Abstract
Objectives
Few prospective studies have examined personality and depression in older adults. We investigated whether the Five Factor Model (FFM) of personality traits --- Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness --- and trait combinations (styles) are related to incident major or minor depression.
Participants/Setting
Prospective data were gathered on a community sample of 512 older adults with disability and a history of significant health care utilization who were enrolled in a Medicare Demonstration Project.
Measurements
Depression and personality traits and styles were assessed at baseline; depression was assessed again at approximately 12 and 22 months.
Design
Participants who developed incident major depression were compared to those free of depression at all three assessments. Similar analyses were done for minor depression.
Results
High Neuroticism and low Conscientiousness were risk factors for both major and minor depression. Combinations of high Neuroticism with low or high Extraversion or high Openness conferred risk for major depression. Other novel findings for major depression revealed new trait combinations of low Conscientiousness with low or high Extraversion, high Openness, or low Agreeableness. Three trait combinations, all involving low Conscientiousness, predicted risk for minor depression: high Neuroticism, high Agreeableness, and low Openness.
Conclusion
The present findings highlight the importance of examining combinations of personality traits or personality styles when identifying those who are most at-risk for geriatric depression. Since other personality domains may modify the risk related to high Neuroticism and low Conscientiousness, the prevention, diagnosis, and treatment of depression could be greatly improved by assessing older patients not only on all five domains of personality but in terms of their combinations.
Keywords: Major depression, minor depression, Neuroticism, Conscientiousness, aging, personality styles, Medicare recipients
Clinically significant mood disorders affect nearly 25% of adults over the age of 65.(1, 2) The societal burden of late-life depression is considerable(1, 2) and the public health burden undeniable: depression increases health care costs(3) and amplifies risk for morbidity and mortality.(4–6) Depression’s societal burden will only be greater in the future as populations worldwide continue to age. For example, by 2030, 20% of the US population is expected to be 65 years of age or older.(7) Despite advances in pharmacological and psychosocial treatments for depression,(8, 9) a substantial portion of patients fail to respond fully to these interventions.(10) Collaborative care studies have revealed similarly sobering findings, (11–13) pointing to the need for a deeper understanding of late-life depression etiology that could inform the development of prevention programs and treatments.
Criteria for diagnosing late-life depression have not been universally endorsed (14) with minor depression’s nosologic status remaining controversial.(15) Prior research typically focused on major depression or dysthymic disorder,(1) to the neglect of the apparently more common experience of minor depression.(16) To date, most studies have primarily relied on treatment-seeking samples. While convenient and informative, these samples are of little relevance to identifying prevention strategies and have limited generalizability.
In contrast, studies of community-based cohorts capture a broader range of depressive symptom severity and are more likely to include individuals not currently in treatment. Prospective studies of community cohorts have consistently shown that personality traits confer risk for clinically significant depression.(17–19) However, most have focused on young adults(20, 21) and none have examined personality predictors of minor depression, which may be etiologically distinct from major depression, though this remains controversial.(20)
From the standpoint of epidemiologic personology(22) and prevention science,(13) prospective research on the personality correlates of late life depression in at-risk community samples should lead to the development of stronger, more targeted treatments and the earlier implementation of person-centered prevention strategies.(23) The Five-Factor Model (FFM) is a multidimensional personality model that specifies that most stable individual differences in emotions, cognition, and behavior can be described by five independent domains: Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness.(24) Research on FFM traits and depression in adults has typically focused on Neuroticism(25, 26) or the additive roles of Neuroticism and Extraversion,(25) yet individual differences in Agreeableness, Openness, or Conscientiousness may also contribute to the development of late life depression. High levels of Agreeableness and Conscientiousness are related to physical health(27, 28) and to the ability to adhere to complex medical regimes,(29) both of which may mitigate socioenvironmental and health-related risks for depression. Higher levels of Openness are related to cognitive flexibility(30) and the presence of larger, supportive social networks,(31) both of which may similarly decrease the risk of developing depression.
Historically, the literature on personality and depression has focused on the independent contributions of individual personality traits. Yet an unexplored possibility is that depression is a product of particular combinations of traits, called personality styles.(32, 33) Personality styles emphasize intraindividual differences as opposed to interindividual differences, and thus are person-centered, rather than variable-centered.(34) Unlike personality types,(35, 36) the concept of personality styles refers to where individuals stand simultaneously on two different domains. For example, “gloomy pessimists” are individuals who score high on Neuroticism and low on Extraversion, and “undercontrolled” individuals score high on Neuroticism and low on Conscientiousness. Recent studies indicate that personality styles hold much promise.(37) Consider the role of the distressed or “Type-D” personality in predicting mortality and cardiovascular disease.(38) Despite its name, “Type-D” personality refers to individuals who score high on negative affect and social inhibition, which are strongly related to Neuroticism and low Extraversion,(38) and, as such, bears a strong resemblance to the “gloomy pessimist” style. Prior research has also shown that the combination of high Neuroticism and low Extraversion may have synergistic effects that lead to depression,(39) though later research was unable to replicate these findings.(40) More broadly, personality styles derived from the FFM are associated with other important health outcomes, such as smoking(37) and HIV disease progression(41) and thus may also contribute to the development of depression.
Based on prior research and theory,(39, 42) we hypothesized that styles characterized by high Neuroticism and low Extraversion (gloomy pessimists) and high Neuroticism and low Conscientiousness (undercontrolled) would be associated with major and minor depression. Given the dearth of research and theory on the risks conferred by other personality trait combinations, these analyses are primarily construed as exploratory or hypothesis-generating. The FFM has been conceptualized as a “hypothesis-generating” tool,(43) especially when applied to clinical issues about which there has been little theorizing or prior research.
