially referred for inclusion in the study were eligible to enroll. Fifteen of the 323 patients (4.8%) who were approached and were eligible to participate in the study declined enrollment, leading to a final enrollment of 308 patients. Baseline data were gathered from patients immediately after consent. Standard data-gathering techniques and instruments and data transfer and management techniques were adopted at each location. Data were collected at each of the 17 sites by dedicated study coordinators who compiled the data and forwarded all information to a central study coordinator for entry in the database. Back pain was listed as a comorbidity by 154 of the 308 patients (50%) at enrollment. Nineteen surgeons performed the procedures; the number of procedures at each site ranged from one to 45 total procedures. At 24 months, 221 patients still were enrolled (71.8% followup rate). Of the 87 patients no longer enrolled at 2 years, five died secondary to complications not related to rev-TKA (1.6%) and 82 were lost to followup (26.6%).
Table 1.
Inclusion and exclusion criteria for the North American Knee Arthroplasty Revision Study Prospective Cohort Study
| Inclusion criteria | Exclusion criteria |
|---|---|
| At minimum, tibial and/or the femoral component requiring reconstruction | Requiring polyethylene exchange only or failed unicondylar prosthesis |
| Signed informed consent obtainable | Informed consent not obtained |
| Failure of a primary TKA | Previous revision surgery to affected knee |
| Age older than 18 years | Metastatic or primary tumor of knee |
| Intact cognition | Reflex sympathetic dystrophy of leg |
| Fluent communication in English | Medically unfit to tolerate surgery |
| Capacity to complete self-administered questionnaire | Progressive muscular condition with quadriceps weakness |
| Ability adhering to the study protocol | Neurologic deficit of affected limb |
| Knee pain associated with spinal pathology |
Data were collected by performing serial assessments of the individual patients. These assessments were completed preoperatively at baseline, intraoperatively, and postoperatively at 6, 12, 18, and 24 months. At baseline, all patients were asked to provide demographic information and their medical histories. Comorbidities were recorded on standardized forms as being “present” or “not present.”
Outcomes were measured using the Medical Outcomes Study SF-36 [24, 25, 33], the WOMAC [2, 3, 34], the functional and clinical components of the Knee Society Severity Index (KSS) [14], and the Lower Extremity Activity Scale (LEAS) [30]. The WOMAC and the SF-36 provide good estimates of patient outcomes following joint replacement [11, 22, 23], and the LEAS was developed specifically for use in the rev-TKA population [30]. All measures, with the exception of the KSS, were completed by the patient at each visit; the KSS was completed by the physician during the patient visit. The measures provided functional assessment scores, which were tabulated for each patient into cumulative scores respective to the individual assessment tools. Additional data were collected regarding patient baseline demographics and comorbidities (Table 2).
Table 2.
Summary of demographics of the 308 patients enrolled in the North American Knee Arthroplasty Revision Study
| Demographic variable | Percentage/value |
|---|---|
| Mean age (range) | 68.7 years (34–85) |
| Mean body mass index (range) | 31.8 kg/m2 (17–60) |
| Females | 53% |
| Males | 47% |
| Race | |
| White | 83% |
| Black | 14% |
| Other | 3% |
| Employment | |
| Retired/disabled | 86% |
| Working | 14% |
| Comorbidities | |
| Osteoarthritis | 75% |
| Hypertension | 62.4% |
| Back pain | 50% |
| Heart disease | 25.9% |
| Diabetes | 23.9% |
To determine the differences in functional improvement between groups, piecewise general linear mixed model regression models (GLMM) were used. These models are more advantageous than regular regression models because they adjust for the correlated nature of repeated measures with time for the same subject in the analysis. Also, the piecewise GLMM estimates two different slopes, each for a segment of the time of followup, which was divided into two periods, Period 1 from baseline to 12 months and Period 2 from 12 months to 24 months. This accounts for the nonlinear nature of improvement after surgery. This also allowed for analysis of the rate of recovery between groups. Additionally, univariate analysis was performed to investigate if there were any major relationships among demographic variables (age, race, gender, educational status, marital status, employment status, and income level), comorbidity status (presence or absence of low back pain), and patient outcomes variables (Medical Outcomes Study SF-36 [24, 25, 33], the WOMAC [2, 3, 34], the functional and clinical components of the KSS [14], and the LEAS [30]) during these same times.
