Abstract
Background
Given the low prevalence of and racial/ethnic disparities in colorectal cancer (CRC) screening, it is important to monitor whether prevalence and disparities are increasing or decreasing over time.
Methods
We estimated the prevalence of CRC screening by year (2001, 2003 and 2005), modality (endoscopy, fecal occult blood test, either) and recency (ever had, up-to-date) for the California population as a whole, major racial/ethnic groups (White, Black, Latino, Asian), and selected Asian subgroups (Chinese, Filipino, Japanese, Korean, Vietnamese) using data from the California Health Interview Survey. All prevalence estimates were age- and gender-standardized.
Results
Between 2001 and 2005, prevalence of up-to-date screening increased significantly among Whites and Latinos but not among Blacks and Asian Americans. Screening prevalence varied substantially among Asian subgroups, with Korean, Filipino and Vietnamese Americans having the lowest prevalence. Korean Americans were the only group in the analysis with a significant decline in screening prevalence between 2001 and 2005. The gap between the highest and lowest up-to-date screening prevalence using any screening modality, exhibited by Japanese and Korean Americans, increased from 18% in 2001 to 30% in 2005.
Conclusions
Findings suggest that we need to intensify efforts to increase colorectal cancer screening, especially among Korean Americans but also among Filipinos, Vietnamese and Latinos.
Keywords: colorectal cancer screening, ethnic disparities, Asian subgroups, California Health Interview Survey
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States (1). According to the U.S. Preventive Services Task Force, routine screening of all men and women aged 50 years or older could reduce CRC deaths by 15% to 59% (2, 3). CRC screening is unique in that two different types of screening tests are recommended: fecal occult blood test (FOBT), a take-home test in which the patient applies small amounts of stool onto a card and returns the card to the provider for analysis, or endoscopic exams (colonoscopy and sigmoidoscopy), which are invasive, time-consuming procedures that must be performed by a health professional. Colonoscopy is becoming the test of choice in the general population and in minority groups (4,5), although primary screening through FOBT would be much cheaper on a population basis (6).
Despite the effectiveness of screening in decreasing both prevalence and incidence of CRC (by removing precancerous polyps), screening utilization is low. In 2005, only 56% of the population in California had received CRC screening according to the guidelines (7). Disparities in CRC screening prevalence exist, with nonwhite persons less likely to be screened than whites, both nationwide (4, 8, 9) and in California (5, 10).
Given the low prevalence and disparities in CRC screening, it is important to monitor trends in screening utilization to determine whether prevalence and disparities are increasing or decreasing over time. However, few studies have examined trends in CRC screening by ethnic group (11,12,13). To address this need, we compare trends in CRC screening from 2001 to 2005 by ethnic group using data from the California Health Interview Survey (CHIS). California data are especially suitable for such comparisons because of the state’s ethnically diverse population (43% White, 36% Latino, 6% African American, 12% Asian American and Pacific Islander (14). Our analyses estimate and compare trends for Whites, Latinos, African Americans and Asians, with Asians further disaggregated into subgroups.
In addition to receipt of any CRC screening, our analyses distinguish type of screening test received, i.e., endoscopy versus FOBT. These tests require very different resources (gastroenterologist or trained health professional versus a simple lab test). Thus it is important to examine trends separately for these screening modalities to estimate future demands on the health care system.
Methods
The CHIS, a telephone survey conducted biennially since 2001, is one of the largest health surveys in the United States (15). Each biennial survey includes over 40,000 households and is designed to provide population-based statewide estimates of health indicators for all major ethnic groups as well as several Asian ethnic groups. The CHIS employs a multi-stage sampling design in which households within geographic strata are selected through random-digit dialing (RDD). Supplements are used to achieve target sample sizes of certain ethnic groups, including Vietnamese and Korean respondents. Each biennial sample is cross-sectional; respondents are not followed longitudinally. Interviews are conducted in English, Spanish, Cantonese, Mandarin, Korean and Vietnamese. The overall response rates for adults were 37.7%, 33.5% and 26.9% in 2001, 2003 and 2005, respectively; however, response rates for older adults were substantially higher (16, 17, 18) The response rates are comparable to other RDD surveys (19). The demographic similarity between the CHIS sample and U.S. Census data for California and comparability of health indicator estimates derived from the CHIS and from other data sources suggest that the CHIS samples are representative and provide reliable statewide estimates (20).