The present study extends prior research in three ways. First, we sampled older adults via analyses of data collected in the context of a Medicare Demonstration project(27) with a relatively greater chronic illness burden, a rapidly growing segment of the aging population with high levels of service utilization, disability, and unmet mental health needs. Second, in addition to examining the effects of Neuroticism and Extraversion on new episodes of depression, we examined the effects of the other three personality domains, Openness to Experience, Agreeableness, and Conscientiousness. Third, in addition to just examining individual personality domains we also examined personality styles, thus making this the first attempt to document the impact of personality styles on geriatric mental health. Fourth, in addition to examining the influence of personality on incident major depression, we examined the effects on incident minor depression.
Methods
Participants
Participants were derived from 1,444 community-dwelling men and women aged 65 to 100 who lived in 19 counties in upstate New York, West Virginia, and Ohio. Participants were enrolled in the Medicare Primary and Consumer-Directed Care Demonstration, conducted by the Monroe County Long Term Care Program, Inc. (Rochester, NY) and the Center for Aging and Healthcare in West Virginia, Inc. (Parkersburg, WV). All participants were required to be enrolled in Medicare Part A and Part B, need or receive help with at least two Activities of Daily Living (ADLs) or three Instrumental Activities of Daily Living (IADLs), and have a recent history of significant use of health care services (hospital, nursing home, Medicare home healthcare, or emergency department). The Medicare demonstration involved a baseline assessment and two additional assessments taking place approximately 12- and 22-months post-baseline.
At baseline, personality was not assessed for 247 participants and not scored for 51 others who failed a cognitive screen (see Weiss and Costa (27) for a description). We also excluded 13 participants who were ineligible for other reasons, 1 not classified with respect to eligibility, 1 who did not provide information on educational achievement, and 7 for whom self-reported disability was unavailable. Of the remaining 1,124 participants, 227 died between baseline and follow-up, 164 were excluded because they failed the cognitive screen at the 22-month follow-up. In addition, 49 participants were excluded because of invalid personality questionnaires (see Weiss and Costa (27), p. 725 for more details), and 23 were excluded because data on depression were unavailable at baseline (n = 1), 12-month follow-up (n = 17 ), or the 22-month follow-up (n = 5).
Measures
Depression
At baseline and both follow-ups, the presence of active major and minor depressive episodes was assessed using the Mini-International Neuropsychiatric Major Depressive Episode Module (MINI-MDE) (44, 45) and scored based on DSM-IV criteria. The patient-rated version of the MINI-MDE is reliable and well-validated.(46) In the present study, the time period was extended to the past month. Data on depression in this sample has been previously reported.(47)
Participants who were not depressed at any of the three time points (n = 390) were compared to participants who were not depressed at baseline, but subsequently developed (1) major depression at either of the two follow-ups (incident major depressed; n = 66) or (2) minor, but not major, depression at either of the follow-ups (incident minor depressed; n = 56). The remaining 149 participants who met criteria for an episode of major or minor depression at baseline were excluded from the analyses.
Personality
Personality was assessed at baseline via the NEO Five Factor Inventory (NEO-FFI46). The NEO-FFI is a well-validated 60-item short form of the 240-item NEO-PI-R in which each of the five domains of the FFM is represented by 12 items.(48) Each item is rated on a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.” Psychometric properties of the NEO-FFI domains in this sample have been previously described.(49)
As specified in the Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual,(48) we scored missing items as neutral and created raw domain scores. We then used the adult combined gender norms in the NEO Manual to convert raw domain scores into T-scores which have a mean of 50 and standard deviation of 10.(48) For the purpose of the analyses, domain T-scores were centered on a mean of 50.
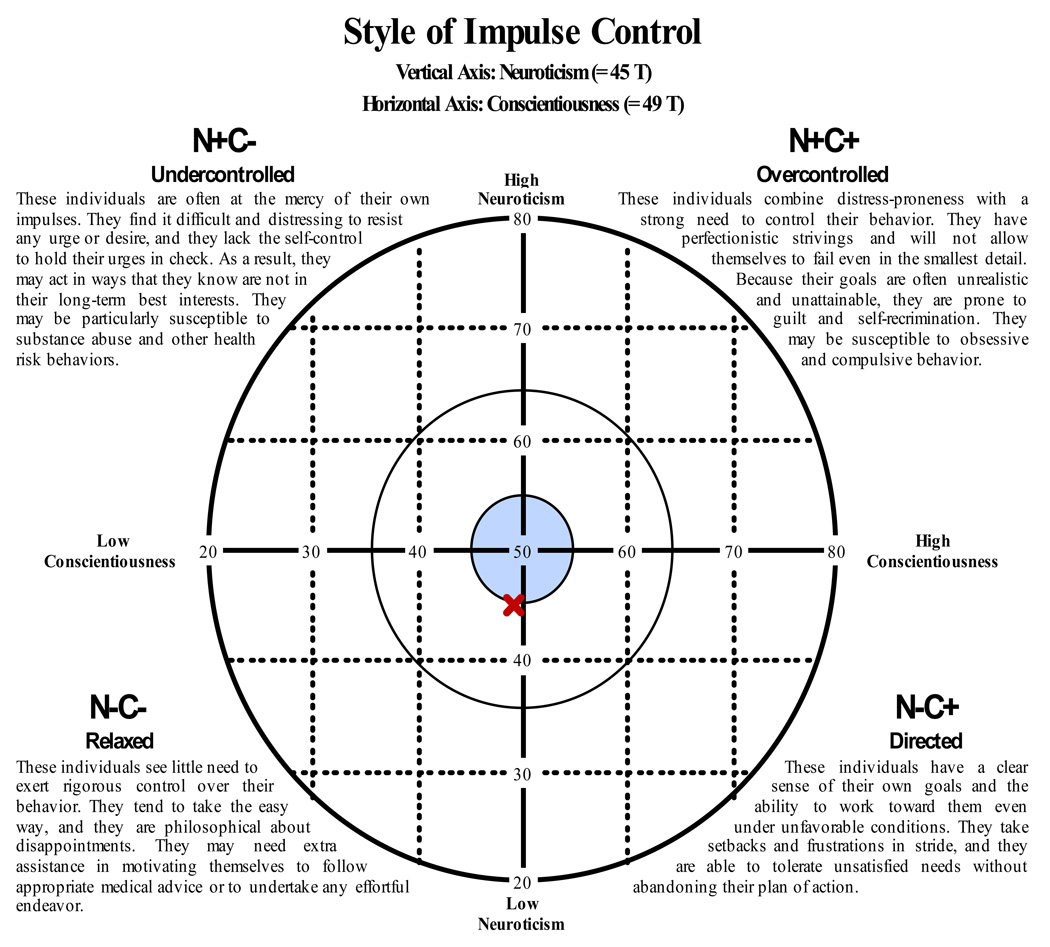
Uncentered domain T-scores scores were used to determine whether participants could be classified in terms of a personality style; that is, a combination of two personality domains. Participants were characterized on NEO style graphs(32) by converting their domain T-scores into z-scores and then plotting all ten possible combinations of two dimensions against one another.(33) Each plot yielded four quadrants reflecting whether a participant was high or low on the first dimension and high or low on the second dimension (see Figure). For each possible pairing of domains, participants whose z-scores were at least one-half standard deviation above or below average for both domains were classified as being high-high (++), high-low (+−), low-high (−+), or low-low (−−); participants who fell into one of these four classifications were coded as 1 for that classification and 0 for the other three classifications. Participants whose z-scores fell within the average range on both domains were classified as not having a style; these participants were coded as 0. Thus, the styles represent individuals who did not score in the average range on both dimensions.
