Abstract
Little data are available on how HIV and other sexually transmitted infections (STIs) affect indigenous people in Latin America, including Peru. We conducted a sero-epidemiologic survey of HIV infection and syphilis in a native community, the Chayahuita, an indigenous population in the Amazon region of Peru. The seroprevalences of HIV and syphilis in adults were 7.5% (6 of 80) and 6.3% (5 of 80), respectively. None of the participants had ever used a condom. Male to male sexual behavior was common. At the current levels of HIV prevalence, there is the risk of a negative impact on the survival of the Chayahuita ethnic group as a whole. The outcomes of this study highlight the need for urgent medical and anthropologic approaches to stop HIV transmission in indigenous Amazonian communities.
Infection by the HIV-1 in Peru has been primarily concentrated in men who have sex with men (MSM),1–5 and to a lesser extent, among heterosexual female commercial sex workers.6 By the end of 2004, the Peruvian Ministry of Health (MoH) estimated ~35,000 cases of HIV infection in all of Peru.7 The department of Loreto in the Peruvian Amazon has the second highest rate of HIV infection, after the capital city Lima.7 Studies of this department and especially its capital, Iquitos, show a more permissive sexual culture that would be expected to increase HIV risk.8–10 Most of the Peruvian indigenous people in Peru live in Loreto, but little is known in this population regarding basic health parameters.11,12 Insufficient information is available regarding the prevalence of HIV and other sexually transmitted infections (STIs) affecting indigenous populations in Peru. Indigenous populations are at particular risk for experiencing an expansion of the HIV epidemic given the difficulty of providing practical health information to such people.13–15
To begin to address this public health issue, we conducted a serosurvey on the prevalence of HIV and syphilis in a native community of the Chayahuita indigenous population in the department of Loreto.
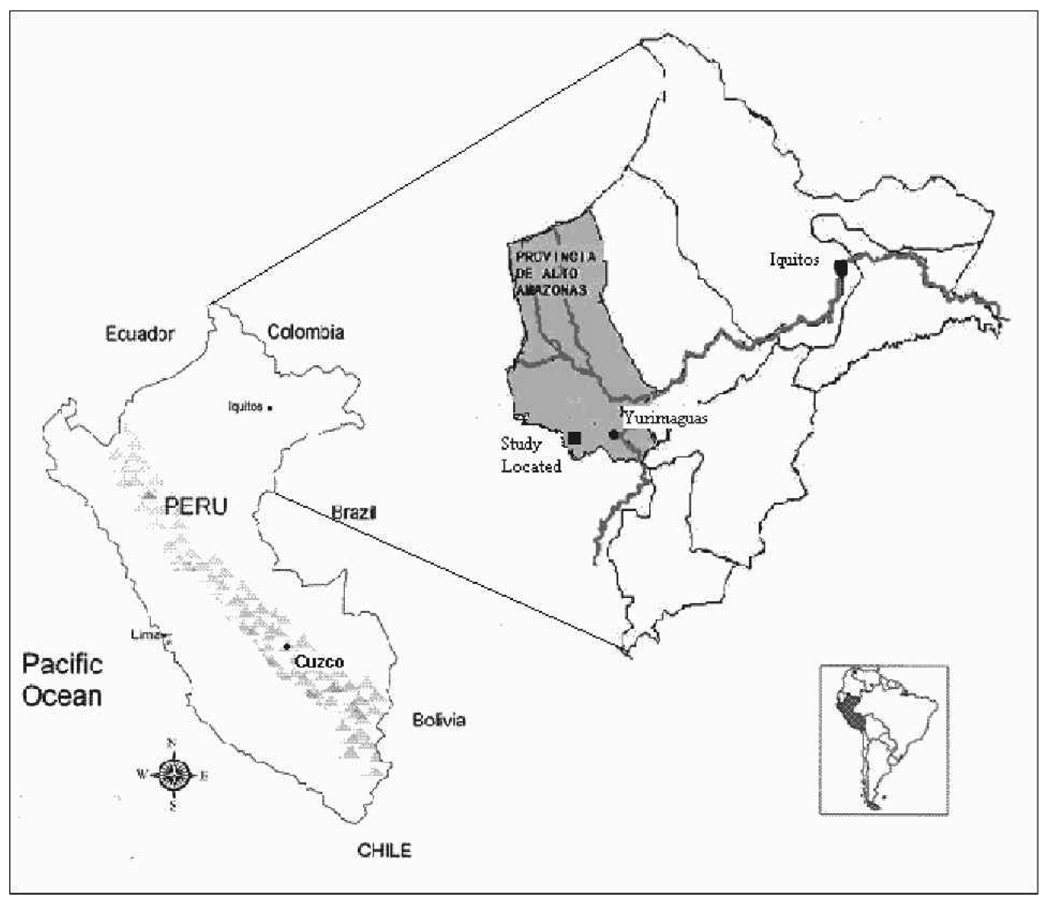
The Chayahuita ethnic groups are Amazonian Aborigines, quite distinct from the indigenous Andean populations (Quechuas) from the sierra of Peru. They live in small geographically partially isolated communities in the Peruvian Amazon province of Loreto in northeastern Peru. There is a health post with a health technician in this community; however, the main hospital is located in Yurimaguas city, which is 12 hours by river or a 24-hour hike (Figure 1).
