Abstract
Objectives
We sought to identify interest in different modes of self-management support among diabetes patients cared for in public hospitals, and to assess whether demographic or disease-specific factors were associated with patient preferences. We explored the possible role of a perceived communication need in influencing interest in self-management support.
Methods
Telephone survey of a random sample of 796 English and Spanish-speaking diabetes patients (esponse rate 47%) recruited from 4 urban US public hospital systems. In multivariate models, we measured the association of race/ ethnicity, primary language, self-reported health literacy, self-efficacy, and diabetes-related factors on patients’ interest in three self-management support strategies (telephone support, group medical visits, and internet -based support). We explored the extent to which patients believed that better communication with providers would improve their diabetes control, and whether this perception altered the relationship between patient factors and self-management support acceptance.
Results
Sixty-nine percent of respondents reported interest in telephone support, 55% in group medical visits, and 42% in internet. Compared to Non-Hispanic Whites, Spanish-speaking Hispanics were more interested in telephone support (OR 3.45, 95%CI 1.97–6.05) and group medical visits (OR 2.45, 95%CI 1.49–4.02), but less interested in internet self-management support (OR 0.56, 95%CI 0.33–0.93). African-Americans were more interested than Whites in all 3 self-management support strategies. Patients with limited self-reported health literacy were more likely to be interested in telephone support than those not reporting literacy deficits. Forty percent reported that their diabetes would be better controlled if they communicated better with their health care provider. This perceived communication benefit was independently associated with interest in self-management support (p<0.001), but its inclusion in models did not alter the strengths of the main associations between patient characteristics and self-management support preferences.
Conclusion
Many diabetes patients in safety-net settings report an interest in receiving self-management support, but preferences for modes of delivery of self-management support vary by race/ethnicity, language proficiency, and self-reported health literacy.
Practice Implications
Public health systems should consider offering a range of self-management support services to meet the needs of their diverse patient populations. More broad dissemination and implementation of self-management support may help address the unmet need for better provider communication among diabetes patients in these settings.
Keywords: diabetes, communication, health literacy, telephone care, group medical visits, racial/ethnic minority, self-management, disparities
1. Introduction
Self-management is the cornerstone of diabetes care, and patients with diabetes must perform multiple self-management activities on a regular basis to help prevent adverse outcomes(1–3). Unfortunately, diabetes-specific disease management support occurs inconsistently during outpatient visits, and information that patients receive is often poorly understood or does not take into account their values and life circumstances (4, 5). Because effective diabetes self-management support requires a complex series of assessments and instructions, patients often require additional support and communication outside of the traditional clinician visit (6).
Common approaches to providing this additional self-management support include telephone-based counseling (7–12), group medical visits(13–21), and, increasingly, computer or internet-based programs (22–30). Efficacy studies of self-management support have shown improvements in patient satisfaction, healthy behaviors, self-efficacy, and, in some cases, utilization and clinical outcomes(31–33). However, implementation of self-management support services varies widely(34, 35), and these interventions often do not reach the populations that need these services the most (4, 36–40). The gap between evidence and practice may be particularly important in safety net settings, such as public hospital systems, that care for a disproportionate share of ethnically diverse and socio-economically vulnerable patients(41, 42), often with very limited resources. Racial/ ethnic minorities and those with limited English proficiency often experience especially poor communication in clinical settings (43–50). These communication disparities are thought to contribute, in turn, to health disparities(51, 52).
The standard practice for targeting self-management support either relies on physician referral, patient self-selection or on clinical factors such as clinical status (e.g., chronically elevated blood glucose level, health care utilization) or psychosocial factors such as self-efficacy. It is unclear whether these methods identify patients who most desire self-management support, and whether self-management support reaches the patients with the greatest potential to benefit. As health systems implement self-management support programs, there is a pressing need to identify which patients are most likely to accept these services and to understand patients’ preferences for various self-management support modalities.
Little is known about the extent to which vulnerable patients are willing to participate in various strategies that may improve their self-management. Also, the extent to which desire for self-management support is associated with patients’ perceptions about communication with their providers remains unclear. Using a large sample of diabetes patients recruited from 4 urban U.S. public hospital systems, we examined: (a) the extent of patients’ acceptance of three diabetes self-management support strategies: telephone care, group medical visits, and internet or computer-based programs and (b) whether limited English proficiency, racial/ethnic minority status, or diabetes-specific clinical factors were associated with preferences for each type of self-management support. Finally, we explored the possible role of an unmet communication need in influencing interest in self-management support.
2. Methods
2.1. Setting and participants
The National Public Health and Hospital Institute (NPHHI) administered this study as part of a larger diabetes care initiative, the Consortium for Quality Improvement in Safety Net Hospitals. The study design has been previously described (42). Seven public hospital and health systems participated: Cambridge Health Alliance, Cambridge, Massachusetts; Community Health Network of San Francisco, San Francisco, California; Cook County Bureau of Health Services, Chicago, Illinois; LSU/ Medical Center of Louisiana, New Orleans, Louisiana; Harborview Medical Center, Seattle, Washington; Memorial Health Care System, New York; Grady Health System, Atlanta, Georgia. The telephone questionnaire that provided data for this study was administered between December 2003 and January 2004 to patients in 4 of the participating health systems: Cook County Bureau of Health Services, Cambridge Health Alliance, Louisiana State University Medical Center, and Community Health Network of San Francisco.
