Abstract
Although much has been written about the utility of applying transactional models to the study of parenting practices, relatively few researchers have used such an approach to examine how children influence maternal wellbeing throughout their development. Using a sample of males from predominantly low-income families, the current study explored reciprocal relations between boys’ overt disruptive behavior (boys’ ages 5 to 10 years) and maternal depressive symptoms. We then examined this model with youth-reported antisocial behaviors (ASB) and maternal depressive symptoms when the boys were older, ages 10 to 15. In middle childhood, evidence was found for both maternal and child effects from boys’ ages 5 to 6 using both maternal and alternative caregiver report of child aggressive behavior. In the early adolescence model, consistent maternal effects were found, and child effects were evident during the transition to adolescence (boys’ ages 11 to 12). The findings are discussed in reference to reciprocal models of child development and prevention efforts to reduce both maternal depression and the prevalence of child antisocial behavior.
Keywords: Maternal depression, Externalizing behavior, Antisocial behavior, Reciprocal effects, Transactional model
Parental psychopathology has been found to be a consistent and robust correlate of children’s maladjustment (DelBello and Geller 2001; Goodman and Brumley 1990; Lapalme et al. 1997). Due to the prevalence of depression, especially in women, maternal depression has been the focus of numerous research studies on parental psychopathology and its association with child psychopathology. Findings in the extant literature provide substantial evidence for an association between maternal depression and negative child outcomes, including internalizing and externalizing child problem behaviors (for reviews of this literature, see Beardslee et al. 1998; Cummings and Davies 1994; Gelfand and Teti 1990).
In addition to research on the relation between maternal depression and different forms of child psychopathology, associations have been found between child characteristics and parental behavior (Bell and Harper 1977; Elgar et al. 2004; Lytton 1990). Rather than consider parent effects on children and child effects on parents to be separate processes, reciprocal models of socialization regard parenting behaviors and child characteristics as recurrent, transactional exchanges over time, where both parties affect the other (Bell 1968; Sameroff 1995). Whereas there is an extensive body of research on reciprocal effects between child disruptive behavior and aspects of parenting (Bell and Harper 1977; Danforth et al. 1991; Johnston and Mash 2001), substantially less attention has been paid to potential bidirectional effects between child disruptive behavior and parental mental health, such as depressive symptoms, over time. As the social and economic cost of adult depression and its association with negative child outcomes is high (Pincus and Petit 2001; Simon and Katzelnick 1997), it is important to better understand risk factors underlying the development and maintenance of both maternal depression and child problem behaviors. Thus, the purpose of the current study was to examine bidirectional processes between sons’ early disruptive and later antisocial behaviors and mothers’ depressive symptoms spanning from when boys were ages 5 to 15.
Maternal Depression and Child Adjustment
The association between maternal depression and poor child outcomes is one of the most robust findings in psychological research. Both maternal clinical depression and sub-clinical, elevated levels of depressive symptoms have been found to be related to child maladjustment (Cummings et al. 2005; Farmer et al. 2002); as a result, the term maternal depression will be used throughout this paper to describe both criteria.
Although researchers have studied children of depressed mothers across both narrowly defined developmental periods and broad age spans (Goodman and Gotlib 1999), there have been consistent findings linking maternal depression to disruptions in both socio-emotional and instrumental (e.g., academic) functioning (Elgar et al. 2004; Gelfand and Teti 1990). Studies of outcomes for school-aged children and adolescents of depressed mothers have documented associations between maternal depression and behavior problems, including higher rates of externalizing problems and more serious forms of antisocial behaviors as assessed by parent, teacher, and self report (Hay et al. 2003; Munson et al. 2001) and teacher reports of academic and behavior problems at school (Sinclair and Murray 1998). Other research using parent and teacher reports has found higher levels of social maladjustment in children of mothers with depressive symptoms, including lower levels of social competence and adaptive functioning (Luoma et al. 2001), as well as poor adjustment and self-esteem (Cummings et al. 2005; Wilkins et al. 2004). Moreover, numerous studies have found elevated rates of internalizing behaviors, especially depression, in children of depressed mothers (Cummings et al. 2005; Hammen and Brennan 2003; Leve et al. 2005).