FIGURE 1.
Chayahuita indigenous people location in Loreto department, Peruvian Amazon.
The population of this community was estimated at 162 persons. They consist of farmers (cultivating primarily yucca, corn, and bananas), fishermen, and hunters. Most of the Chayahuita population are married or cohabitating. This population also has their own dialect, however, the men speak Spanish. This community is highly illiterate, illiteracy is more prevalent among the women reaching 50%; school is taught in Spanish although the teachers are bilingual Chayahuita/Spanish. In general, the men among this population have more freedom than the women.16,17
In May 2004, the Ministry of Health’s (MoH) Office of Epidemiology received a report of the death of a patient diagnosed with AIDS from the Chayahuita community. With approval from the MoH and from Chayahuita community leaders, a MoH epidemiologist visited this community to provide public health information about HIV and AIDS and to determine the prevalence of HIV and syphilis infection in the community. The field visit was coordinated with the highest authority of the community called the Apu. Respecting Chayahuita traditions and customs, the Apu and the men of the community (the heads of families) gave their verbal and written consent to interview and take blood samples of their family members, who also gave their verbal consent. All men and women older than 18 years of age were invited to participate voluntarily in the study. Individuals less than 18 years of age were included when requested by the head of the family. All study participants received pre-test counseling as a group before participating and post-test counseling after test results were available. This study was approved by the MoH and Universidad Peruana Cayetano Heredia Ethical Committees.
Interviews were conducted in Spanish using standard MoH epidemic report forms for STIs and HIV/AIDS, with epidemiology and risk behavior information. MSM was defined as a man reporting ever having sex with a man. Blood samples were collected, coded and kept frozen at [minus]20°C and transported to the local hospital. Samples were tested for HIV by ELISA according to the manufacturer’s instructions (Genscreen Bonus HIV Ag-Ab; Bio Rad, Marnes-la-Coquette, France). Positive results were confirmed by Western blot (Inno-Lia HIV ½; Inno-Chenetics, Zwijnaarde, Germany) or an in-house immunofluorescent assay at the National Health Institute (INS) in Lima. A rapid plasma reagin (RPR) test was performed and the FTA-abs (fluorescent treponemal antibody absorption test; Zeus Scientific, Raritan, NJ) was done in Lima to confirm the syphilis diagnosis. The FTA-abs reactive cases described were considered latent syphilis because no patient had syphilis-related symptoms at the time of the evaluation.
Of the 162 inhabitants, 117 (72.2%) completed the questionnaires and provided blood samples. The study group included 37 children (< 15 years old) and 80 adults. All 37 children (18 boys and 19 girls) were negative for HIV ELISA and RPR. Among the 80 adults, there were 6 of 80 HIV-positive cases (7.5%) and 5 of 80 syphilis cases (6.3%). No cases of co-infection of HIV and syphilis were detected.
Within the male population, HIV was most frequent among MSM compared with those reporting only heterosexual contact: 4 of 21 (19%) versus 1 of 26 (3.8%), respectively; OR 5.88 (P = 0.11 by Fisher exact test). However FTB-ab positive was less frequent among the MSM 1 of 21 (4.8%) than heterosexual men 4 of 26 (15.4%); fewer MSM had positive syphilis serology (OR, 0.28; P = 0.25 by Fisher exact test). Women (33 of 33) reported only heterosexual sex. None of the adult participants had ever a used condom (Table 1).
TABLE 1.