Results
Patients with low back pain at baseline had worse SF-36 scores compared with patients without back pain (Table 3): Bodily Pain (p = 0.004), General Health (p = 0.0003), Physical Function (p = 0.002), Physical Component Score (p = 0.007), Vitality (p = 0.001), Social Function (p = 0.036), Mental Health (p = 0.002), and Mental Component Score (p = 0.003). Additionally, patients with back pain had worse scores (p = 0.007) on the WOMAC pain standardized instrument at baseline than patients who did not have back pain. Twelve months after surgery, outcomes as measured by these SF-36 instruments (all p < 0.05) and the WOMAC pain (p = 0.001), WOMAC function (p = 0.006), LEAS (p = 0.0002), and KSS function (p = 0.02) instruments were worse for patients undergoing rev-TKA with low back pain when compared with patients undergoing rev-TKA without low back pain. Patients undergoing rev-TKA with low back pain had worse WOMAC scores than those without low back pain at 24 months: WOMAC pain (p = 0.044), WOMAC function (p = 0.003), and KSS function (p = 0.018) instruments and SF-36 standardized instruments: Bodily Pain (p = 0.00001), Physical Component Score (p = 0.014), Vitality (p = 0.017), and Social Function (p = 0.049).
Table 3.
Mean functional improvement for patients with low back pain (+) and without back pain (−) after rev-TKA
| Instrument | Baseline | 12 months | 24 months | |||
|---|---|---|---|---|---|---|
| comorbid back pain | comorbid back pain | comorbid back pain | ||||
| (−) | (+) | (−) | (+) | (−) | (+) | |
| SF-36 Bodily Pain | 33.32 | 27.45* | 61.01 | 42.34* | 55.98 | 39.79* |
| SF-36 General Health | 69.84 | 60.98* | 68.21 | 59.71* | 65.26 | 61.66 |
| SF-36 Mental Component | 50.09 | 45.94* | 52.51 | 49.06* | 52.51 | 50.19 |
| SF-36 Mental Health | 73.51 | 66.52* | 76.30 | 69.86* | 76.91 | 73.47 |
| SF-36 Physical Component | 31.98 | 29.73* | 39.81 | 34.46* | 38.54 | 34.78* |
| SF-36 Physical Function | 32.82 | 25.41* | 49.10 | 37.79* | 45.82 | 45.07 |
| SF-36 Social Function | 59.07 | 52.06* | 75.54 | 64.49* | 75.47 | 67.10* |
| SF-36 Vitality | 47.37 | 39.74* | 57.32 | 46.74* | 55.37 | 47.62* |
| WOMAC function | 33.24 | 36.18 | 19.59 | 25.54* | 21.30 | 28.59* |
| WOMAC pain | 9.44 | 10.74* | 4.64 | 6.91* | 5.51 | 7.06* |
| KSS function | 39.20 | 35.75 | 59.62 | 51.58* | 58.70 | 46.24* |
| LEAS | 7.78 | 7.20 | 9.69 | 8.26* | 9.09 | 8.32 |
* p < 0.05; patients with back pain have significantly worse scores than patients without back pain; KSS = Knee Society Severity Index; LEAS = Lower Extremity Activity Scale.
