Abstract
Open repair of full-thickness tears of the rotator cuff generally improves function, although anatomic failures are not uncommon. We asked whether the presence or absence of an anatomic repair influenced outcomes. We retrospectively analyzed 47 patients (49 shoulders) treated by open proximalized reinsertion of the supraspinatus tendon for chronic retracted detachment. The mean age of the patients at the time of surgery was 59 years. At a minimum 60-month followup (mean, 87 months; range, 60–133 months), we observed an improvement in the age- and gender-adjusted Constant-Murley score from 67% preoperatively to 95% postoperatively and in the pain score. With the last followup MRI, the supraspinatus tendon had reruptured in five patients (12%); the presence of a rerupture did not negatively influence the functional result. Once healing of the repaired tendons was achieved, supraspinatus muscle atrophy never worsened. However, on MRI, fatty infiltration of the supraspinatus, infraspinatus, and subscapularis muscles increased postoperatively despite tendon healing. Radiographic centering of the humeral head was preserved and glenohumeral arthritis remained stable. Functional results were better when the standardized supraspinatus muscle area was greater than 0.5 at the final evaluation.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Open repair of full-thickness tears of the rotator cuff reportedly provides reliable improvement in function and pain [3, 5, 7, 18, 24] and general health status enhancement [23]. However, short- to intermediate-term studies have noted a 7% to 31% rate of anatomic failure after surgical repair of small to intermediate tears [4, 8, 10, 11, 14, 17, 29, 35] as opposed to a much higher failure rate after repairs of massive tears [5, 7, 10, 11, 17, 18, 29, 33]. Age older than 65 years, number and degree of retractions of initially torn tendons, and fatty infiltration of the rotator cuff muscles reportedly predict retear regardless of the repair technique [1, 3, 12, 15, 24, 33]. Retears are not necessarily synonymous with clinical failure [20], but they usually are associated with poorer function and more severe degenerative changes of the rotator cuff muscles than are successful repairs [8, 12, 14, 15, 29]. Although fatty infiltration affecting the muscular body of the repaired tendons apparently never decreases even after successful healing [8, 14, 22], the reversibility of supraspinatus muscle atrophy after structural healing has been reported [27]. Retears also may influence the progression of degenerative changes of the glenohumeral joint [37].
A tension-free repair of the torn tendons is required to enhance the chance of healing of the tendon-bone attachment [16, 26]. Because removal of the abnormal tendon border increases the defect size, we routinely perform proximalized tendon-bone reinsertion located at the cartilage-bone junction of the humeral head. Previous studies reported proximalized bone-tendon reinsertion might increase the rates of healing of the supraspinatus muscle tendon provided there was limited fatty degeneration of the rotator cuff muscles before surgery [8, 12, 15, 19].
Therefore, our objectives were to (1) document the minimal 5-year functional outcome of patients who underwent standardized open surgical repair for complete detachment of the supraspinatus muscle tendon; (2) describe the state of repair, muscle atrophy, and fatty infiltration on postoperative MRI of the rotator cuff muscles; (3) determine the influence of postoperative MRI findings on final functional outcome; and (4) determine whether the repair benefits glenohumeral arthritis and subacromial space height.
Materials and Methods
From March 1995 to November 2001, we performed open surgery for a torn rotator cuff tear in 97 patients (104 shoulders). For this review, we included patients with (1) a chronic retracted full-thickness detachment of the supraspinatus tendon on the humeral head apex [2] treated with open repair; (2) persistent pain and/or shoulder disability after at least 6 months of nonoperative treatment; (3) an age younger than 65 years and/or the need or desire to improve abduction strength; and (4) minimum 5-year clinical and radiographic followup after surgery. We excluded patients with (1) a prior attempt at rotator cuff repair; (2) an irreparable tear, defined as a torn tendon retracted to the glenoid rim; and (3) osteoarthritis rated as Stage III or greater according to Samilson and Prieto [25] or rheumatoid disease of the glenohumeral joint. Forty-seven patients (49 shoulders) met the inclusion criteria. Twenty-three patients were men and 24 were women. All patients had chronic shoulder pain that had been treated with medication, physical therapy, and/or subacromial injection of cortisone. The mean duration of symptoms before surgery was 27 months (range, 10–180 months). The ages of the patients at the time of surgery ranged from 40 to 70 years (mean, 58.8 ± 7 years). The right shoulder was treated in 35 patients, the left shoulder was treated in 10 patients, and a bilateral staged procedure was performed in two patients. The dominant shoulder was involved in 37 cases (75.5%). Twenty-eight patients (60%) were involved in strenuous activities at work or regularly practiced some sport. One patient (one shoulder) died of an unrelated cause, and two patients (two shoulders) were lost to followup. The 44 remaining patients (46 shoulders) were evaluated clinically and with use of standard radiographs. The minimum followup was 60 months (mean, 87 months; range, 60–133 months).