Characteristics of the study population and HIV and syphilis
| Characteristic | HIV [N positive/tested (%)] | Syphilis [N positive/tested (%)] | ||
|---|---|---|---|---|
| Age (yr) | ||||
| 0–15 | 0/37 | 0.0% | 0/37 | 0.0% |
| 16–30 | 3/55 | 5.5% | 3/55 | 5.4% |
| 31–45 | 3/18 | 17.0% | 1/18 | 5.5% |
| 46–60 | 0/7 | 0.0% | 1/7 | 14.3% |
| Sex | ||||
| Female | 1/33 | 3.0% | 2/33 | 6.1% |
| Male | 5/47 | 10.6% | 3/47 | 6.4% |
| Male sexual behavior | ||||
| Heterosexual | 1/26 | 3.8% | 4/26 | 15.4% |
| Bisexual | 1/17 | 5.9% | 1/17 | 5.9% |
| Homosexual | 3/4 | 75.0% | 0/4 | 0.0% |
| History of an STI* | ||||
| Positive | 4/80 | 5.0% | 1/80 | 1.3% |
Sexually transmitted infection including urethral secretion, genital ulcer, or inguinal bubo in the previous 6 months.
Previously in Latin America, some cases of HIV infection have been reported among indigenous tribes in Brazil18 and in Honduras. A higher HIV seroprevalence than the general population has been documented among the Garifunas indigenous people.4 To our knowledge, this report is the first to describe HIV infection in an indigenous community in Peru.
Both HIV and syphilis were found only in adults. HIV prevalence rates were 10 and 3 times those reported in the general Peruvian population for men and women, respectively.4,7
In the Chayahuita population, behaviors previously reported as part of their cultural tradition, included early initiation into sexual activity and male polygamy.16 In this study, we found a high frequency of MSM behavior in young men (21 of 47, 44.1%) and no condom use. MSM behavior was found to be a risk factor for HIV among Chayahuita, in the small subgroup of male homosexuals (N = 4), 3 of whom 75% were infected. However, the rate of syphilis seropositivity was lower among the MSM than heterosexual men. Syphilis, as well as other non-venereally transmitted treponematoses, is well known to be endemic in the Americas, long before the introduction of HIV. Syphilis (or other treponematoses) was probably introduced into the community before HIV and is transmitted independent of people infected with HIV, most likely by chance.
In retrospect, we suspect that the index case was a Chayahuita man who acquired the HIV during military service and returned to this community infected. This man died in 2001 from complications of AIDS. His widow was found to be HIV positive; after the death of her husband, the widow married her former brother-in-law. We have not confirmed whether widow inheritance is a cultural tradition. However, studies in this ethnic group should investigate this question, because in other places, widow inheritance has been shown to be a risk factor for the spread of the epidemic.19,20 It is possible that HIV infection may have spread from the initial case to bisexual and homosexual people in this population. A sexual network study to determine how HIV entered and spread through this relatively isolated community is planned.
We found that the prevalence of syphilis in the Chayahuita was higher than in the general population of the city of Iquitos, the capital of Loreto, a place considered to be a hotbed of STIs.4,8 Genital ulcer disease increase the risk for HIV transmission.21 Even though treponemal and HIV infections involved distinct people in our study, finding syphilis or other genital ulcer diseases in this population could indicate that the Chayahuita and other similar groups could have an enhanced risk of HIV acquisition.
It is a major concern that none of the participants reported ever using a condom. Condoms are not part of the culture norms of this indigenous group, although the MoH does offer free condoms in this community. However, given the current levels of HIV prevalence, HIV/AIDS is likely to present a significant future threat to the Chayahuita and similar groups. This study highlights the need for an urgent medical and anthropological approach to stop HIV transmission in indigenous Amazonian communities.
Acknowledgments
Financial support: This study was supported by U.S. Public Health Service National Institutes of Health/Fogarty International Center Global Infectious Disease Training Grant, “Endemic Infectious Diseases of the Peruvian Amazon,” D43 TW007120 (EG, Peruvian Program Director).