Figure 1.
Example style graph of the combination of Neuroticism and Conscientiousness (Style of Impulse Control). Individuals who fall within the area of the blue circle are considered not to have a type; that is, those who score within one-half standard deviation (t-score between 45 and 55) from the mean on Neuroticism or Conscientiousness.
Covariates
Demographic covariates included gender (0 = male; 1 = female), age, highest educational achievement (1 = 8th grade or less; 2 = some high school, but did not graduate; 3 = high school graduate or GED; 4 = some college or two year degree; 5 = four year college graduate; 6 = more than a four year college degree), number of self-reported chronic illnesses, a composite measure of disability based on modified questions from the Home Care version of the Minimum Data Set(50) and a composite subjective health score based on the Physical Summary scale of the SF-36(51) and answers to two questions: “Compared to others your age would you say your ability to care for yourself is?” and “Compared to others your age would you say your health is?” Principal components analysis indicated that these three scores formed a single component; we therefore used the mean of these scales. Finally, because participants took part in an intervention study, we included a categorical variable indicating which intervention they received (0 = standard care; 1 = health care vouchers; 2 = home care nurse; 3 = vouchers plus home care nurse).
Statistical Analyses
We conducted two series of logistic regression analyses to examine the influence of personality traits on incident major and minor depression. First, we examined the independent influence of the five NEO-FFI domain scores and their interactions, controlling for covariates. These analyses informed our approach to the hypothesis-generating analyses. Second, we examined the effect of personality styles. As described in the Introduction, the hypothesis-testing analyses focused on the joint contributions of Neuroticism and Extraversion (N+E−) as well as Neuroticism and Conscientiousness (N+C−). To reduce the number of potential hypothesis-generating analyses we concentrated on those domains that were shown to confer risk in the first set of analyses. For example, if a high level of Neuroticism was shown to confer risk, we examined whether it, in combination with high or low levels of Openness and Agreeableness and low levels of Extraversion and Conscientiousness elevated risk (analyses of the combinations of high Neuroticism with low Extraversion or low Conscientiousness were construed as hypothesis-testing). In the first block, we entered all the covariates. In the second block, we entered four dummy-coded (0 or 1) variables that indicated participants’ personality style for each pair of domains (i.e., high on both domains, low on both domains, high on the first, low on the second; low on the first, high on the second). Participants not classified in terms of a style received a score of 0 on all four dummy-coded variables. Odds ratios thus show the likelihood of depression for participants who are one of the four styles compared to all other participants. In our second set of analyses, we take a more clinical approach and ask whether individuals who score beyond a specified threshold on two personality traits are more likely to develop depression. The threshold is 1/2 SD above and/or below the mean in the current sample.
Finally, although we set the significance level to p < .05, to balance concerns over Type I and Type II errors, we indicate which findings are significant at a more stringent level of significance (p < .01), in addition to those significant at the p < .05 level.
Results
Table 1 shows the demographic and descriptive data for all participants at baseline, grouped by depression status at follow-up. Note that all participants were screened for depression at each assessment and were excluded if they met the criteria for depression at baseline; thus, all participants were free of depression at baseline. In addition, all participants were cognitively intact at each assessment. Compared to healthy elderly individuals, participants in this sample had significantly more health conditions and hospitalizations and significantly lower physical and mental health functioning.(52)
Table 1.
Baseline Characteristics of the Total Sample and by Depression Status at Follow-up
| Depression Status at Follow-up | ||||||||
|---|---|---|---|---|---|---|---|---|
| No Depression | Major Depression | Minor Depression | Total | |||||
| Baseline | M | SD | M | SD | M | SD | M | SD |
| Age | 78.90 | 7.38 | 78.89 | 6.64 | 78.09 | 6.72 | 78.56 | 7.21 |
| Education | 2.98 | 1.39 | 2.50 | 1.35 | 2.80 | 1.31 | 2.92 | 1.36 |
| Self-reported chronic illnesses | 4.48 | 2.08 | 5.08 | 2.16 | 4.13 | 1.82 | 4.61 | 2.13 |
| ADL restrictions | 0.83 | 1.16 | 0.89 | 1.08 | 0.96 | 1.28 | 0.89 | 1.18 |
| IADL restrictions | 3.32 | 1.85 | 3.51 | 1.79 | 3.45 | 1.74 | 3.46 | 1.80 |
| Subjective health | 0.12 | 0.80 | −0.16 | 0.64 | −0.05 | 0.76 | 0.00 | 0.79 |
| NEO-FFI domain T-scores | ||||||||
| Neuroticism | 49.64 | 7.50 | 56.85 | 8.40 | 53.42 | 8.55 | 52.22 | 8.54 |
| Extraversion | 47.21 | 7.19 | 44.86 | 7.13 | 45.46 | 9.17 | 46.43 | 7.50 |
| Openness to Experience | 44.21 | 7.27 | 43.46 | 8.15 | 44.63 | 9.30 | 44.29 | 7.64 |
| Agreeableness | 49.61 | 8.54 | 46.21 | 10.27 | 50.25 | 8.48 | 48.93 | 8.83 |
| Conscientiousness | 47.09 | 7.35 | 42.43 | 7.93 | 43.11 | 9.85 | 46.10 | 7.93 |
| N | % | N | % | N | % | N | % | |
| Gender | ||||||||
| Male | 99 | 25 | 15 | 23 | 6 | 11 | 156 | 24 |
| Female | 291 | 75 | 51 | 77 | 50 | 89 | 505 | 76 |
Note. N = 512. The sample ranged from 65 to 100 years of age, n = 390 for no depression, n = 66 for incident major depression, n = 56 for incident minor depression.
