Abstract
Objectives
To explore the association between adult day care (ADC) attendance and utilization of home-based formal services among people with Alzheimer’s Disease (AD).
Methods
Data for this secondary analysis came from a longitudinal parent study of 457 subjects from 16 ADC programs and an Alzheimer’s diagnostic center in metropolitan Chicago. We used the method of Generalized Estimating Equations to model the use of home-based formal services over time.
Results
Adjusting for relevant covariates, more days of ADC use at each follow-up was associated with decreased use of home-based formal services (coefficient = −.25, p < .0001). Older, unmarried caregivers who are children of the care recipients had lower use of home-based services.
Discussion
Results suggest that ADC services may substitute for specific types of home-based formal services. The projected increase in AD prevalence over the next several decades warrants a clearer understanding of how people with AD use formal services. (150 Words).
Keywords: Adult day services, Home and community-based services, Long-term care, dementia, longitudinal study
Introduction
Home and community-based services (HCBS) include a wide range of preventive and supportive services (District XI Area Agency on Aging, 2006; Wiener, Tilley, & Alecxih, 2002) and play an important role in the long-term care continuum. HCBS are designed to help older adults maintain a level of independence in their homes and communities and to assist informal caregivers in their caregiving tasks. Numerous studies have focused on examining the association between informal and formal care in the community setting (Davey et al., 2005; Davey & Patsios, 1999; McCamish-Svensson, Samuelsson, Hagberg, Svensson, & Dehlin, 1999; Noelker & Bass, 1989) and on identifying predictors of HCBS utilization among older adults (Alkema, Reyes, & Wilber, 2006; Biegel, Bass, Schulz, & Morycz, 1993; Bookwala et al., 2004; Borrayo, Salmon, Polivka, & Dunlop, 2002; Gill, Hinrichsen, & DiGiuseppe, 1998; Johnson & Wolinsky, 1996). However, among older adults who use formal HCBS, there is surprisingly little research exploring how consumers piece-together these various preventive and supportive services (Douglass & Fox, 1999), especially longitudinal research among persons with Alzheimer’s disease (AD).
The primary objective of this secondary analysis was to explore the association between community-based and home-based formal services among people with AD. In particular, we explored whether utilization of one type of community-based, formal service – adult day care (ADC) – was associated with utilization of similar home-based, formal services – specifically, homemaker, personal care, and visiting nurse services, or if ADC is used in place of these services. As the baby boom population ages, the number of people with Alzheimer’s disease (AD) is projected to almost triple from 4.5 million currently to 13.2 million by the year 2050 (Hebert et al., 2003). Since caregivers of people with AD are more likely to use supportive services than caregivers of people without AD, we can expect a concomitant increased demand for supportive services. Because long-term care is a process, understanding how individuals with AD move in and out of service utilization has critical federal and state policy implications.
Whether users of ADC with AD also use other types of services, particularly home-based services, is largely unknown. Clearly, there are circumstances where individuals with AD and their caregivers might use homemaker, personal care, and visiting nurse services to supplement ADC resources. For example, home-based services might be used on days when the individual does not attend ADC, during weekday evenings, and on weekends or holidays. By utilizing ADC, individuals with AD and their caregivers may become more familiar and comfortable with the types of services provided and hence may solicit similar service provision in their home environment, especially as increased frailty, impairment, or transportation becomes a barrier to attending ADC. On the other hand, individuals with AD and their caregivers may instead choose ADC programming over home-based service provision for various reasons including financial, socialization of the individual with AD, or respite for the caregiver. The question of whether individuals with AD use home-based formal services in place of community-based ADC services (substitution effect) or in addition to them (complement effect) has not been adequately explored.
There is very little research that has examined the utilization of and characteristics associated with combined community-based and home-based formal service use. Biegel et al. (1993) reported that users of both in-home (i.e., home-based) and out-of-home (i.e., community-based) services perceived adequate social support from their informal networks, had lower levels of caregiver emotional strain, and reported that their care recipients had less ADL impairment compared with users of in-home services only. Leon and colleagues (2000) found that the use of ADC, homemaker, and personal care services among individuals with AD was more frequent among individuals with more severe disease (i.e., advanced stages of dementia); however, their results were based on cross-sectional data and information about the simultaneous use of those three services was not provided. Aside from these reports, we know very little about the patterns of combined use of home- and community-based services among older adults with AD.
From a general service provider and policy perspective, it is important to understand patterns of HCBS utilization and the types of caregivers and care recipients who are most likely to use particular combinations of services (Alkema, Reyes, & Wilber, 2006). From an ADC provider’s perspective, this knowledge may help in the development and marketing of innovative programs designed to serve distinct populations along the aging and AD continuum. From a health policy perspective, this knowledge may guide decisions about eligibility for and appropriate use of publicly-funded services.
We used the behavioral model of health service utilization developed by Andersen (Andersen, 1968; Andersen & Newman, 1973; Andersen, 1995) to guide our conceptual framework. Commonly used to examine predictors of formal health service utilization, the behavioral model has three components: predisposing factors, enabling conditions, and need variables. We included the characteristics of both the AD care recipient and the primary caregiver in conceptualizing these three components. Predisposing factors include the care recipient and caregiver characteristics such as age, sex, race, marital status, relationship to the care recipient (i.e., spouse or child) and years providing care. Enabling conditions include variables such as education, income, as well as whether the care recipient lived alone or with others. Need variables include care recipient impairment and illness-related factors, such as limitation in activities of daily living or cognitive impairment that prompt the use of formal services. In addition, the number of hours the caregivers provided per week and whether other informal or unpaid caregivers provided assistance or care to the care recipient were also considered need characteristics. Need characteristics represent the most immediate cause of formal service utilization and are the strongest predictors of utilization of formal health services (Bookwala et al., 2004; Douglass, 1994).
Our primary research hypothesis in this secondary analysis was that ADC use is negatively associated with the utilization of home-based formal services, specifically, homemaker, personal care, and visiting nurse services, over time. Second, we hypothesized that the need characteristics of the behavioral model would drive utilization of home-based formal services.
