Abstract
Healthcare administrators and physicians alike are navigating an increasingly complex and highly regulated healthcare environment. Unlike in the past, institutions now require strong collaboration among physician and administrative leaders. As providers and managers are trained and work differently, new methods are needed to provide the infrastructure and resources necessary to create, nurture, and sustain alignment between them. We describe four initiatives by administrators and physicians at Hospital for Special Surgery to work together in mutually beneficial relationships that help us achieve the highest level of patient care, satisfaction and safety. These initiatives include improving management efficiency through an orthopaedic service line structure, helping individual physicians grow their practices through the demand-office-operating room initiative of the Physicians Service Department, controlling costs through the supply effectiveness policy, and promoting teamwork in innovation through the technology transfer program.
Introduction
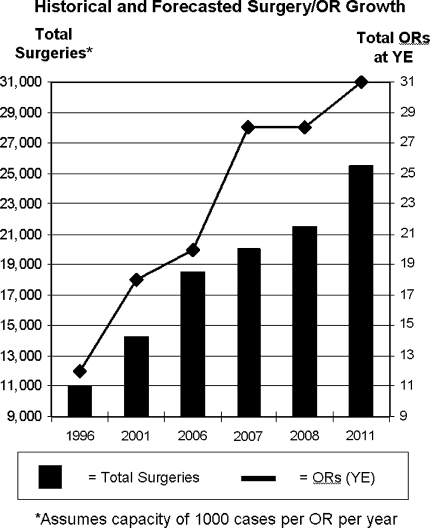
In a rapidly changing healthcare delivery environment [5], Hospital for Special Surgery (HSS) has gradually evolved to meet the needs of our modern healthcare system. HSS was founded in 1863 as The Hospital for the Relief of the Ruptured and Crippled and has since grown from a local hospital serving crippled children and wounded soldiers to an internationally known center for treating musculoskeletal diseases. HSS has a strong organizational model that evolves each year. We have been successful in our commitment to support a three-part mission of clinical, research, and educational excellence even in the face of a growing demand for our services (Fig. 1). Strong financial performance has enabled this continued expansion and reinvestment in our patient care practices, research endeavors, and strong educational program—the pillars which are the foundation for our strong reputation. We believe it is our ability to align physician and hospital incentives that allows us to fulfill our mission.
Fig. 1.
This graph represents the historical and predicted numbers for the total amount of surgeries and the total number of operating rooms at HSS from 1996–2011.
Over the last 30 years, healthcare spending and the scope and complexities of hospital management have grown. During this period of rapid growth, alignment between hospitals and physicians, or managers and providers has deteriorated in many institutions. The increase in information and medical knowledge available to managers has played a key role in increasing external regulation and financial incentives that have led to “a substantial erosion” of physicians’ medical dominance and autonomy [2]. Besides blaming factors that diminish their autonomy, doctors also cite concerns over resource availability and management’s focus on financial rather than clinical priorities as strains to the doctor-manager relationship [2, 5, 8]. This deterioration has led to greater inefficiency, increased costs and, at times, compromised care [2, 9].
At HSS, we believe the alignment of physicians and administration is critical to fulfilling our mission, achieving our goals, and enabling our growth for the common good of our physicians, institution, and our patients [2, 3, 5, 7–9]. Robert McGowan suggests, “when hospitals and physicians work well together, they can better provide patient care efficiently and cost effectively. But hospitals and physicians face many challenges today that can undermine their close working relationship” [7]. To address this opportunity, HSS has created a collaborative healthcare management model focused on the alignment of physicians and the hospital. At HSS, the physicians and hospital leadership work together with a shared commitment to ensure the highest quality of patient care and a strong financial foundation so as to ensure the continued growth and prosperity of the institution. The administrative management team at HSS has as a key goal to support and to ensure our physicians are successful clinically, academically, and economically which, in return, helps the hospital do the same.