Both groups of patients showed improvement from baseline to 12 months postsurgery in most instruments (Table 3). The back pain group showed improvement in SF-36 Bodily Pain (p < 0.0001), Physical Function (p < 0.0001), Physical Component Score (p < 0.0001), Vitality (p = 0.001), Social Function (p < 0.0001), and the Mental Component Score (p = 0.009). This group also showed improvement during the first year postsurgery in WOMAC Function (p < 0.0001), WOMAC Pain (p < 0.0001), WOMAC Stiffness (p < 0.0001), and KSS Function (p < 0.0001). In addition, the group with low back pain showed improvement from 12 months to 24 months postsurgery in the SF-36 Physical Function (p = 0.0199). The group without low back pain showed improvement from baseline to 12 months postsurgery in SF-36 Bodily Pain (p < 0.0001), Physical Function (p < 0.0001), Physical Component Score (p < 0.0001), Vitality (p < 0.0001), Social Function (p < 0.0001), and the Mental Component Score (p = 0.045). This group also showed improvement during the first year postsurgery in WOMAC Function (p < 0.0001), WOMAC Pain (p < 0.0001), WOMAC Stiffness (p < 0.0001), KSS Function (p < 0.0001), and the LEAS (p = 0.009).
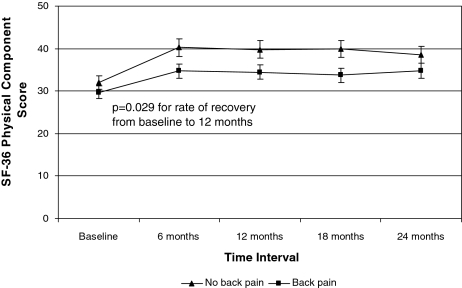
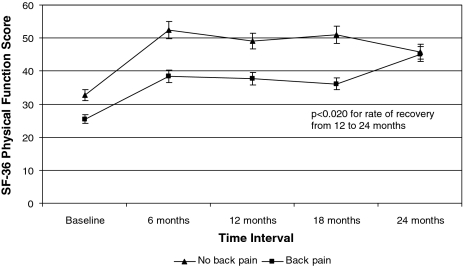
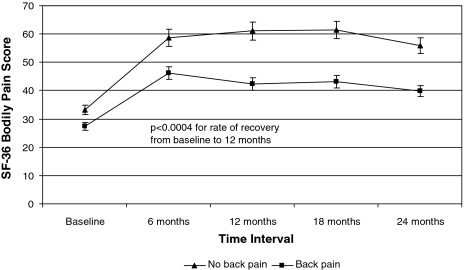
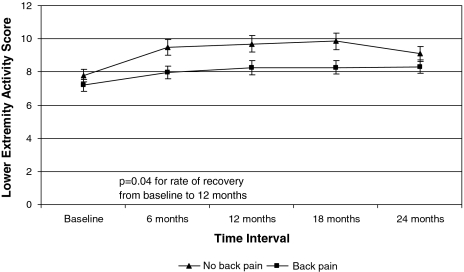
Patients undergoing rev-TKA with low back pain had slower recovery compared with patients without low back pain as measured by average scores with time between baseline and 12 months postsurgery in the SF-36 Bodily Pain (p = 0.0004), SF-36 Physical Component Score (p = 0.029), and LEAS (p = 0.04). For the period from 12 to 24 months postsurgery, the patients with low back pain had faster recovery in the SF-36 Physical Function Score (p = 0.020) compared with patients without low back pain (Figs. 1–4).
Fig. 2.
Differences in recovery are shown for patients with and without baseline low back pain for the SF-36 Physical Component Score. Patients with baseline back pain recovered more slowly than patients without back pain.
Fig. 3.
Differences in recovery are shown for patients with and without baseline low back pain for the SF-36 Physical Function scale. Patients with baseline back pain recovered more slowly than patients without back pain.
Fig. 1.
Differences in recovery are shown for patients with and without baseline low back pain for the SF-36 Bodily Pain scale. Patients with baseline back pain recovered more slowly than patients without back pain.
Fig. 4.
Differences in recovery are shown for patients with and without baseline low back pain for the Knee Society Severity Index outcome scale. Patients with baseline back pain recovered more slowly than patients without back pain.