In 41 shoulders (83.7%), the infraspinatus tendon insertion, as determined clinically and with preoperative computed tomography arthrogram and confirmed intraoperatively, was intact. In eight shoulders (16.3%), a full-thickness tear of the supraspinatus and infraspinatus tendons was present. Associated rotator cuff lesions included degenerative rupture or dislocation of the long head of the biceps in nine cases, a delamination tear of the infraspinatus tendon in 16 cases, and detachment of the superior third of the subscapularis tendon in seven cases.
We performed all operations with the patients in a lateral position. A superolateral approach, with an 8- to 10-cm long incision, was used. The anterior part of the lateral deltoid muscle was elevated subperiosteally from the lateral aspect of the acromion. The deltoid muscle was split between its anterior and lateral portions parallel to its muscle fibers. We released the coracoacromial ligament. An anteroinferior acromioplasty was performed with an osteotome. Once the subacromial bursa was released, we inspected the rotator cuff. The intervals between the supraspinatus and the infraspinatus and between the supraspinatus and the subscapularis were opened. The degenerative tendon tear border was excised. We made an intraarticular incision located between the capsule and the labrum, allowing lateral mobilization of the torn tendon. A deep osseous anteroposterior trough was created with a dental burr at the humeral head cartilage-bone junction. The free border of the tendon was inserted deeply in the trough and maintained with two or three paired nonabsorbable transosseous sutures (Fig. 1). We repaired the full-thickness tear of the infraspinatus tendon using the same procedure as described for the supraspinatus in eight cases. Tenodesis of the long head of the biceps was performed in four cases because it either was degenerated or dislocated. We treated delamination tears of the infraspinatus tendon by curettage followed by closure of its border with absorbable sutures in seven cases. The detached superior border of the subscapularis was reinserted on the lesser tuberosity with two or three nonabsorbable anchors (Quick Anchor Plus; Mitek; Johnson and Johnson, Norwood, MA) after local débridement in seven cases. We closed the interval between the infraspinatus and the supraspinatus and between the subscapularis and the supraspinatus with absorbable sutures with Number 2 Vicryl (Ethicon; Johnson and Johnson, Westwood, MA) to ensure the cuff repair was watertight. The resistance of the repair then was tested intraoperatively with the arm at the side. Secure deltoid repair was achieved using nonabsorbable transacromial suture with Number 3 Mersuture (Ethicon).
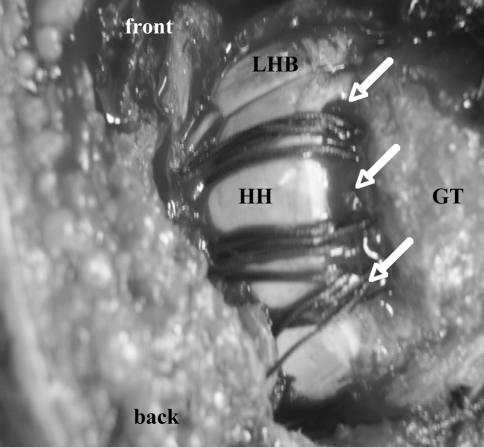
Fig. 1.
A photograph shows the operative view of a full-thickness tear of the supraspinatus tendon (right shoulder). The humeral head (HH) cartilage is visible. The anteroposterior trough (three arrows) is located at the humeral head cartilage-bone junction. Three paired nonabsorbable sutures are passed through the lateral cortex, the bony trough, and the tendon stump in a U configuration. A paired suture corresponds to two stitches crossing each other in a cruciform pattern at the tendon level. Knots subsequently will be tightened on the lateral cortex of the greater tuberosity (GT) of the humerus with care being taken to tie the ends from the same suture to one another. LHB = long head of the biceps brachii tendon.
Postoperatively, rotator cuff repairs were protected in an abduction brace as recommended [13] at 60° for 6 weeks. All patients were referred to a rehabilitation unit 2 to 3 days after surgery. Then, therapist-assisted passive mobilization of the shoulder was started once a day above the abduction level of 60°. After 6 weeks, gradual return to the side was begun in combination with self-assisted pendulum and active shoulder range-of-motion exercises, including scapular stabilization, under the supervision of the physiotherapist. Progressive strengthening of the joint started after 10 weeks.
We evaluated patients preoperatively and prospectively followed each with clinical examinations 6 weeks, 3 months, 6 months, and 1 year postoperatively, according to the method of Constant and Murley [6]. The Constant-Murley score was calculated as an absolute numeric value and as a percentage of an age- and gender-matched normal score (the relative Constant-Murley score). We measured pain using a visual analog scale ranging from 0 (severe pain) to 15 (no pain) as previously described [8]. At the time of last followup, assessment of range of motion and evaluation of abduction strength using a digital dynamometer with the arm abducted 90° were performed.