Domain-level Personality and Incident Depression
Using logistic regression, we predicted incident depression from baseline personality, controlling for gender, age, education, chronic illness, disability, and subjective health. The same pattern emerged for both major and minor incident depression: Elevated Neuroticism and low levels of Conscientiousness confer risk (see Table 2). Only the effect of Neuroticism on incident major depression, however, was significant at p < .01. None of the covariates, measured at baseline, including disability and subjective health, were significant predictors of either major or minor incident depression.
Table 2.
Baseline Predictors of Incident Major and Minor Depression: Results of Multivariate Logistic Regressions
| Incident Depression |
||||
|---|---|---|---|---|
| Major | Minor | |||
| OR | 95% CI | OR | 95% CI | |
| Female vs. Male | 1.024 | 0.487–2.154 | 2.184 | 0.856–5.572 |
| Age | 1.023 | 0.980–1.068 | 0.988 | 0.947–1.030 |
| Education | 0.878 | 0.694–1.110 | 0.877 | 0.691–1.113 |
| Self-reported chronic illnesses | 1.052 | 0.917–1.208 | 0.885 | 0.761–1.028 |
| Composite disability score | 0.936 | 0.662–1.323 | 0.994 | 0.705–1.401 |
| Subjective health | 0.706 | 0.448–1.128 | 0.849 | 0.548–1.316 |
| Neuroticism | 1.086*a | 1.045–1.128 | 1.045* | 1.003–1.088 |
| Extraversion | 0.988 | 0.946–1.032 | 0.989 | 0.948–1.033 |
| Openness | 0.998 | 0.956–1.043 | 1.013 | 0.970–1.057 |
| Agreeableness | 0.984 | 0.948–1.020 | 1.021 | 0.982–1.062 |
| Conscientiousness | 0.951* | 0.914–0.989 | 0.954* | 0.917–0.993 |
Note. n = 66 for major depression, n = 56 for minor depression, and n = 390 for no depression. OR = Odds ratios; CI = Confidence interval.
p < .05.
p < .01.
These odds ratios indicate that each one point increase in Neuroticism is equal to an 8.6% and 4.5% increase in the likelihood of major and minor depression, respectively, and that each point decrease in Conscientiousness is equal to 4.9% and 4.6% increase in their respective likelihood of major and minor depression, respectively. By raising odds ratios to a power equal to the standard deviation (10), we can determine that a standard deviation increase in Neuroticism was related to a 2.28 and 1.55 increases the likelihood of major and minor depression, respectively. Likewise, every standard deviation increase in Conscientiousness was related to a 0.60 and 0.62 factor decrease in the likelihood of major and minor depression, respectively.
We were next interested in whether the linear combination of two traits confers risk for incident major and minor depression. We ran a series of regressions predicting both types of depression from the main effects and interaction of each pair of traits, controlling for the covariates. None of these interactions were significant and these analyses will not be discussed further.
Personality Styles and Incident Depression
Although we found no interaction between traits assessed continuously, the combination of scoring at the extreme of two traits may confer risk for incident depression. Thus, in our second set of analyses, we take a more clinical approach and test whether surpassing a certain threshold (1/2 SD above and below the mean) on two traits in combination predicted depression. We again used logistic regression to examine whether incident depression was related to baseline personality, controlling for the covariates (see Table 3). Six of the eight combinations that include low Conscientiousness were associated with subsequent major depression: undercontrolled (N+C−), lethargic (E−C−), and undistinguished (A−C−), at p < .01 and funlovers (E+C−), dreamers (O+C−), and reluctant scholars (O−C−) at p < .05. Only the relaxed (N−C−) and well-intentioned (A+C−) styles were not risk-factors. Thus, in combination with low levels of Conscientiousness, high and low levels of both Extraversion and Agreeableness confer risk and in no case did a style that included high Conscientiousness emerge as a significant protective factor. Not surprisingly, three styles that include high Neuroticism were associated with incident major depression: the gloomy pessimist (N+E−), overly emotional (N+E+), and hypersensitive (N+O+). The easy-going (N−A+) style was protective. These styles were significant at p < .05.
Table 3.