We merged data from the 2001, 2003, and 2005 surveys and created an analysis dataset consisting of adults 50 years of age and older with no history of CRC. We defined ever screened by FOBT as an affirmative response to “Have you ever had a blood stool test using a home test kit?” Respondents who responded affirmatively were also asked how long ago was their test: ≤1, >1 to 2, >2 to 3, >3 to 5, or >5 years ago. We defined up-to-date with FOBT as FOBT ≤1 year ago. We defined ever screened by endoscopy as an affirmative response to “Have you ever had a sigmoidoscopy or colonoscopy?” In 2001 and 2003, this question also included proctoscopy. In 2005 only, respondents were asked whether the exam was a sigmoidoscopy or colonoscopy. Respondents with a past exam were asked how long ago was their most recent exam: ≤1, >1 to 2, >2 to 3, >3 to 5, >5 to 10, or >10 years ago. Due to the inability to identify type of exam and time frame consistently across all surveys, we defined up-to-date with endoscopy as any endoscopic exam during the past 5 years. Up-to-date by endoscopy or FOBT was defined as FOBT ≤1 year ago and/or any endoscopic procedure during the past 5 years. Since the reason for FOBT/endoscopy was asked in 2001 and 2003 but not 2005, we estimated prevalence of CRC screening for any reason to maintain consistency across surveys.
We estimated screening prevalence by year (2001, 2003 and 2005) and modality (endoscopy, FOBT, either) for the California population as a whole, major ethnic groups (White, Black, Latino, Asian), and Asian subgroups with sufficient sample size (Chinese, Filipino, Japanese, Korean, Vietnamese). Prevalences were estimated using the CHIS-provided replicate weights and the survey proportion command in Intercooled Stata 9.1 (21). We estimated both crude prevalences and adjusted prevalences that standardized the prevalences in each ethnic group in each year to the age and gender distribution of the 2001 California population. We tested for differences in prevalence between 2001 and 2005 within each ethnic group, and among groups in each year, using Wald tests of hypotheses of equal proportions. These tests followed guidelines for hypothesis tests using multiple CHIS surveys (19).
Results
The numbers of respondents included in the analyses are provided at the bottom of Table 1. Table 1 and Table 2 display standardized prevalences of ever and up-to-date CRC screening, respectively, by year for each ethnic group. Crude prevalences were generally similar to the standardized prevalences; the largest differences were for the Latino and Vietnamese populations, which tended to have prevalences adjusted upward 1–3% due to the standardization (data not shown).
Table 1.
Estimated age-and gender-standardized proportions of California residents ages 50 years and older who have ever received CRC screening *
| Ever screened by endoscopy or FOBT | |||||
|---|---|---|---|---|---|
| Ethnic Group | 2001 | 2003 | 2005 | Change, 2001 to 2005 | P, difference between 2001 and 2005 |
| All | 69% | 70% | 73% | 4% | <.001 |
| White (W) | 74% | 75% | 78% | 4% | <.001 |
| Black (B) | 71% | 70% | 76% | 5% | .06 |
| Asian (A) | 58% | 59% | 62% | 4% | .07 |