Child Effects on Parents and Reciprocal Models
Child effects models emphasize the influence of children’s attributes and behaviors on their parents. The literature on parenting is replete with theoretical models and empirical evidence of child effects on parents. Belsky’s (1984) landmark paper on the determinants of parenting provides a foundation for reciprocal parenting models by positing that characteristics of both the parent and child contribute to adaptive and dysfunctional parenting. A well-known example of a reciprocal parenting model is Patterson’s coercive model of parenting (1982), in which a cycle of negative reinforcement is established when child noncompliance is reinforced by the parent. Accordingly, parents unwittingly reinforce a child’s disruptive behavior by paying more attention to it and not responding to the child’s prosocial behavior (Eddy et al. 2001; Prinzie et al. 2004). These types of coercive parenting practices have been linked back to long-term difficulties for children, particularly in rates of externalizing behaviors (Campbell et al. 2000; Dishion and Patterson 1997; Keenan and Shaw 1995). Other studies have found that child externalizing problems and delinquency in late childhood and adolescence influence parenting behaviors, such as monitoring, closeness, and discipline (Kandel and Wu 1995; Fite et al. 2006). In accounting for child effects on parenting in the late school-age period and adolescence, Fite et al. (2006) suggest that perhaps parents of children with elevated behavior problems become disenfranchised from their parenting role and feel hopeless in their attempts to discipline children, resulting in lower levels of supervision and closeness, as well as higher rates of inconsistent discipline.
Just as child behaviors are thought to influence parenting, a number of studies have found evidence for child effects on other adult behaviors, including marital quality (Cui et al. 2007; Leve et al. 2001), alcohol consumption (Pelham et al. 1997), social life (Donenberg and Baker 1993), parenting self efficacy (Cutrona and Trouman 1986; Teti and Gelfand 1991) and stress (Baker and Heller 1996; Feske et al. 2001). Moreover, there is a growing body of research on child effects and maternal depression. Findings that are consistent with a child effects model of maternal depression include higher rates of maternal depressive symptoms in samples of clinic-referred versus normal children (Brown et al. 1988; Fergusson et al. 1993) and in mothers whose children have more behavioral or emotional problems (Civic and Holt 2000). However, these findings could also be explained by the aversive effect of higher levels of maternal depression on child behavior or biases in ratings of child behavior by depressed caregivers. Other studies have found child effects on maternal depression as early as infancy. For example, Field et al. (1988) found that when infants of depressed mothers interacted with non-depressed adults in avoidant and unresponsive ways, non-depressed adults began to exhibit depressed-like manners in these interactions. Other infant studies have found that behavior problems and irritability in infants are associated with the persistence (Ghodsian et al. 1984) and onset of maternal clinical depression (Murray et al. 1996).
One child effects study addressed the methodological limitations of correlational studies by utilizing an experimental design. Pelham and colleagues (1997) asked married couples and single mothers to interact with 5- to12-year-old boys who were trained to behave in either a normal or defiant manner. While waiting to have a second interaction with the same boy, the adults completed questionnaires, including one assessing depressive symptoms. Those who had interacted with the defiant boys reported significantly higher levels of depressive symptoms than those interacting with nondefiant children.
Another study used a longitudinal design to examine whether individual differences in initial child behavior and child frontal asymmetry (i.e., EEG) were associated with changes in maternal report of depressive symptoms one year later (Forbes et al. 2006). Results indicated that mothers whose 3 to 9 year old children had either below average affect regulation and/or right frontal EEG asymmetry reported increased depressive symptoms one year later.