Potential participants were first identified by querying each health system’s electronic administrative databases. These databases include information about all patients treated within each system of care. We used a standard algorithm to identify patients with a primary or secondary diabetes-related ICD-9 diagnosis code (ICD 250.xx) associated with either an outpatient or inpatient visit between January 1, 2000 to December 31, 2002. Patients eligible for the telephone questionnaire had to be 18 years or older, and have 2 or more outpatient visits during the study period. Patients with only gestational diabetes (ICD 648.0x) and abnormal glucose tolerance (ICD 648.8) were excluded. 1706 potential subjects were randomly selected for the telephone questionnaire and, apart from telephone numbers, all other patient-level data were de-identified. We used stratified random sampling to obtain equal numbers of White, African-American, and Hispanic respondents, with a goal of approximately 200 subjects from each site. The survey was conducted in English and Spanish. Using standard procedures, the questionnaire was translated into Spanish and back-translated into English until concordance in meaning was achieved. Subjects who self-identified as Asian/Pacific Islanders and Native Americans, or speaking a language other than English or Spanish, were excluded from the telephone survey due to insufficient population sizes across the four sites.
We confirmed the diagnosis of diabetes during the telephone survey. After obtaining verbal informed consent from each participant, trained interviewers from the opinion research firm Multicultural Connections conducted the interviews. The protocol was approved by the human subjects committees at all participating hospitals and institutions.
2.2. Measures
2.2.1. Outcomes
Interest in self-management support strategies
In order to gauge respondents’ interest in various self-management support strategies, we asked: (a) “Would you be interested in receiving phone calls at home on a regular basis from your doctor, nurse practitioner, or other health providers to check in with you about your diabetes and your health?”; (b) “Would you be interested in receiving some of your health care with other patients who have diabetes? In other words, having your doctor, nurse practitioner, or other health providers work with you in a group that has other diabetes patients?”; (c) “If you had access to a computer and/or internet, would you be interested in using the computer or internet to regularly check in with your doctor, nurse practitioner, or other health providers about your diabetes and your health?” For all three items, responses of “yes” and “maybe” were collapsed and compared to “no.” In addition, we created a measure of overall self-management support interest, as an additive scale ranging from 0–3, such that interest in each mode was given 1 point.
2.2.2 Sociodemographic factors
Respondents reported their race, ethnicity, language preference, insurance status and educational attainment. To assess English language proficiency, we asked patients whether they spoke English only, English better than any other language, English and another language equally well, or another language better than English. We considered those patients who reported speaking another language better than English to have limited English proficiency (53).
2.2.3. Self-reported Health Literacy
To estimate health literacy, interviewers asked participants how often they have problems learning about their medical condition because of difficulty understanding written information. Responses were recorded on a Likert scale from “no problems” to “often have problems”. This item has been previously validated against in-person health literacy measurement (54, 55) among English speakers (56). Using a separate sample of ethnically diverse public hospital patients with diabetes for whom we had in-person health literacy scores, we re-validated the health literacy item among English and Spanish speakers and found similar test characteristics (Area Under Receiver Operating Curve 0.74, p=0.03). The categories were collapsed such that patients who reported “any” or more frequent problems learning about their health care because of difficulty understanding written materials were considered to have limited self-reported health literacy.
2.2.4. Diabetes-specific factors
Patients reported the duration of their diabetes and their use of oral medications and/or insulin. We used questions from the FACCT Diabetes Care Survey to assess use of diabetes education services, including diabetes classes, one-on-one diabetes education, and receipt of educational materials, over the prior 2 years (57).Because of its association with self-management behaviors (58), we assessed diabetes self-efficacy using a validated scale that asks patients to rate their difficulty in managing their diabetes over the prior six months (59). The scale scores range from 0–15, with higher scores indicating better self-efficacy. Perceived diabetes control was measured with the question, “How well do you feel your diabetes has been controlled in the past six months?” Health status was measured with a single item, with response options ranging from poor to excellent.
2.2.5. Perceived benefit of improved communication
In order to measure participants’ perceptions of the benefit of improved communication with clinicians for their diabetes control, we asked subjects “If you were able to communicate better with your doctor, nurse practitioner, or other health providers – so you would understand each other better- how much better do you think you’d be able to control your diabetes?” The response options were: “no change,” “better,” or “much better.” Those who reported that their diabetes control would be “better” or “much better” were considered to have perceived communication benefit. This is a novel question which was designed to avoid the ceiling effect commonly observed in assessments measuring patients’ satisfaction with their patient-provider communication(46). Using the measure, we sought to explore whether patient’s perceived need for better communication might influence their desire for and acceptability of different approaches to providing self-management support above and beyond socio-demographic and other diabetes-specific domains described above.
2.3 Analysis
We constructed demographic categories incorporating both race and language, identifying patients who were non-Hispanic White, Non-Hispanic Black, English-speaking Hispanic, and Spanish speaking Hispanic. This permitted direct comparison between English and Spanish-speaking Hispanic patients, in order to separate a language effect from a culture effect (60). In our analysis, we present below summary results including the number of patients expressing interest in each mode of self-management support. For each strategy, we used multivariate logistic regression to explore associations with demographic and clinical characteristics, self-reported health literacy, diabetes self-efficacy, and language proficiency. The rationale for this analysis was to assess whether certain subgroups clearly expressed a preference for one particular self-management support strategy, because that would have implications for improving diabetes management in safety-net settings. The same set of potential predictors was retained in multivariate models regardless of their associated p-values so that effects could be compared across models.