Discussion
Because of the expected increase in demand for TKAs and rev-TKAs [18–20] and the cost associated with these procedures [21], it is essential for surgeons and patients to understand the potential limitations on recovery that comorbid conditions might have. Previous studies document patient characteristics influence overall functional recovery [12, 13, 15, 29], including one study that suggests low back pain is a preintervention predictor of outcomes [8]. Because of the large percentage of patients reporting low back pain, we therefore (1) determined the differences in baseline SF-36, WOMAC, Knee Society scores in patients without and with back pain; (2) determined the improvement in patients without and with back pain after revision TKA; and (3) compared the speed and completeness of recovery in the two groups at 12 and 24 months.
There were numerous limitations to this study. First, greater than 20% of the cohort was lost to followup, which could affect the overall results of the study because patients who dropped out might have differed from the ones who continued in the study. However, the patients who dropped out were equally represented in both groups (patients with and without baseline back pain), therefore the overall impact should be small. Second, although the sample size was adequate to detect absolute differences between groups, additional analyses into trends in outcomes would require larger sample sizes to ensure enough power to detect differences. For example, we observed trends toward faster recovery for patients without low back pain for other parts of the SF-36 (General Health, Mental Health, Social Functioning, and Mental Component Scores) that were not statistically significant but still might be clinically important for the practicing surgeon when managing patient expectations. In addition, there were trends toward worsening function (as measured by WOMAC and KSS function scores) for patients with low back pain. Examining these trends in studies with longer followup (more than 2 years) could provide a more detailed look at the impact that low back pain has on functional outcomes after rev-TKA. Also, if the sample size in each group increased to 200, the power to detect a difference between groups of 5 points could have increased to greater than 95% from 80%. Third, although patients without back pain served as control subjects for the patients with back pain, we did not compare these outcomes with a group of patients undergoing primary knee arthroplasty, which might provide more information about the distinctions between patients undergoing primary knee arthroplasty versus patients undergoing revision knee arthroplasty. Fourth, the cohort was recruited from tertiary care centers with residency programs, which might not be representative of the general population needing revision knee arthroplasty [20]. Associated with this is the fact that this cohort was culled from patients who agreed to enroll in this clinical trial, who may be substantially different than those who chose not to participate, although the number who did not agree to participate was small (less than 5%). This is a potential problem with all clinical trials. Fifth, the data collected for the study used several questionnaires that relied on patient self-report rather than medical records or care provider information, especially for baseline medical history. The lack of confirmation with other sources could lead to bias in patient group assignment regarding whether back pain was present at baseline. Back pain is a common condition but one that can have many underlying causes that might not involve the knee at all. Therefore, it might be difficult to assign all of the recovery, or lack thereof, to whether a patient reports back pain as opposed to any other comorbidity, groups of comorbidities, or other demographic factors.
Despite these limitations, our data suggest patients with low back pain have lower functional and outcome scores after rev-TKA than those without low back pain and generally recover more slowly in terms of function than patients without low back pain. Although all patients, regardless of comorbidity status, improved in most functional outcomes measures during the first year after undergoing rev-TKA, which is consistent with results from prior studies [6, 9, 10, 15, 17], orthopaedic surgeons recommending revision knee arthroplasty should alert patients with low back pain to the possibility of slower or less complete recovery. Doing so could contribute to improved patient satisfaction with this procedure and more involved participation by patients in their postoperative treatment.
Acknowledgments
We thank the North American Knee Arthroplasty Revision Study investigators for their assistance in securing data for this article.
Principal Investigator: K. Saleh, MD, MSc, University of Virginia, Charlottesville, VA
Co-Investigators: C. Clark, MD, University of Iowa, Iowa City, IA; G. Engh, MD, Anderson Orthopedic Institute, Alexandria, VA; D. Heck, MD, Indiana University, Indianapolis, IN; D. Hungerford, MD, Johns Hopkins School of Medicine, Baltimore, MD; R. Iorio, MD, Lahey Clinic, Burlington, MA; K. Krackow, MD, Buffalo General Hospital-Kaleida Health, Buffalo, NY; P. Lotke, MD, University of Pennsylvania, Philadelphia, PA; W. Macaulay, MD, Columbia University, New York, NY; S. MacDonald, MD, London Health Sciences Center, London, Canada; M. Mont, MD, Mount Sinai, Baltimore, MD; J. Rand, MD, Mayo Clinic, Scottsdale, AZ; H. Rubash, MD, Massachusetts General Hospital, Boston, MA; G. Scuderi, MD, Insall, Scott, Kelly Institute, New York, NY; S. Scully, MD, Mayo Clinic, Rochester, MN; R. Windsor, MD, The Hospital for Special Surgery, New York, NY.