| Latino (L) | 49% | 55% | 60% | 11% | <.001 |
| P, comparisons among groups | P<.001: WA, WL, BA, BL, AL | P<.001: WA, WL, BA, BL P<.001: WB |
P<.001: WA, WL, BA, BL | ||
| Asian subgroups | |||||
| Japanese (J) | 71% | 72% | 77% | 6% | .29 |
| Chinese (C) | 59% | 64% | 64% | 5% | .20 |
| Filipino (F) | 56% | 54% | 66% | 10% | .07 |
| Vietnamese (V) | 53% | 63% | 60% | 7% | .18 |
| Korean (K) | 49% | 43% | 33% | −16% | .002 |
| P, comparisons among groups | P<.001: JV, JK P<.01: JF P<.05: JC, CK |
P<.001: JK, CK P<.01: JF, VK |
P<.001: JK, CK, FK, VK P<.01: JC, JV P<.05: JF |
||
| Ever screened by endoscopy | |||||
| 2001 | 2003 | 2005 | Change, 2001 to 2005 | P, difference between 2001 and 2005 | |
| All | 52% | 53% | 60% | 8% | <.001 |
| White (W) | 56% | 58% | 65% | 9% | <.001 |
| Black (B) | 55% | 55% | 59% | 4% | .19 |
| Asian (A) | 42% | 44% | 52% | 10% | <.001 |
| Latino (L) | 37% | 38% | 47% | 10% | <.001 |
| P, comparisons among groups | P<.001: WA, WL, BA, BL | P<.001: WA, WL, BA, BL P<.01: AL |
P<.001: WA, WL, BL P<.05: WB, BA |
||
| Asian subgroups | |||||
| Japanese (J) | 57% | 55% | 67% | 10% | .09 |
| Chinese (C) | 43% | 47% | 55% | 12% | .003 |
| Filipino(F) | 35% | 41% | 50% | 15% | .01 |
| Vietnamese (V) | 36% | 46% | 50% | 14% | .02 |
| Korean (K) | 37% | 33% | 30% | −7% | .18 |
| P, comparisons among groups | P<.001: JF, JV, JK P<.01: JC |
P<.001: JK P<.01: JF, CK |
P<.001: JK, CK P<.01: JF, FK, VK P<.05: JC, JV |
||
| Ever screened by FOBT | |||||
| 2001 | 2003 | 2005 | Change, 2001 to 2005 | P, difference between 2001 and 2005 | |
| All | 50% | 51% | 50% | 0% | .29 |
| White (W) | 57% | 56% | 55% | −2% | .01 |
| Black (B) | 53% | 50% | 56% | 3% | .29 |
| Asian (A) | 38% | 38% | 36% | −2% | .22 |
| Latino (L) | 27% | 37% | 35% | 8% | <.001 |
| P, comparisons among groups | P<.001: WA, WL, BA, BL, AL P<.05: WB |
P<.001: WA, WL, BA, BL P<.01: WB |
P<.001: WA, WL, BA, BL | ||
| Asian subgroups | |||||
| Japanese (J) | 51% | 52% | 48% | −3% | .63 |
| Chinese (C) | 40% | 38% | 36% | −4% | .26 |
| Filipino(F) | 38% | 35% | 44% | 6% | .28 |
| Vietnamese (V) | 29% | 44% | 29% | 0% | .97 |
| Korean (K) | 24% | 21% | 4% | −20% | <.001 |
| P, comparison among groups | P<.001: JV, JK P<.01: CK, FK P<.05: JF, CV |
P<.001: JK, CK, VK P<.05: JC, JF, FK |
P<.001: JK, CK, FK, VK P<.01: JV P<.05: JC, FV |
||
| Sample sizes | |||||
| 2001 | 2003 | 2005 | |||
| All | 23866 | 19111 | 21692 | ||
| White | 18355 | 14236 | 16912 | ||
| Black | 1094 | 1174 | 913 | ||
| Asian (all) | 1572 | 1418 | 1586 | ||
| Latino | 1881 | 1574 | 1537 | ||
| Asian subgroups † | |||||
| Japanese | 214 | 195 | 210 | ||
| Chinese | 388 | 503 | 541 | ||
| Filipino | 276 | 248 | 229 | ||
| Vietnamese | 310 | 175 | 224 | ||
| Korean | 250 | 177 | 248 | ||
Analyses were conducted using California Health Interview Survey data with survey replicate weights and survey data procedures for proportion estimation. P values are from Wald tests of hypotheses of equality of two proportions.
Sample sizes for Asian subgroups do not sum to the Asian total because the Asian category includes smaller Asian subgroups not listed separately.
Table 2.