In addition, to better understand the construct of perceived communication benefit, we first present its frequency in this sample. We used t-test and Chi-squared test for continuous and categorical comparisons respectively. We then performed an exploratory analysis to examine its possible associations with patients’ overall self-management acceptance, a score ranging from 0 (no interest in any self-management-support mode) up to 3 (corresponding to interest in all 3 modes). We used ordered logistic regression, with adjustment for demographic and clinical characteristics, diabetes self-efficacy, self-reported health literacy, and primary language, using the same set of covariates as in the models for self-management support preferences. We hypothesized that perceived communication benefit would be associated with self-management support acceptance even when adjusting for patient characteristics as above.
Finally, we performed an additional set of exploratory analyses that included perceived communication benefit as a potential covariate in the multivariate models of self-management support acceptance. To determine whether perceived communication benefit contributed to the understanding of self-management support acceptance, we also performed a likelihood ratio test comparing the fit of the multivariate models with and without adjustment for perceived communication benefit.
To account for the clustering of patients within health system, we included study site as a fixed effect in all models(61). For each model, the following interactions were tested based on a priori hypotheses: age and race/language category; race/language category and health literacy; educational attainment and race/language category; and educational attainment and health literacy.
3. Results
Across the four sites, 39,576 ambulatory patients with diabetes were identified as eligible for the survey. Of these, 1706 randomly selected patients constituted the pool from which potential participants were contacted. We reached 1693 by telephone, and 796 completed the questionnaire, for a response rate of 47%. Interviewers obtained verbal informed consent in English or Spanish.
One-third of respondents identified themselves as Non-Hispanic White, one third as non-Hispanic Black, and one-third as Hispanic. Overall, patients had low educational attainment, and were predominantly uninsured or publicly insured (Table 1). Three hundred eleven participants (39%) reported problems learning about their health due to difficulty understanding written materials and were categorized as having limited self-reported health literacy. Mean duration of diabetes was 11 years, with 91 individuals (12%) reporting poor or very poor diabetes control. Although we do not have information about non-responders, when compared to the patients in the electronic database from the 4 sites, the survey participants were on average slightly older (mean age 56 versus 54, p<0.001) and included a greater proportion of women (62% versus 54%, p<0.001).
Table 1.
Patient Characteristics
| Characteristics | Total (N = 796) |
|---|---|
| Age, mean (SD) | 58 (12) |
| Female gender | 492 (62) |
| Race/ Ethnicity, number (%) | |
| Black/ Non-Hispanic | 265 (33) |
| Hispanic | 267 (33) |
| White/ Non-Hispanic | 264 (33) |
| Years with diabetes, mean (SD) | 11 (10) |
| Insulin use | 305 (38) |
| Limited health literacy | 311 (39) |
| Diabetes control | |
| Excellent | 114 (15) |
| Well | 341 (43) |
| Fair | 239 (30) |
| Poor | 70 (9) |
| Very Poor | 21 (2) |
| Language, N(%) | |
| Spanish | 188 (23) |
| English | 608 (76) |
| Education level, N(%) | |
| More than high school | 221(27) |
| High school graduate | 229 (29) |
| Less than high school | 346 (43) |
| Type of insurance | |
| No insurance | 249 (31) |
| Public Insurance | 425 (53) |
| Private insurance | 83 (10) |
| Other insurance | 39 (5) |
| Self-efficacy score, mean(SD) | 11.5 (2.9) |
| Seen by diabetes educator N(%) | 321 (40) |
| Received educational materials, N(%) | 373 (47) |
| Attended a diabetes class, N(%) | 229 (29) |
| Fair or poor health status, N(%) | 390 (49) |
| Study site, N(%) | |
| Cambridge, MA | 211 (26) |
| San Francisco, CA | 205 (26) |
| Chicago, IL | 196 (24) |
| New Orleans, LA | 184 (23) |
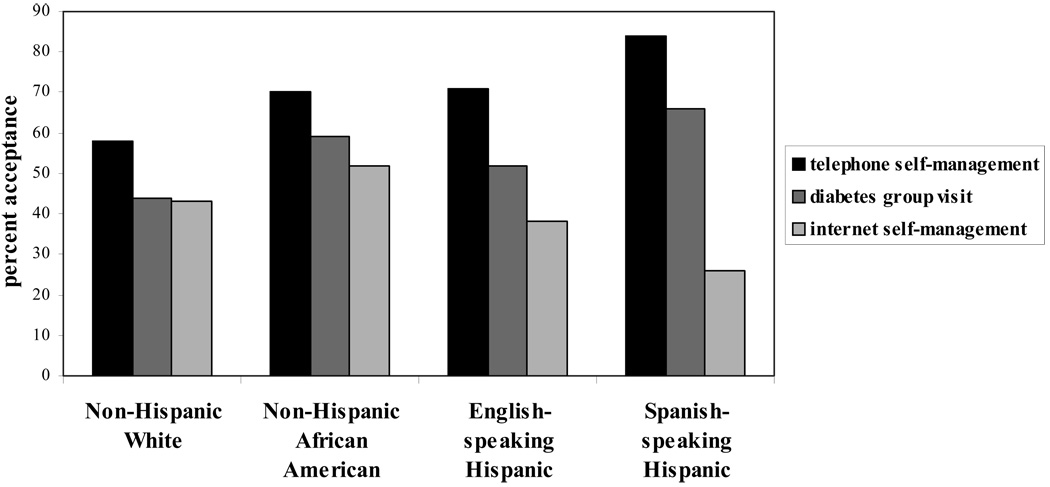
Overall, 551 participants (69%) reported interest in telephone self-management support, 439 participants (55%) in group medical visits, and 332 (42%) in internet-based self-management support. One-hundred forty-three respondents (18%) reported no interest in any of the self-management support modes; 183 (23%) were interested in 1 mode, 271 (34%) in two modes, and 199 (25%) in all 3 modes. Patients’ preferences for the 3 diabetes self-management support strategies varied by racial/ethnic group (Figure 1). While we did not have information about provider-patient language concordance, preferences for self-management support did not differ for the subset of patients who reported needing an interpreter compared to the sample overall (p for all >0.20).