In this article, we will discuss why alignment is important as well as provide four detailed examples of practices at HSS that highlight the cooperation and collaboration between physicians and the hospital, resulting in a more efficient, productive, and safer patient care environment. It is through this strong partnership between physicians and administrators that we have been able to align incentives to achieve our goals of clinical, research, and educational excellence. Efforts have been made on both an organizational and policy level. On the organizational level, two initiatives include the creation of an efficient and manageable orthopaedic service line structure and the Physician Service Department’s demand-office-operating room (DOOR) initiative to ensure the success and efficiency of individual physician practices. On the policy level, alignment has been fostered through the supply management effectiveness and technology transfer programs—policies developed to maximize our purchasing initiatives and to foster collaboration on the development of innovative technologies.
Management Efficiency through the Orthopaedic Service Line Structure
There are many initiatives and agendas in a large orthopaedics department. Sometimes, different agendas among physicians can ultimately result in increased inefficiencies and increased healthcare costs. Matters are complicated even further with the involvement of additional departments (e.g., radiology, anesthesiology, internal medicine, rheumatology, neurology and physiatry). For example, HSS has over 90 orthopaedic surgeons, each a leader in his or her respective field. They commit substantial time to the research and educational programs at HSS in addition to building their individual practices. As most of our surgeons are private practitioners, there is a risk of too much decentralization and the emergence of conflicting agendas with little coordination or appreciation for the greater good. To address this challenge, HSS has enhanced the way we organize and manage our orthopaedics and related departments that ultimately allows for greater alignment between physicians and managers.
Our institution organizes our orthopaedics department into 10 distinct service lines each reporting to the surgeon-in-chief. The service lines consist of groups of surgeons specializing in similar clinical areas: adult reconstruction and joint replacement, pediatrics, foot and ankle, hand and upper extremity, spine, scoliosis, sports medicine and shoulder, limb lengthening, trauma, and metabolic bone. The intent of this structure is to harness the individual initiative and innovation to support certain clinical, educational, and research-based initiatives that can only be achieved through the collective efforts of orthopaedists with similar interests. Each service line has clear organizational structures, missions, and member accountability that facilitate the support of all service members to achieve predetermined goals. Additionally, HSS management has committed dedicated administrators to help each service to develop these organizational structures, streamline decision-making processes, form strategic plans, and address service resource needs, all while seeking to promote, maintain, and harness the individual strengths of each service line member.
This organizational structure of the service line approach has dedicated leaders on both the physician and administrative sides to help foster alignment. Each service line has a chief or co-chiefs or some governing body or committee with different charges to include clinical protocol development, research registries, fellowship program management, marketing initiatives, and other strategic priorities. Individual surgeons are involved at the committee level and are able to provide valuable input to solutions that are of benefit to them individually and their colleagues collectively. The service chiefs report to the Surgeon-in-Chief who has responsibility for all 10 service lines. The Surgeon-in-Chief holds regular meetings of the 10 service chiefs to discuss issues that affect all of the services. The Surgeon-in-Chief also requires each service chief to provide regular updates of the progress of the individual services. Each service chief is then partnered with a member of the hospital’s service line department to ensure the execution of various initiatives. The service line department member reports directly to the CEO. This structure fosters better collaboration since it is easier for executive administration to work with the chiefs or committees of these specific service lines directly rather than every physician individually. The service line department liaison helps the service chief(s) develop strategies and then works with other departments to analyze and provide data (e.g., volume, managed care); to identify the appropriate forums to discuss service issues to foster better collaboration between hospital administration, attending office staffs, and other service lines; and to address physical space and staffing resource needs as appropriate. For this system to work effectively, physicians must understand their department responsibilities and have a clear sense of their priorities. In this way, the services function similarly to state governments managing local initiatives through the collaboration between the service chief(s) and the service line department administrator. Each service is then responsible to report to the Surgeon-in-Chief and CEO who function similarly to the federal government.