Baseline Personality Styles Associated with Incident Major and Minor Depression: Results of Multivariate Logistic Regressions
| Incident Depression |
||||||
|---|---|---|---|---|---|---|
| Major | Minor | |||||
| Personality Style | n | OR | 95% CI | n | OR | 95% CI |
| Style of well-being | ||||||
| N+E−: Gloomy pessimists | 132 | 2.365* | 1.011–5.532 | 123 | 1.854 | 0.767–4.483 |
| N+E+: Overly emotional | 56 | 2.957* | 1.130–7.737 | 49 | 1.716 | 0.582–5.057 |
| N−E+: Upbeat optimists | 74 | 0.382 | 0.096–1.519 | 79 | 1.117 | 0.386–3.230 |
| N−E−: Low-keyed | 118 | 0.603 | 0.212–1.720 | 119 | 0.757 | 0.271–2.114 |
| No style | 76 | 76 | ||||
| Style of defense | ||||||
| N+O−: Maladaptive | 166 | 2.365 | 0.858–6.522 | 153 | 1.404 | 0.531–3.712 |
| N+O+: Hypersensitive | 27 | 3.600* | 1.012–12.812 | 24 | 1.911 | 0.506–7.210 |
| N−O+: Adaptive | 47 | 0.866 | 0.212–3.534 | 48 | 0.922 | 0.254–3.343 |
| N−O−: Hyposensitive | 168 | 0.479 | 0.150–1.532 | 172 | 0.589 | 0.208–1.666 |
| No style | 48 | 49 | ||||
| Style of anger control | ||||||
| N+A−: Temperamental | 107 | 2.155 | 0.976–4.761 | 91 | 0.987 | 0.402–2.425 |
| N+A+: Timid | 74 | 1.557 | 0.654–3.711 | 74 | 1.494 | 0.630–3.546 |
| N−A+: Easy-going | 128 | 0.338* | 0.119–0.966 | 133 | 0.597 | 0.242–1.476 |
| N−A−: Cold blooded | 66 | 0.545 | 0.173–1.714 | 67 | 0.758 | 0.255–2.250 |
| No style | 81 | 81 | ||||
| Style of impulse control | ||||||
| N+C−: Undercontrolled | 139 | 3.267*a | 1.481–7.206 | 128 | 3.005* | 1.232–7.332 |
| N+C+: Overcontrolled | 37 | 1.309 | 0.401–4.281 | 35 | 1.069 | 0.257–4.456 |
| N−C+: Directed | 75 | 0.455 | 0.117–1.774 | 78 | 1.055 | 0.331–3.366 |
| N−C−: Relaxed | 116 | 0.862 | 0.330–2.248 | 118 | 1.323 | 0.492–3.557 |
| No style | 89 | 87 | ||||
| Style of activity | ||||||
| E+C−: Funlovers | 67 | 3.453* | 1.195–9.982 | 63 | 1.515 | 0.551–4.167 |
| E+C+: Go-getters | 47 | 1.285 | 0.302–5.476 | 49 | 1.281 | 0.402–4.088 |
| E−C+: Plodders | 65 | 2.441 | 0.793–7.518 | 63 | 1.190 | 0.402–3.520 |
| E−C−: The lethargic | 177 | 4.064*a | 1.630–10.131 | 167 | 1.810 | 0.826–3.967 |
| No style | 100 | 104 | ||||
| Style of learning | ||||||
| O+C−: Dreamers | 48 | 3.588* | 1.088–11.833 | 45 | 2.424 | 0.681–8.622 |
| O+C+: Good students | 15 | 3.090 | 0.524–18.220 | 15 | 2.573 | 0.428–15.451 |
| O−C+: By-the-bookers | 101 | 1.476 | 0.469–4.640 | 102 | 1.758 | 0.571–5.417 |
| O−C−: Reluctant scholars | 210 | 3.305* | 1.240–8.813 | 202 | 2.887* | 1.072–7.775 |
| No style | 82 | 82 | ||||
| Style of character | ||||||
| A+C−: Well-intentioned | 116 | 1.680 | 0.738–3.823 | 120 | 2.601* | 1.086–6.230 |
| A+C+: Effective altruists | 64 | 0.347 | 0.073–1.650 | 68 | 1.253 | 0.404–3.886 |
| A−C+: Self-promoters | 35 | 1.436 | 0.413–4.986 | 33 | 0.986 | 0.193–5.049 |
| A−C−: The undistinguished | 133 | 2.888*a | 1.344–6.207 | 120 | 2.306 | 0.940–5.657 |
| No style | 108 | 108 | ||||
Note. For each style, group membership was coded 1; participants who were not classified into a style were coded 0 on all four group membership variables. All analyses control for gender, age, education, number of self-reported chronic illnesses, composite disability score, and subjective health. n = 66 for major depression, n = 56 for minor depression, and n = 390 for no depression. OR = Odds ratio; CI = Confidence interval
p < .05.
p < .01.
Analysis of the styles that examined incident minor depression revealed that, as with major depression, the undercontrolled style of impulse control (N+C−) and reluctant scholar style of learning (O−C−) were associated with incident minor depression (p < .05). In addition, the well-intentioned (A+C−) style of character was also associated with minor depression (p < .05).
Discussion
Consistent with previous findings,(25, 26) we found higher Neuroticism to be a risk marker for incident major and minor depression, independent of demographic and health risk factors. Lower Conscientiousness also emerged as a significant risk marker. None of the other personality domains were, by themselves, related to incident major or minor depression.
By examining trait combinations, we found evidence that Extraversion, Openness, and Conscientiousness played a role in determining whether high Neuroticism was related to incident major depression: the gloomy pessimists (N+E−), overly emotional (N+E+), hypersensitive (N+O+), and undercontrolled (N+C−) were at greater risk than other participants. We also found that low Extraversion, low Openness, and low Agreeableness amplify the risk conferred by low Conscientiousness.
Whereas these and other trait combinations were prospectively associated with major depression, only three styles, the undercontrolled (N+C−), reluctant scholars (O−C−), and well-intentioned (A+C−), were associated with minor depression. These findings raise the possibility that personality styles may be less important in the etiology of minor depression, even while the individual domains of Neuroticism and Conscientiousness are just as central to minor as major depression.
Individuals with the combination of high Neuroticism and low Conscientiousness – the undercontrolled style – appear to be the most vulnerable to developing depression. Individuals characterized by the undercontrolled style often find it difficult to control their impulses(37), even when they know their actions are incongruent with their long-term interests.(33) In the present research, this dispositional difficulty with impulse control was associated with the development of both major and minor depression, perhaps because these individuals are particularly vulnerable to the deleterious effects of poor self-management of health concerns. Neuroticism has long been identified as a risk-factor for depression; low Conscientiousness may augment that risk, high Conscientiousness may mitigate it.
