Abstract
Bone morphogenetic proteins (BMPs) are currently approved for spinal fusion, tibial fracture repair, and maxillofacial bone regeneration. However, BMP pleiotropism, paradoxical activities on precursor cells, and unexpected side effects at local and ectopic sites may limit their usage. Thus, the need remains for alternative osteoinductive factors that provide more bone-specific activities with fewer adverse effects. Nell-1 [Nel-like molecule-1; Nel (a protein highly expressed in neural tissue encoding epidermal growth factor like domain)] is a novel osteogenic protein believed to specifically target cells committed to the osteogenic lineage. The objective of this project is to incorporate Nell-1 into a moldable putty carrier that can adapt to bony defects and deliver Nell-1 to the local microenvironment. We show here that moldability can be achieved by mixing hyaluronan hydrogel with two types of particles: demineralized bone powder for osteoconductivity, and biomimetic apatite-coated alginate/chitosan microparticles for controlled Nell-1 delivery. Besides enhancing overall osteoconductivity of the carrier, the biomimetic apatite coating also provides a more sustained release (∼ 15% cumulative release over 30 days) and greatly reduces the initial burst release that is observed with non-coated alginate/chitosan microparticles (∼ 40% release after 1 day). The efficacy of Nell-1 delivery from these carriers was evaluated in a rat spinal fusion model against Nell-free carriers as controls. 4 weeks post-implantation, Nell-1 enhanced spinal fusion rates as measured by manual palpation, radiographs, high resolution micro-computerized tomography (μCT), and histology. This moldable putty carrier system appears to be a suitable carrier for promoting osteogenesis, and will be further evaluated in larger animal models over longer periods to follow the remodeling of the regenerated bone.
Keywords: Biomimetic apatite, Alginate, Chitosan, Microparticles, Nell-1, Controlled release, Bone tissue engineering
1. Introduction
Loss of bone structures due to bone tumor, trauma, reconstructive surgery, and degenerative disorders remains a significant health problem impairing the quality of life for patients suffering from bone loss. Regeneration of the bone defects by bone grafts is the most frequently used approach for skeletal reconstruction. Autologous bone graft harvested from the iliac crest has been considered the “gold standard” for bone graft material [1-3]. However, donor sites have limited availability and contribute to increased surgical time and hospital stay as well as other complications such as donor site morbidity, pain, infection, pelvic fracture, and wound breakdown. In addition, variations in the osteogenic potential of the graft material make autograft harvest less than ideal [4-7]. As a result, various osteoinductive growth factor-based therapies have been developed in an attempt to find an effective and safer method of bone regeneration.
Among the various osteoinductive factors available, bone morphogenetic proteins (BMPs) are believed to be the most potent osteoinductive factors and have been extensively studied for the treatment of many bone fractures and bone defects [8, 9]. However, BMPs are highly pleiotropic molecules exhibiting high functional heterogeneity during growth and development of numerous tissues [10, 11]. The functional heterogeneity of the BMPs and non-specificity for osteoblasts may explain in part the clinically documented side effects such as unwanted bone formation, unpredictable side effects (such as native bone resorption, implant fracture, soft tissue swelling, osseous overgrowth), and other complications in areas away from the implant site [12]. Furthermore, the use of collagen sponges as carriers may contribute toward the supraphysiological, milligram-level doses of BMP formulations. Hence, there is a need to develop alternative osteoinductive growth factors and delivery strategies to provide an efficient, safe, and desirable bone-specific effect.
We have identified Nell-1 [Nel-like molecule-1; Nel (a protein strongly expressed in neural tissue encoding epidermal growth factor like domain)] to be excessively expressed within active bone forming sites of human craniosynostosis patients [13, 14]. Nell-1 is a secretory molecule containing a signal peptide sequence, an NH2-terminal thrombospondin (TSP)-like module which may bind heparin and anchor Nell-1 to the ECM, five von Willebrand factor C domains which may be involved in homotrimeric oligomerization, and six epidermal growth factor (EGF)-like domains which can bind calcium [15, 16] (Fig. 1). Transgenic mice overexpressing Nell-1 demonstrated calvarial overgrowth and premature suture closure [14]. Conversely, a mouse model with mutated N-ethyl-N-nitrosourea-induced alleles, including Nell-1, resulted in cranial and other vertebral skeletal defects [17]. Furthermore, Nell-1 is directly regulated by runt-related transcription factor 2 (Runx2/Cbfa1), which is essential for osteoblast differentiation, further suggesting its osteogenic specificity [18]. Taken together, the data suggest that Nell-1 has a distinct and specialized role in bone formation.
Figure 1.
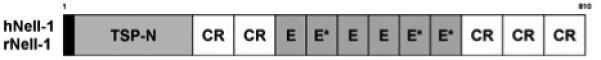
Schematic structure of human and rat Nell-1. Nell-1 is highly conserved across species. Human and rat Nell-1 share a 93% homology in predicted amino acids. Nell-1 contains several highly conserved motifs including a secretory signal peptide (black box), NH2-terminal TSP-1-like module (TSP-N), von Willebrand factor C domains (CR), EGF-like domains (E), and Ca2+ binding EGF-like domains (E*).
Moreover, because Nell-1 is a secreted protein that can be delivered extracellularly, controlled delivery systems can be used to maximize biological efficiency. Indeed, delivery of recombinant Nell-1 protein in pre-formed polyglycolide-lactide scaffolds has been shown to accelerate osteogenic differentiation in vitro and calvarial bone formation in vivo [19]. The osteogenic potential of Nell-1 to induce in vivo calvarial regeneration was equivalent to BMP-2.