Estimated age- and gender-standardized proportions of California residents ages 50 years and older who have received up-to-date CRC screening*
| Up-to-date screening, by endoscopy or FOBT | |||||
|---|---|---|---|---|---|
| Ethnic Group | 2001 | 2003 | 2005 | Change, 2001 to 2005 | P, difference between 2001 and 2005 |
| All | 53% | 52% | 56% | 3% | <.001 |
| White (W) | 56% | 55% | 59% | 3% | <.001 |
| Black (B) | 56% | 55% | 57% | 1% | .84 |
| Asian (A) | 46% | 45% | 49% | 3% | .12 |
| Latino (L) | 40% | 41% | 47% | 7% | .003 |
| P, comparisons among groups | P<.001: WA, WL, BA, BL P<.01: AL |
P<.001: WA, WL, BA, BL | P<.001: WA, WL, BL. P<.01: BA |
||
| Asian subgroups | |||||
| Japanese (J) | 57% | 55% | 59% | 2% | .78 |
| Chinese (C) | 47% | 51% | 53% | 6% | .18 |
| Filipino (F) | 43% | 38% | 46% | 3% | .56 |
| Vietnamese (V) | 42% | 53% | 49% | 7% | .22 |
| Korean (K) | 39% | 34% | 29% | −10% | .04 |
| P, comparisons among groups | P<.01: JV, JK P<.05: JF |
P<.001: JK, CK P<.01: JF, VK P<.05: CF, FV |
P<.001: JK, CK, FK, VK P<.05: JF |
||
| Up-to-date screening with endoscopy | |||||
| 2001 | 2003 | 2005 | Change, 2001 to 2005 | P, difference between 2001 and 2005 | |
| All | 43% | 44% | 48% | 5% | <.001 |
| White (W) | 45% | 47% | 52% | 7% | <.001 |
| Black (B) | 48% | 45% | 50% | 2% | .35 |
| Asian (A) | 36% | 38% | 42% | 6% | .005 |
| Latino (L) | 33% | 31% | 39% | 6% | .005 |
| P, comparisons among groups | P<.001: WA, WL, BA, BL | P<.001: WA, WL, BL P<.01: BA, AL |
P<.001: WA, WL, BL P<.01: BA |
||
| Asian subgroups | |||||
| Japanese (J) | 49% | 49% | 53% | 4% | .50 |
| Chinese (C) | 38% | 42% | 46% | 8% | .05 |
| Filipino (F) | 31% | 32% | 37% | 6% | .24 |
| Vietnamese (V) | 32% | 42% | 43% | 10% | .08 |
| Korean (K) | 30% | 31% | 28% | −2% | .64 |
| P, comparisons among groups | P<.01: JF, JV, JK P<.05: JC |
P<.01: JF, JK P<.05: CK |
P<.001: JK, CK P<.01: JF, VK |
||
| Up-to-date screening with FOBT | |||||
| 2001 | 2003 | 2005 | Change, 2001 to 2005 | P, difference between 2001 and 2005 | |
| All | 23% | 19% | 20% | −3% | <.001 |
| White (W) | 25% | 20% | 21% | −5% | <.001 |
| Black (B) | 24% | 22% | 20% | −4% | .08 |
| Asian (A) | 19% | 15% | 16% | −3% | .23 |
| Latino (L) | 14% | 17% | 17% | 3% | .07 |
| P, comparisons among groups | P<.001: WA, WL, BL P<.01: BA, AL |
P<.001: WA, BA P<.01: WL, BL |
P<.01: WA P<.05: WL |
||
| Asian subgroups | |||||
| Japanese (J) | 25% | 19% | 19% | −6% | .24 |
| Chinese (C) | 18% | 17% | 18% | 0% | .96 |
| Filipino(F) | 18% | 11% | 19% | 1% | .77 |
| Vietnamese (V) | 16% | 17% | 10% | −6% | .10 |
| Korean (K) | 14% | 7% | 2% | −12% | <.001 |
| P, comparisons among groups | P<.05: JV, JK | P<.01: JK, CK P<.05: VK |
P<.001: JK, CK, FK P<.01: VK P<.05: CV, FV |
||
Analyses were conducted using California Health Interview Survey data with survey replicate weights and survey data procedures for proportion estimation. P values are from Wald tests of hypotheses of equality of two proportions. Sample sizes are provided in Table 1.