We obtained standardized radiographic examinations (true anteroposterior radiographs of the glenohumeral joint with the arm in internal, external, and neutral rotation and a transscapular view) under fluoroscopic control for each patient preoperatively and at the latest followup. One of the investigators (CM) not involved in the surgery categorized arthritis of the glenohumeral joint according to Samilson and Prieto [25]. Specifically, 12 (24.5%) shoulders were considered free of arthritis, 34 (69.4%) were classified as Stage 1, and three (6%) as Stage 2. None was rated Stage 3 or Stage 4. We measured subacromial space (SAS) height on plain anteroposterior radiographs of the glenohumeral joint in neutral rotation. The preoperative SAS height ranged from 3 to 13 mm with a mean of 9.24 ± 2.35 mm in the series as a whole (Table 1).
Table 1.
Preoperative radiologic and computed tomography characteristics
| Variables | Isolated SSP detachment | SSP and ISP detachment | Overall |
|---|---|---|---|
| Number (%) | 41 (83.7) | 8 (16.3) | 49 (100) |
| Subacromial space height (mm) | 9.85 | 6.75 | 9.24 |
| Fatty muscle infiltration* | 0.66 | 1.54 | 0.81 |
| Standardized muscle area† | 0.61 | 0.56 | 0.59 |
* According to the criteria described by Goutallier et al. [14]; †standardized muscle area is defined by the cross-sectional area of the supraspinatus muscle to the cross-sectional area of its fossa; SSP = supraspinatus tendon; ISP = infraspinatus tendon.
All patients had a preoperative computed tomography arthrogram, and 37 had preoperative MRI. At least one of these preoperative studies was available for review for each patient at the time of this investigation. Four patients (four shoulders) were unable to return for postoperative MRI for reasons not related to the results of the surgery. According to the staging system of Goutallier et al. [14], mean preoperative fatty muscle infiltration (FMI) was 0.81 ± 0.67 (range, 0–3; median, 0.67). Supraspinatus muscle atrophy was measured on the most lateral image on which the scapular spine was in contact with the scapular body on the oblique and sagittal views (the Y-shaped view) as described by Thomazeau et al. [29]. We digitally measured the cross-sectional areas of the supraspinatus muscle and its fossa using a picture-analyzing system (OsiriX DICOM viewer, open-source software). Results were expressed as the standardized muscle area (SMA) defined by the cross-sectional area of the muscle to the cross-sectional area of the fossa [12, 28, 34] (Table 1). At last followup, repaired tendon healing, fatty infiltration of the rotator cuff muscles, and supraspinatus muscle atrophy were evaluated with standardized MRI by an experienced musculoskeletal radiologist (CM) who was blinded to the clinical data of the patient. Examination was performed with the arm positioned in neutral rotation on a 1.5-T magnetic resonance system (Signa; GE Healthcare Technologies, Waukesha, WI) with a four-channel phased-array shoulder coil. The slice thickness was 3 mm with a gap ranging from 0.4 to 1.5 mm. The field of view ranged from 140 to 160 mm; the image matrix was 384 × 256, 416 × 288, or 416 × 256; and the number of excitations was three or two. We assessed healing or rerupture of the repaired supraspinatus or infraspinatus tendon on oblique coronal fast spin echo fat-saturated T2-weighted sequences. When a fluid-equivalent signal or nonobservation of the supraspinatus or infraspinatus tendon was found on at least one section, the diagnosis of a full-thickness rerupture was made. We assessed FMI according to a classification derived from Goutallier et al. [14] as adapted for use with MRI [34] on oblique parasagittal T1-weighted fast spin echo sequences. The stages identified were Stage 0, normal muscle; Stage 1, some fatty streaks; Stage 2, manifest fatty infiltration but less fat than muscle; Stage 3, as much fat as muscle; and Stage 4, more fat than muscle. Fatty muscle infiltration was expressed as a mean for the supraspinatus, infraspinatus, and subscapularis muscles.
Numerical data were expressed as mean with standard deviation. We retrospectively defined two groups according to the preoperative state of the infraspinatus tendon, which was either intact (Group 1) or ruptured (Group 2).We determined differences in the Constant-Murley score, pain scores, and strength between the preoperative and postoperative periods using the nonparametric test of Wilcoxon (paired groups) and between the two categorical groups at last followup using the Mann-Whitney rank sum test (unpaired groups). We analyzed differences in FMI and SMA between categorical groups using the Mann-Whitney rank sum test. We determined whether MRI findings (repaired tendons state, FMI, and standardized muscle area) correlated with the final functional result using Fisher’s exact test. To determine the influence of postoperative supraspinatus muscle atrophy on functional outcome, we compared the Constant-Murley scores for patients according to a SMA threshold set at 0.5 using the Mann-Whitney rank sum test [28]. We then determined whether the operative procedure and repair healing, as assessed on last followup MRI, influenced subacromial space height and glenohumeral arthritis using the Mann-Whitney rank sum test and Fisher’s exact test, respectively.