In this study, we report a moldable carrier formulation for controlled local Nell-1 delivery. Chitosan and alginate are naturally occurring polymers used for pharmaceutical and biomedical applications as drug delivery systems [20-23]. In addition to having biocompatible and biodegradable characteristics, one of the interesting properties of chitosan is its cationic nature and high charge density in solution. This allows the formation of stable ionic complexes with multivalent water-soluble anionic polymers under mild physiological conditions [24, 25]. Alginate is an anionic polysaccharide and forms complexes with polycations such as calcium, chitosan, polylysine [26, 27]. These properties have been widely used for the delivery of various proteins and for the encapsulation of cells. To enhance the osteoconductivity of alginate/chitosan, we coated these particles with a biomimetic apatite coating process [28-30]. Alginate/chitosan particles were produced by ionic gelation methods and incubated in simulated body fluids to obtain biomimetic apatite layers that facilitate bone formation. Since Nell-1 (isoelectric point < 6) is negatively charged at neutral pH, we hypothesize that apatite coating can reduce initial burst release by comparing release kinetics of recombinant human Nell-1 protein from apatite-coated and un-coated alginate/chitosan particles. The in vivo osteogenic capacity of the particles loaded with Nell-1 was evaluated in a rat spinal fusion model.
2. Materials and methods
2.1. Materials
Chitosan (Mw 400,000, 85% deacetylated) and sodium alginate (viscosity 250 cP, 2% w/v) were purchased from Sigma-Aldrich Inc. (St. Louis, MO). Calcium chloride was purchased from EMD Chemicals Inc. (Gibbstown, NJ). Sheep demineralized bone particles (212∼850 μm) and recombinant hyaluronan were generously donated by the Musculoskeletal Transplant Foundation (Edison, NJ). Recombinant human Nell-1 protein (rhNell-1) was produced and purified from CHO cells (Aragen Bioscience, Morgan Hill, CA).
2.2. Preparation of alginate/chitosan microparticles
Alginate/chitosan microparticles were prepared by an ionic gelation method [31]. Alginate (0.1% w/v) was prepared by dissolving sodium alginate in distilled water and chitosan (0.1% w/v) was prepared by dissolving chitosan in 0.05% acetic acid aqueous solution. A solution of alginate (0.1%, w/v) was added drop by drop to 0.75 mM calcium chloride aqueous solution containing chitosan under gentle stirring. The ratio of sodium alginate: calcium chloride: chitosan was 6:1:6 (w/w/w). The obtained microparticles were collected by centrifugation at 4,500 g for 30 min and were washed three times with distilled water.
2.3. Biomimetic apatite coating process
Apatite coating solution was prepared as described in our earlier studies [28-30]. Briefly, supersaturated simulated body fluid (SBF) solution was prepared by sequentially dissolving CaCl2, MgCl2·6H2O, NaHCO3, and K2HPO4·3H2O in ddH2O. Solution pH was lowered to 6 by adding 1M hydrochloric acid to increase the solubility. Na2SO4, KCl, and NaCl were added and the final pH was adjusted to 6.5 (SBF 1). Mg2+ and HCO3- free SBF (SBF 2) was prepared by adding CaCl2 and K2HPO4·3H2O in ddH2O and pH was lowered to 6. KCl and NaCl were added and the final pH was adjusted to 6.8. All solutions were sterile filtered through a 0.22 μm PES membrane (Nalgene, NY). The obtained alginate/chitosan particles were incubated in SBF 1 for 6 h and changed to Mg2+ and HCO3- free SBF 2 for another 12 h at 37°C under gentle stirring. Coated particles were washed with ddH2O to remove excess ions and lyophilized prior to further studies.
2.4. Characterization of apatite coating
The surface morphology of the microparticles after apatite coating was observed using scanning electron microscopy (SEM, JEOL JSM-6700, Tokyo, Japan). Prior to SEM analysis, the samples were mounted on aluminum stubs and carbon coated.
Attenuated Total Reflection-Fourier Transform Infrared Spectroscopy (ATR-FTIR) was used to analyze the chemical structure of the microparticles before and after incubation in SBF. The samples were placed in contact with diamond ATR window. FTIR (Avatar 360 Thermo Nicolet spectrometer) transmittance spectra from 2000 to 400 cm-1 wavenumbers were obtained.
2.5. In vitro release of protein
To determine if apatite coating can reduce initial burst release, the release kinetics of recombinant human Nell-1 protein from apatite-coated and un-coated alginate/chitosan particles was compared. After apatite coating, 100 μg recombinant human Nell-1 (in PBS) was lyophilized onto 50 mg of particles, and Nell-loaded particles were immersed in 1 ml of 10 mM phosphate buffered saline (PBS, pH 7.4) at 37°C under gentle shaking. The particles were centrifuged and the incubating solution was replaced with 1 mL of fresh solution at predetermined time points over 30 days. The amount of released Nell-1 protein in the supernatant was measured using the 3-(4-carboxybenzoyl)quinoline-2-carboxaldehyde (CBQCA) protein assay. The CBQCA protein assay kit was chosen because it is very reliable and sensitive assay to quantify proteins in solution with detection sensitivity as low as 10 ng of protein per mL. We found the BCA assay to be reliable at protein concentrations above 10 μg/mL, and microBCA to be reliable above 1 μg/ml. The experiment was performed in triplicate and the amount of protein released was expressed as a percentage of the initial amount of protein loaded.