Finally, one recent study using the same cohort of children as the current study tested a reciprocal model by using child behavior at 1.5 years to predict trajectories of maternal depression over an eight and a half year span, and then used these trajectory groups to predict child outcomes at ages 11 and 12 (Gross et al., submitted for publication). Their results found support for a transactional model; disruptive child behavior in the toddler period was associated with increased risk for persistence of moderate to high levels of maternal depressive symptoms, which in turn was associated with increased risk of boys’ and teacher reports of adolescent antisocial behavior. However, the models tested in this study and other previous research have yet to explore the ongoing nature of reciprocal effects between child disruptive behavior and maternal depressive symptoms over short spans of time (e.g., on a year to year basis), or to compare parent and/or child effects during different developmental periods.
Collectively, the aforementioned findings on parent and child effects suggest the presence of bidirectional relations between maternal depression and child development. However, in most cases, the studies looked at parent or child effects separately instead of examining questions about mutual influence and the possibility that the behavior of each party may continue to affect and intensify the other’s behavior throughout development. The current study explored the possibility of reciprocal relations between maternal depression and developmentally typical antisocial behaviors from middle childhood through adolescence.
The theoretical groundwork to explain such a mechanism can be found in previous work on both parenting and depression. Maternal depression compromises parenting in ways that are associated with difficulties in child behavior (Goodman and Gotlib 1999; Zahn-Waxler et al. 1990) and may create dysfunctions in the parent–child relationship (Nelson et al. 2003). When children display challenging behavior, parents are more likely to lose confidence in their parenting abilities, which in turn can maintain or intensify feelings of depression (Cutrona and Trouman 1986; Nelson et al. 2003). Completing the cycle, depression continues to be associated with less effective parenting strategies and coercive interactions that aggravate both the parent’s depression and child’s disruptive behavior (Goodman and Gotlib 1999; Patterson 1982). Whereas this process has not been outlined explicitly in the extant literature, Coyne’s interpersonal model of depression provides a basis for parent–child bidirectional effects by describing how depressed adults elicit negative reactions from others that intensify the depressed adults’ unhappiness and negativity in a cycle of mutual distress (Coyne et al. 1987). Moreover, Patterson’s coercive cycle, which is grounded in both theoretical and empirical work, is the analogous process in parenting and many of the concepts in Patterson’s model are applicable to this situation.
Timing of Effects
Whereas the extant literature provides both theoretical and limited empirical support for a reciprocal effects model between maternal depression and child disruptive behavior, a key question remains about the timing of these effects. Specifically, it is unclear if there are developmental periods when bidirectional or unidirectional relations are more evident than during other periods. From the perspective of physical maturation and the changes in children’s social environment, there are reasons to believe that two transition points would be particularly stressful for children and parents. First, from the perspectives of both physical and social maturation, the transition to adolescence is a time where hormonal changes and social expectations are high, as youth face multiple challenges in social domains (e.g., social roles, vocational decisions, peer influences) and neurobehavioral changes associated with puberty (Dahl 2004). Although the majority of adolescents report having happy, pleasant relations with their parents (Rutter et al. 1976; Steinberg 2001), some research suggests that even normative parent–adolescent conflict can cause distress for parents, especially mothers (Steinberg and Steinberg 1994; Silverberg and Steinberg 1990).
Another critical developmental transition marked by changes in both social and academic domains is the transition to formal schooling at ages 5 to 6. This time period may encompass a period of vulnerability not typically emphasized in the extant literature. The transition to school, though marked by less pronounced physiological (Rimm-Kaufman and Pianta 2000) or cognitive (Flavell 1988; Nelson 1996) maturation, is a time of social transition for children. At formal school entry, many children transition from spending most of their day with adults to spending an increasing amount of time with other children (Rimm-Kaufman and Pianta 2000). Even children who have received care from a non-parental caregiver prior to this transition (e.g., preschool, daycare) are vulnerable to experiencing problems (Rimm-Kaufman 2004). In kindergarten, there is a significant increase in the demands made on children’s social skills, work-related skills (including compliance to instructions and the ability to work independently), self-regulation, and academic readiness. One study using a large, national sample (N=3,595) found that based on teachers’ reports, almost half of children entering school experienced some difficulty in the transition to kindergarten (Rimm-Kaufman et al. 2000).