Design and Methods
Subjects
Data for this secondary analysis came from a longitudinal, quasi-experimental parent study designed to examine the impact of adult day care services on nursing home placement in community-dwelling individuals with Alzheimer’s disease (AD). Care recipients with AD were asked to take part in a family and community eldercare services research project and were recruited from two sources in the metropolitan Chicago community. Care recipients using day care at baseline came from 16 adult day care (ADC) service sites in metropolitan Chicago and those not using day care at baseline came from the Rush Alzheimer’s Disease Center (RADC), a federally funded Alzheimer’s diagnostic center also serving metropolitan Chicago. In the parent study of the effect of day care on nursing home placement, the RADC care recipients were included as a comparison group that was not using day care at baseline. In this secondary analysis of data from the parent study, we included the RADC group to assess the level of formal, home-based service use among community-dwelling people with AD who were not using day care at baseline. Although our sample was chosen with respect to day care use at baseline, we recognized that some of those in the ADC group would stop using day care and some of those in the RADC group would start using day care. Because of this possibility of cross-over between day care users and non-users over time, we measured day care use by all care recipients at each 3-month follow-up point.
Information about the ADC sites has been provided elsewhere (McCann et al., 2005); but in summary, all programs were not-for-profit, were comparable in hours of operation and types of activities and services provided to clients, and included both social and health components (combined models). All programs provided assistance with personal care, oral medication administration, and blood pressure and weight monitoring, and about half of the programs provided more extensive health and rehabilitation services. About half the programs provided caregiver support groups, caregiver counseling, and case management, but none offered overnight or weekend respite services. Admission and discharge criteria were similar across programs.
Study enrollment began in March 1999 and continued for 3 years. Depending on date of enrollment, recipients were followed for a minimum of 24 to a maximum of 48 months with follow-up ending at time of death, nursing home placement, or study completion in August 2004. All care recipients were required to be age 65 or older, to meet standard diagnostic criteria for AD, and to reside in a community setting, excluding assisted living or nursing care facilities. The diagnosis of possible, probable, or highly probable AD was made by a board-certified neurologist (coauthor: NTA) using criteria of the joint working group of the National Institute of Neurologic and Communicative Disorders and Stroke and Alzheimer's Disease and Related Disorders Association (McKhann et al., 1984). Care recipients recruited from ADC sites were required to have used day care for a minimum of three months at baseline and to have attended the program at least two days a week during the previous month. To increase comparability between care recipients from ADC and RADC sites, the RADC care recipients were frequency-matched to ADC users by age group (65–74, 75–84, 85+), gender, race, and level of cognitive impairment (mild, moderate, severe) at baseline.
Of eligible care recipients, 516 (72.5%) agreed to participate in the study. We restricted this current analytic sample to care recipients who had non-missing service utilization data at baseline and for at least one other time point, resulting in a sample size of 457 (88.6% of enrolled care recipients), 193 (42.2%) from ADC sites and 264 (57.8%) from the Rush Alzheimer’s Disease Center. For these analyses, care recipients’ data were retained until a nursing home placement event and/or until a change in caregiver was observed (i.e., care recipients had the same caregiver(s) at all time points). Consent procedures were approved by the IRB at Rush University Medical Center and included verbal and written consent documents.
Measures
Older Adult (Care Recipient) Measures
At baseline, data were obtained on care recipients’ age, sex, marital status, race, education, income, and living arrangement. Age was analyzed as a continuous variable. Marital status was analyzed as married or not married. Race was dichotomized as black versus white and other races. Fewer than 2% (n=7) of our care recipients were from a racial or ethnic group other than black or white. We ran our analyses excluding the 7 participants belonging to other racial or ethnic groups and the results were unchanged; therefore, we included them in the white group in all reported analyses. Education was assessed in terms of years of completed schooling and analyzed as a continuous variable. The care recipient’s total annual family income was reported as a continuous variable using ten income categories and the "show-card" method employed in the Established Populations for Epidemiologic Studies of the Elderly projects (Cornoni-Huntley, Brock, Ostfeld, Taylor, & Wallace, 1986). For some analysis, we used two indicator variables instead: 1) income equal to $25,000 or more versus less than $25,000; and 2) an indicator variable for those whose income was missing. Because program payment source information was available only for ADC users (51% were self-pay), we did not include payment source in our analyses, and instead used income. Living arrangement was characterized as living alone or living with others and was reassessed at each follow-up.
At baseline and every 6 months, cognitive impairment was assessed by the Mini-Mental State Examination (MMSE) (Folstein, Folstein, & McHugh, 1975), a 20-item measure of orientation, memory, attention, language and visual-spatial abilities. The possible range of scores is 0–30 with lower scores indicating greater cognitive impairment. At each 3-month interview with the caregiver, we collected data on the care recipient’s physical function using items from the Katz Activities of Daily Living Scale to measure the ability to independently perform six basic self-care activities: bathing; dressing; walking across a small room; transferring from bed to a chair; using the toilet; and eating (Cornoni-Huntley, Brock, Ostfeld, Taylor, & Wallace, 1986; the “grooming” item was not included in our analyses). Each item was rated as 0 (“no help required”) or 1 (“needs help/unable to perform”) with the previous month used as the time frame of reference. Items were summed to produce a score ranging from 0 to 6 based on the number of activities performed requiring assistance, with higher scores indicating greater functional impairment. Both the MMSE and the Katz ADL scale were included as time-varying measures in the multivariate modeling.
Caregiver Measures
At baseline, we collected data on caregiver age, sex, marital status, race, education, relationship to the care recipient, years providing care, self-reported hours of care provided weekly, and whether other informal or unpaid caregivers provided assistance or care to the care recipient. Age, education, years providing care, and hours of care provided weekly were analyzed as continuous variables. ‘Hours of care provided weekly’ was assessed every three months to tell us, on average, how many hours of care were provided in a typical week; it was included as a time-varying measure in the multivariate modeling. The coding of marital status and race was identical to the care recipient data. Relationship to the care recipient was coded as spouse, child, or other. For analysis, we used the grouping variables of spouse (reference category), married child, unmarried child, and other.