2.6. Moldable putty preparation
For the experimental group, 10 μg recombinant human Nell-1 (in PBS) was lyophilized onto 10 mg of apatite-coated alginate/chitosan particles. For Nell-free control, PBS alone was lyophilized onto alginate/chitosan particles. Prior to implantation, each respective powder was resuspended in PBS and mixed with 100 mg of demineralized bone powder and 220 mg of hyaluronan to form moldable putty.
2.7. Rat spinal fusion model
Male athymic rats were obtained from Taconic (Hudson, NY) at 10-12 weeks of age. All animals were maintained and handled in compliance with the institutional regulations established and approved by the Animal Research Committee at the University of California, Los Angeles. Rats were housed in cages under standard laboratory conditions and fed rat chow and water ad libitum. All surgical protocols were approved by the Animal Research Committee before animal experimentation. 5% isoflurane was administered to induce anesthesia, followed by 2% isoflurane via nose cone to maintain sedation. The lumbar region was shaved and surgically prepped with three alternating washes of betadine and alcohol. One longitudinal incision in the dorsal skin at the midline of the lumbar spine and two longitudinal fascial incisions approximately 3 mm lateral to the spinus processes were made. The L4 and L5 transverse processes were then bilaterally exposed and decorticated with a high-speed burr. The implants were positioned over the L4-5 transverse processes. 4-0 Vicryl absorbable sutures were used to close the fascia and skin. Postoperatively, the rats were provided with analgesics (0.05 mg/kg buprenorphine) for two days and antibiotics (trimethoprim/sulfamethoxazole) for seven days. Animals were sacrificed at 4 weeks after implantation to determine spinal fusion by manual palpation, radiographs, microCT analysis, and histology (n = 5, per condition).
2.8. Manual palpation and radiograph
Fusion with the implanted graft was assessed by manual palpation and high-resolution posteroanterior radiographs. Following euthanasia via CO2 asphyxiation, the spines of the rats were dissected and extracted. Three independent observers palpated the spines and assessed if there was any movement within the intervertebral spaces of L4 and L5. The spines were classified as either fused (no mobility) or not fused (mobility). At least two of the three evaluators had to assess the spine to be fused for it to be categorized as being fused. Radiographs were also utilized to determine if fusion occurred. Fusion was noted when continuous bony trabeculation is clearly observed between the L4-L5 region.
2.9. Three-dimensional micro-computerized tomography scanning
To quantify bone formation, the dissected spines were placed in 10% buffered formalin for a minimum of 48 hours. Upon fixation, three-dimensional micro-computerized tomography (μCT) acquisition and analysis of the spines were obtained using the Scanco μCT 40 (Scanco, Southeastern, PA) at the highest scanning resolution (10 μm). The microCT data was collected at 55 kVp and 72 μA and reconstructed using a cone-beam algorithm provided by Scanco. Visualization and 3D reconstruction of the data was performed using microCT analysis software (Scanco Medical). Continuous bone formation was assessed by analyzing reconstructed coronal cross-sectional images. In addition, bone volume/total volume (BV/TV) between L4 and L5 transverse processes was calculated with CT-based morphometric analysis.
2.10. Histological evaluation
The specimens were decalcified using standard 10% decalcifying HCl solution (Cal-Ex) (Fisher Scientific, Fairlawn, NJ) for five to seven days. The decalcified spines were then washed with running tap water and transferred to 70% ethanol. Coronal sections were cut to include the implant and L4-L5 transverse processes. The specimens were then embedded in paraffin wax and tissue sections were cut at 5 μm. Hematoxylin and eosin staining was performed.
2.11. Statistical analysis
For the morphometric analysis, Student’s t test was used to compare differences between two groups. p < 0.05 was considered statistically significant.
3. Results
3.1. Characterization of apatite-coated microparticles
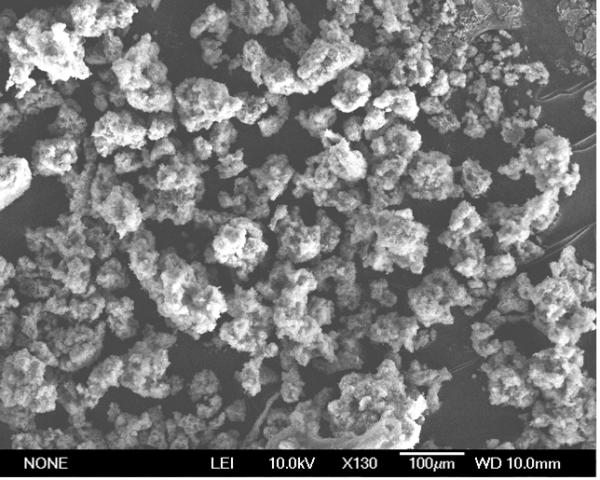
Alginate/chitosan particles fabricated in this study had a size distribution in the range of 10∼60 μm and a mean diameter of 27 μm from image analysis of micrographs using Bioquant software. Apatite coating of the alginate/chitosan particles was achieved by incubating alginate/chitosan particles in simulated body fluids. A uniform layer of apatite coating was observed on the surface of particles and the apatite coating exhibited plate-like morphology (Fig. 2b).
Figure 2.

SEM micrographs of alginate/chitosan microparticles prepared by ionic gelation methods after immersing in SBF. A plate-like apatite layer was formed on the surface of microparticles after immersing in SBF (b). Alginate/chitosan microparticles prior to apatite coating (c).
Formation of apatite layer on the particles was also confirmed with ATR-FTIR (Fig. 3). ATR-FTIR spectra for the mineralized alginate/chitosan particles exhibited the sharp characteristic peaks of the phosphate group (PO43-) (around 1020 (ν3), 960 (ν1), 600 (ν4), and 560 cm-1 (ν4)) and carbonate group (CO32-) (around 1640 (ν3) and 860 cm-1 (ν2)) indicating carbonated hydroxyapatite [Ca10(PO4)3(CO3)3(OH)2] structure formation.