Our findings broaden the understanding of personality and depression in the elderly in several ways. First, in addition to the anticipated effect of Neuroticism, our findings highlight the role of low Conscientiousness in predicting incident depression among the frail elderly. Individuals low in Conscientiousness may be more challenged by needing to manage their own care, navigating the complexities of the health care delivery system, and achieving personal goals despite limitations.(53) Second, our findings highlight the importance of considering styles or combinations of personality domains. The analysis of styles suggests that rather than high Conscientiousness being protective, low Conscientiousness confers risk for mood disorders in this sample. Moreover, this risk is not solely specific to combinations of low Conscientiousness with high Neuroticism, but is also seen in combination with high or low scores on Extraversion, Agreeableness, and Openness. The findings that both low and high levels of Extraversion confer risk for depression in this context is particularly noteworthy as prior research on the role of low Extraversion in depression have been conflicting.(26)(54) Too often it is erroneously assumed that either high or low levels of a trait are pathogenic. The analysis of personality styles is not based on this assumption. Instead, it is consistent with the idea that high and low levels of traits can be pathogenic, and that all traits have adaptive and maladaptive consequences.(48) Third, while Neuroticism is strongly related to depression risk, many individuals who are high in Neuroticism live depression-free lives even in extreme old age, as data from this sample attest. Our findings suggest the intriguing possibility that those who live depression-free despite high levels of Neuroticism possess particular traits that serve to protect them, such as average to high Conscientiousness.
These findings should be of interest to treatment-providers. It is the rare clinician who ignores patient personality in creating and sustaining patient relationships, formulating assessments, and planning prevention, treatment or service-delivery strategies. Rather, clinicians adopt nuanced and complex views of their patients. By introducing the idea of personality styles to geriatric psychiatry, we aim to avoid the Scylla of the standard one-trait emphasis on, for example, Neuroticism and the Charybdis of examining personality disorders with dubious validity and relevance to older adults.(55) Moreover, an emphasis on styles points to different approaches to depression prevention and treatment in the elderly. Because low Conscientiousness by itself or in combination with other domains confers risk for incident depression over and above that posed by Neuroticism, strategies to enhance the ability of individuals to identify or maintain roles, hobbies, and routines may be particularly effective,(56) as deficits in these goal-oriented behaviors are distinguishing features of patients low in Conscientiousness. Our findings point to the potential utility of personality styles in identifying patients who might benefit from a trial targeting the prevention of major depression. Such an approach should be the focus of future intervention research.
The analysis of styles also has practical utility in daily practice. In contrast to personality scientists, who are trained to think dimensionally, clinicians tend to think categorically. Style membership is a source of conceptual economy for the clinician, as it conveys information about two or more variables simultaneously.(57)
The present study was not without limitations. First, while we reduced the number of significance tests for the styles analyses by focusing only on styles related to Neuroticism and Conscientiousness, we did not use a formal correction to control for Type I errors. We chose this approach because, in the presence of a large number of predictors, standard methods of correcting for Type I errors (e.g., the Bonferroni) overcorrect and lead to a preponderance of Type II errors. While Type I errors are serious in clinical intervention studies, as they can lead to the implementation of costly programs that may be ineffective, Type II errors are more serious when they impair capacity to identify at-risk individuals. Given the significant unmet need for services among the depressed elderly, statistical procedures that further obscure risk detection are highly questionable. To alleviate concerns about Type I errors, however, we did note which findings were significant at a more stringent p-value (p < .01) and focus discussion on findings that were theoretically meaningful. Second, the present sample was mostly white and unique in its advanced age, poor health, and lower educational achievement. Therefore, the present findings may not describe general characteristics of major and minor depression or apply to other populations. Third, the MINI-MDE has not been used to assess minor depression nor validated against measures of minor depression. As such, the results for minor depression should be interpreted more cautiously than those with respect to major depression. Finally, data on prior depressive episodes were unavailable.
In conclusion, the present research demonstrates that combinations of traits influence risk for depression in the frail elderly. Our findings suggest that assessment of all five personality domains could improve the quality of care in geriatric depression and underscore the need for prevention studies that target participants who are high in Neuroticism and low in Conscientiousness. To gain a better, more nuanced understanding of depression and to be able to better predict who is at risk for major or minor depression requires the assessment of the full FFM and other clinical measures. Studying how these factors work synergistically and examining predictors that are common to and unique to different mood disorders will enable us to understand the biopsychosocial causes of depression and help insure the psychological and perhaps even the physical well-being of the oldest members of our communities.
Acknowledgements
We thank the Centers for Medicare and Medicaid Services for sponsoring the Medicare demonstration, “A Randomized Controlled Trial of Primary and Consumer Directed Care for People with Chronic Illnesses,” CMS 95-C-90467. We also are grateful to the P.I., Gerald M. Eggert, and the Co-PI, Brenda Wamsley, of the demonstration and the staff who collected the data as well as the patients and caregivers who participated in the demonstration. Additionally, Bruce Friedman acknowledges time funded by the National Institute of Mental Health for Mentored Research Scientist Development Award K01 MH64718-01 and Paul R. Duberstein acknowledges funding from United States Public Health Service Grant K24MH072712. We also wish to thank Ben Chapman and Robert McCrae for their thoughtful comments and suggestions on an earlier draft. This research was supported in part by the Intramural Research Program of the National Institute on Aging/NIH.
Footnotes
Disclosure: Paul T. Costa, Jr. receives royalties from the Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI).
Contributor Information
Alexander Weiss, Department of Psychology, School of Philosophy, Psychology, and the Language Sciences, The University of Edinburgh
Angelina R. Sutin, Laboratory of Personality and Cognition, National Institute on Aging, National Institutes of Health, Department of Health and Human Services
Paul R. Duberstein, Laboratory of Personality and Development, Department of Psychiatry, University of Rochester Medical Center
Bruce Friedman, Departments of Community and Preventive Medicine, and Psychiatry, University of Rochester Medical Center
R. Michael Bagby, Clinical Research Department, Centre for Addiction and Mental Health, Toronto, Canada
Paul T. Costa, Jr., Laboratory of Personality and Cognition, National Institute on Aging, National Institutes of Health, Department of Health and Human Services.