Predictor variable: Adult day care (ADC) use
ADC use was assessed every three months for both ADC and RADC groups and included as a time-varying measure in the multivariate model. Caregivers were asked how many days per week (0–7), on average, their care recipients attended day care during the previous month. Because our sample consisted of two somewhat distinct groups, we also measured ADC use as a dichotomous variable indicating whether the care recipient was recruited from one of the ADCs at baseline or not (i.e., care recipients attending ADC at baseline [1] vs. not attending ADC at baseline [0]).
Outcome measure: Home-based formal services
At baseline and each 3-month follow-up, for up to 48 months, we collected utilization data on a variety of home and community-based services. For this analysis, we focused on three home-based services that are commonly used and that closely approximate the services provided in a typical ADC: homemaker services, personal care services, and visiting nurse services. At each interview, the caregiver was asked whether the care recipient had used any of the services since the last interview. Because of the relatively low utilization of homemaker, personal care, and visiting nurse services (16%, 18%, and 5%, respectively, at baseline), we combined the three home-based services into a dichotomous variable indicating whether the care recipient used any of the services or none of the services (1=yes, 0=no). The three home-based services selected are homogeneous enough to be meaningfully aggregated without raising significant concerns about variation in different factors predicting each (Biegel et al., 1993).
Analysis
We modeled the use of home-based formal services over time using a generalized linear model, fit using the method of Generalized Estimating Equations (GEE),1 which, at a given time point, is equivalent to a logistic regression model. Because the data are repeated measures, we must take into account the correlation between observations from the same person. In GEE models, this is done by first specifying a "working correlation" matrix that defines the correlations between observations at any pair of time points for a given person2. We fit our GEE models using the GENMOD® procedure of SAS® Version 8 (SAS Institute Inc., 2000).
Our model building strategy proceeded in three steps. First, we established separate models based on the behavioral model of health service use for both caregivers and care recipients. This was important to understand the unique factors affecting health service use in caregivers and care recipients. In each of the two models, we included study time, predisposing factors (i.e., sociodemographic variables and caregiver-reported years providing care), enabling factors (i.e., education, income, and living arrangements), and need factors (i.e., care recipient cognitive impairment, physical function, number of hours of care provided per week, and whether other informal or unpaid caregivers provided assistance or care). In each of these two models, we also included all significant two-way interaction terms, including significant interaction terms with study time.
Second, we combined the caregiver and care recipient models, retaining key conceptual variables from the behavioral model of health service utilization such as caregiver age and care recipient: age, sex, and race. We dropped other variables that were not significant or that were highly correlated with variables already in the model, such as caregiver race (i.e., the race of all caregiver and care recipient dyads was identical). For caregivers, the variables included in the combined model were: study time, age, sex, years providing care, marital status and relationship to care recipient, hours of care provided weekly, other informal or unpaid caregivers, and the interaction of these grouping variables with age. For the care recipients, the variables included in the model were: study time, age, sex, race, living alone, an interaction term for age with sex, income, MMSE and the Katz ADL scale. Because financial resources might affect use of services, in this step, we also added care recipient income to the combined model.
In the third step, we added the time-varying measure of ADC use to the model. Although our care recipients were recruited from two different sources (ADC programs and the RADC Alzheimer’s disease clinic), we measured ADC use for all participants at each 3-month follow up. Over the course of the study, 16% of the RADC care recipients used ADC services and 4% of participants recruited from ADC programs did not use ADC services at one or more follow-up points. Because participants in both groups used adult day services, it made sense to combine the groups and use ADC as a time-varying covariate in our analysis.
In a series of sensitivity analyses, we examined whether different ways of characterizing our outcome variable or some of our predictors altered the results from our final model. First, we substituted a continuous-level outcome variable for our dichotomous "any use" outcome variable. The continuous-level outcome variable (0–15) reflects the average intensity of service use. It is the sum of the number of services used (0–3) times the frequency of using each of the three services over the past three months (1–5), where 1 = less often than once a month, 2 = 1 to 3 times a month, 3 = once a week, 4 = 2 to 4 times a week, and 5 = 5 or more times a week. Because the total frequency of service use ranged from 0 to 15 and most of the data were low values, we modeled this variable as a count variable using the Poisson distribution and a log link in the GEE model. Second, we also tested whether a different characterization of living arrangement (lived alone for all observations, currently living alone but was living with others before, or currently living with someone but was living alone before) resulted in differences in our model results, because, ostensibly, a change in living environment could co-occur with a change in help provided by family caregivers or in help received from formal care services. Third, because we had missing income data, we replaced the income variable with both caregiver and care recipient education indicators to see if this altered the results of our final model. We also substituted a dichotomous income measure (income less than $25,000 vs. $25,000 or more, or income missing) to see if there were any model differences.
Finally, because 42.2% of the care recipients were recruited from ADC sites and hence considered ADC users at baseline, and 57.8% were recruited from the Rush Alzheimer’s Disease Center and considered ADC non-users at baseline, we conducted a sensitivity analysis to address the possibility that unmeasured differences in care recipients recruited from these two sources might have affected the study results. We used propensity analysis to re-examine our final models. The propensity score for an individual is defined as the conditional probability of being in a specific group given the individual’s covariates (D’Agostino, 1998). In observational studies where random assignment is not possible, the propensity score can be used to balance the covariates in the two groups and thus reduce potential bias due to unmeasured differences. Specifically, we first used multiple logistic regression to model the predicted probability (propensity) of using day care at baseline. Then, using the method of Rosenbaum and Rubin (1983) following the example given in D’Agostino, Jr. (1998), we re-fit our core models adjusting for the propensity to be a day care user at baseline. We considered three different approaches in separate models: including the predicted propensity in the model, including the quintile of the propensity as a categorical variable, and including the median propensity within the quintile. All three approaches left our conclusions unchanged, and thus we do not report on them further.