Figure 3.

ATR-FTIR spectra of alginate/chitosan microparticles (a) and alginate/chitosan microparticles after immersing in SBF (b). After immersing in SBF, alginate/chitosan microparticles exhibited the sharp characteristic peaks of the phosphate group (PO43-) (around 1020 (ν3), 960 (ν1), 600 (ν4), and 560 cm-1 (ν4)) and carbonate group (CO32-) (around 1640 (ν3) and 860 cm-1 (ν2)).
3.2. In vitro release of proteins from microparticles
To determine if apatite coating can reduce initial burst release, the release kinetics of recombinant human Nell-1 protein from apatite-coated and uncoated alginate/chitosan particles was investigated by incubating the microparticles in PBS (Fig. 4). As expected, the release of Nell-1 from uncoated alginate/chitosan microparticles exhibited a rapid burst release profile. Approximately 40% of the initially loaded Nell-1 was released during the first day, followed by slow release during the subsequent month. We have investigated the release kinetics for the various formulations of the microparticles with alginate/chitosan ratios of 5:1, 2.5:1, 1.6:1, 1:1. Release profiles were similar for all experimental formulations, with significant initial burst releases. The alginate/chitosan ratio of 1:1 was chosen in the subsequent experiments because it provided the highest yield. In contrast, the burst release of Nell-1 was significantly reduced by the apatite coating. Approximately 2% of Nell-1 was released from apatite-coated alginate/chitosan microparticles during day 1, and Nell-1 was steadily released at 0.5%/day up to 15% after 30 days. Relative to their uncoated counterparts, the release of Nell-1 from apatite-coated alginate/chitosan microparticles was well controlled and showed a near zero-order release profile over the experimental time period.
Figure 4.

In vitro release of Nell-1 from alginate/chitosan (AG/CS) microparticles in PBS. Sustained release of Nell-1 was observed from the apatite-coated alginate/chitosan microparticles (n=3, mean ± SD).
3.3. Fusion assessment
At four weeks post implantation, spinal fusion was assessed by manually palpating the harvested spines for any anterior-posterior or lateral movements. Fusion rate in the spines treated with Nell-1 was higher than that of the control spines (Table 1). Three of the five rat spines implanted with Nell-1 were considered fused without any intersegmental motion. None of the five rat spines implanted with Nell-free controls fused. Radiographic images showed new bone bridging the L4 and L5 transverse processes in four of five rats implanted with Nell-1 (Fig. 5a). Only one of five rats implanted with Nell-free controls showed a bony bridge and the other four rats showed small bone mass with gaps between the host bone and implanted materials (Fig. 5d).
Table 1.
Fusion assessment results
| Fusion rate (%) |
||
|---|---|---|
| Control | Nell-1 | |
| Manual palpation | 0 | 60 |
| Radiograph | 20 | 80 |
| Micro-CT | 0 | 60 |
Figure 5.
Radiographic images of Nell-1 treated spine (a) and PBS treated control group (d) 4 weeks after implantation. Micro-computerized tomography (μCT) scanning of Nell-1 (b, c) and PBS (e, f) treated spine: middle panels (b, e) show reconstructed 3D images; right panels (c, f) show coronal section images of 3D μCT. New bone formation bridging the transverse processes of L4 and L5 was observed in the Nell-1 treated spine. For the control group, there was no evidence of a bony bridge and large clefts were observed between two transverse processes (arrows). (g) Quantification of bone volume/total volume (BV/TV) between L4 and L5 transverse processes. Significant difference from control was noted; *p < 0.01.
3.4 Three-dimensional micro-computerized tomography images
Manual palpation and radiographic findings of bone formation in the spines were confirmed by 3D microCT analysis. Three of five rat spines implanted with Nell-1 demonstrated new bone formation between the transverse processes of L4 and L5 (Fig. 5b). Nell-free controls induced minimal spinal fusion without close contact of tissue mass with the transverse processes in the graft region (Fig. 5e). Additionally, multiple coronal sections were reconstructed to evaluate the formation of a bony bridge between the transverse processes. Bone masses bridging the transverse processes of L4 and L5 formed in the fused spines implanted with Nell-1 (Fig. 5c). For the spines implanted with Nell-free controls, there was no evidence of a bony bridge between L4 and L5 transverse processes and large clefts were observed between the two transverse processes (Fig. 5f). MicroCT-based morphometric analysis demonstrated significantly higher bone volume between the transverse processes in the Nell-1 group (p = 0.007) compared to the Nell-free control group (Fig. 5g).
3.5. Histological analysis
The quality of newly formed bone was further evaluated by hematoxylin-eosin staining. Nell-1 delivery promoted more bone formation compared to the control group. Cortical-like bone bridges connecting two involved transverse processes were observed in the fused Nell-1 samples (Fig. 6a). New bone tissue was forming from the decorticated transverse processes and cartilaginous tissues were detected around the demineralized bone matrix material suggesting endochondral bone formation (Fig. 6c and 6e). There was no significant inflammatory reaction in the graft area. In contrast, there was minimal evidence of new bone formation with the absence of a bony bridge formation in the intertransverse areas in the Nell-free control group (Fig. 6b). Under high magnification, fibrous tissues were more prominent in the implant area of the Nell-free control samples (Fig. 6d and 6f). The implanted particles were not detectable in the graft area, presumably because the concentration of particles initially mixed with bone putty is too low. We have previously injected the microparticles into the muscle pouch of rats, and histological analyses showed no evidence of migration of the particles to the distant tissues at 4 weeks.