Figure legend.
Telephone was more acceptable than group medical visits (McNemar Χ2, p for all <0.001) and internet (McNemar Χ2, p for all <0.001) for all 4 groups. Internet was significantly less accepted by Hispanics than telephone or group visits (McNemar Χ2, p for all <0.05)
In multivariate models, compared to Non-Hispanic Whites, Spanish-speaking Hispanics were more interested in telephone support (OR 3.45, 95%CI 1.97–6.05) and group medical visits (OR 2.45, 95%CI 1.49–4.02), but less interested in internet self-management(OR 0.56, 95%CI 0.33–0.93). African-Americans were more interested than Whites for all 3 self-management support strategies (Table 2). In addition, older patients reported less interest in all three self-management support strategies. Those with lower educational attainment were more likely to report an interest in telephone and group medical visits but less likely to report an interest in internet-based support. Limited self-reported health literacy was independently associated with greater interest of telephone self-management support. Self-efficacy was not associated with interest in any self-management support mode (Table 2). We did not find significant interactions between race/language group and age, health literacy, or educational attainment on interest in any self-management support strategy (all p-values > 0.20).
Table 2.
Characteristics associated with Telephone, Group Medical Visit, and Internet Self-Management Support Acceptance.
| Telephone Self- | Group Medical | Internet Self- | |
|---|---|---|---|
| Management | Visits | Management | |
| Characteristic | AOR (CI) | AOR (CI) | AOR (CI) |
| Age, for 5-year increase | |||
| above sample mean | 0.89 (0.82–0.96)* | 0.90 (0.84–0.97)* | 0.85 (0.79–0.92)* |
| Female gender | 1.03 (0.72–1.47) | 0.98 (0.70–1.35) | 0.99 (0.71–1.38) |
| Race/ language | |||
| Non-Hispanic (NH) White | 1.00* | 1.00* | 1.00* |
| NH African American | 1.52 (0.99–2.33)* | 1.75 (1.17–2.63)* | 1.59 (1.06–2.40)* |
| English-speaking Hispanic | 1.74 (0.94–3.21)* | 1.36 (0.78–2.38)* | 0.81 (0.45–1.45)* |
| Spanish-speaking Hispanic | 3.45 (1.97–6.05)* | 2.45 (1.49–4.02)* | 0.56 (0.33–0.93)* |
| Years with diabetes | 1.00 (0.98–1.02) | 1.02 (1.00– 1.03)† | 0.99 (0.97–1.01) |
| Insulin Use | 0.99 (0.68–1.45) | 0.82 (0.58–1.16) | 1.24 (0.88–1.77) |
| Limited self-reported health | 1.74 (1.19–2.54)* | 1.16 (0.83–1.63) | 0.79 (0.56–1.13)† |
| literacy | |||
| Very poor diabetes control | 1.92 (0.47–7.78) | 2.97 (0.92–9.58)† | 1.87 (0.62–5.67) |
| Education level | |||
| More than high school | 1.00† | 1.00† | 1.00* |
| High school graduate | 1.56 (1.01–2.40)† | 0.71 (0.47–1.07)† | 0.69 (0.46–1.04)* |
| Less than high school | 1.42 (0.91–2.22)† | 1.01 (0.67–1.53)† | 0.52 (0.34–0.79)* |
| Type of insurance | |||
| No insurance | 1.00 | 1.00 | 1.00 † |
| Public insurance | 1.04 (0.69–1.56) | 1.02 (0.70–1.48) | 0.93 (0.63–1.36)† |
| Private insurance | 0.78 (0.42–1.44) | 0.85 (0.48–1.51) | 0.99 (0.55–1.76)† |
| Other insurance | 0.92 (0.40–2.14) | 0.89 (0.42–1.89) | 2.38 (1.08–5.22)† |
| Self-efficacy score | 0.98 (0.91–1.04) | 0.98 (0.92–1.04) | 0.98 (0.92–1.04) |
| Seen by diabetes educator | 1.25 (0.84–1.87) | 1.42 (0.99–2.04)† | 0.82 (0.56–1.19) |
| Attended a diabetes class | 1.12 (0.74–1.70) | 1.32 (0.91–1.93)† | 1.27 (0.87–1.86) |
| Received educational | 0.82 (0.57–1.18) | 0.91(0.65–1.26) | 0.91 (0.64–1.28) |
| materials | |||
| Fair or poor health status | 1.36 (0.95–1.95)† | 1.50 (1.08–2.08)* | 0.93 (0.66–1.30) |
p<0.05
p<0.20
In our exploratory analysis of perceived communication benefit, 315 (40%) patients reported that their diabetes would be better controlled if they communicated better with their regular health care provider. Racial/ ethnic minority participants were more likely to perceive a benefit of better communication than non-Hispanic White participants (47% vs. 25%, p<0.001). Among Hispanic participants, English and Spanish speakers were equally likely to report a communication benefit (46% vs. 47%, P=0.93). Participants who perceived a benefit to better communication were more likely to report limited health literacy (52% vs. 31%, p<0.001), and lower self-efficacy (p<0.001). After adjustment for all demographic and clinical factors in Table 2, perceiving a benefit to communication was independently associated with overall self-management interest (AOR 2.1, 95%CI 1.6–2.8). When perceived communication benefit was added to the models shown in Table 2, it was significantly associated with interest in telephone (AOR 2.84, 95%CI 1.90–4.42) and group visit (AOR 2.03, 95% CI 1.44–2.87) self-management support, but was not associated with internet self-management support (AOR 1.25, 95%CI 0.89–1.78). The relationships between other predictors and interest in self-management support did not substantively change (data not shown). Adding perceived communication as a co-variate improved the model fit relative to the model including all other co-variates in Table 2 for telephone self-management support (χ2 27, p<0.001) and group visits (χ2 17, p<0.001), but not internet/ computer-based support (χ2 1.6, p=0.20).