Results
We followed study care recipients for up to 48 months with an average of 85% of survivors participating at each follow-up (range = 77% to 100%). The average time on study was 2.1 years (standard deviation [sd] = 1.2) which provided an average of 6.1 data points in our multivariate models. At the time of the baseline evaluation, 193 care recipients (42.2%) were using ADC services from 2 to 6 days a week for an overall mean of 1.6 days per week (sd = 2.1) in the group as a whole. Over the entire 48-month observation period, the average use of ADC was 1.4 days per week (sd = 2.0).
Table 1 is a summary of the sample characteristics at baseline by ADC use. ADC recipients were slightly older, had fewer years of education, were less likely to be married, were less likely to be living alone, had worse cognitive and physical function, and lower income than their RADC counterparts. At baseline, ADC recipients indicated having used fewer homemaker and visiting nurse services than their RADC counterparts. Overall, ADC recipients used fewer total services than their counterparts. At baseline, caregivers of ADC recipients were younger, less likely to be male, more likely to be black, less likely to be married, more likely to be a child of the recipient, reported having provided more years of care, and more likely to report that other informal or unpaid caregivers had also been providing assistance to the recipient, compared with their RADC caregiver counterparts.
Table 1.
Characteristics of the sample at baseline, by ADC use, Mean (standard deviation) and percentages
| Variable | Total (N=457) |
ADC (n = 193) |
RADC (n = 264) |
p value a |
|---|---|---|---|---|
| Care Recipient Characteristics | ||||
| Age | 80.0 (6.5) | 81.4 (6.3) | 79.1 (6.5) | 0.0002 |
| Male gender | 31.5% | 29.5% | 33.0% | 0.4368 |
| Black race | 27.6% | 32.1% | 24.2% | 0.0625 |
| Education | 11.7 (3.7) | 10.9 (4.0) | 12.2 (3.3) | 0.0002 |
| Married | 40.6% | 23.4% | 53.0% | <0.0001 |
| Living alone | 10.7% | 6.2% | 14.0% | 0.0078 |
| MMSE score (range: 0–30) | 13.7 (8.0) | 12.6 (7.5) | 14.5 (8.3) | 0.0130 |
| Katz disability score (range: 0–6) | 1.9 (2.0) | 2.1 (1.7) | 1.7 (2.1) | 0.0273 |
| Income category (range: 1–10) b | 4.5 (2.7) | 3.7 (2.2) | 5.1 (2.8) | <0.0001 |
| Caregiver Characteristics | ||||
| Age | 60.1 (13.3) | 57.9 (12.3) | 61.6 (13.7) | 0.0032 |
| Male gender | 24.1% | 12.4% | 32.6% | <0.0001 |
| Black race | 27.7% | 32.8% | 24.0% | 0.0370 |
| Education | 14.3 (2.9) | 14.1 (2.7) | 14.4 (2.9) | 0.3008 |
| Married | 71.3% | 65.6% | 75.4% | 0.0230 |
| Relation to care recipient | <0.0001 | |||
| Spouse | 32.8% | 20.2% | 42.1% | |
| Child | 56.5% | 66.8% | 48.9% | |
| Other | 10.7% | 13.0% | 9.1% | |
| Years providing care | 3.8 (3.5) | 4.4 (3.8) | 3.4 (3.3) | 0.0018 |
| Hours providing care per week | 49.2 (55.0) | 51.5 (51.5) | 47.6 (57.4) | 0.4643 |
| Other informal or unpaid caregivers | 56.7% | 64.9% | 50.8% | 0.0026 |
| Home-based Formal Services | ||||
| Homemaker services | 15.6% | 10.0% | 19.7% | 0.0050 |
| Personal care attendant | 17.5% | 14.0% | 20.1% | 0.0908 |
| Visiting nurse | 5.0% | 1.6% | 7.6% | 0.0036 |
| Any use of all three services (composite) | 27.8% | 19.7% | 33.7% | 0.0009 |
| Community-based Formal Service | ||||
| Total adult day care use (range: 0–7) | 3.9 (1.2) | 0 (0) | <0.0001 |
for difference between groups
income data missing for 9.84% of ADC group and 13.64% of RADC group.
Table 2 shows the results of the multivariate modeling of the “any use of home-based services” (i.e., homemaker services, personal care services, or visiting nurse services) outcome variable over time. In the interest of space, the table shows only the final two models – the model that resulted from combining the best caregiver and best care recipient models (combined model) and then the combined model when ADC was added (final model).
Table 2.
Modeling ‘any use of services’ (homemaker services, personal care services, or visiting nurse services) using the Generalized Estimating Equations method with a logit link function and a binomial error term, estimate (standard error)
| Combined | Final | |
|---|---|---|
| Variable | Model | Model |
| Intercept | −3.24 (0.60)*** | −2.66 (0.61)*** |
| Study time | 0.20 (0.04)*** | 0.20 (0.04)*** |
| Predisposing Factors | ||
| Caregiver (CG) age | 0.05 (0.03) | 0.04 (0.03) |
| CG sex (male) | 0.45 (0.23) | 0.36 (0.23) |
| CG years providing care | 0.02 (0.02) | 0.02 (0.02) |
| CG relationship to recipient, (spouse = reference group) | ||
| CG – married child | 0.38 (0.62) | 0.39 (0.63) |
| CG – single child | 0.65 (0.62) | 0.46 (0.63) |
| CG – other relative | 1.27 (0.57)* | 1.30 (0.59)* |
| CG age × married child | −0.07 (0.03) | −0.06 (0.04) |
| CG age × single child | −0.07 (0.04)* | −0.09 (0.04)* |
| CG age × other relative | −0.07 (0.04) | −0.07 (0.04) |
| Care Recipient (CR) age | 0.01 (0.02) | 0.02 (0.02) |
| CR sex (male) | 0.03 (0.25) | 0.09 (0.25) |
| CR race (black) | 0.35 (0.22) | 0.32 (0.22) |
| CR age × sex | 0.09 (0.03)** | 0.10 (0.03)** |
| Enabling Factors | ||
| CR income | 0.13 (0.04)*** | 0.09 (0.04)* |
| CR living alone at baseline | 1.25 (0.30)*** | 1.02 (0.31)*** |
| Need Factors | ||
| CR MMSEa | −0.01 (0.01) | −0.02 (0.01) |
| CR Katza | 0.28 (0.04)*** | 0.28 (0.04)*** |
| Hours providing care per weeka | −0.00 (0.00) | −0.00 (0.00) |
| Other informal or unpaid caregivers | 0.34 (0.19) | 0.39 (0.19)* |
| Total adult day care use (time-varying)b | - | −0.25 (0.04)*** |
p ≤ .05
p ≤ .01
p ≤ .001
Hours providing care per week, MMSE, & Katz were analyzed as time-varying measures.