To date we know of only one study that has examined the effects of timing in reciprocal models of maternal depression and children’s behavior (Jaffee and Poulton 2006). When the authors examined child effects in a sample of 5 to 15 year olds, children’s anxious/depressed behavior predicted increases in mother’s subsequent internalizing symptoms when the children were ages of 5 and 7 years but not thereafter. Girls’ (but not boys’) antisocial behavior predicted increases in mothers’ internalizing symptoms throughout the time period examined. Although the authors hypothesized that the strongest effects of mother’s depression on her child would occur during periods of transition, they found that maternal depression predicted children’s subsequent anxious/depression symptoms at numerous time intervals (from children’s ages 5 to 7, 9 to 11, and 11 to 13). Finally, maternal effects on girls’ antisocial behavior were found throughout the period studied, whereas maternal effects on boys’ antisocial behavior were limited to the transition to middle childhood (boys’ ages 5 to 7). In this study, both child and maternal effects were consistently found when children were ages 5 and 7, which provides further evidence that the transition to school may be a time of vulnerability for families.
In summary, the extant literature provides theoretical models and some empirical support for reciprocal effects between maternal well-being and child problem behavior. Whereas reciprocal models have been tested with respect to parenting practices and child problem behavior, they have been applied less often to parental functioning. The current study applies a reciprocal effects model to explore the interplay between maternal depressive symptoms and child aggressive behavior during middle childhood (boys’ ages 5 to 10). We then apply the same methodology during the transition to adolescence and middle adolescence (boys’ ages 10 to 15) by examining the interplay between maternal depressive symptoms and youth antisocial behavior. For the middle childhood model, we chose to focus on more overt and reactive forms of child antisocial behavior, which are more normative during this period than during adolescence, particularly among boys (Keenan and Shaw 1997). In the age 10–15 model, we focused on more covert and proactive forms of antisocial behavior as the child factor because of the increasing frequency and distressing nature of these behaviors in adolescence (Loeber and Stouthamer-Loeber 1998). Whereas later antisocial behavior is often predicted by early aggression (Loeber et al. 1997), we believed it was important to examine these behaviors in two different models as a substantial number of children display high levels of only one of these behaviors during one period of development and not the other (Moffitt 1993; Nagin and Tremblay 1999).
In accord with previous research, we hypothesized that both parent and child effects would be present throughout the age periods being studied, as evidenced by good fitting models that depicted these relations. We further hypothesized that when specific paths were examined, both parent and child effects would be more prevalent during periods of physical and/or social transition, specifically the transition to early adolescence (ages 11 to 12) and the transition to school (ages 5 to 6). We tested these hypotheses by using a parallel processing model that allowed us to examine the overall fit of a reciprocal model of maternal depressive symptoms and childhood problem behavior and investigate the strength of these relations across time.
Method
Participants
Subjects were recruited from the Allegheny County Women, Infants and Children (WIC) program in the Pittsburgh Metropolitan area (Shaw et al. 1998). The sample was restricted to boys because of the larger study’s primary goal, to examine antecedents of antisocial behavior. Out of 421 families approached at WIC sites, 310 participated in the first assessment when the boys were 18 months old. At the time of recruitment, all families met the income requirements for WIC and had a child between 6 and 17 months of age. At the initial assessment, mothers ranged in age from 17 to 43 (M=28). Fifty-three percent of the sample was European American, 36% African American, 5% biracial, and 6% other (e.g., Hispanic, Asian). Based on the respondents’ reports, mean per capita family income was $241 per month ($2,892 per year), with a Hollingshead socioeconomic status score of 24.8, indicative of a working class sample. The retention rate was fairly high, with 291 families (93.9% of the original sample of 310) participating in at least one of the assessments from ages 10 and 15. Alternate caregivers (AC) were invited to participate in the assessments, beginning when the boys were age 5. The vast majority of alternate caregivers identified themselves as the child’s biological father (e.g., 81.2% at boys’ age 5; 75.0% at boys’ age 10). Other alternate caregivers included stepfathers, boyfriends of the mother, grandparents, and other relatives (aunts, uncles). In most cases (82.2%), the alternate caregiver was the same respondent at the assessments from ages 5 and 10. When the respondent changed, data from different reporters were used in the models.