Results
The average Constant-Murley scores improved postoperatively in all series (Table 2). We noted postoperative improvement in the average score for shoulder pain, the average score for activities of daily living, active flexion, and overall average abduction strength. Although there was no difference (p = 0.39) in the postoperative relative Constant-Murley score between Group 1 and Group 2, postoperative mean flexion and external rotation were greater (p = 0.04 and p < 0.001, respectively) in Group 1.
Table 2.
Clinical parameters related to the nature of the preoperative rotator cuff tendon tear
| Clinical parameters | SSP detachment (N = 40) | SSP and ISP detachment (N = 6) | Overall (N = 46) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | p Value* | Preoperative | Postopera-tive | p Value* | Preoperative | Postoperative | p Value* | |
| Constant-Murley score | |||||||||
| Absolute (points) | 54.6 | 74.1 | < 0.0001 | 46.3 | 71 | 0.03 | 53.3 | 73.7 | < 0.0001 |
| Relative† (%) | 68 | 94.7 | < 0.0001 | 61 | 97.3 | 0.03 | 67.1 | 95 | < 0.0001 |
| Pain score‡ (points) | 5.9 | 13.1 | < 0.0001 | 5.3 | 12.8 | 0.03 | 5.9 | 13 | < 0.0001 |
| Activities of daily living score (points) | 9.4 | 17.3 | < 0.0001 | 8.8 | 16.7 | 0.03 | 9.3 | 17.2 | < 0.0001 |
| Active motion (degrees) | |||||||||
| Flexion | 125.6 | 137 | 0.02 | 116 | 118.3 | 1 | 124.5 | 134.5 | 0.03 |
| Abduction | 120.2 | 125.4 | 0.37 | 115 | 118.3 | 0.75 | 119.5 | 124.5 | 0.34 |
| External rotation | 41.5 | 43.1 | 0.25 | 42.5 | 42.5 | 0.91 | 40.8 | 43 | 0.32 |
| Internal rotation (thoracic level reached with thumb) | 7.1 | 6.4 | 0.12 | 7.7 | 7.3 | 1 | 7.2 | 6.5 | 0.11 |
| Abduction strength | |||||||||
| Kilograms§ | 4.9 | 5.7 | 0.03 | 2.8 | 4.2 | 0.03 | 4.65 | 5.7 | 0.008 |
| Points|| | 8.7 | 11.5 | 0.03 | 4.7 | 8.5 | 0.03 | 8.2 | 11.5 | 0.008 |
* According to the Wilcoxon signed rank test with p < 0.05 as the level of significance; †the relative Constant-Murley score is the percentage of an age- and gender-related normal value according to the system of Constant-Murley [6]; ‡as measured with a visual analog scale on which 15 indicates no pain and 0 indicates intolerable pain; §strength was measured with a digital dynamometer with the arm in 90° scapular abduction, the elbow extended, resistance applied at the wrist, and the forearm pronated; ||according to the scoring system of Constant-Murley; patients with active abduction less than 90° are given 0 points for strength; SSP = supraspinatus tendon; ISP = infraspinatus tendon.
Healing of supraspinatus tendon repair was observed in 37 of the 42 shoulders and rerupture in five (12%) as assessed by MRI. All five retears were located on the greater tuberosity and, thus, appeared smaller than the preoperative tears. Retear rates of the supraspinatus tendon were similar (p = 0.55) in both groups (Table 3). In Group 1, eight de novo complete detachments were observed, including two infraspinatus tendons and six subscapularis tendons. No additional de novo rupture was observed in Group 2. Standardized supraspinatus muscle area increased (Group 1) or remained stable (Group 2) after successful healing of supraspinatus tendon repair. In contrast, when a retear occurred, supraspinatus muscle atrophy always worsened in both groups (Table 3). Fatty infiltration of the three muscles progressed with time in the entire group, from 0.8 ± 0.61 preoperatively to 1.74 ± 0.74 postoperatively (p < 0.0001) and in Group 1 (p < 0.0001) regardless of repair healing. The FMI of the three muscles was similar in Group 1 and Group 2 preoperatively (p = 0.09) and at last evaluation (p = 0.06). None of the preoperative MRI parameters predicted a postoperative retear (Table 4).
Table 3.
Postoperative MRI findings as a function of rotator cuff tendon state
| Variables | SSP detachment (N = 37) | SSP and ISP detachment (N = 5) | ||||
|---|---|---|---|---|---|---|
| Intact or healed (%) | Retorn (%) | Torn (%) | Intact or healed (%) | Retorn (%) | Torn (%) | |
| Rotator cuff tendon | ||||||
| SSP | 33 (89.2) | 4 (10.8) | — | 4 (80) | 1 (20) | — |
| ISP | 35 (94.5) | — | 2 (0.05) | 5 (100) | 0 | — |
| SSC | 31 (84) | — | 6 (0.16) | 5 (100) | — | 0 |
| Standardized muscle area | 0.79 | 0.62 | — | 0.57 | 0.3 | — |
| Fatty muscle infiltration | ||||||
| SSP | 1.57 | 1.5 | — | 2 | 3 | — |
| ISP | 1.65 | — | 2 | 3.6 | — | — |
| SSC | 1.5 | — | 1.5 | 3 | — | — |
SSP = supraspinatus tendon; ISP = infraspinatus tendon; SSC = subscapularis tendon.