REFERENCES
- 1.Bautista CT, Sanchez JL, Montano SM, Laguna-Torres VA, Lama JR, Sanchez JL, Kusunoki L, Manrique H, Acosta J, Montoya O, Tambare AM, Avila MM, Vinoles J, Aguayo N, Olson JG, Carr JK. Seroprevalence of and risk for HIV-1 infection among South American men who have sex with men. Sex Transm Inf. 2004;80:498–504. doi: 10.1136/sti.2004.013094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tabet S, Sanchez J, Lama J, Goicochea P, Campos P, Rouillon M, Cairo JL, Ueda L, Watts D, Celum C, Holmes KK. HIV, syphilis and heterosexual bridging among Peruvian men who have sex with men. AIDS. 2002;16:1271–1277. doi: 10.1097/00002030-200206140-00010. [DOI] [PubMed] [Google Scholar]
- 3.Cáceres C, Gotuzzo E, Wignall S, Campos M. Sexual behavior and frequency of antibodies to type 1 human immunodeficiency virus (HIV-1) in a group of Peruvian male homosexuals. Bull Pan Am Health Organ. 1991;25:306–319. [PubMed] [Google Scholar]
- 4.United Nations Programme on HIV/AIDS (UNAIDS), World Health Organization (WHO) Ginebra: UNAIDS/WHO; AIDS Epidemic Update: December 2004. 2004
- 5.Evans CA, Friedland JS, Gotuzzo E. HIV in South America. Medicine. 2001;29:37–38. doi: 10.1383/medc.33.6.44.66003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCarthy MC, Wignall FS, Sanchez J, Gotuzzo E, Alarcon J, Phillips I, Watts DM, Hyams KC. The epidemiology of HIV-1 infection in Peru, 1986–1990. AIDS. 1996;10:1141–1145. [PubMed] [Google Scholar]
- 7.General Office of Epidemiology of the Peruvian Ministry of Health (OGE) [Accessed October 25, 2005];Epidemiological situation of HIV/AIDS in Peru. 2005 Available at http://www.oge.sld.pe/vigilancia/Boletines/2005/SE42/Bolet%EDn%20Epidemiol%F3gico%20N%2042.pdf.
- 8.Paris M, Gotuzzo E, Goyzueta G, Aramburú J, Cáceres C, Crawford D. Motorcycle taxi drivers and sexually transmitted infections in a Peruvian Amazon City. Sex Transm Dis. 2001;28:11–13. doi: 10.1097/00007435-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Cáceres C, Mendoza W, Yon C, Rosasco A, Cabezudo C. SIDA en el Perú: Imágenes de Diversidad, Situación y Perspectivas de la Epidemia en Chiclayo, Cuzco e Iquitos. Lima: UPCH y REDES Jóvenes; 1998. [Google Scholar]
- 10.National Institute of Statistics and Informatics. [Accessed November 2, 2005];The Demographic and Family Health Survey. 2000 Available at http://www.inei.gob.pe.
- 11.National Institute of Statistics and Informatics. [Accessed October 10, 2005];Indigenous Populations in the Amazon Region. 1997 Available at http://www.inei.gob.pe.
- 12.General Office of Epidemiology of the Peruvian Ministry of Health. [Accessed October 9, 2005];Health Care Situation of the Indigenous Populations in Peru. 2003 Available at http://www.oge.sld.pe/.
- 13.Butler JC, Crengle S, Cheek JE. Emerging infectious diseases among indigenous people. Emerg Infec Dis. 2001;7:554–555. doi: 10.3201/eid0707.017732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mckenna N. A disaster waiting to happen. WorldAIDS. 1993;27:5–9. [PubMed] [Google Scholar]
- 15.United Nations Programme on HIV/AIDS (UNAIDS), World Health Organization (WHO), Pan American Health Organization (PAHO) Ginebra: UNAIDS/WHO/PAHO; HIV and AIDS in the America: An Epidemic With Many Faces. 2001
- 16.Fuentes A. Porque las Piedras no Mueren, Historia, Sociedad y Ritos de los Chayahuitas del Alto Amazonas. Lima: Centro Amazónico de Antropología y Aplicación Práctica; 1988. [Google Scholar]
- 17.Dradi MP. La Mujer Chayahuita: ¿un Destino de Marginación? Lima: Instituto Nacional de Planificación. Fundación Friedrich Ebert; 1989. [Google Scholar]
- 18.Anonymous Brazil launches anti-AIDS campaign for indians. Education and prevention. AIDS Wkly. 1996;9:9. [PubMed] [Google Scholar]
- 19.Nyindo M. Complementary factors contributing to the rapid spread of HIV-I in sub-Saharan Africa: a review. East Afr Med J. 2005;82:40–46. doi: 10.4314/eamj.v82i1.9293. [DOI] [PubMed] [Google Scholar]
- 20.Okeyo TM, Allen AK. Influence of widow inheritance on the epidemiology of AIDS in Africa. Afri J Med Prac. 1994;1:20–25. [PubMed] [Google Scholar]
- 21.Dickerson MC, Johnston J, Delea TEM, White A, Andrews E. The causal role for genital ulcer disease as a risk factor for transmission of human immunodeficiency virus. An application of the Bradford Hill criteria. Sex Transm Dis. 1996;23:429–440. doi: 10.1097/00007435-199609000-00015. [DOI] [PubMed] [Google Scholar]