Adult day care use = time-varying measure of total amount of day care use (range: 0–7).
The best caregiver model (data not shown) showed that use of home-based services increased over time. Among the predisposing factors, use of home-based services was slightly higher among older spouse caregivers and according to the number of years having provided care. Home-based service use differed by the caregiver’s relationship to the care recipient. Compared to spouses, all other caregiving relationship pairs (e.g., married child, single child, other relative) had higher use of home-based services at baseline. While service use increased among all caregivers, a significant interaction of “other” relative caregiver with study time indicated that other relatives providing care had a lower rate of increase in use of services over time compared to spouse caregivers. Significant interactions of caregiver age with each of the three types of caregiver relationship (i.e., married child, single child, and other relative) indicated use of services with age varied among the four groups. Caregiver education, an enabling factor was not associated with home-based service use. Among the need factors, other informal or unpaid caregivers providing care was associated with higher home-based service use. In the caregiver model, the predisposing factor (i.e., caregiver relationship to recipient) of the behavioral model was most strongly associated with home-based service use.
The best care recipient model (data not shown) showed that there were no trends over time in service use. Among the predisposing factors, non-significant main effects of care recipient age and sex coupled with the significant interaction of age with sex indicated that older male care recipients had higher use of any services compared to younger men and women of any age. Among the enabling factors, the use of home-based services was associated with the care recipient living alone at baseline. For the need factors, both lower cognitive impairment (MMSE) and greater functional impairment (Katz ADL scale) were associated with higher service use. In the care recipient model, the enabling factor (i.e., living alone) of the behavioral model was most strongly associated with home-based service use.
The best combined caregiver and care recipient model (Table 2) shows that home-based service use increased over time, and there was no significant effect modification of this trend. Among the predisposing factors, the main effect of "other relative” being the caregiver was significant, and there were significant or marginally significant interactions between each relationship contrast and the age of the caregiver. Examining the coefficients, we saw that the trend among non-spouse caregivers was to use fewer services if they were older, but among spouse caregivers, the older the spouse, the more services were used. The interaction of care recipient age with sex was still highly significant. Among the enabling factors, care recipients’ higher income was associated with higher home-based service use, as was service use for recipients living alone at baseline. For the need factors, only functional impairment (Katz ADL scale) was significantly associated with higher service use in the combined model; that is, after controlling for the caregiver variables, lower cognitive functioning (MMSE) was no longer associated with service use. In the combined model, the predisposing (i.e., caregiver relationship to recipient) and the enabling factors (i.e., living alone) were most strongly associated with home-based service use.
In the final model (Table 2), adding the time-varying ADC use variable to the combined model did not substantively alter any of the estimates or associations from the combined model, except that the need factor of “other informal or unpaid caregivers” was significantly associated with higher home-based service use compared with the marginally significant association in the combined model. In this final model, the predisposing factor (i.e., caregiver relationship to recipient) of the behavioral model remained the most strongly associated with home-based service use and the association of the enabling factor ‘living alone’ decreased slightly. The time-varying ADC use variable was inversely associated with service use; that is, more days of ADC use each week was associated with lower use of any home-based services.
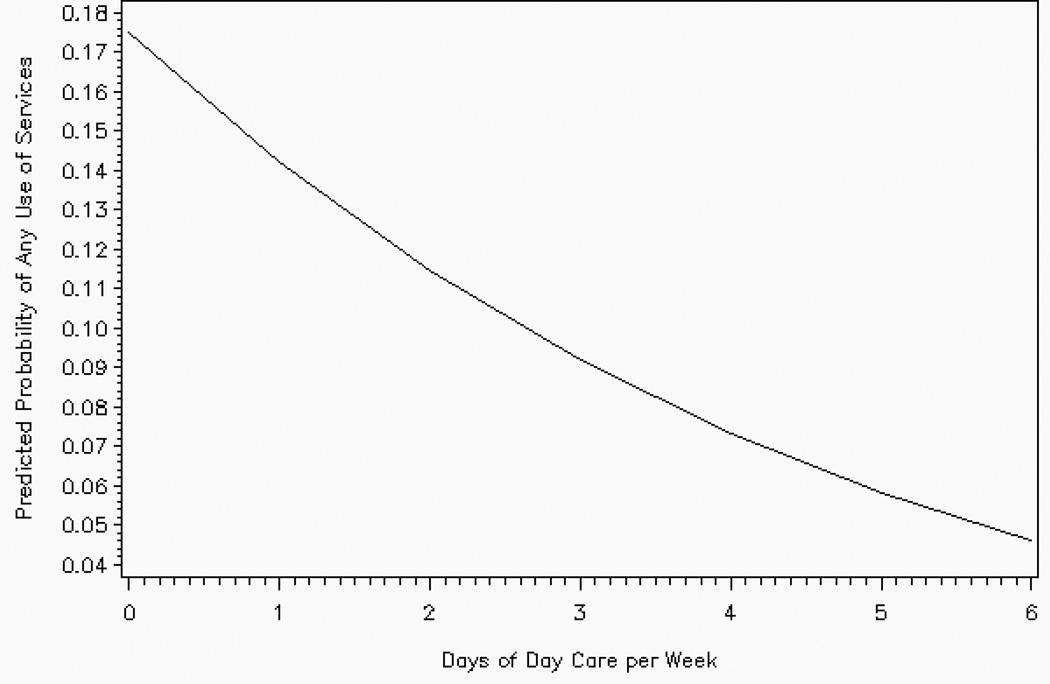
We used the results of the final model to illustrate the probability of home-based service use as a function of the days of day care used per week (Figure 1). We plotted the predicted probabilities from the final model for a typical person (i.e., female spouse caregiver of average age, caring for a non-black care recipient of average age who is not living alone, with average values for the other covariates) at baseline. Although the maximum possible number of days of day care is seven, only one observation attained this value and thus we plotted our probabilities for 0–6 days of day care per week; note that this one observation was not influential in the model estimates. The figure shows that the more days of day care used per week, the lower the use of other home-based services.