As an example, the Sports Medicine and Shoulder Service at HSS is led by two co-chiefs who are a part of a five-person executive committee that oversees all aspects of the service either directly or by delegating responsibility to individual members. These co-chiefs would be like state Governors. Example initiatives the service has addressed in the past few years include the development of a service research plan, the development of an ACL registry, the improvement of the fellows’ research program, and the creation of member criteria and expectations. Beyond these initiatives, other priorities delegated to service member subcommittees include the development of the sports primary care fellowship, implementation of a new physician assistant schedule, and execution of two annual educational courses inviting members of the regional community to learn more about the service and the hospital. The 29 service members attend a monthly business meeting to discuss progress on various initiatives. Other services have their own structure and specific initiatives that concern their service, but hold similar meetings to ensure they are meeting their goals as a service. The goal for this structure is to create and maintain an efficient system by which physicians can take responsibility for the management of the respective services, which leads to a stronger fulfillment of our institutional mission.
Physician Service Department and the Demand-Office-Operating Room Initiative
The service line structure has been critical to align incentives of the individual surgeons to their respective services—to ensure surgeon support for initiatives that strengthen and build these groups. HSS also has an entire program to facilitate success and nurture the individual physician. The goal is to make each individual surgeon productive clinically and satisfied economically so he or she can take part in important educational and research-based initiatives that benefit both the physician and the hospital. This initiative is focused on three parts; increasing the demand for our physicians’ services, maximizing the efficiency of physicians’ offices, and optimizing efficiency in the operating room. HSS has a Physician Services Department to help achieve these goals. The Physician Services Department created a program called the “demand-office-operating room” (DOOR) initiative, whereby the Physician Services Department helps the individual surgeon increase demand for his or her services and to improve office and operating room efficiency.
First, the Physician Services Department works with public relations to increase demand through selective advertising including patient mailings, Internet postings, and public relations efforts to heighten patient awareness. HSS does this for every new physician who begins practicing at the Hospital.
Second, the Physician Services Department also works with the new physician to help them develop, manage, and maintain an efficient and successful office. This is first achieved by providing an experienced transitional office staff and helping the physician find a permanent staff by managing the staff interview process. Additionally, the Department offers courses and information to educate him or her as to how to begin and maintain a strong clinical practice. The Department provides advice for physical space allocation and suggests qualified contractors and suppliers for construction. Beyond helping the physician at the start of his or her practice, the Department continues to serve as an ongoing resource for the physician as he or she addresses the challenges that face any new physician, including questions about billing and other areas of office efficiency. This continued support includes monthly reviews to assess financial performance as well as yearly meetings to address a physician’s professional and educational activities. By helping the individual physician grow his or her practice, the hospital benefits as well by having their name and services associated with the physician.
The third component of the DOOR initiative relates to operating room efficiency, which is essential to surgeon satisfaction and the hospital’s financial performance. HSS is constantly working to improve operating room efficiency through teams dedicated to reducing turnover time, and analysis of staffing to ensure the most effective utilization of resources while guaranteeing quality standards are met. HSS has a surgeon-led Operating Room Block Time Committee that meets regularly to review data to allocate block time and to provide training and appropriate staffing of scrub technicians, physician assistants, residents, and fellows to improve OR efficiency. This committee has representation from all of the orthopaedic service lines. In addition, an OR subcommittee ensures that the quality of care continuously improves or stays the same even as surgical volume increases (Fig. 1). One new initiative requires patients to have two forms of ID in the preoperative holding area before he or she even enters the OR. Another initiative administers satisfaction exit polls to medical staff as well as to patients and their families. By better managing our physicians’ time and ensuring quality standards are met, we keep the physicians and their patients satisfied, while also helping the hospital reduce costs by maximizing efficient use of the operating rooms and other limited resources.
Supply Management Effectiveness Policy
HSS also strives to decrease costs, and align physician and hospital incentives through hospital policy. The goal of the supply management effectiveness policy is to control implant and product pricing through hospital and physician collaboration. By negotiating fair and set prices for orthopaedic implants, an immediate reduction of expenses is achieved. In order to accomplish this goal, healthcare manufacturers, administrators, and providers must work together to negotiate reasonable prices for implants. These negotiations require teamwork between management and physicians to maximize cost savings. First, surgeon input is essential to understand and outline the uses of different implants and medical devices. Surgeons are responsible for explaining the frequency of their use and also analyzing competing products. For example, for large hip deformities or revisions, the doctor must explain the need for a modular hip stem so management can effectively negotiate. Management involvement is critical to negotiations so that physicians can choose appropriate implants and devices that work best for the patient at advantageous prices [10]. This strategy affords the surgeon a wide array of implant options providing the patient with the highest level of quality, while reducing cost at the same time. The surplus saved is then reinvested at the service level in research, patient care, education or other venues that will improve medical care. The physicians do not benefit financially directly, but their services collectively do. Therefore, this “institutional gainsharing” [4] is effective, legal, and feasible.