Figure 6.
Histological features of the graft site. Hematoxylin-eosin staining on Nell-1 treated (a, c, e) and PBS treated (b, d, f) spine 4 weeks after implantation. Arrows indicate cortical-natured bone bridges connecting two involved transverse processes identified by dotted lines (a). Cartilaginous tissues (arrowheads) were detected around the demineralized bone matrix material in Nell-1 group (e). Original magnification: 9.8× (a, b) and 100× (c-f).
4. Discussion
Bone regeneration treatments using osteoinductive factors such as BMPs appear capable of inducing bone formation. However, a significant drawback of the current protein-based therapies is their lack of specificity for osteoblasts. Most known osteoinductive BMPs are involved in multiple physiologic processes and have important roles in organogenesis [32]. From a clinical perspective, the functional heterogeneity and administration of milligram doses of BMPs may limit their use due to unwanted bone formation, other unpredictable side effects, and cost considerations. Runx2/Cbfa1 is essential for osteoblast formation and function. BMPs are known to upregulate Runx2/Cbfa1 expression [33-36], resulting in the induction of osteogenic differentiation of both osseous and nonosseous mesenchymal cells [37, 38]. Therefore, there is a need to identify crucial soluble downstream mediators of Runx2/Cbfa1 for protein-based therapies. Nell-1 has three Runx2/Cbfa1 binding sites (osteoblast-specific cis-acting element 2 [OSE2]) within its promoter. This suggests that Nell-1 acts as a critical downstream mediator of Runx2/Cbfa1 in regulating osteogenic differentiation. Previous in vitro and in vivo data confirm that Nell-1, unlike BMPs, act specifically on further differentiated osteogenic lineage cells [18].
Although very small quantities of Nell-1 are required for osteoinduction, high doses of Nell-1 are necessary in direct therapeutic application. This is due to a short half life and rapid degradation of proteins once they are secreted. Our previous studies demonstrated that Nell-1 is able to successfully fuse the posterior lateral lumbar spine of a rat using an adenovirus overexpressing Nell-1 [39]. Although gene therapy can provide essential osteoinductive factors, the current status of gene therapy limits actual clinical application. Human application is impractical because of the issues related to virus safety and immunogenicity. In this study, we have developed a novel growth factor delivery system consisting of polysaccharide-based microparticles and a biomimetic apatite layer on its surface for use as an injectable bone substitute. Polysaccharides, such as chitosan and alginate used in this study, are naturally derived polymers. They are cost-effective, biodegradable, and biocompatible. Additionally, they can be easily manipulated into various forms such as beads, micro/nano particles, and gels under mild conditions [20-23].
Chitosan is enzymatically degraded in vivo by lysozymes, which target acetylated residues. Proteolytic enzymes may also exhibit some activity with chitosan. Resulting degradation products are chitosan oligosaccharides of different lengths [40]. Degradation kinetics are inversely related to the degree of crystallinity, which is determined by the degree of deacetylation. Highly deacetylated forms of chitosan, typically greater than 85%, show the lowest degradation rates and may last several months in vivo. Less deacetylated and therefore less crystalline chitosan degrades more rapidly. To achieve desired rapid degradation, side chains have been added to alter molecular chain packing and increase the amorphous fraction. Alginate gels degradation is less controlled and is believed to involve a de-crosslinking mechanism, in which the divalent cations (typically calcium) are exchanged with monovalent cations from surrounding media. Alginate gels undergo slow dissolution (∼ 8 weeks) in vivo [41] and the de-crosslinking site may release high molecular weight strands that must be cleared from the body. The ionic-crosslinked alginate/chitosan microparticles reported in this study may have slower degradation rates than the individual un-crosslinked components because chitosan-alginate complexation retards the dissolution of alginate particles. It was shown that alginate/chitosan scaffolds implanted into the muscle pouch of the rat were completely degraded at 12 weeks and well integrated with adjacent muscle without adverse inflammatory or foreign body reactions [42].
In previous studies, we have developed a rapid biomimetic processing strategy. This strategy confers uniform, biocompatible apatite coatings of controlled composition throughout the pores of complex three-dimensional scaffolds via modification of the conventional simulated body fluid immersion approach [28-30]. By identifying of the dominant processing parameters during apatite formation and limiting the availability of essential ions governing nucleation and growth kinetics, we accelerated the conventional biomimetic apatite coating process from 14-21 days to 1-2 days. This created uniform, osteoconductive coatings in three-dimensional complex structures. We have demonstrated that apatite microenvironments derived from this process may enhance cellular expression of mature osteoblastic genes (osteopontin, osteocalcin, bone sialoproteins) in two-dimensional and three-dimensional systems.
In this study, Nell-1 was lyophilized onto alginate/chitosan particles and its in vitro release kinetics were evaluated. A burst release pattern of Nell-1 was observed from alginate/chitosan particles, while Nell-1 showed more sustained release from apatite-coated particles (Fig. 4). At pH 7.4, Nell-1 carries a net negative charge (isoelectric point = 5.66) and can interact electrostatically with cationic chitosan. In contrast, there may be electrostatic repulsions between Nell-1 and the alginate carboxylic groups. Varying the alginate:chitosan ratios 5:1, 2.5:1, 1.6:1, 1:1 within the range that prevented particle aggregation did not significantly alter Nell-loading or initial release kinetics. Calcium phosphate is widely used as a delivery carrier for DNA, protein, and peptide because of its high affinity for macromolecules [43-45]. The apatite coating increased the protein retention capacity of the particles, such that we could load milligram-level doses onto apatite-coated particles. Sustained release of Nell-1 from apatite-coated particles can be explained by the electrostatic interaction between negatively charged Nell-1 and positively charged adsorption sites of apatites. It is also possible that high surface area due to the plate-like morphology of the particles presented more binding surfaces for non-specific protein absorption. Furthermore, crystallinity and solubility of hydroxyapatite particles can also influence protein release kinetics [46]. Other studies have demonstrated that the surface charge and texture of hydroxyapatite particles influence the adsorption of proteins and affect the protein release from the particles [47]. Since the final apatite formation and structure can be controlled by regulating apatite coating process parameters such as ionic strength, pH, and concentration of crystal growth inhibitor (Mg2+ and HCO3-) in SBF solution [28, 48], temporal control over the delivery of proteins can be achieved by regulating these coating process parameters.