University of Minnesota:
T. Gioe, MD, Veteran Affairs Medical Center, Minneapolis, MN; R. Kyle, MD, Hennipen County Medical Center, Minneapolis, MN; K. Hepburn, PhD, R. Kane, MD, K. Saleh, MD, and M. Swiontkowski, Fairview University Medical Center, Minneapolis, MN
University of Virginia:
T. Brown, MD; Q. Cui, MD; W. Mihalko, MD, PhD
Central Project Team Coordinators: L. Saleh, BSN, University of Toronto, Toronto, Canada (1995–1999); A. Macaulay, PhD, Columbia University, New York, NY (1998–1999); J. Agel, MA, University of Minnesota, Minneapolis, MN (1999–2001); M. Celebresse, MA, MSc, University of Minnesota, Minneapolis, MN (2001–2003); N. Miller, MSc, and K. Schwartz, MSc, University of Minnesota, Minneapolis, MN (2003-present)
NAKAR Statisticians: B. Bershadsky, PhD, University of Minnesota, Minneapolis, MN; A. Gafni, PhD, University of McMaster, Hamilton, Canada; M. Kuskowski, PhD, University of Minnesota, Minneapolis, MN; G. Norman, PhD, University of Minnesota, Minneapolis, MN; R. Tweedie, PhD, University of Minnesota, Minneapolis, MN; W. Novicoff, PhD, University of Virginia, Charlottesville, VA
Contributing Investigators (contributed to the study by recruiting and inducting patients): M. Bostrom, MD, The Hospital for Special Surgery, New York, NY; R. Bourne, MD, London Health Sciences Center, London, Canada; H. Clark, MD, Insall, Scott, Kelly Institute, New York, NY; F. Cushner, MD, Insall, Scott, Kelly Institute, New York, NY; S. Haas, MD, The Hospital for Special Surgery, New York, NY; W. Healy, MD, Lahey Clinic, Burlington, MA; R. Laskin, MD, The Hospital for Special Surgery, New York, NY; J. Marsh, MD, University of Iowa, Iowa City, IA; J. McAuley, Anderson Orthopedic Institute, Alexandria, VA; R. McCalden, London Health Sciences Center, London, Canada; C. Nelson, MD, University of Pennsylvania, Philadelphia, PA; C. Rorabeck, MD, London Health Sciences Center, London, Canada; J. Schmidt, MD, University of Minnesota, Minneapolis, MN; N. Scott, MD, Insall, Scott, Kelly Institute, New York, NY
Footnotes
One or more of the authors (WMM, KJS) have received funding from the Orthopaedic Research Educational Foundation.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.American Academy of Orthopedic Surgeons. National Hospital Discharge Survey, 1991–2004. US Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Health Statistics. Available at: http://www.aaos.org/Research/stats/Knee%20Revision%20Chart.pdf. Accessed May 31, 2008.