Figure 1.
Predicted probability of using home-based formal services by day care use, (based on final model in Table 2)
Sensitivity Analysis
When we substituted the continuous-level outcome variable of home-based service use for the dichotomous variable, we found no substantive differences in the model; that is, ADC use was inversely associated with frequency of service use (coefficient = −0.18, p < 0.001 compared with −0.25, p < 0.001 for the dichotomous outcome). However, we found one notable difference in the model regarding race. In the model with the continuous-level outcome variable, blacks had significantly higher frequency of service use, although this was not observed when the outcome variable was analyzed as a dichotomy. We found no significant associations of changes in living arrangement with service use. We also found no substantive model differences when we substituted the caregiver and care recipient education indicators for income (i.e., neither education indicator was statistically associated with the outcome), nor when we substituted the dichotomous income indicator (income less than $25,000 vs. $25,000 or more, or income missing) for the continuous level income variable. Thus, the small percentage of missing income data did not affect our study results.
Discussion
In this secondary analysis of data from a study of the effect of adult day care (ADC) on nursing home placement, we examined patterns of HCBS use over time among people with AD. Our sample included care recipients with AD who were using little or no ADC services and others who were using high levels of ADC services. We hypothesized that ADC use was negatively associated with the utilization of home-based formal services, specifically, homemaker, personal care, and visiting nurse services, over time. Our results indicate that among care recipients with AD, adjusting for other relevant factors, ADC use is indeed associated with lower use of home-based, formal services over time. Second, we hypothesized that the need characteristics of the behavioral model would drive utilization of home-based formal services among the ADC clients with AD. Surprisingly, we found that the predisposing and enabling characteristics of the behavioral model appeared to drive the utilization of home-based formal services more so than the need characteristics. The following predisposing and enabling factors were associated with increased use of home-based formal services controlling for ADC use: older male care recipients, a primary caregiver who was someone other than the child or the spouse of the care recipient with AD, recipient higher income, and recipient living alone. Older, unmarried child caregivers had lower use of home-based formal services. Need factors associated with increased use of home-based formal services included other informal or unpaid caregivers also providing care and care recipient functional, but not cognitive, impairment.
There are at least three ways to interpret the inverse association between day care use and home-based formal services. First, the negative association may reflect a difference in the types of services needed based on the individual’s disease characteristics. However, two factors counter this reasoning: 1) the home-based services we included in our analysis overlapped with services offered in most ADC programs, and 2) this negative association remained, even after we controlled for indicators of disease severity. Controlling for cognitive function, physical function, and weekly hours of care, ADC services were associated with a decreased use of homemaker, personal care, and visiting nurse services, suggesting that ADC and home-based services meet similar care recipient needs. ADC programs may be especially adept at tailoring their programs to both clients’ and caregivers’ changing needs over time, hence minimizing the need for supplemental, home-based care.
Second, the negative association between ADC and home-based formal services may reflect a difference in caregiver preferences for service delivery venue, that is, in-home vs. out-of-home services. Preferences for service location may originate from care recipient mobility factors, transportation issues, scheduling convenience, or simply from comfort or familiarity with services that have been employed over a period of time. Although we did not have measures of preference for service venue, it is possible that the greater use of home-based services by particular types of caregivers is a reflection of these underlying preferences.
Third, the negative association between ADC and home-based formal services might reflect differences in availability, accessibility, or affordability of ADC versus home-based services. For example, research documents that home-based services are not available, accessible, or affordable for large segments of the population (Wiener, Tilly, & Alecxih, 2002). The same may be true for ADC services. For example, the nationwide ADC capacity is approximately 150,000 older adults daily (NADSA, 2008); therefore, based on the current population of 4.5 million older adults with AD, the existing ADCs could only accommodate 3.3% of the people with AD. This assumes that 100% of all ADC recipients have a diagnosis of AD, whereas AD and other dementias currently represent approximately half of the diagnoses in ADCs (Alzheimer’s Association and the National Alliance for Caregiving, 2004). Nonetheless, we did not have measures of availability, accessibility, or affordability to know whether care recipients and caregivers had a choice in services. We did find that higher income was associated with greater use of home-based services, but ADC use attenuated this effect. We also know that the study recipients all lived within a 50-mile radius of Rush University Medical Center and that this urban geographic area has many ADC and home care programs, so we believe that availability was not a key factor in service use. It is possible that accessibility to ADC may have played a role in service use because some ADC programs did not provide transportation or care recipients may have lived outside the catchment area.
Regardless of the reasons for differences in use of ADC versus home-based services, our results suggest that ADC services may be providing a substitute for specific types of home-based formal services and that among people with AD, even controlling for cognitive and physical impairment, ADC users are less likely to use home-based services. Some might argue that the very nature of ADC programs limits opportunities to use home-based formal services, thus creating an artifactual relation between the two. However, personal care, homemaker, and visiting nurse services are generally available at evening and weekend times so it is possible to use both services concurrently. The central point of these data is that if people are using enough ADC services, they tend not to use in-home services. From a programmatic and policy perspective, this is an important empirical finding.