This paper focuses on the delivery of Nell-1 from an apatite surface. Efforts are ongoing to incorporate Nell-1 into the core of the alginate/chitosan microparticle in order to achieve controlled release over longer periods. Our alginate/chitosan particles are designed simply as protein delivery vehicles, and not to provide mechanical support. We believe that if they provide the proper protein loading and release kinetics, then they can be incorporated into other scaffolds. It is also interesting to note that the apatite-coated particles exhibited less aggregation compared to uncoated particles. It is possible that the plate-like morphology of the apatite-coated particles inhibited interparticle cohesion, reducing particle aggregation due to surface charge repulsion. Regardless of the mechanism, the apatite coating facilitated mixing with demineralized bone and hyaluronan to produce a moldable putty. Our current putty formulation was designed to be easily shaped for packing into the osseous defects, and not optimized for weight bearing. This putty is very similar in handling characteristics as commercially available bone putty (DBX, Synthes).
The implantation of the microparticles loaded with Nell-1 enhanced spinal fusion rates in rats as detected by manual palpation, radiographs, high resolution μCT, and histology. Taken together, these data suggest that this putty formulation for local Nell-1 delivery represents a practical approach for future clinical product development of safe and effective orthobiologic formulations.
5. Conclusions
A moldable putty carrier for controlled delivery of Nell-1 (osteoinductive growth factor which provides a more bone-specific effect) was developed as an injectable bone substitute formulation using alginate-chitosan microparticles. Release studies demonstrated that apatite-coated microparticles serve as a more efficient carrier of Nell-1, providing sustained delivery of this protein. Furthermore, implantation of the microparticles loaded with Nell-1 improved spinal fusion rates. Thus, this delivery system might be a useful adjunct for alternative osteoinductive therapeutics.
Acknowledgements
This work was supported by UC Discovery grant Bio 07-10677 and NIH/NIDCR R01 DE016107.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
Drs. Wu, Ting, and Soo are co-founders of Bone Biologics Inc., which licensed Nell-1 related patent application from UCLA.
References
- 1.Ozaki W, Buchman SR, Goldstein SA, Fyhrie DP. A comparative analysis of the microarchitecture of cortical membranous and cortical endochondral onlay bone grafts in the craniofacial skeleton. Plast Reconstr Surg. 1999;104:139–47. [PubMed] [Google Scholar]
- 2.Canady JW, Zeitler DP, Thompson SA, Nicholas CD. Suitability of the Iliac Crest as a Site for Harvest of Autogenous Bone-Grafts. Cleft Palate-Cran J. 1993;30:579–81. doi: 10.1597/1545-1569_1993_030_0579_sotica_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Strong EB, Moulthrop T. Calvarial bone graft harvest: A new technique. Otolaryng Head Neck. 2000;123:547–52. doi: 10.1067/mhn.2000.110541. [DOI] [PubMed] [Google Scholar]
- 4.Laurie SWS, Kaban LB, Mulliken JB, Murray JE. Donor-Site Morbidity after Harvesting Rib and Iliac Bone. Plast Reconstr Surg. 1984;73:933–8. doi: 10.1097/00006534-198406000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Kurz LT, Garfin SR, Booth RE. Harvesting Autogenous Iliac Bone-Grafts - a Review of Complications and Techniques. Spine. 1989;14:1324–31. doi: 10.1097/00007632-198912000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Kline RM, Wolfe SA. Complications Associated with the Harvesting of Cranial Bone-Grafts. Plast Reconstr Surg. 1995;95:5–13. [PubMed] [Google Scholar]
- 7.Wolfe SA. Complications of harvesting cranial bone grafts. Plast Reconstr Surg. 1996;98:567. doi: 10.1097/00006534-199609000-00039. [DOI] [PubMed] [Google Scholar]
- 8.Kang Q, Sun MH, Cheng H, Peng Y, Montag AG, Deyrup AT, et al. Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery. Gene Ther. 2004;11:1312–20. doi: 10.1038/sj.gt.3302298. [DOI] [PubMed] [Google Scholar]
- 9.Govender S, Csimma C, Genant HK, Valentin-Opran A, Grp BS. Recombinant human bone morphogenetic protein-2 for treatment of open tibial fractures - A prospective, controlled, randomized study of four hundred and fifty patients. J Bone Joint Surg Am. 2002;84A:2123–34. doi: 10.2106/00004623-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Ducy P, Karsenty G. The family of bone morphogenetic proteins. Kidney Int. 2000;57:2207–14. doi: 10.1046/j.1523-1755.2000.00081.x. [DOI] [PubMed] [Google Scholar]