- 2.Bellamy N, Buchanan WW. Outcome measurement in osteoarthritis clinical trials: the case for standardization. Clin Rheumatol. 1984;3:293–303. [DOI] [PubMed]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed]
- 4.Bozic KJ, Durbhakula S, Berry DJ, Naessens JM, Rappaport K, Cisternas M, Saleh KJ, Rubash HE. Differences in patient and procedure characteristics and hospital resource use in primary and revision total joint arthroplasty: a multicenter study. J Arthroplasty. 2005;20(suppl 3):17–25. [DOI] [PubMed]
- 5.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994;271:1349–1357. [DOI] [PubMed]
- 6.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. [DOI] [PubMed]
- 7.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: long-term results. Clin Orthop Relat Res. 2001;392:272–278. [DOI] [PubMed]
- 8.Escobar A, Quintana JM, Bilbao A, Azkarate J, Guenaga JI, Arenaza JC, Gutierrez LF. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology. 2007;46:112–119. [DOI] [PubMed]
- 9.Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963–974. [DOI] [PubMed]
- 10.Hartley RC, Barton-Hanson NG, Finley R, Parkinson RW. Early patient outcomes after primary and revision total knee arthroplasty: a prospective study. J Bone Joint Surg Br. 2002;84:994–999. [DOI] [PubMed]
- 11.Hawker G, Melfi C, Paul J, Green R, Bombardier C. Comparison of a generic (SF-36) and a disease specific (WOMAC) (Western Ontario and McMaster Universities Osteoarthritis Index) instrument in the measurement of outcomes after knee replacement surgery. J Rheumatol. 1995;22:1193–1196. [PubMed]
- 12.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–173. [DOI] [PubMed]
- 13.Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA. Patient outcomes after knee replacement. Clin Orthop Relat Res. 1998;356:93-110. [DOI] [PubMed]
- 14.Insall JN, Dorr LD, Scott RD, Norman WS. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 15.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1719–1724. [DOI] [PubMed]
- 16.Kane RL, Saleh KJ, Wilt TJ, Bershadsky B, Cross WW III, MacDonald RM, Rutks I. Total knee replacement. Evid Rep Technol Assess (Summ). 2003;86:1–8. [PMC free article] [PubMed]
- 17.Kennedy DM, Stratford PW, Riddle DL, Hanna SE, Golish JD. Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther. 2008;88:22–32. [DOI] [PubMed]
- 18.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. [DOI] [PubMed]
- 19.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. [DOI] [PubMed]
- 20.Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24:195–203. [DOI] [PubMed]
- 21.Lavernia C, Lee DJ, Hernandez VH. The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res. 2006;446:221–226. [DOI] [PubMed]
- 22.Lequesne M. Indices of severity and disease activity for osteoarthritis. Semin Arthritis Rheum. 1991;20(6):48–54. [DOI] [PubMed]
- 23.Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB, Kinemax Outcomes Group. Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am. 2001;83:1856–1864. [DOI] [PubMed]
- 24.McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. [DOI] [PubMed]
- 25.McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. [DOI] [PubMed]
- 26.National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum. 2008;58:26–35. [DOI] [PMC free article] [PubMed]
- 27.National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, US Department of Health and Human Services. Handout on Health: Backpain. Bethesda, MD: National Institutes of Health; 2005. NIH Publication No 05-5282.
- 28.Rand JA, Ilstrup DM. Survivorship analysis of total knee arthroplasty: cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am. 1991;73:397–409. [PubMed]
- 29.Rasanen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynanen OP, Roine RP. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78:108–115. [DOI] [PubMed]
- 30.Saleh KJ, Mulhall K, Bershadsky B, Ghomrawi H, White LE, Buyea CM, Krackow K. Development and validation of a lower-extremity activity scale: use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am. 2005;87:1985–1994. [DOI] [PubMed]
- 31.Saleh KJ, Santos ER, Ghomrawi HM, Parvizi J, Muhall KJ. Socioeconomic issues and demographics of total knee arthroplasty revision. Clin Orthop Relat Res. 2006;446:15–21. [DOI] [PubMed]
- 32.Shields RK, Enloe LJ, Leo KC. Health related quality of life in patients with total hip or knee replacement. Arch Phys Med Rehabil. 1999;80:572–579. [DOI] [PubMed]
- 33.Ware JE Jr, Sherborne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [DOI] [PubMed]
- 34.Whitehouse SL, Lingard EA, Katz JN, Learmonth ID. Development and testing of a reduced WOMAC function scale. J Bone Joint Surg Br. 2003;85:706–711. [PubMed]