In this secondary analysis, we considered elements of both care recipient and caregiver needs. We adjusted for care recipient cognitive impairment, physical function, living arrangements, and income, as well as caregiver marital and employment status, and receiving caregiving assistance, and we found that adult day care use apparently satisfies needs, at least to the extent that other services are not being used. Thus, although we did not conduct a formal needs assessment or examine care recipient or caregiver perceptions of services, we believe that home- and community-based service use is largely a function of a consumer’s preference for service delivery venue. Further exploration is needed into how care recipient disease characteristics and needs interplay with caregiver needs and how both parlay into formal service utilization. Of course, we examined only a limited number of home-based services in this analysis. As states struggle with myriad fiscal and administrative constraints associated with home- and community-based service programs, examining patterns of service use and non-use will become even more critical.
Contrary to the vast majority of research demonstrating need characteristics to be the strongest of the behavioral model factors to predict utilization of formal health services, our results indicated that the predisposing and enabling characteristics had the strongest associations with use of home-based services. One explanation for our contrary finding is how we operationalized the behavioral model factors. For example, predisposing factors traditionally include the sociodemographic characteristics of the care recipient and the recipient-caregiver dyad (Noelker & Bass, 1989), complemented recently by psychosocial factors (Andersen, 1995). Thus, we considered the caregiving relationship dyad (i.e., spouse, child, or other relative to the care recipient) to be a predisposing characteristic. Enabling characteristics are defined as resources that promote or inhibit service use (Noelker & Bass, 1989). As such, we characterized the care recipient’s living alone at baseline as an enabling characteristic. Need factors traditionally refer to the care recipient’s illness and impairment characteristics and caregiving-related stress and burden (Noelker & Bass, 1989). Thus, we felt that the care recipient’s cognitive impairment and physical function clearly characterized recipient need and the number of caregiving hours provided per week and whether other informal or unpaid caregivers provided care characterized caregiver need.
The primary strengths of this longitudinal dataset are the number and spacing of follow-up assessments, the degree of specificity, and the high follow-up participation rates. The care recipients were assessed at six-month intervals and the caregivers were assessed at three-month intervals over approximately four years for a total of 15 data collection points (an average of 6.1 data points in our final multivariate model). The narrow spacing of the assessments allows for more precision in estimating changes in services utilization. We also created dynamic models by using time-varying measures, which evaluated changes in important predictors every 3 months, and we had high baseline (73%) and follow-up participation rates (85%). Furthermore, by design, our eligibility criteria gave us a group of both highly-committed day care users and a group of non-day care users who were comparable in terms of need.
There are limitations to our analyses. Foremost is that our analyses focused on ADC and three specific formal home-based services; therefore, our findings may not generalize to other types of home and community-based formal services. We share another limitation with many other ADC studies, which is the inherent heterogeneity of ADCs regarding structure, operations, activities, and client mix. That is, by aggregating all ADCs and then examining an association between their utilization and an outcome, we have likely minimized the unique explanatory ability of certain ADCs to be associated with certain HCBS (Baumgarten et al., 2002). Further, we did not measure caregiver attitudes or perceptions of HCBS which would have likely yielded important information about service use (Collins, Stommel, King, & Given, 1991), as would have HCBS payment source information. Finally, this secondary analysis was limited to people with AD; thus, our findings may not generalize to ADC clients with other health conditions
In summary, we found that greater ADC use was predictive of lower home-based, formal services utilization over time; that is, more day care resulted in less in-home services. It has been projected that because of the changing demographic features of the aging population, a greater emphasis will be placed on formal home and community-based services in the future resulting in increased expenditures and utilization (Bass, Noelker, & McCarthy, 1999; Wiener, Tilly, & Alecxih, 2002). The projected increase in AD prevalence over the next several decades (Hebert et al., 2003) warrants a clearer understanding of how this special population of consumers and their caregivers need, use, and pay for formal home and community-based services. Further investigation is needed examining how services substitute for one another, the relative differences in cost-effectiveness of services, and the care recipient and caregiver outcomes associated with each. This information will provide needed evidence to policymakers and legislators charged with identifying mechanisms to fund adequate services for this population. Minimally, understanding the patterns of home- and community-based services utilization and the types of caregivers and care recipients who are most likely to use particular combinations of services will enhance the value of existing programs. This knowledge may also provide the impetus for creating new programs, customizing treatment plans, or encouraging collaborative relationships between agencies that serve individuals with AD and their caregivers
Acknowledgments
This research was supported by grants from the National Institutes of Health, National Institute on Aging, [NIH/NIA: R01-AG10315 and R01-AG09966]. The authors thank the adult day care staff, the care recipients, and their caregivers for their time and dedication to this project. We also thank Ms. Melinda Scheuer and her staff of research assistants for data collection activities, Mr. George Dombrowski and his staff for data management, and Ms. Woojeong Bang, Mr. Todd Beck, Ms. Linyun Zhou, and Ms. Liping Gu, for analytic programming and analyses. We also thank Dr. Tricia J. Johnson, Director, Center for Health Management & Policy Research and Economist in the Department of Health Systems Management at Rush University Medical Center, for her helpful review of the manuscript. We would also like to acknowledge the contribution of Dr. David W. Gilley to the original conceptualization of the parent study.
Footnotes
We used a logit link function and a binomial error term to model the outcome of "any use" versus "no use" at each time point.
Like other repeated-measures approaches, this is assumed to be the same correlation matrix for all persons. However, unlike other repeated-measures approaches, the estimates obtained from the model are robust to misspecification of the structure of this matrix. That is, unlike, for example, the compound symmetry assumption required in standard fixed-effects repeated measures analysis, the parameter estimates and standard errors from GEE are consistent estimators of their true values regardless of how the "working correlation" matrix is specified, when the "empirical" or "sandwich" variance estimator is used, as we do here (Diggle et al., 2002; Zeger & Liang, 1986). As is commonly done, we chose the “working” within-person correlation matrix to have identical correlations for each pair of times of observation ("exchangeable" structure).