Data from families were included in the analyses if they had at least one report of maternal depression and one report of child behavior. There were 284 families included in the middle childhood (boys’ ages 5–10) model with maternal reports of child aggressive behavior; 240 families in the model with AC-reported child aggressive behavior; and 270 families in the adolescent model. Families (n=4) were removed from the sample if any of their total Beck scores exceeded 39 points (i.e., if any of their scores were extreme outliers, which can bias structural models and reduce model fit). The subsample of families with AC data was not significantly different from the families with only maternal report when compared on maternal age (t=0.06, ns), maternal education (t=1.69, ns) or socioeconomic status (t=0.40, ns). Families who had AC data were significantly higher in family income than those who did not have AC data (t=2.18, p<0.05).
Procedures
For the purpose of this study, mothers and target children were seen either in the laboratory and/or home when the children were 5, 6, 8, 10, 11, 12, and 15 years old. Demographic variables, including income and both parents’ occupation and education, were collected at the beginning of each interview. Mothers completed the Beck Depression Inventory at all time points. Maternal and alternate caregiver reports of child behavior were obtained using the Child Behavior Checklist when the boys were 5, 6, 8, and 10 years old. Youth completed the Self Report of Delinquency when they were 10, 11, 12, and 15 years old.
Measures
Beck Depression Inventory
Mothers completed the Beck Depression Inventory (BDI) (Beck et al. 1961), a widely used measure of depressive states, at all assessments. This 21-item measure is appropriate for measuring intensity and detecting depressive symptoms in both psychiatric and normal populations. For each item, respondents are asked to read four statements that correspond to the clinical presentation of depression and that vary in intensity (no symptomatology to severe symptomatology), and then select the statement that best describes how they have been feeling over the past 6 months. Scores for each statement are summed to obtain a total score. Reliability and external validity of the BDI are high (Beck et al. 1988). In this sample, the internal consistency of the BDI ranged from 0.85 to 0.91, with an average Cronbach’s alpha of 0.88 across all seven time points. The overall average total BDI score for all individuals in this sample across all time points was 7.03. The means and standard deviations of the BDI total score at each interview are presented in Table 1. This table also includes the percentage of respondents with scores of 10 or higher, which is considered the cut-off for mild to moderate depression (Beck et al. 1988). As can be seen in Table 1, a significant minority of mothers reported elevated rates of symptoms when their sons were age 5 (29.5%), with this rate generally showing a gradual decline with children’s age (i.e., 22.6% at boys’ age 15).
Table 1.
Descriptive statistics Clinical range was defined as 90th percentile or higher for the aggression subscale on the CBCL and total BDI scores of 10 or higher.