Table 4.
Clinical, radiologic, and MRI findings in Group 1
| Variables | Preoperative value | Postoperative value | ||||
|---|---|---|---|---|---|---|
| Intact repairs (N = 33) | Retears (N = 4) | p Value | Intact repairs (N = 33) | Retears (N = 4) | p Value | |
| Age (years) | 58.2 | 56.3 | 0.61* | 65.6 | 63 | 0.47* |
| Gender ratio (male/female) | 19/14 | 1/3 | 0.21† | 19/14 | 1/3 | 0.21† |
| Constant-Murley score | ||||||
| Absolute (points) | 57 | 45 | 0.06‡ | 75.8 | 69.2 | 0.50‡ |
| Relative (%) | 71 | 58.5 | 0.12‡ | 97 | 89 | 0.84‡ |
| Pain score (points) | 6.3 | 5 | 0.03‡ | 13.5 | 12.5 | 0.56‡ |
| Activities of daily living score (points) | 10 | 7 | 0.12‡ | 17.7 | 15.2 | 0.30‡ |
| Flexion (degrees) | 129.7 | 97.5 | 0.01‡ | 140.5 | 127.5 | 0.12‡ |
| Abduction strength | ||||||
| Kilograms | 4.8 | 2.5 | 0.18‡ | 5.8 | 5.7 | 0.87‡ |
| Points | 10.7 | 5.7 | 0.12‡ | 11.7 | 11.5 | 0.87‡ |
| Subacromial space height (mm) | 9.8 | 9.5 | 0.74‡ | 10.6 | 10.2 | 0.83‡ |
| Standardized muscle area§ | 0.6 | 0.5 | 0.73‡ | 0.79 | 0.62 | < 0.0001‡ |
| Fatty muscle infiltration|| | 0.77 | 0.5 | 0.49‡ | 1.7 | 1.4 | 0.75‡ |
* According to the Student’s t-test; †according to the chi square test; ‡according to the Mann-Whitney rank sum test; the level of significance is set at p < 0.05; §standardized muscle area is defined by the cross-sectional area of the supraspinatus muscle to the cross-sectional area of its fossa; ||according to the criteria described by Goutallier et al. [14].
The five shoulders with tendon retears had similar Constant-Murley scores (p = 0.9) compared with those with healed repairs. In Group 1, preoperative pain score and active flexion were higher (p = 0.03 and p = 0.01, respectively) in shoulders that had successful tendon healing compared with those that did not (Table 4). The higher functional scores were observed (p = 0.01) when standardized supraspinatus muscle area was greater than 0.5.
Glenohumeral arthritis remained stable (p = 0.22) with time. Postoperatively, six (14%) shoulders remained free of arthritis, 29 (69%) shoulders were classified as Stage 1, and seven (17%) as Stage 2. Mean subacromial space height improved (p = 0.02) from 9.41 ± 2.37 mm (range, 3–13 mm) preoperatively to 10.26 ± 2.08 mm (range, 5–14 mm) postoperatively in all series and in Group 1. Mean SAS height was stable in Group 2 (p = 0.4) between the preoperative and postoperative periods. Overall, mean SAS height was not influenced by supraspinatus tendon healing (p = 0.83). However, after supraspinatus tendon healing, the mean SAS was greater (p = 0.03) in Group 1 in comparison with Group 2 (Table 5).
Table 5.
Clinical, radiologic, and MRI findings in successful repairs of the supraspinatus tendon
| Variables | SSP detachment (N = 33) | SSP and ISP detachment (N = 4) | p Value |
|---|---|---|---|
| Followup (months) | 89.3 | 81.2 | 0.43* |
| Age (years) | 65.6 | 69.2 | 0.59* |
| Gender ratio (male/female) | 19/14 | 0/4 | 0.03† |
| Constant-Murley score | |||
| Absolute (points) | 75.8 | 67.1 | 0.22‡ |
| Relative (%) | 97 | 96.3 | 0.61‡ |
| Pain score (points) | 13.5 | 13 | 0.99‡ |
| Activities of daily living score (points) | 17.7 | 16.2 | 0.39‡ |
| Flexion (degrees) | 140.5 | 112.5 | 0.02‡ |
| Abduction strength | |||
| Kilograms | 5.8 | 3.6 | 0.20‡ |
| Points | 11.7 | 7.2 | 0.15‡ |
| Subacromial space height (mm) | 10.6 | 7.7 | 0.03‡ |
| Standardized muscle area | 0.79 | 0.57 | 0.54‡ |
| Fatty muscle infiltration | 1.7 | 2 | 0.23‡ |
* According to the Student’s t-test; †according to the chi square test; ‡according to the Mann-Whitney rank sum test; the level of significance is set at p < 0.05; SSP = supraspinatus tendon; ISP = infraspinatus tendon.