- 11.Wang JC, Kanim LEA, Yoo S, Campbell PA, Berk AJ, Lieberman JR. Effect of regional gene therapy with bone morphogenetic protein-2-producing bone marrow cells on spinal fusion in rats. J Bone Joint Surg Am. 2003;85A:905–11. doi: 10.2106/00004623-200305000-00020. [DOI] [PubMed] [Google Scholar]
- 12.van den Bergh JPA, ten Bruggenkate CM, Groeneveld HHJ, Burger EH, Tuinzing DB. Recombinant human bone morphogenetic protein-7 in maxillary sinus floor elevation surgery in 3 patients compared to autogenous bone grafts - A clinical pilot study. J Clin Periodontol. 2000;27:627–36. doi: 10.1034/j.1600-051x.2000.027009627.x. [DOI] [PubMed] [Google Scholar]
- 13.Ting K, Vastardis H, Mulliken JB, Soo C, Tieu A, Do H, et al. Human NELL-1 expressed in unilateral coronal synostosis. J Bone Miner Res. 1999;14:80–9. doi: 10.1359/jbmr.1999.14.1.80. [DOI] [PubMed] [Google Scholar]
- 14.Zhang XL, Kuroda S, Carpenter D, Nishimura I, Soo C, Moats R, et al. Craniosynostosis in transgenic mice overexpressing Nell-1. J Clin Invest. 2002;110:861–70. doi: 10.1172/JCI15375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuroda S, Tanizawa K. Involvement of epidermal growth factor-like domain of NELL proteins in the novel protein-protein interaction with protein kinase C. Biochem Bioph Res Co. 1999;265:752–7. doi: 10.1006/bbrc.1999.1753. [DOI] [PubMed] [Google Scholar]
- 16.Kuroda S, Oyasu M, Kawakami M, Kanayama N, Tanizawa K, Saito N, et al. Biochemical characterization and expression analysis of neural thrombospondin-1-like proteins NELL1 and NELL2. Biochem Bioph Res Co. 1999;265:79–86. doi: 10.1006/bbrc.1999.1638. [DOI] [PubMed] [Google Scholar]
- 17.Desai J, Shannon ME, Johnson MD, Ruff DW, Hughes LA, Kerley MK, et al. Nell1-deficient mice have reduced expression of extracellular matrix proteins causing cranial and vertebral defects. Hum Mol Genet. 2006;15:1329–41. doi: 10.1093/hmg/ddl053. [DOI] [PubMed] [Google Scholar]
- 18.Truong T, Zhang XL, Pathmanathan D, Soo C, Ting K. Craniosynostosis-associated gene Nell-1 is regulated by Runx2. J Bone Miner Res. 2007;22:7–18. doi: 10.1359/jbmr.061012. [DOI] [PubMed] [Google Scholar]
- 19.Aghaloo T, Cowan CM, Chou YF, Zhang XL, Lee HF, Miao S, et al. Nell-1-induced bone regeneration in calvarial defects. Am J Pathol. 2006;169:903–15. doi: 10.2353/ajpath.2006.051210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Martino A, Sittinger M, Risbud MV. Chitosan: A versatile biopolymer for orthopaedic tissue-engineering. Biomaterials. 2005;26:5983–90. doi: 10.1016/j.biomaterials.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 21.Tonnesen HH, Karlsen J. Alginate in drug delivery systems. Drug Dev Ind Pharm. 2002;28:621–30. doi: 10.1081/ddc-120003853. [DOI] [PubMed] [Google Scholar]
- 22.Rajaonarivony M, Vauthier C, Couarraze G, Puisieux F, Couvreur P. Development of a New Drug Carrier Made from Alginate. J Pharm Sci. 1993;82:912–7. doi: 10.1002/jps.2600820909. [DOI] [PubMed] [Google Scholar]
- 23.Dodane V, Vilivalam VD. Pharmaceutical applications of chitosan. Pharm Sci Technol To. 1998;1:246–53. [Google Scholar]
- 24.Calvo P, RemunanLopez C, VilaJato JL, Alonso MJ. Novel hydrophilic chitosan-polyethylene oxide nanoparticles as protein carriers. J Appl Polym Sci. 1997;63:125–32. [Google Scholar]
- 25.Shu X, Zhu KJ. A novel approach to prepare tripolyphosphate/chitosan complex beads for controlled release drug delivery. Int J Pharm. 2000;201:51–8. doi: 10.1016/s0378-5173(00)00403-8. [DOI] [PubMed] [Google Scholar]
- 26.Becker TA, Kipke DR, Brandon T. Calcium alginate gel: A biocompatible and mechanically stable polymer for endovascular embolization. J Biomed Mater Res. 2001;54:76–86. doi: 10.1002/1097-4636(200101)54:1<76::aid-jbm9>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 27.Coppi G, Iannuccelli V, Leo E, Bernabei MT, Cameroni R. Chitosan-alginate microparticles as a protein carrier. Drug Dev Ind Pharm. 2001;27:393–400. doi: 10.1081/ddc-100104314. [DOI] [PubMed] [Google Scholar]
- 28.Chou YF, Chiou WA, Xu YH, Dunn JCY, Wu BM. The effect of pH on the structural evolution of accelerated biomimetic apatite. Biomaterials. 2004;25:5323–31. doi: 10.1016/j.biomaterials.2003.12.037. [DOI] [PubMed] [Google Scholar]
- 29.Chou YF, Dunn JCY, Wu BM. In vitro response of MC3T3-E1 preosteoblasts within three-dimensional apatite-coated PLGA scaffolds. J Biomed Mater Res B. 2005;75B:81–90. doi: 10.1002/jbm.b.30261. [DOI] [PubMed] [Google Scholar]