References
- 1.Charney DS, Reynolds CF, Lewis L, et al. Depression and bipolar support alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry. 2003;60:664–672. doi: 10.1001/archpsyc.60.7.664. [DOI] [PubMed] [Google Scholar]
- 2.Lebowitz BD, Pearson JL, Schneider LS, et al. Diagnosis and treatment of depression in late life: Consensus statement update. JAMA. 1997;278:1186–1190. [PubMed] [Google Scholar]
- 3.Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 4.Beekman AT, Penninx BW, Deeg DJ, et al. Depression and physical health in later life: results from the Longitudinal Aging Study Amsterdam (LASA) J Affect Disord. 1997;46:219–231. doi: 10.1016/s0165-0327(97)00145-6. [DOI] [PubMed] [Google Scholar]
- 5.Frojdh K, Hakansson A, Karlsson I, et al. Deceased, disabled or depressed - A population-based 6-year follow-up study of elderly people with depression. Soc Psychiatry Psychiatr Epidemiol. 2003;38:557–562. doi: 10.1007/s00127-003-0670-z. [DOI] [PubMed] [Google Scholar]
- 6.Blazer DG, Hybels CF. What symptoms of depression predict mortality in community-dwelling elders? J Am Geriatr Soc. 2004;52:2052–2056. doi: 10.1111/j.1532-5415.2004.52564.x. [DOI] [PubMed] [Google Scholar]
- 7.United States Census Bureau. National Population Projections. 2003 [Google Scholar]
- 8.American Psychiatric Association: Practice guidelines for the treatment of patients with major depressive disorder. Am J Psychiatry. 2000;157:1–78. [PubMed] [Google Scholar]
- 9.Hollon SD, Thase ME, Markowitz JC. Treatment and prevention of depression. Psychological Science in the Public Interest. 2002;3:39–77. doi: 10.1111/1529-1006.00008. [DOI] [PubMed] [Google Scholar]
- 10.Lee AS. Better outcomes for depressive disorders? Psychol Med. 2003;33:769–774. doi: 10.1017/s003329170300802x. [DOI] [PubMed] [Google Scholar]
- 11.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing Suicidal Ideation and Depressive Symptoms in Depressed Older Primary Care Patients: A Randomized Controlled Trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 12.Bartels SJ, Coakley EH, Zubritsky C, et al. Improving access to geriatric mental health services: A randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004;161:1455–1462. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- 13.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 14.Blazer DG. Depression in late life: Review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 15.Pincus HA, Davis WW, McQueen LE. ‘Subthreshold’ mental disorders: A review and synthesis of studies on minor depression and other ‘brand names’. Br J Psychiatry. 1999;174:288–296. doi: 10.1192/bjp.174.4.288. [DOI] [PubMed] [Google Scholar]
- 16.Lyness JM, Kim J, Tang W, et al. The clinical significance of subsyndromal depression in older primary care patients. Am J Geriatr Psychiatry. 2007;15:214–223. doi: 10.1097/01.JGP.0000235763.50230.83. [DOI] [PubMed] [Google Scholar]
- 17.Krueger RF. Personality Traits in Late Adolescence Predict Mental Disorders in Early Adulthood: A Prospective-Epidemiological Study. J Pers. 1999;67:39–65. doi: 10.1111/1467-6494.00047. [DOI] [PubMed] [Google Scholar]
- 18.Pelkonen M, Marttunen M, Aro H. Risk for depression: A 6-year follow-up of Finnish adolescents. J Affect Disord. 2003;77:41–51. doi: 10.1016/s0165-0327(02)00098-8. [DOI] [PubMed] [Google Scholar]
- 19.Kendler KS, Kuhn J, Prescott CA. The Interrelationship of Neuroticism, Sex, and Stressful Life Events in the Prediction of Episodes of Major Depression. Am J Psychiatry. 2004;161:631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- 20.Ormel J, Oldehinkel AJ, Brilman EI. The interplay and etiological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first and recurrent depressive episodes in later life. Am J Psychiatry. 2001;158:885–891. doi: 10.1176/appi.ajp.158.6.885. [DOI] [PubMed] [Google Scholar]
- 21.Steunenberg B, Beekman ATF, Deeg DJH, et al. Personality and the onset of depression in late life. J Affect Disord. 2006;92:243–251. doi: 10.1016/j.jad.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Krueger RF, Caspi A, Moffitt TE. Epidemiological personology: The unifying role of personality in population-based research on problem behaviors. J Pers. 2000;68:967–998. doi: 10.1111/1467-6494.00123. [DOI] [PubMed] [Google Scholar]
- 23.Smit F, Ederveen A, Cuijpers P, et al. Opportunities for cost-effective prevention of late-life depression: An epidemiological approach. Arch Gen Psychiatry. 2006;63:290–296. doi: 10.1001/archpsyc.63.3.290. [DOI] [PubMed] [Google Scholar]
- 24.McCrae RR, Costa PT., Jr . Personality in adulthood: A Five-Factor Theory perspective. New York, NY: Guilford Press; 2003. [Google Scholar]
- 25.Kendler KS, Gatz M, Gardner CO, et al. Personality and major depression: A Swedish longitudinal, population-based twin study. Arch Gen Psychiatry. 2006;63:1113–1120. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- 26.Duberstein PR, Pálsson SP, Waern M, et al. Personality and risk for depression in a birth cohort of 70-year-olds followed for 15 years. Psychol Med. 2008;38:663–671. doi: 10.1017/S0033291707002620. [DOI] [PubMed] [Google Scholar]
- 27.Weiss A, Costa PT., Jr Domain and facet personality predictors of all-cause mortality among medicare patients aged 65 to 100. Psychosom Med. 2005;67:724–733. doi: 10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- 28.Chapman BP, Lyness JM, Duberstein P. Personality and medical illness burden among older adults in primary care. Psychosom Med. 2007;69:277–282. doi: 10.1097/PSY.0b013e3180313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christensen AJ, Smith TW. Personality and patient adherence: Correlates of the 5-Factor Model in renal dialysis. J Behav Med. 1995;18:305–313. doi: 10.1007/BF01857875. [DOI] [PubMed] [Google Scholar]