There were four complications in the 44 patients. One patient had paresis of the ulnar nerve through abduction splint compression and underwent surgical neurolysis after an 8-month attempt of nonoperative treatment. Three patients had postoperative reflex sympathetic dystrophy and received medical treatment. Two of them reported persistent pain and lack of motion and would decline the procedure. An additional procedure was performed in two patients. One patient who had repair of the supraspinatus and infraspinatus tendons underwent open tenodesis of the long head of the biceps muscle for chronic tendinitis 79 months after the initial procedure. Another patient underwent open repair of the infraspinatus tendon 29 months after the first procedure performed for an isolated tear of the supraspinatus tendon. In both patients, the previous repair was considered healed at the time of the reoperation.
Discussion
Surgical repair of rotator cuff tears reportedly leads to substantial improvement in range of motion and pain [1, 5, 7, 8, 10, 11, 16–18, 24, 37]. The size of a rotator cuff tear reportedly is not only correlated with the postoperative functional outcome [5, 10, 11, 15, 17, 18, 24, 37], but also with structural changes of rotator cuff muscles after repair (retear rate, volume changes, and fatty infiltration) [7, 8, 12, 21, 27, 28, 30, 31]. However, the longer-term relationship of the state of repair and the muscles is unknown. Therefore, our objectives were to (1) document the minimal 5-year functional outcome of patients who underwent standardized open surgical repair for complete detachment of the supraspinatus muscle tendon; (2) analyze the state of repair, muscle atrophy, and fatty infiltration on postoperative MRI of the rotator cuff muscles; (3) determine the influence of postoperative MRI findings on final functional outcome; and (4) evaluate the benefit of repair on glenohumeral arthritis and subacromial space height.
We recognize some limitations may affect the findings of the current study. First, full-thickness tears of the supraspinatus muscle tendon were categorized retrospectively into two groups according to the presence of a full-thickness tear of the infraspinatus tendon, but it is possible other confounding variables such as delamination tear of the infraspinatus or detachment of the superior third of the subscapularis tendon may have affected functional outcome and the retear rate. However, rates of associated lesions were similar between the two categorical groups. Therefore, it is probable they did not preclude further comparison between groups. Second, standard MRI is limited when evaluating the anatomic repair. Although we used fat-suppressed sequences, MRI may have underestimated small and partial-thickness recurrent cuff tears. The analysis of our anatomic data therefore is affected by the accuracy of the MRI. MRI, however, allowed us to accurately evaluate progression of fatty muscle infiltration and supraspinatus muscle atrophy in a noninvasive way [9, 30, 34].
Previous evaluations of surgical repair of medium-sized rotator cuff tears [5, 8, 10, 16] found considerable improvement in the Constant-Murley score parameters (Table 6). Although combined repairs of complete detachments of the supraspinatus and infraspinatus reportedly provide similar functional results as repairs of an isolated detachment of supraspinatus tendon [16], we also found the latter yielded considerably better active flexion and external rotation than repairs of both tendons.
Table 6.
Summary of studies comparing postoperative functional parameters, retear rates, and structural changes
| Study | Followup (months) | Number of cases | Surgical technique | Imaging assessment | Functional parameters | SSP retear rate | SSP muscle atrophy | FMI |
|---|---|---|---|---|---|---|---|---|
| Thomazeau et al. [29] | 21 | n = 30 | Tendon-to-bone reinsertion | MRI | ROM: improved | 20% | Improved | — |
| Pain: improved | ||||||||
| Strength: improved | ||||||||
| Knudsen et al. [21] | 28 | n = 32 | Tendon-to-bone reinsertion | MRI | ADL: improved | 31% | — | — |
| ROM: improved | ||||||||
| Pain: improved | ||||||||
| Strength: stable | ||||||||
| Schaefer et al. [27] | 12 | n = 17 | Tendon-to-bone reinsertion or tendon suture | MRI | Constant-Murley score: improved | — | Stable or improved | — |
| Fuchs et al. [8] | 38 | n = 22 (SSP) | Tendon-to-bone reinsertion with plate augmentation | MRI | ADL: improved | 13% | Stable | Increased |
| n = 10 (SSC) | ||||||||
| ROM: improved | ||||||||
| Pain: improved | ||||||||
| Strength: improved | ||||||||
| Goutallier et al. [16] | 30 | n = 27 | Transosseous reinsertion ± muscular advancement | CT-arthrogram | ADL: improved | 15%* | — | — |
| ROM: stable | ||||||||
| Pain: improved | ||||||||
| Strength: improved | ||||||||
| Zilber et al. [35] | 42 | n = 30 | Transosseous reinsertion | MRI | ROM: improved | 7% | — | — |
| Pain: improved | ||||||||
| Strength: improved | ||||||||
| Current study | 87 | n = 46 | Proximalized transosseous reinsertion | MRI | ADL: improved | 12% | Stable or improved | Increased |
| ROM: improved | ||||||||
| Pain: improved | ||||||||
| Strength: improved |
* Evaluation performed 1 year postoperatively; SSP = supraspinatus; FMI = fatty muscle infiltration; SSC = subscapularis; CT = computed tomography; ROM = range of motion; ADL = activities of daily living.