- 30.Chou YF, Huang WB, Dunn JCY, Miller TA, Wu BM. The effect of biomimetic apatite structure on osteoblast viability, proliferation, and gene expression. Biomaterials. 2005;26:285–95. doi: 10.1016/j.biomaterials.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Rodriguez ML, Holgado MA, Sanchez-Lafuente C, Rabasco AM, Fini A. Alginate/chitosan particulate systems for sodium diclofenac release. Int J Pharm. 2002;232:225–34. doi: 10.1016/s0378-5173(01)00915-2. [DOI] [PubMed] [Google Scholar]
- 32.Zhao GQ. Consequences of knocking out BMP signaling in the mouse. Genesis. 2003;35:43–56. doi: 10.1002/gene.10167. [DOI] [PubMed] [Google Scholar]
- 33.Nakashima K, de Crombrugghe B. Transcriptional mechanisms in osteoblast differentiation and bone formation. Trends Genet. 2003;19:458–66. doi: 10.1016/S0168-9525(03)00176-8. [DOI] [PubMed] [Google Scholar]
- 34.Komori T, Yagi H, Nomura S, Yamaguchi A, Sasaki K, Deguchi K, et al. Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell. 1997;89:755–64. doi: 10.1016/s0092-8674(00)80258-5. [DOI] [PubMed] [Google Scholar]
- 35.Yamaguchi A, Komori T, Suda T. Regulation of osteoblast differentiation mediated by bone morphogenetic proteins, hedgehogs, and Cbfa1. Endocr Rev. 2000;21:393–411. doi: 10.1210/edrv.21.4.0403. [DOI] [PubMed] [Google Scholar]
- 36.Lee KS, Hong SH, Bae SC. Both the Smad and p38 MAPK pathways play a crucial role in Runx2 expression following induction by transforming growth factor-beta and bone morphogenetic protein. Oncogene. 2002;21:7156–63. doi: 10.1038/sj.onc.1205937. [DOI] [PubMed] [Google Scholar]
- 37.Ahrens M, Ankenbauer T, Schroder D, Hollnagel A, Mayer H, Gross G. Expression of Human Bone Morphogenetic Proteins-2 or Proteins-4 in Murine Mesenchymal Progenitor C3h10t1/2 Cells Induces Differentiation into Distinct Mesenchymal Cell Lineages. DNA Cell Biol. 1993;12:871–80. doi: 10.1089/dna.1993.12.871. [DOI] [PubMed] [Google Scholar]
- 38.Katagiri T, Yamaguchi A, Komaki M, Abe E, Takahashi N, Ikeda T, et al. Bone Morphogenetic Protein-2 Converts the Differentiation Pathway of C2c12 Myoblasts into the Osteoblast Lineage. J Cell Biol. 1994;127:1755–66. doi: 10.1083/jcb.127.6.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lu SS, Zhang X, Soo C, Hsu T, Napoli A, Aghaloo T, et al. The osteoinductive properties of Nell-1 in a rat spinal fusion model. Spine J. 2007;7:50–60. doi: 10.1016/j.spinee.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 40.Suh JKF, Matthew HWT. Application of chitosan-based polysaccharide biomaterials in cartilage tissue engineering: a review. Biomaterials. 2000;21:2589–98. doi: 10.1016/s0142-9612(00)00126-5. [DOI] [PubMed] [Google Scholar]
- 41.Cai XX, Lin YF, Ou GM, Luo E, Man Y, Yuan QA, et al. Ectopic osteogenesis and chondrogenesis of bone marrow stromal stem cells in alginate system. Cell Biol Int. 2007;31:776–83. doi: 10.1016/j.cellbi.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 42.Li ZS, Ramay HR, Hauch KD, Xiao DM, Zhang MQ. Chitosan-alginate hybrid scaffolds for bone tissue engineering. Biomaterials. 2005;26:3919–28. doi: 10.1016/j.biomaterials.2004.09.062. [DOI] [PubMed] [Google Scholar]
- 43.Shen H, Tan J, Saltzman WM. Surface-mediated gene transfer from nanocomposites of controlled texture. Nat Mater. 2004;3:569–74. doi: 10.1038/nmat1179. [DOI] [PubMed] [Google Scholar]
- 44.Olton D, Li JH, Wilson ME, Rogers T, Close J, Huang L, et al. Nanostructured calcium phosphates (NanoCaPs) for non-viral gene delivery: Influence of the synthesis parameters on transfection efficiency. Biomaterials. 2007;28:1267–79. doi: 10.1016/j.biomaterials.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 45.Habraken WJEM, Wolke JGC, Jansen JA. Ceramic composites as matrices and scaffolds for drug delivery in tissue engineering. Adv Drug Deliver Rev. 2007;59:234–48. doi: 10.1016/j.addr.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 46.Matsumoto T, Okazaki M, Inoue M, Yamaguchi S, Kusunose T, Toyonaga T, et al. Hydroxyapatite particles as a controlled release carrier of protein. Biomaterials. 2004;25:3807–12. doi: 10.1016/j.biomaterials.2003.10.081. [DOI] [PubMed] [Google Scholar]
- 47.Kandori K, Shimizu T, Yasukawa A, Ishikawa T. Adsorption of Bovine Serum-Albumin onto Synthetic Calcium Hydroxyapatite - Influence of Particle Texture. Colloid Surface B. 1995;5:81–7. [Google Scholar]
- 48.Barrere F, van Blitterswijk CA, de Groot K, Layrolle P. Influence of ionic strength and carbonate on the Ca-P coating formation from SBFx5 solution. Biomaterials. 2002;23:1921–1930. doi: 10.1016/s0142-9612(01)00318-0. [DOI] [PubMed] [Google Scholar]