- 30.McCrae RR, Costa PT., Jr . In: Conceptions and correlates of Openness to Experience, in Handbook of personality psychology. Hogan R, Johnson J, Briggs S, editors. San Diego, CA: Academic Press; 1997. pp. 825–847. [Google Scholar]
- 31.Lang FR, Staudinger UM, Carstensen LL. Perspectives on socioemotional selectivity in late life: how personality and social context do (and do not) make a difference. J Gerontol B Psychol Sci Soc Sci. 1998;53:P21–P29. doi: 10.1093/geronb/53b.1.p21. [DOI] [PubMed] [Google Scholar]
- 32.Costa PT, Jr, McCrae RR. Manual supplement for the NEO-4. Odessa, FL: Psychological Assessment Resources; 1998. [Google Scholar]
- 33.Costa PT, Jr, Piedmont RL. In: Interpretation of the NEO personality inventory profiles of Madeline G. Self, partner and an integrated perspective, in Paradigms of personality assessment. Wiggins JS, editor. New York, NY: Guilford Press; 2003. [Google Scholar]
- 34.Asendorpf JB. Head-to-head Comparison of the Predictive Validity of Personality Types and Dimensions. European Journal of Personality. 2003;17:327–346. [Google Scholar]
- 35.Block J. Lives through time. Berkeley, CA: Bancroft Books; 1971. [Google Scholar]
- 36.Funder DC. The personality puzzle. 2nd. New York, NY: W. W. Norton; 2001. [Google Scholar]
- 37.Terracciano A, Costa PT., Jr Smoking and the Five-Factor Model of personality. Addiction. 2004;99:472–481. doi: 10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Denollet J. DS14: Standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med. 2005;67:89–97. doi: 10.1097/01.psy.0000149256.81953.49. [DOI] [PubMed] [Google Scholar]
- 39.Gershuny BS, Sher KJ. The relation between personality and anxiety: Findings from a 3-year prospective study. J Abnorm Psychol. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- 40.Jorm AF, Christensen H, Henderson AS, et al. Predicting anxiety and depression from personality: Is there a synergistic effect of neuroticism and extraversion? J Abnorm Psychol. 2000;109:145–149. doi: 10.1037//0021-843x.109.1.145. [DOI] [PubMed] [Google Scholar]
- 41.Ironson GH, O'Cleirigh C, Weiss A, et al. Personality and HIV disease progression: Role of NEO-PI-R openness, extraversion, and profiles of engagement. Psychosom Med. 2008;70:245–253. doi: 10.1097/PSY.0b013e31816422fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chapman BP, Duberstein PR, Lyness JM. The distressed personality type: Replicability and general health associations. European Journal of Personality. 2007;21:911–929. [Google Scholar]
- 43.Duberstein PR, Conwell Y, Seidlitz L, et al. Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J Gerontol B Psychol Sci Soc Sci. 2000;55:P18–P26. doi: 10.1093/geronb/55.1.p18. [DOI] [PubMed] [Google Scholar]
- 44.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 45.Sheehan DV, Janavs J, Baker R, et al. MINI - Mini International Neuropsychiatric Interview - English Version 5.0.0 - DSM-IV. J Clin Psychiatry. 1998;59:34–57. [PubMed] [Google Scholar]
- 46.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–241. [Google Scholar]
- 47.Friedman B, Conwell Y, Delavan RL. Correlates of late-life major depressions: A comparison of urban and rural primary care patients. Am J Geriatr Psychiatry. 2007;15:28–41. doi: 10.1097/01.JGP.0000224732.74767.ad. [DOI] [PubMed] [Google Scholar]
- 48.Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) prefessional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 49.Weiss A, Costa PT, Jr, Duberstein PR, et al. Cross-sectional age differences in personality among Medicare patients aged 65 to 100. Psychol Aging. 2005;20:182–185. doi: 10.1037/0882-7974.20.1.182. [DOI] [PubMed] [Google Scholar]
- 50.Morris JN, Hawes C, Fries BE, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30:293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- 51.Ware JE, Kosinski M. Lincoln, RI: QualityMetric; 2001. SF-36 Physical & Mental Health Summary Scales: A manual for users of version 1, 2. [Google Scholar]
- 52.Löckenhoff CE, Sutin AR, Ferrucci L, et al. Personality, subjective health, and vulnerability: The association between NEO-PI-R and SF-36 in advanced age differs across samples that vary in impairment levels. Journal of Research in Personality. in press. [Google Scholar]
- 53.Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychol Bull. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- 54.McCray LW, Bogner HR, Sammel MD, et al. The role of patient personality in the identification of depression in older primary care patients. Int J Geriatr Psychiatry. 2007;22:1095–1100. doi: 10.1002/gps.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abrams RC, Bromberg CE. Personality disorders in the elderly: A flagging field of inquiry. Int J Geriatr Psychiatry. 2006;21:1013–1017. doi: 10.1002/gps.1614. [DOI] [PubMed] [Google Scholar]
- 56.Chapman B, Duberstein P, Lyness JM. Personality traits, education, and health-related quality of life among older adult primary care patients. Jour J Gerontol B Psychol Sci Soc Sci. 2007;62:P343–P352. doi: 10.1093/geronb/62.6.p343. [DOI] [PubMed] [Google Scholar]
- 57.Costa PT, Herbst JH, McCrae RR, et al. The replicability and utility of three personality types. European Journal of Personality. 2002;16:S73–S87. [Google Scholar]