The structural outcomes of rotator cuff tendon repairs have been reported for series in which the repairs were performed using various operative techniques [4, 8, 10, 14, 15, 17, 21, 27–29, 35, 37]. Anatomic failure rates of 7% to 31% were observed after open repair of moderate tears at short- to midterm [8, 16, 21, 27, 35]. Because it was suggested most recurrences develop within the first 6 months after cuff repair [20], our findings suggest open proximalized transosseous reinsertion of torn tendons provided durable stabilization of bone-tendon healing. With the small number of failed supraspinatus repairs in combined ruptures, an adverse effect of an associated detachment of the infraspinatus tendon on structural outcome was not observed, in contradiction to previous findings [17]. Complete detachment of the supraspinatus muscle rapidly impairs its muscular volume [31]. Although it is believed severe fatty degeneration of the rotator cuff muscles is irreversible after rotator cuff repair, there is still controversy regarding the capability of rotator cuff muscles atrophy to improve after repair. In a recent report [8], it was suggested preoperative supraspinatus muscle atrophy cannot be reversed even after successful repairs. In contrast, Schaefer et al. [27] reported surgical repair of a supraspinatus complete full-thickness tear resulted in stabilization or an increase of muscular volume in a 12-month followup MRI. Consistent with previous findings [27, 29], we found atrophy of the supraspinatus muscle worsened exclusively after repair failure. In contrast, successful healing had a poor influence on FMI, which never improved. This inevitable progression of the degenerative muscular disease has been observed by others [8, 14, 31, 32] and remains unexplained.
Although functional results tend to be better in patients with healed rotator cuffs [1, 8, 11, 15, 17], several studies reported a poor correlation between clinical outcome and anatomic integrity after open repair of moderate-to-intermediate tears [10, 20, 21]. We also found the Constant-Murley scores did not correlate with the integrity of the supraspinatus tendon nor did abduction strength, mobility, and activities of daily living. Our observations do not agree with those of previous studies [11, 17, 29] suggesting repairs that successfully healed resulted in better improvement in abduction strength and activities of daily living. The influence of the recurrent tears on the final functional outcome may have been limited as a result of their size, which always was smaller than the initial tears. We also found a standardized muscle area greater than 0.5 was associated with higher relative Constant-Murley scores. Shen et al. [28] reported the cross-sectional area of the supraspinatus muscle correlated with functional outcome of repair of an isolated full-thickness tear of the supraspinatus tendon. We speculate SMA would correlate with improvement of the relative Constant-Murley score and that supraspinatus muscle atrophy tends to improve after successful healing of its tendon [29]. This being the case, SMA would be a determining factor influencing functional outcome of the rotator cuff after surgical repair.
Zingg et al. [36] reported glenohumeral arthritis and humeral head ascension (evaluated by the narrowing of the subacromial space) increased in correlation with the progressive extent of rotator cuff tear as assessed on MRI. In our study, subacromial space height remained stable or increased regardless of tendon healing. This observation suggests the current surgical procedure provided effective stabilization of the humeral head and resulted in limited progression of arthritis at a mean of 7 years.