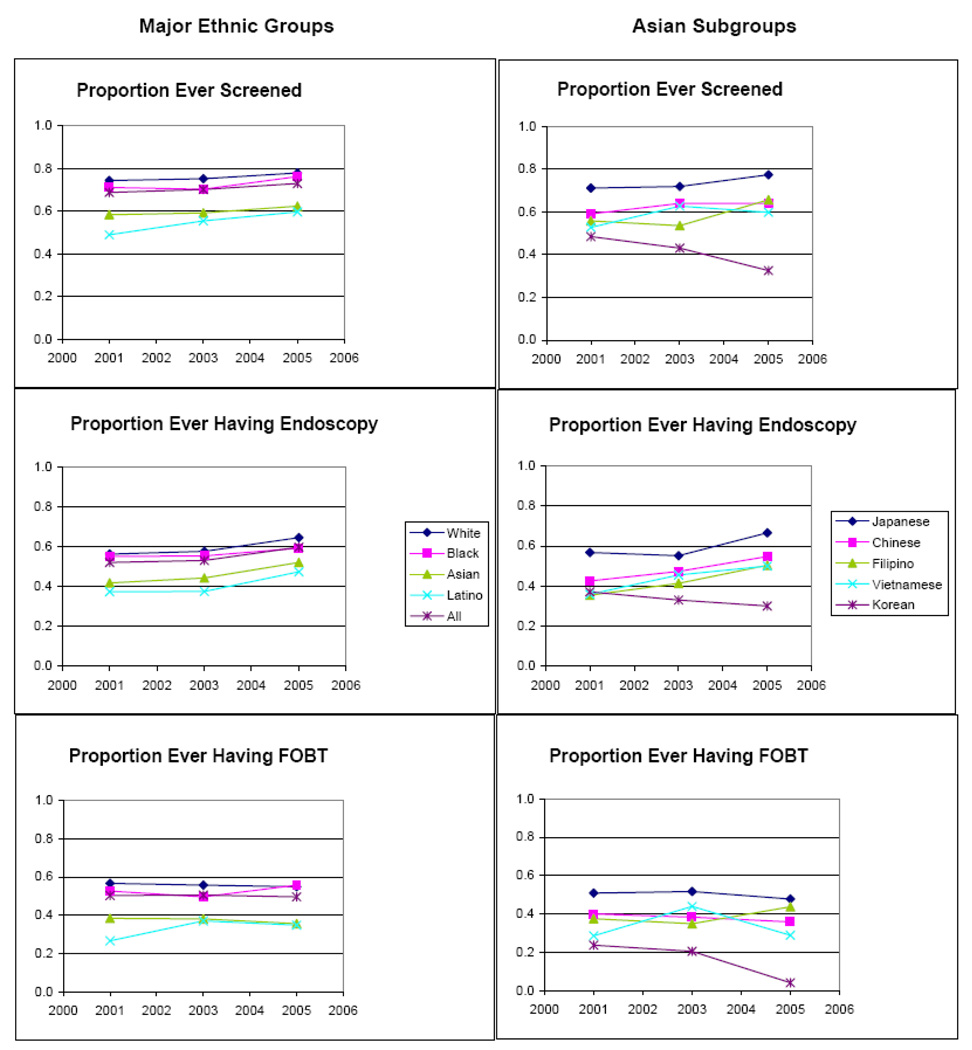
Table 1 provides prevalences of ever receiving CRC screening. These trends are also illustrated in Figure 1. Prevalences of ever screened by FOBT or endoscopy were higher among Whites and Blacks than among Latinos and Asians (all Asian ethnicities combined) over all three surveys. Among major ethnic groups, the greatest disparity in 2001 was a difference of 25% [95% CI: (22%, 29%)] between Latinos and Whites. Prevalences increased significantly from 2001 to 2005 in the state population overall and among Whites and Latinos. However, despite an 11% increase among Latinos, their rate was among the lowest for the major ethnic groups in 2005 and fell short of Whites by 18% [95% CI: (15%, 22%)]. Results for the Asian subgroups show even larger differences. Over all surveys, the Japanese had the highest prevalence while Koreans had the lowest prevalence (all p<.001). The difference in prevalence between these two groups increased from 22% [95% CI: (11%, 34%)] in 2001 to 44% [95% CI: (34%, 55%)] in 2005, attributable largely by a 16% decrease among Koreans from 2001 to 2005.