HSS recently instituted a new policy that helps achieve this goal. The supply management effectiveness policy both defines what constitutes savings and addresses the allocation of the savings. The policy applies to all orthopaedic service lines and the departments of anesthesiology, neurology, pathology, physiatry, radiology, and rheumatology (ie, medical departments). The policy assumes and expects that both physicians and hospital administrators will work together to manage the institution’s expenses and to always maintain the highest patient safety and quality standards.
The supply management effectiveness policy applies to all current hospital non-salary operating expense reductions resulting from the partnership between hospital management and physicians. This mainly includes reduced costs due to vendor price negotiations for supplies and implants or changes to practice patterns but only applies to previously existing expenses. Net savings reflects the impact of any reduced cost attributable to the initiative; it does not include price negotiations on new products or technology or any other “cost avoidance” initiatives (i.e., initiatives in which price negotiations for a certain set of items results in the avoidance of purchasing other new supplies and/or implants). The policy only applies to initiatives that result in savings of $10,000 or more and must be formally approved by the appropriate manager, CFO, and service chief.
Net savings are allocated between the hospital, individual service lines and different departments by predetermined percentages (Table 1). If multiple physician departments take part in a negotiation that results in savings, the departments split the allocated amount not allocated to the hospital amongst themselves equally in years 1 to 3 respectively unless predetermined adjustment is agreed upon prior to negotiations. By the end of the program’s fourth year, all savings are allocated to the hospital.
Table 1.
Allocation of net savings according to new HSS supply management effectiveness policy
| Year 1 | Year 2 | Year 3 | Year 4 | |
|---|---|---|---|---|
| Orthopaedic Initiatives | ||||
| Hospital | 60% | 70% | 80% | 100% |
| Orthopaedic service line | 20% | 15% | 10% | 0% |
| Surgeon-in-chief’s fund | 20% | 15% | 10% | 0% |
| Nonorthopaedic Initiatives | ||||
| Hospital | 60% | 70% | 80% | 100% |
| Relevant medical department fund | 40% | 30% | 20% | 0% |
The policy does not cover the use of these savings as each department has their own guidelines on their use. Amounts allocated for hospital operations are included in the current year’s income statement to support existing operations. The orthopaedic services and medical departments can use savings to support educational and research endeavors but may not reimburse or pay physicians for private use. All uses must comply with hospital special purpose fund, travel, and 501(c)(3) policy rules and all other hospital guidelines and policies and procedures.
Technology Transfer Program
A primary mission of HSS is to advance the science of orthopaedic surgery, rheumatology, and their related disciplines to improve patient care. As with other academic institutions HSS recognizes that an essential outcome of providing patient care is performing research and scholarly activities, which may lead to the discovery and development of ideas and products with commercial importance to the medical community. The protection of these intellectual property rights can lead to the development of knowledge, products, and procedures that increase the public usefulness of these activities. It is important, therefore, that the Hospital assists its physicians and staff in protecting and developing ideas competently and efficiently through a critical assessment of the potential and value of their ideas and through the protection and management of the rights to those ideas. This alignment can protect and help physician interests. However, it is also important to recognize that if HSS has contributed to the creation and development of intellectual property, HSS, as a tax-exempt entity and depending on the terms of its funding sources, may not release its ownership right to such intellectual property without receiving appropriate compensation for its interest. Thus, alignment or agreement between the inventor(s) and the Hospital benefits both parties. The agreement is intended to set forth the rights and obligations arising from the creation, development, protection, and commercialization of intellectual property, whether or not such property is patentable, copyrightable, or subject to trade secret or other confidentiality protection.