| M | SD | Total N | % clinical range | |
|---|---|---|---|---|
| Maternal depressive symptoms, age 5 | 7.79 | 6.62 | 261 | 29.5 |
| Maternal depressive symptoms, age 6 | 6.73 | 6.13 | 241 | 25.7 |
| Maternal depressive symptoms, age 8 | 6.41 | 6.70 | 233 | 20.6 |
| Maternal depressive symptoms, age 10 | 6.34 | 5.83 | 227 | 24.7 |
| Maternal depressive symptoms, age 11 | 6.80 | 6.57 | 221 | 24.4 |
| Maternal depressive symptoms, age 12 | 6.59 | 6.24 | 216 | 24.1 |
| Maternal depressive symptoms, age 15 | 6.61 | 7.62 | 212 | 22.6 |
| Aggressive behavior, age 5 maternal report | 11.43 | 6.48 | 259 | 21.6 |
| Aggressive behavior, age 6 maternal report | 10.82 | 6.86 | 247 | 23.5 |
| Aggressive behavior, age 8 maternal report | 8.28 | 6.18 | 235 | 11.5 |
| Aggressive behavior, age 10 maternal report | 8.08 | 6.23 | 218 | 12.8 |
| Aggressive behavior, age 5 AC report | 11.10 | 6.84 | 183 | 14.1 |
| Aggressive behavior, age 6 AC report | 8.82 | 5.84 | 150 | 12.0 |
| Aggressive behavior, age 8 AC report | 9.06 | 7.80 | 127 | 15.7 |
| Aggressive behavior, age 10 AC report | 9.17 | 7.00 | 136 | 18.4 |
| Antisocial behavior, age 10 | 3.33 | 43.63 | 226 | |
| Antisocial behavior, age 11 | 3.38 | 3.54 | 226 | |
| Antisocial behavior, age 12 | 3.49 | 3.89 | 221 | |
| Antisocial behavior, age 15 | 5.02 | 5.71 | 212 |
Clinical range was defined as 90th percentile or higher for the aggression subscale on the CBCL and total BDI scores of 10 or higher.
Child Behavior Checklist
Child disruptive behavior was measured at ages 5, 6, 8, and 10 using the Child Behavior Checklist (CBCL) (Achenbach 1991). The CBCL is a widely used measure of childhood adjustment problems. Parents use a three-point scale to report on the occurrence and frequency of a number of problem behaviors. For purposes of the present study, we selected the 20-item Aggressive Behavior scale because of its focus on overt and primarily reactive, disruptive behavior, which is common for this age group. Items include arguing, destroying one’s own and others’ belongings, being disobedient, fighting with other children, and threatening others. The Aggressive Behavior scale has good psychometric properties (Achenbach 1991) and has been widely used in research on developmental psychopathology. In this sample, the percentage of children scoring at or above the borderline clinical range (i.e., 90th percentile) on the Aggressive Behavior scale ranged from 11.5% at age 8 to 23.5% at age 6 when maternal report was used and 12.0% at age 6 to 18.4% at age 10 for AC report (see Table 1). Cronbach alphas for the Aggressive Behavior scale ranged from.87 to.90 for maternal report and.87 to.93 for AC report. Means and standard deviations for both maternal- and AC-reported aggressive behavior are presented in Table 1.
Self-Reported Delinquency
Youth completed one of two versions of the Self-Reported Delinquency (SRD) measure at ages 10, 11, 12, and 15 (Elliot et al. 1985). The version for younger youth was administered at ages 10, 11, and 12, and the older version was administered at age 15. The SRD is a questionnaire that assesses the context and frequency of offending and examines overt, covert, destructive, and nondestructive offenses. Youth use a three-point scale to report on the occurrence and frequency of a number of delinquent behaviors. Self-reported measures of delinquency have been shown to have strong psychometric properties, with test–retest reliabilities ranging from 0.75 to 0.98 and internal consistency alphas from 0.65 to 0.92 (Krueger et al. 1994). The SRD is considered a highly respected self-report assessment of delinquency with good psychometric properties. Because the version of the SRD for older youth has more items, for this analysis the 33 items that were common across versions of the SRD were selected, with scores on each item summed to form a total self-reported delinquency score (see Appendix A for list of items used). In this sample, the reliability of these 33 items ranged from 0.79 at age 10 to 0.87 at age 15.
Missing Data
We examined patterns of missing data before addressing substantive research questions. This examination revealed that between 8% to 24% of cases were missing maternal depression data or maternal reports of boys’ aggressive behavior at any study wave. Between 17% and 22% of boys did not provide self reports on their antisocial behavior at ages 10 to 15. There were 240 families who had at least one AC report between boys’ ages 5 and 10 (86% of the sample). Consequently, AC models were estimated using this subsample of families. From 23% to 47% of AC reports were missing at any wave between boys’ ages 5 and 10.