4. Discussion and Conclusion
4.1. Discussion
There has been very little research contrasting self-management support strategies, and health systems need this information in order to decide how to best deliver self-management support(62) There has recently been a focus on internet self-management support applications, often to the exclusion of other strategies(24, 30), and this may be particularly problematic for ethnically diverse, underprivileged populations. To our knowledge, this is first study to describe self-management support preferences in a large, racially diverse sample of diabetes patients recruited from multiple public hospital systems. Overall, there was considerable interest in self-management support strategies, particularly via the telephone. Nevertheless, no single approach was universally preferred by all patients and preferences varied considerably by race, ethnicity, and health literacy level.
Although interest in self-management support was high across the entire sample, we found that racial/ ethnic minorities, in general, expressed more interest in self-management support strategies compared to non-Hispanic whites. Racial and ethnic minority patients may report a greater interest in self-management support because their level of unmet need for such services is particularly great. Consistent with prior studies, Spanish speakers in this study expressed greater interest than English speakers in telephone self-management support and group medical visits (17, 63). However, Hispanic participants were significantly less interested than non-Hispanics in internet-based self-management support. Since prior work in other settings has shown high acceptance of carefully developed, computer-based health interventions among Hispanics who are trained in their use (30, 64, 65), this finding may reflect a general discomfort with internet use due to a lack of familiarity. Racial/ ethnic differences in patients’ preferences for different communication modalities underscore the need to provide an array of approaches for patients in safety-net settings and to match the strategy with patient preferences. Given the fact that socio-economically vulnerable populations are disproportionately affected by diabetes and its complications, even the modest differences in interest amongst the self-management support strategies that we observed could have important public health, clinical and policy implications.
We found that patients who reported limited health literacy were more likely to prefer telephone self-management support, and that self-reported health literacy was associated with perceived communication benefit. This suggests that patients with limited self-reported health literacy are aware of the need for improved communication, and that health systems should not underestimate their willingness to participate in such initiatives. Although ‘perceived communication benefit’ is a novel measure that requires more detailed examination in concert with other communication scales, the fact that it is correlated with self-reported health literacy, another marker of impaired communication, should encourage its further study.
Perceived communication benefit did not appear to mediate the relationship between patient characteristics and self-management support interest. This suggests that the current practice of directing self-management support to patients based on criteria such as metabolic control or health care utilization may not be a comprehensive way to identify and target interested patients. It may also be effective to direct self-management support to diabetes patients with limited health literacy or those reporting an unmet communication need .
Our study has several limitations. Although the response rate of 47% is similar to other diabetes studies, such as the 53% response rate in the TRIAD study (66–68), it limits our ability to generalize the study results. The secular trend of declining response rates to telephone surveys likely affected our study as well(69, 70). Moreover, since individual question non-response is much lower in telephone interviews than face-to-face interviews, telephone surveys can produce comparable-quality data to those produced by a face-to-face survey for many characteristics, despite a difference in response rates(71). Despite the response rate, this survey provides a starting point for more definitive investigation of patient preferences, including improved sampling. Our results may not be generalizable to those without telephone access- a small but important group(72). It is likely that our use of a telephone survey led to an over-estimate of telephone self-management support acceptability. Although we did not measure computer access among participants, we did attempt to account for differential computer use by asking patients to report their preferences under the assumption that they had access to the internet. In the survey, rather than measuring acceptance of a particular intervention, we asked patients if they would consider each self-management support strategy in general. Although patients’ perceptions of an actual, specific implementation of that strategy may differ substantially, the patterns we detected were similar to acceptance of an actual diabetes intervention in a similar population(73). We did not ask participants to rank the strategies. Because patient data were de-identified for the survey, we could not compare patients’ reported diabetes control to clinical measures such as their hemoglobin A1C. In addition, we did not measure health literacy directly, but used a previously validated single item(56) to estimate health literacy, and further validated this item using a diverse sample of diabetes patients from one site. This may have under-estimated the prevalence of limited health literacy; thus, the literacy effects may have been stronger with direct health literacy measurement. Nevertheless, we expect that the overall direction of these effects would be similar and any difference would be small given that the prevalence of limited self-reported health literacy in our sample was similar to measured health literacy found in similar patient populations(74). Finally, although we asked patients to report their level of diabetes control, we did not define “diabetes control” in the survey. Prior studies suggest patients and providers may differ in their interpretation of “control” (75, 76), with some patients interpreting control over diabetes as the level of its intrusiveness into their lives. Nonetheless, even in the context of this interpretation, we believe that the extent of a communication benefit still confers insight into self-management support interest.