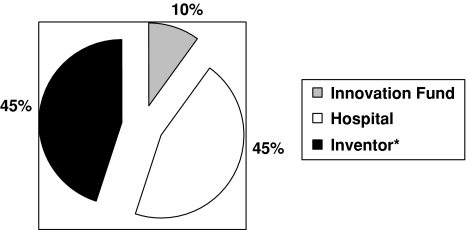
Under our policy, all revenue payments arising from the creation, development, or commercialization of intellectual property discovered with the help of the Hospital will be paid directly to HSS for distribution. Examples of such revenue payments are up-front license fees, milestone payments, and running royalties. Prior to making any distribution of “royalty revenue” to the inventor(s) or HSS, HSS will reimburse the inventor(s) and HSS for the direct, out-of-pocket costs incurred by HSS and/or the inventor(s) in pursuing patent or other protection for the intellectual property and/or in developing and/or managing the intellectual property (“invention costs”). “Royalty revenue” received minus invention costs incurred will determine the “net revenue,” which will be available for distribution by a predetermined allocation scheme (Fig. 2). Under older policies, the distribution of “net revenue” heavily favored the institution, which encouraged physicians to avoid involving the hospital with their private endeavors. Today’s policy shares payments more evenly and fosters greater collaboration between the hospital and its physicians.
Fig. 2.
Distribution of net revenue received as compensation for intellectual property rights discovered by inventors through collaboration with the Hospital is split into three categories. *If the inventor(s) are HSS Physician(s): 100% of that inventor(s)’ share of the Net Revenue will be distributed to such inventor(s). If the inventor(s) are not HSS Physicians: 75% of that inventor(s)’ share of the Net Revenue will be distributed to the inventor(s).
As for the disclosure and ownership of an intellectual property, a new promoting system has been developed to promote fairness for all parties involved. If an HSS physician creates, develops, and/or takes steps to protect intellectual property without using HSS resources, his or her only obligation under this policy is to disclose to the HSS Office of Technology Development (OTD) the intellectual property being created, developed, or protected. Disclosure is required to enable HSS to make a determination, through information provided by the HSS physician, as to whether the HSS physician used HSS resources to create, develop and/or protect the intellectual property. An HSS physician who has not used and does not intend to use HSS resources in such intellectual property activity is under no obligation under this policy to assign his or her rights to such intellectual property to HSS. If, however, an HSS physician has used HSS resources at any stage in the creation, protection, or development of intellectual property, that physician will be required to assign his or her interest in such intellectual property to HSS. In return for his or her contributions to the development of the intellectual property and his or her assigning his or her interest in such intellectual property to HSS, the HSS physician will be compensated in accordance with the terms of this policy and the policy will apply in all respects to such assigned intellectual property. The Hospital can legally and financially penalize any physician who violates this disclosure agreement.
In addition to this policy, HSS has established an Innovation Fund in the Research Division of HSS. The Innovation Fund provides a mechanism to support the additional efforts that are often necessary to bring new concepts and inventions to the patent, copyright, and/or licensing stage. The goal of the Fund is to provide inventor(s) with financial support to aid in bringing new products and processes into the medical marketplace for the public good. Funds can be used to support research and development efforts aimed at potential licensing to the commercial sector. Funding for the Innovation Fund will be supported from the distribution of revenues received from commercialization of intellectual property, which is just an additional example of how physician and hospital incentives can be aligned to work together.
Discussion
As the business of healthcare grows increasingly complex and highly regulated, doctors alone cannot effectively provide care. Business-minded administrators are now required to make decisions on care provision, which has somewhat diminished the physician’s autonomy in making all care decisions. Thus, collaboration and alignment between the two is necessary. While HSS has found ways to accomplish this difficult task, we are not the only institution to implement changes to foster alignment between providers and managers. The orthopaedic service line structure has been used by other institutions to optimize patient-centered care. Kwon et al. described the use of the spine service line at New England Baptist Hospital to minimize healthcare costs and increase quality of care [6]. The institution also benefited from the gathering of registry-like data which would allow analysis of outcomes to improve outcomes. Similarly, HSS service lines have clear structures, missions, and member accountability that includes the gathering of data to improve decision making. In addition, each service line’s governing body both coordinates the efforts of the Service and works in concert with the other Service leaders to reduce cost and increase efficiency at the hospital level.