Figure 1.
Estimated age- and gender-standardized proportions of California residents aged 50 or older who have ever received CRC screening
Between 2001 and 2005, prevalence of ever screened by endoscopy significantly increased in the state population overall and among Whites, Latinos, and Asians, as well as among Chinese, Filipino and Vietnamese. There was no significant increase among Blacks, Japanese or Koreans. Over all surveys, the highest prevalence of endoscopy was observed among Whites, followed by Blacks, Asians and Latinos. Prevalence of endoscopy was significantly higher among Japanese Americans than among Korean and Filipino Americans in all three surveys.
Among major ethnic groups, Latinos had the lowest prevalence of ever screened by FOBT in 2001. This group had a significant increase of 8% over the four-year period, and differences among these groups decreased from 2001 to 2005, with the largest difference in 2001, a difference of 30% [95% CI: (27%, 33%)] between Whites and Latinos, decreasing to 20% in 2005 [95% CI: (17%, 23%)]. This decreasing gap reflected a significant decrease among Whites combined with a significant increase among Latinos. Among the Asian subgroups, the Japanese had the highest prevalence while Koreans had the lowest across all surveys. The difference in prevalence between these two groups increased from 27% [95% CI: (15%, 38%)] in 2001 to 44% [95% CI: (35%, 52%)] in 2005, due largely to a 20% drop in prevalence of FOBT receipt among Koreans from 2001 to 2005.
Trends were similar for up-to-date screening (Table 2). Prevalence of up-to-date screening by FOBT or endoscopy increased in the population overall and among Whites and Latinos, and decreased among Korean Americans, who had low prevalence in all years and a 10% drop from 2001 to 2005. The gap between the highest and lowest up-to-date screening prevalence using any screening modality, exhibited by Japanese and Korean Americans, increased from 18% in 2001 to 30% in 2005. Prevalence of up-to-date endoscopy increased in most groups from 2001 to 2005, and prevalence of up-to-date FOBT showed declines or no increase. In 2005, lowest prevalences of being up-to-date with endoscopy were among Korean and Filipino Americans.
Discussion
Our analysis indicates that the overall proportion of people who had ever been screened for CRC increased from 2001 to 2005 in California, with increases ranging from 4% among Whites to 11% among Latinos. Although disparities in screening prevalence among the four major racial/ethnic groups decreased during this time period, the basic pattern remained, with Whites and African Americans having higher prevalence than Asian Americans and Latinos. Increases in CRC screening have also been observed in other analyses (12, 22, 23). Only one of these analyses provides CRC screening prevalence for the four major racial/ethnic groups and their findings are very similar to ours (23). Our findings are also consistent with the general trend of increasing utilization of colonoscopies and declining utilization of FOBT (11, 13, 23, 24); however, our analyses indicate that Latinos had increased FOBT utilization.
Our analysis shows that combining Asian American groups masks disparities that exist between groups. Japanese Americans, many of whom have lived in the United States for several generations, had the highest screening prevalence of all Asian Americans and the highest prevalence of endoscopy. Their screening prevalence was very similar to that of Whites, who generally had the highest prevalence. Korean Americans, on the other hand, had the lowest screening prevalence for endoscopy, FOBT and the two combined, and were the only group in this analysis that had a significant decline in CRC screening. Korean Americans are among the more recent immigrant groups; 76% are foreign born and about 34% have no health insurance (25). These factors may explain their low CRC screening utilization (26, 27). During the same time period, prevalence of endoscopy significantly increased among Chinese, Filipino and Vietnamese Americans, while their prevalences of FOBT receipt were not significantly changed. Thus, as among Whites, Blacks and Latinos, increases in screening among Asian Americans were generally due to increased utilization of endoscopy. A recent analysis of CRC screening in Filipinos suggests that within ethnic subgroup, more educated and acculturated persons with higher income may tend to obtain endoscopies while more recent immigrants with lower levels of education and income tend to obtain FOBTs (28).