4.2. Conclusion
In summary, diabetes patients seen in safety-net settings expressed substantial interest in diabetes self-management support, and preferences for self-management support strategy varied by race/ethnicity, language proficiency, and self-reported health literacy. These findings are consistent with prior studies demonstrating that tailored health education and behavior change programs delivered via information technologies are acceptable to vulnerable groups (12, 30, 77, 78).
4.3. Practice Implications
Our findings suggest that most diabetes patients treated in safety-net settings are interested in receiving some adjunctive form of self-management support to help achieve greater self-management success. Because different subgroups report distinct self-management support preferences, health systems and practitioners should offer a range of supportive strategies to improve patient self-management. Practitioners should consider the population in choosing a support modality, and tailor resources to their patients’ preferences. Many patients report an unmet need for better communication to support their efforts to self-manage their condition. Given the high prevalence of limited health literacy and the extent to which patients, particularly racial/ethnic minorities, perceive a benefit of improved provider communication for their diabetes control, the design and delivery of self-management support interventions should directly address the communication barriers experienced by vulnerable groups.
Acknowledgments
Funding: Urmimala Sarkar is supported by National Research Service Awards Grant Number 1 T32 HP19025. John Piette is a VA Career Scientist. Dean Schillinger is supported by a NIH Mentored Clinical Scientist Award K-23 RR16539-05. Support for this research was provided by the National Public Health and Hospital Institute and The Commonwealth Fund. The views presented here are those of the authors and should not be attributed to the Commonwealth Fund or its directors, officers, or staff.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Fisher EB, Brownson CA, O'Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health. 2005;95(9):1523–1535. doi: 10.2105/AJPH.2005.066084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press, Institute of Medicine Committee on Quality of Health Care in America; 2001. [PubMed] [Google Scholar]
- 3.Mensing C, Boucher J, Cypress M, et al. National standards for diabetes self-management education. Task Force to Review and Revise the National Standards for Diabetes Self-Management Education Programs. Diabetes Care. 2000;23(5):682–689. doi: 10.2337/diacare.23.5.682. [DOI] [PubMed] [Google Scholar]
- 4.Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52(3):315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 5.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–252. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239–243. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chumbler NR, Neugaard B, Ryan P, Qin H, Joo Y. An observational study of veterans with diabetes receiving weekly or daily home telehealth monitoring. J Telemed Telecare. 2005;11(3):150–156. doi: 10.1258/1357633053688723. [DOI] [PubMed] [Google Scholar]
- 8.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24(2):202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 9.Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization. A randomized, controlled trial. Ann Intern Med. 1998;129(8):605–612. doi: 10.7326/0003-4819-129-8-199810150-00004. [DOI] [PubMed] [Google Scholar]
- 10.Piette JD. Interactive voice response systems in the diagnosis and management of chronic disease. Am J Manag Care. 2000;6(7):817–827. [PubMed] [Google Scholar]
- 11.Weinberger M, Kirkman MS, Samsa GP, et al. A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: impact on glycemic control and health-related quality of life. J Gen Intern Med. 1995;10(2):59–66. doi: 10.1007/BF02600227. [DOI] [PubMed] [Google Scholar]
- 12.Piette JD, McPhee SJ, Weinberger M, Mah CA, Kraemer FB. Use of automated telephone disease management calls in an ethnically diverse sample of low-income patients with diabetes. Diabetes Care. 1999;22(8):1302–1309. doi: 10.2337/diacare.22.8.1302. [DOI] [PubMed] [Google Scholar]
- 13.Lorig K, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Annals of Behavioral Medicine. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 14.Lorig K, Ritter P, Stewart A, et al. Chronic Disease Self-Management Program: 2-year health status and health utilization outcomes. Medical Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Kim S, Love F, Questberg D, Shea JA. Association of Health Literacy With Self-Management Behavior in Patients with Diabetes. Diabetes Care. 2004;27(12):2980–2982. doi: 10.2337/diacare.27.12.2980. [DOI] [PubMed] [Google Scholar]
- 16.Culhane-Pera K, Peterson KA, Crain AL, et al. Group visits for Hmong adults with type 2 diabetes mellitus: a pre-post analysis. J Health Care Poor Underserved. 2005;16(2):315–327. doi: 10.1353/hpu.2005.0030. [DOI] [PubMed] [Google Scholar]
- 17.Lorig K, Ritter P, Jacquez A. Outcomes of Border Health Spanish/ English Chronic Disease Self-Management Programs. Diabetes Educator. 2005;31(3):401–409. doi: 10.1177/0145721705276574. [DOI] [PubMed] [Google Scholar]