References
- Alkema GE, Reyes JY, Wilber KH. Characteristics associated with home- and community-based service utilization for Medicare managed care consumers. The Gerontologist. 2006;46:173–182. doi: 10.1093/geront/46.2.173. [DOI] [PubMed] [Google Scholar]
- Alzheimer's Association and the National Alliance for Caregiving. Families care: Alzheimer's caregiving in the United States. Report. 2004. p. 2004. [Google Scholar]
- Andersen RM. A Behavioral Model of Families’ Use of Health Services. Chicago: Center for Health Administration Studies; 1968. [Google Scholar]
- Andersen R. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the U.S. Milbank Memorial Fund Quarterly. 1973;51:95–124. [PubMed] [Google Scholar]
- Bass DM, Noelker LS, McCarthy CA. The influence of formal and informal helpers on primary caregivers’ perceptions of quality of care. Journal of Applied Gerontology. 1999;18:177–200. [Google Scholar]
- Baumgarten M, Lebel P, Laprise H, Leclerc C, Quinn C. Adult day care for the frail elderly: Outcomes, satisfaction, and cost. Journal of Aging and Health. 2002;14:237–259. doi: 10.1177/089826430201400204. [DOI] [PubMed] [Google Scholar]
- Biegel DE, Bass DM, Schulz R, Morycz R. Predictors of in-home and out-of-home service use by family caregivers of Alzheimer’s disease patients. Journal of Aging and Health. 1993;5:419–438. doi: 10.1177/089826439300500401. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Zdaniuk B, Burton L, Lind B, Jackson S, Schulz R. Concurrent and long-term predictors of older adults’ use of community-based long-term care services: The caregiver health effects study. Journal of Aging and Health. 2004;16:88–115. doi: 10.1177/0898264303260448. [DOI] [PubMed] [Google Scholar]
- Borrayo EA, Salmon JR, Polivka L, Dunlop BD. Utilization across the continuum of long-term care services. The Gerontologist. 2002;42:603–612. doi: 10.1093/geront/42.5.603. [DOI] [PubMed] [Google Scholar]
- Collins C, Stommel M, King S, Given CW. Assessment of the attitudes of family caregivers toward community services. The Gerontologist. 1991;31:756–761. doi: 10.1093/geront/31.6.756. [DOI] [PubMed] [Google Scholar]
- Cornoni-Huntley J, Brock DB, Ostfeld AM, Taylor JO, Wallace RB. Established Populations for Epidemiologic Studies of the Elderly: Resource Data Book. Washington, DC: U.S. Department of Health and Human Services; 1986. (Rep. No. NIH Pub No. 86-2443). [Google Scholar]
- D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Davey A, Femia EE, Zarit SH, Shea DG, Sundstrom G, Berg S, Smyer MA, Savla J. Life on the edge: Patterns of formal and informal help to older adults in the United States and Sweden. Journal of Gerontology: Social Sciences. 2005;60:281–288. doi: 10.1093/geronb/60.5.s281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey A, Patsios D. Formal and informal community care to older adults: Comparative analysis of the United States and Great Britain. Journal of Family and Economic Issues. 1999;20:271–300. [Google Scholar]
- Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of longitudinal data. 2nd ed. NY: Oxford University Press; 2002. [Google Scholar]
- District XI Area Agency on Aging. Home & Community Based Services. 2006 Retrieved September 12, 2006 from http://www.distxiaaoa.com/home.htm. [Google Scholar]
- Douglas C, Fox PJ. Health care utilization among clients with Alzheimer’s disease: Public policy implications from the California Alzheimer's Disease Diagnostic and Treatment Center Program. The Journal of Applied Gerontology. 1999;18:99–121. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gill CE, Hinrichsen GA, DiGiuseppe R. Factors associated with formal service use by family members of patients with dementia. The Journal of Applied Gerontology. 1998;17:38–52. [Google Scholar]
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the U.S. population: Prevalence estimates using the 2000 census. Archives of Neurology. 2003;60:1119–1122. doi: 10.1001/archneur.60.8.1119. [DOI] [PubMed] [Google Scholar]
- Johnson RJ, Wolinsky FD. Use of community-based long-term care services by older adults. Journal of Aging & Health. 1996;8:512–537. doi: 10.1177/089826439600800403. [DOI] [PubMed] [Google Scholar]
- Leon J, Neumann PJ, Hermann RC, Hsu MA, Cummings JL, Doraiswamy PM, Marin D. Health-related quality-of-life and service utilization in Alzheimer’s disease: A cross-sectional study. American Journal of Alzheimer’s Disease. 2000;15:94–108. [Google Scholar]
- McCamish-Svensson C, Samuelsson G, Hagberg B, Svensson T, Dehlin O. Informal and formal support from a multi-disciplinary perspective: A Swedish follow-up between 80 and 82 years of age. Health and Social Care in the Community. 1999;7:163–176. doi: 10.1046/j.1365-2524.1999.00173.x. [DOI] [PubMed] [Google Scholar]
- McCann JJ, Hebert LE, Li Y, Wolinsky FD, Gilley DW, Aggarwal NT, Miller JM, Evans DA. The effect of adult day care services on time to nursing home placement in older adults with Alzheimer’s disease. The Gerontologist. 2005;45:754–763. doi: 10.1093/geront/45.6.754. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- National Adult Day Services Association (NADSA) Adult day services: overview and facts. 2008 Retrieved June 12, 2008 from http://www.nadsa.org/adsfacts/default.asp.
- Noelker LS, Bass DM. Home care for elderly persons: Linkages between formal and informal caregivers. Journal of Gerontology. 1989;44:63–70. doi: 10.1093/geronj/44.2.s63. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DA. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- SAS Institute Inc. SAS/STAT® User's Guide, Version 8. Cary, NC: SAS Institute Inc; 2000. [Google Scholar]
- Short P, Leon J National Medical Expenditure Survey Research Findings 5, Agency for Health Care Policy and Research. Use of home and community services by persons ages 65 and older with functional difficulties. Rockville, MD: Public Health Service; 1990. (DHHS Publication No. (PHS) 90-34666). [Google Scholar]
- Wiener JM, Tilly J, Alecxih LM. Home and community-based services in seven states. Health Care Financing Review. 2002;23:89–114. [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]