Strengths and Limitations
Our analysis used a population–based, ethnically diverse sample that included non-English-speaking-Asian Americans, who are often excluded from national surveys. However, Japanese and Filipino Americans were only interviewed in English due to limited resources and the fact that more than 70% speak English very well (29). Overall, our results represent screening trends in California, but may not represent trends in other states. All data are based on self-report and may therefore be subject to social desirability and recall bias. Because of data limitations, some respondents who had had a colonoscopy 5–10 years ago may have been incorrectly classified as not up-to-date, resulting in an underestimate. Because the reason for last CRC test was not ascertained for all three surveys, our analysis included tests obtained for any reason, not routine screening exclusively. This may have overestimated routine screening prevalences.
Conclusion
Our results show that disparities in CRC screening among racial/ethnic groups in California are persisting and in some cases increasing rather than decreasing. Screening trends varied substantially among Asian subgroups, with Korean, Filipino and Vietnamese Americans having the lowest prevalence of up-to-date screening. Korean Americans were unique in being the only group in our analyses with screening prevalence that significantly declined between 2001 and 2005. This demonstrates the importance of disaggregating Asian subgroups. During the same time period, up-to-date CRC screening increased significantly among Whites and Latinos. These trends suggest that we need to intensify efforts to increase CRC screening, especially among Korean Americans but also among Filipino and Vietnamese Americans and Latinos. Research suggests that screening programs that are culturally sensitive and that address beliefs and barriers pertaining to CRC screening in these communities will be most effective. In conjunction with these efforts, we also need to establish programs that provide free or low-cost diagnostic follow-up and treatment for patients who have positive screening results and no health insurance coverage.
Acknowledgments
Financial support: This work was supported by Grant GHN04K from the California Program on Access to Care (CPAC), California Policy Research Center, University of California Office of the President. The views and opinions expressed do not necessarily represent those of The Regents of the University of California, CPAC, its advisory board, or any State or County executive agency represented thereon. AEM was also support by U01CA114640 and CMC by NIH/NCI grant P30 CA 16042.
References
- 1.American Cancer Society. Cancer Facts & Figures 2007. Atlanta (GA): American Cancer Society; 2007. [Google Scholar]
- 2.U.S. Preventive Services Task Force (USPSTF) [[cited 2008 Jun 10]];Rockville (MD): Agency for Healthcare Research Quality; Screening for colorectal cancer. 2002 Available from: http://www.ahrq.gov/clinic/uspstf/uspscolo.htm.
- 3.Selby JV, Friedman GD, Quesenberry CP, Jr, Weiss NS. A case control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326:653–657. doi: 10.1056/NEJM199203053261001. [DOI] [PubMed] [Google Scholar]
- 4.Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15:389–394. doi: 10.1158/1055-9965.EPI-05-0678. [DOI] [PubMed] [Google Scholar]
- 5.Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and Non-Latino whites. Cancer. 2005;104 Supp 12:S2940–S2947. doi: 10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher JA, Fikry C, Troxel AB. Cutting cost and increasing access to colorectal cancer screening: another approach to following the guidelines. Cancer Epidemiol Biomarkers Prev. 2006;15:108–113. doi: 10.1158/1055-9965.EPI-05-0198. [DOI] [PubMed] [Google Scholar]
- 7.California Health Interview Survey. [[cited 2008 Sep 22]];Los Angeles (CA): UCLA Center for Health Policy Research; CHIS 2005 Adult Public Use File, Release 1 [database on the Internet] c2007 Available from http://www.ucla.chis.edu.