- 18.Roter DL, Stashefsky-Margalit R, Rudd R. Current perspectives on patient education in the US. Patient Educ Couns. 2001;44(1):79–86. doi: 10.1016/s0738-3991(01)00108-2. [DOI] [PubMed] [Google Scholar]
- 19.Clancy DE, Cope DW, Magruder KM, Huang P, Salter KH, Fields AW. Evaluating group visits in an uninsured or inadequately insured patient population with uncontrolled type 2 diabetes. The Diabetes educator. 2003;29(2):292–302. doi: 10.1177/014572170302900220. [DOI] [PubMed] [Google Scholar]
- 20.Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22(12):2011–2017. doi: 10.2337/diacare.22.12.2011. [DOI] [PubMed] [Google Scholar]
- 21.Trento M, Passera P, Tomalino M, et al. Group visits improve metabolic control in type 2 diabetes: A 2-year follow-up. Diabetes Care. 2001;24(6):995–1000. doi: 10.2337/diacare.24.6.995. [DOI] [PubMed] [Google Scholar]
- 22.Fiscella K, Geiger HJ. Health information technology and quality improvement for community health centers. Health Aff (Millwood) 2006;25(2):405–412. doi: 10.1377/hlthaff.25.2.405. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow R, Bull S. Making a difference with interactive technology: considerations in using and evaluating computerized aids for diabetes self-management education. Diabetes Spectrum. 2001;14(2):99–106. [Google Scholar]
- 24.Glasgow RE, Bull SS, Piette JD, Steiner JF. Interactive behavior change technology. A partial solution to the competing demands of primary care. Am J Prev Med. 2004;27 2 Suppl:80–87. doi: 10.1016/j.amepre.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 25.Glasgow RE, Nutting PA, King DK, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28(1):33–39. doi: 10.2337/diacare.28.1.33. [DOI] [PubMed] [Google Scholar]
- 26.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care? J Amer Med Assoc. 2003;290(2):259–264. doi: 10.1001/jama.290.2.259. [DOI] [PubMed] [Google Scholar]
- 27.McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care. 2001;24(8):1328–1334. doi: 10.2337/diacare.24.8.1328. [DOI] [PubMed] [Google Scholar]
- 28.Dang S, Ma F, Nedd N, Aguilar EJ, Roos BA. Differential resource utilization benefits with Internet-based care coordination in elderly veterans with chronic diseases associated with high resource utilization. Telemed J E Health. 2006;12(1):14–23. doi: 10.1089/tmj.2006.12.14. [DOI] [PubMed] [Google Scholar]
- 29.Shea S, Starren J, Weinstock RS, et al. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) Project: rationale and design. J Am Med Inform Assoc. 2002;9(1):49–62. doi: 10.1136/jamia.2002.0090049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shea S, Weinstock RS, Starren J, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. J Am Med Inform Assoc. 2006;13(1):40–51. doi: 10.1197/jamia.M1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: Chronic disease self-management programs for older adults. Annals of Internal Medicine. 2005;143(6):427–438. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 32.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 33.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. The American journal of managed care. 2005;11(8):478–488. [PMC free article] [PubMed] [Google Scholar]
- 34.Li R, Simon J, Bodenheimer T, et al. Organizational factors affecting the adoption of diabetes care management processes in physician organizations. Diabetes Care. 2004;27(10):2312–2316. doi: 10.2337/diacare.27.10.2312. [DOI] [PubMed] [Google Scholar]
- 35.Rittenhouse DR, Robinson JC. Improving quality in Medicaid: The use of care management processes for chronic illness and preventive care. Medical Care. 2006;44(1):47–54. doi: 10.1097/01.mlr.0000188992.48592.cd. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen-Bohlman Lea., editor. Institute of Medicine. Health Literacy: A prescription to end confusion. Washington, D.C: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 37.Shojania KG, Grimshaw JM. Still no magic bullets: Pursuing more rigorous research in quality improvement. The American journal of medicine. 2004;116(11):778–780. doi: 10.1016/j.amjmed.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 38.Agency for Healthcare Research and Quality. U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality; National Healthcare Disparities Report. 2005 December 2005. Report No.: AHRQ Publication No. 06-0017.
- 39.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Reports. 2006;121(3):245–254. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: Overcoming impediments to prevention and control. J Amer Med Assoc. 2004;291(21):2616–2622. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 41.Eakin EG, Bull SS, Glasgow RE, Mason M. Reaching those most in need: A review of diabetes self-management interventions in disadvantaged populations. Diabetes/metabolism research and reviews. 2002;18(1):26–35. doi: 10.1002/dmrr.266. [DOI] [PubMed] [Google Scholar]
- 42.The Commonwealth Fund. Regenstein M, Huang J, Cummings L, Lessler D, Reilly B, Schillinger D. Caring for patients with diabetes in safety net hospitals and health systems; Caring for patients with diabetes in safety net hospitals and health systems. 2005 June 2005. Report No.: Commonwealth Fund pub. 826.
- 43.Healthy People 2010. [Accessed August 6, 2006];Health Communication. http://www.healthypeople.gov/document/html/volume1/11healthcom.htm.