Along with aligning incentives on a macro level, HSS nurtures effective alignment of incentives between the individual surgeons and the hospital. The physician department maintains these goals by providing the necessary resources to optimize the surgeon’s demand while streamlining both the office and the operating room. These initiatives benefit both the surgeon and hospital by creating clinicians who are clinically busy and academically successful while lowering costs and reducing waste that the hospital has to cover.
With regard to collaboration in supply purchasing, literature suggests surgeons support hospital efforts to limit the number of vendors as long as their own choice of vendor is not constrained [1, 4, 10]. The major drivers of surgeons’ alignment and stance toward cost containment are their tenure with and receipt of financial payments from the vendor [1]. The supply management effectiveness Policy helps to align these divergent goals by affording the surgeon a wide array of implant options while reducing cost at the same time. The surplus saved is then reinvested in research, patient care, and teaching/training—all areas to help improve patient care, an objective all physicians support.
Finally, HSS’s technology transfer and intellectual property policies assist its physicians and staff in protecting and developing ideas competently and efficiently through a critical assessment of the potential value of their ideas and through the protection and management of the rights to those ideas. This alignment can protect both the interest of the surgeon and the hospital. Additionally, the Innovation Fund provides a mechanism to support new concepts and inventions that helps physicians and the institution explore new technology to help the medical community.
A critical element of successful hospitals is the strong partnership and collaboration between physicians and administrators. At HSS, we attribute a substantial portion of the strength of the institution to this partnership. The areas reviewed in this paper are just four examples of how we work to collaborate together to align physician and hospital incentives. We continue to refine and expand our methods of alignment to maximize efficiency and create the best patient care environment possible.
Footnotes
This work was performed at Hospital for Special Surgery, New York, NY.
References
- 1.Burns LR, Housman MG, Booth RE, Koenig A. Implant vendors and hospitals: competing influences over product choice by orthopedic surgeons. Health Care Manage Rev. 2009;34:2–18. [DOI] [PubMed]
- 2.Davies HT, Harrison S. Trends in doctor-manager relationships. BMJ. 2003;326:646–649. [DOI] [PMC free article] [PubMed]
- 3.Dirschl DR, Goodroe J, Thornton DM, Eiland GW. AOA Symposium. Gainsharing in orthopaedics: passing fancy or wave of the future? J Bone Joint Surg Am. 2007;89:2075–2083. [DOI] [PubMed]
- 4.Healy WL. Gainsharing: a primer for orthopaedic surgeons. J Bone Joint Surg Am. 2006;88:1880–1887. [DOI] [PubMed]
- 5.Kaissi A. Manager-physician relationships: an organizational theory perspective. Health Care Manag (Frederick). 2005;24:165–176. [DOI] [PubMed]
- 6.Kwon B, Tromanhauser SG, Banco RJ. The spine service line: optimizing patient-centered spine care. Spine. 2007;32(11 Suppl):S44–S48. [DOI] [PubMed]
- 7.McGowan RA. Strengthening hospital-physician relationships. Healthc Financ Manage. 2004;58:38–40, 42. [PubMed]
- 8.Rundall TG, Davies HT, Hodges CL. Doctor-manager relationships in the United States and the United Kingdom. J Healthc Manag. 2004;49:251–268; discussion 268–270. [PubMed]
- 9.Sanfilippo F, Bendapudi N, Rucci A, Schlesinger L. Strong leadership and teamwork drive culture and performance change: Ohio State University Medical Center 2000-2006. Acad Med. 2008;83:845–854. [DOI] [PubMed]
- 10.Young DW. Using bundled prices and deep discounts to obtain managed care contracts: seller beware! Healthc Financ Manage. 2008;62:98–102, 104. [PubMed]