- 8.James TM, Greiner KA, Ellerbeck EF, Feng C, Ahluwalia JS. Disparities in colorectal cancer screening: a guideline-based analysis of adherence. Ethn Dis. 2006;16:228–233. [PubMed] [Google Scholar]
- 9.Pollack LA, Blackman DK, Wilson KM, Seeff LC, Nadel MR. Colorectal cancer test use among Hispanic and Non-Hispanic U.S. populations. [[cited 2007 Nov 27]];Prev Chronic Dis [serial on the Internet] 2006 Apr;3(2):A50. Available from http://www.cdc.gov/pcd/issues/2006/apr/05_0120.htm. [PMC free article] [PubMed]
- 10.American Cancer Society, California Division and Public Health Institute, California Cancer Registry. California Cancer Facts and Figures 2007. Oakland (CA): American Cancer Society, California Division; 2006. [Google Scholar]
- 11.Phillips KA, Liang SY, Ladabaum U, et al. Trends in colonoscopy for colorectal cancer screening. Med Care. 2007;45:160–167. doi: 10.1097/01.mlr.0000246612.35245.21. [DOI] [PubMed] [Google Scholar]
- 12.Kang-Kim M, Betancourt JR, Ayanian JZ, Zaslavsky AM, Yucel RM, Weissman JS. Access to care and use of preventive services by Hispanics. State-based variations from 1991 to 2004. Med Care. 2008;46:507–515. doi: 10.1097/MLR.0b013e31816dd966. [DOI] [PubMed] [Google Scholar]
- 13.Robertson RH, Burkhardt JH, Powell MP, Eloubeidi MA, Pisu M, Weissman NW. Trends in colon cancer screening procedures in the US Medicare and Tricare population: 1999 – 2001. Prev Med. 2006;42:460–462. doi: 10.1016/j.ypmed.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Census Bureau. [[cited 2008 Jun 14]];U.S. Census Bureau; State Population Estimates, Characteristics - Race and Hispanic Origin [table on the Internet] 2007 Jul; Available from http://www.census.gov/popest/states/asrh/SC-EST2007-04.html.
- 15.California Health Interview Survey (CHIS) [[cited 2008 Jun 14]];Los Angeles, CA: UCLA Center for Health Policy Research; [homepage on the Internet] 2007 About CHIS; [about 1 screen]. Available from http://www.chis.ucla.edu/about.html.
- 16.California Health Interview Survey. Los Angeles (CA): UCLA Center for Health Policy Research; CHIS 2001 Methodology Series: Report 4 - Response Rates. 2002
- 17.California Health Interview Survey. Los Angeles (CA): UCLA Center for Health Policy Research; CHIS 2003 Methodology Series: Report 4 - Response Rates. 2005
- 18.California Health Interview Survey. Los Angeles (CA): UCLA Center for Health Policy Research; CHIS 2005 Methodology Series: Report 4 - Response Rates. 2007
- 19.California Health Interview Survey. Los Angeles (CA): UCLA Center for Health Policy Research; CHIS Methodology Paper: Examining Trends and Averages Using Combined Cross-Sectional Survey Data from Multiple Years. 2007
- 20.California Health Interview Survey. Los Angeles (CA): UCLA Center for Health Policy Research; Technical Report No. 1: The CHIS 2001 Sample: Response Rate and Representativeness. 2003
- 21.StataCorp. Statistical Software: Release 9.1. College Station (TX): Stata Corporation; 2005. [Google Scholar]
- 22.Kim JA, Porterfield D, Gizlice Z. Trends in up-to-date status in colorectal cancer screening, North Carolina, 1998–2002. N C Med J. 2005;66:420–426. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Colorectal Cancer Test Use - Maryland, 2002–2006. MMWR Morb Mortal Wkly Rep. 2007;56:932–936. [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Use of Colorectal Cancer Tests – United States, 2002, 2004, and 2006. MMWR Morb Mortal Wkly Rep. 2008;57:253–258. [PubMed] [Google Scholar]
- 25.Brown ER, Ojeda VD, Wyn R, Levan R. Racial and ethnic disparities in access to health insurance and health care. Los Angeles (CA): UCLA Center for Health Policy Research and Kaiser Family Foundation; 2000. Apr, Sponsored by the Kaiser Family Foundation. [Google Scholar]
- 26.Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites: Cultural influences or access to care? Cancer. 2006;107:184–192. doi: 10.1002/cncr.21968. [DOI] [PubMed] [Google Scholar]
- 27.Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean Immigrants in the United States. Am J Prev Med. 2000;18:62–68. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- 28.Maxwell AE, Danao L, Crespi CM, Antonio C, Garcia GM, Bastani R. Disparities in receipt of FOBT versus endoscopy among Filipino American immigrants. Cancer Epidemiol Biomarkers Prev. 2008;7:1963–1967. doi: 10.1158/1055-9965.EPI-07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.S. Census Bureau. U.S. Department of Commerce: American Community Survey Reports. The American Community - Asians: 2004. 2007 Feb;