- 44.Freimuth VS. The chronically uninformed: Closing the knowledge gap in health. In: Ray EB, Donohew L, editors. Communication and Health: Systems and Applications. Hillsdale, NJ: Lawrence Erlbaum Associates; 1990. [Google Scholar]
- 45.Eng TR, Maxfield A, Patrick K, Deering MJ, Ratzan SC, Gustafson DH. Access to health information and support: a public highway or a private road? J Amer Med Assoc. 1998;280(15):1371–1375. doi: 10.1001/jama.280.15.1371. [DOI] [PubMed] [Google Scholar]
- 46.Stewart AL, Napoles-Springer A, Perez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–339. doi: 10.1111/1468-0009.00138. 274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. J Amer Med Assoc. 1997;277(4):350–356. [PubMed] [Google Scholar]
- 48.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. An exploratory study of communication with Spanish-speaking patients. J Gen Intern Med. 2004;19(2):167–174. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14(7):409–417. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cooper L, Roter D. Patient-provider communication: the effect of race and ethnicity on process and outcomes of healthcare. In: Smedley B, Stith A, Nelson A, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: The National Academies Press; 2002. pp. 552–593. [Google Scholar]
- 52.Cooper LA, Beach MC, Johnson RL, Inui TS. Delving below the surface. Understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21 Suppl 1:S21–S27. doi: 10.1111/j.1525-1497.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grubbs V, Chen AH, Bindman AB, Vittinghoff E, Fernandez A. Effect of awareness of language law on language access in the health care setting. J Gen Intern Med. 2006;21(7):683–688. doi: 10.1111/j.1525-1497.2006.00492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 55.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 56.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 57.FACCT. [Accessed July 12, 2006];Diabetes Care Survey. http://www.markle.org/resources/facct/doclibFiles/documentFile_311.pdf.
- 58.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 59.Heisler M, Smith D, Hayward R, Krein KreinS, Kerr E. How well do patients$#x00027;,assessments of their diabetes self-management correlate with actual glycemic control and receipt of recommended diabetes services? Diabetes Care. 2003;26(3):738–743. doi: 10.2337/diacare.26.3.738. [DOI] [PubMed] [Google Scholar]
- 60.Corbett KK, Gonzales R, Leeman-Castillo BA, Flores E, Maselli J, Kafadar K. Appropriate antibiotic use: variation in knowledge and awareness by Hispanic ethnicity and language. Prev Med. 2005;40(2):162–169. doi: 10.1016/j.ypmed.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 61.McCulloch C, Searle S. Generalized, Linear, and Mixed Models. Vol. Section 1.6b. New York: Wiley & Sons; 2001. p. 17. [Google Scholar]
- 62.Goldman LE, Handley M, Rundall TG, Schillinger D. Current and future directions in Medi-Cal chronic disease care management: a view from the top. Am J Manag Care. 2007;13(5):263–268. [PubMed] [Google Scholar]
- 63.Piette JD. Patient education via automated calls: a study of English and Spanish speakers with diabetes. Am J Prev Med. 1999 Feb;17:138–141. doi: 10.1016/s0749-3797(99)00061-6. [DOI] [PubMed] [Google Scholar]
- 64.Hahn EA, Cellal D, Dobrez DG, et al. Quality of life assessment for low literacy Latinos: a new multimedia program for self-administration. J Oncol Manag. 2003;12(5):9–12. [PubMed] [Google Scholar]
- 65.Leeman-Castillo BA, Corbett KK, Aagaard EM, Maselli JH, Gonzales R, Mackenzie TD. Acceptability of a bilingual interactive computerized educational module in a poor, medically underserved patient population. J Health Commun. 2007;12(1):77–94. doi: 10.1080/10810730601096630. [DOI] [PubMed] [Google Scholar]
- 66.Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93(10):1713–1719. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Murray E, Lo B, Pollack L, et al. The impact of health information on the internet on the physician-patient relationship: patient perceptions. Arch Intern Med. 2003;163(14):1727–1734. doi: 10.1001/archinte.163.14.1727. [DOI] [PubMed] [Google Scholar]
- 68.The Translating Research Into Action for Diabetes (TRIAD) study: a multicenter study of diabetes in managed care. Diabetes Care. 2002;25(2):386–389. doi: 10.2337/diacare.25.2.386. [DOI] [PubMed] [Google Scholar]
- 69.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. J Amer Med Assoc. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 70.Prevalence of current cigarette smoking among adults and changes in prevalence of current and some day smoking--United States, 1996–2001. MMWR Morb Mortal Wkly Rep. 2003;52(14):303–304. 306–307. [PubMed] [Google Scholar]
- 71.Biemer P. Nonresponse Bias and Measurement Bias in a Comparison of Face to Face and Telephone Interviewing. Journal of Official Statistics. 2003;17(2):295–320. [Google Scholar]
- 72.Blumberg SJ, Luke JV, Cynamon ML. Telephone coverage and health survey estimates: evaluating the need for concern about wireless substitution. Am J Public Health. 2006;96(5):926–931. doi: 10.2105/AJPH.2004.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schillinger D, Hammer H, Wang F, et al. Seeing in 3-D: Examining the Reach of Diabetes Self-Management Support Strategies in a Public Health Care System. Health Educ Behav. 2007 doi: 10.1177/1090198106296772. [DOI] [PubMed] [Google Scholar]
- 74.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20(2):175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hunt LM, Arar NH, Larme AC. Contrasting patient and practitioner perspectives in type 2 diabetes management. West J Nurs Res. 1998;20(6):656–676. doi: 10.1177/019394599802000602. discussion 677-82. [DOI] [PubMed] [Google Scholar]
- 76.Hunt LM, Pugh J, Valenzuela M. How patients adapt diabetes self-care recommendations in everyday life. J Fam Pract. 1998;46(3):207–215. [PubMed] [Google Scholar]
- 77.Farmer A, Gibson OJ, Tarassenko L, Neil A. A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med. 2005;22(10):1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 78.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: a randomized, controlled trial. Med Care. 2000;38(2):218–230. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]