We found open repair of a complete detachment of the supraspinatus tendon led to durable functional improvement after a standardized surgical protocol. Anatomic failure of repaired tendons, which was observed in a relatively low number of cases, had a poor influence on the long-term functional results. Supraspinatus muscle atrophy could be reversed after successful healing of the repair. The best Constant-Murley scores were obtained when the postoperative standardized area of the supraspinatus muscle was greater than 0.5. Glenohumeral arthritis progression was limited and centering of the humeral head was preserved in most of the shoulders.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bellumore Y, Mansat M, Assoun J. [Results of the surgical repair of the rotator cuff. Radio-clinical correlation] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1994;80:582–594. [PubMed]
- 2.Bernageau J. Roentgenographic assessment of the rotator cuff. Clin Orthop Relat Res. 1990;254:87–91. [PubMed]
- 3.Bigliani LU, Cordasco FA, McIlveen SJ, Musso ES. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am. 1992;74:1505–1515. [PubMed]
- 4.Calvert PT, Packer NP, Stoker DJ, Bayley JI, Kessel L. Arthrography of the shoulder after operative repair of the torn rotator cuff. J Bone Joint Surg Br. 1986;68:147–150. [DOI] [PubMed]
- 5.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears: a prospective long-term study. J Bone Joint Surg Am. 2001;83:71–77. [DOI] [PubMed]
- 6.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed]
- 7.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed]
- 8.Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88:309–316. [DOI] [PubMed]
- 9.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. [DOI] [PubMed]
- 10.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53. [PubMed]
- 11.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. [DOI] [PubMed]
- 12.Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007;16:691–696. [DOI] [PubMed]
- 13.Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experimental rotator cuff repair: a preliminary study. J Bone Joint Surg Am. 1999:81:1281–1290. [DOI] [PubMed]
- 14.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed]
- 15.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554. [DOI] [PubMed]
- 16.Goutallier D, Postel JM, Van Driessche S, Godefroy D, Radier C. Tension-free cuff repairs with excision of macroscopic tendon lesions and muscular advancement: results in a prospective series with limited fatty muscular degeneration. J Shoulder Elbow Surg. 2006;15:164–172. [DOI] [PubMed]
- 17.Harryman DT 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA 3rd. Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed]
- 18.Hawkins RJ, Misamore GW, Hobeika PE. Surgery for full-thickness rotator-cuff tears. J Bone Joint Surg Am. 1985;67:1349–1355. [PubMed]
- 19.Hersche O, Gerber C. Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elbow Surg. 1998;7:393–396. [DOI] [PubMed]
- 20.Jost B, Pfirrmann CW, Gerber C, Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82:304–314. [DOI] [PubMed]
- 21.Knudsen HB, Gelineck J, Søjbjerg JO, Olsen BS, Johannsen HV, Sneppen O. Functional and magnetic resonance imaging evaluation after single-tendon rotator cuff reconstruction. J Shoulder Elbow Surg. 1999;8:242–246. [DOI] [PubMed]
- 22.Matsumoto F, Uhthoff HK, Trudel G, Loehr JF. Delayed tendon reattachment does not reverse atrophy and fat accumulation of the supraspinatus: an experimental study in rabbits. J Orthop Res. 2002;20:357–363. [DOI] [PubMed]
- 23.Mc Kee M, Yoo DJ. The effect of surgery for rotator cuff disease on general health status. J Bone Joint Surg Am. 2000;82:970–979. [DOI] [PubMed]
- 24.Romeo AA, Hang DW, Bach BR Jr, Shott S. Repair of full-thickness rotator cuff tears: gender, age, and other factors affecting outcome. Clin Orthop Relat Res. 1999;367:243–255. [DOI] [PubMed]
- 25.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456–460. [PubMed]
- 26.Sano H, Uhthoff HK, Backman DS, Brunet JA, Trudel G, Pham B, Ishii H. Structural disorders at the insertion of the supraspinatus tendon: relation to tensile strength. J Bone Joint Surg Br. 1998;80:720–725. [DOI] [PubMed]
- 27.Schaefer O, Winterer J, Lohrmann C, Laubenberger J, Reichelt A, Langer M. Magnetic resonance imaging for supraspinatus muscle atrophy after cuff repair. Clin Orthop Relat Res. 2002;403:93–99. [DOI] [PubMed]
- 28.Shen PH, Lien SB, Shen HC, Lee CH, Wu SS, Lin LC. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg. 2008;17:1–7. [DOI] [PubMed]
- 29.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344:275–283. [DOI] [PubMed]
- 30.Tingart MJ, Apreleva M, Lehtinen JT, Capell B, Palmer WE, Warner JJ. Magnetic resonance imaging in quantitative analysis of rotator cuff muscle volume. Clin Orthop Relat Res. 2003;415:104–110. [DOI] [PubMed]
- 31.Uhthoff HK, Matsumoto F, Trudel G, Himori K. Early reattachment does not reverse atrophy and fat accumulation of the supraspinatus: an experimental study in rabbits. J Orthop Res. 2003;21:386–392. [DOI] [PubMed]
- 32.van de Sande MA, Stoel BC, Obermann WR, Tjong a Lieng JG, Rozing PM. Quantitative assessment of fatty degeneration in rotator cuff muscles determined with computed tomography. Invest Radiol. 2005;40:313–319. [DOI] [PubMed]
- 33.Walch G, Maréchal E, Maupas J, Liotard JP. [Surgical treatment of rotator cuff rupture: prognostic factors] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1992;78:379–388. [PubMed]
- 34.Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998;33:163–170. [DOI] [PubMed]
- 35.Zilber S, Carillon Y, Lapner PC, Walch G, Nové-Josserand L. Infraspinatus delamination does not affect supraspinatus tear repair. Clin Orthop Relat Res. 2007;458:63–69. [DOI] [PubMed]
- 36.Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89:1928–1934. [DOI] [PubMed]
- 37.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–2431. [DOI] [PubMed]