For each of these variables, we conducted analyses to see if the variable’s missing status was associated with any other study variables. Of the 84 tests performed, just 6 revealed significant associations (7%), suggesting that AC data were missing at random (MAR), and that maternal depression, mothers’ reports of boys’ aggressive behavior, and boys’ reports of antisocial behavior were not MAR. As these few associations were small in magnitude, we interpreted them as largely being due to chance. Consequently, we employed full information maximum likelihood (FIML) when fitting models, which estimates missing values using all available data and can be used with data that are not MAR (for more information, see Enders 2001). FIML-based parameter estimates provide less biased information than ad hoc procedures such as listwise deletion, pairwise deletion, or imputation (Schafer 1997).
Analysis Plan
The overarching goal of the current study was to increase understanding of how changes in boys’ disruptive and antisocial behavior were associated with changes in maternal depression over time and conversely, how changes in maternal depression were related to changes in disruptive and antisocial behavior. To fully understand this phenomenon, we conducted five distinct phases of latent growth curve modeling (LGCM) and structural equation modeling (SEM).
Procedurally, latent growth modeling applied within a SEM framework involves adapting confirmatory factor analysis (CFA) while accounting for the mean structure. Individuals’ scores on a variable assessed repeatedly over time are used to construct latent variables for initial status and linear growth rate, which is also known as the slope (for more detail on SEM-based latent growth modeling, see Bollen and Curran 2006). Both of these latent constructs are defined by all repeated measures of the variable. Loadings of the intercept term are constrained to be equal over time, and loadings for the linear growth component are constrained to correspond to measurement timing (e.g., “0” for the maternal depression score at the child’s birth, “1” for her depression at child’s age 1, “2” for her depression at child’s age 2, and so forth). This forces information about the variables’ means into the latent constructs. Consequently, an average value for each latent construct is estimated (e.g., mean values for initial status and the rate of linear growth, known as the fixed effects), as are variances of the intercept and slope, their covariance/correlation, and the residual variances of the repeated measure (typically constrained to be equal over time; collectively, these variance components are referred to as random effects).
Following preliminary analysis that examined the correlations between all variables (see Table 2 and Table 3), we first explored whether there was change in maternal depression and boys’ aggressive behavior over time. This involved testing two LGCMs, which was an obligatory precursor to examining more complex growth models. We estimated one unconditional LGCM (i.e., a growth model without any predictors) for maternal depression between boys’ ages 5 and 10 years, and one for mother-reported boys’ aggressive behavior problems from boys’ ages 5 to 10 years. For these models, time was centered at boys’ age 5.
Table 2.
Study variable correlations
| Variable | Maternal depression | Aggression, PC report | Aggression, AC report | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| 1 | Dep 5 years | |||||||||||
| 2 | Dep 6 years | 0.66** | ||||||||||
| 3 | Dep 8 years | 0.61** | 0.68** | |||||||||
| 4 | Dep 10 years | 0.54** | 0.56** | 0.61** | ||||||||
| 5 | Mat Agg 5 years | 0.37** | 0.35** | 0.31** | 0.28** | |||||||
| 6 | Mat Agg 6 years | 0.41** | 0.40** | 0.33** | 0.29** | 0.71** | ||||||
| 7 | Mat Agg 8 years | 0.26** | 0.35** | 0.36** | 0.26** | 0.61** | 0.65** | |||||
| 8 | Mat Agg 10 years | 0.19** | 0.24** | 0.23** | 0.31** | 0.39** | 0.51** | 0.63** | ||||
| 9 | AC Agg 5 years | 0.12 | 0.23** | 0.16* | 0.12 | 0.40** | 0.44** | 0.41** | 0.43** | |||
| 10 | AC Agg 6 years | 0.18* | 0.25** | 0.16 | 0.16 | 0.41** | 0.54** | 0.44** | 0.35** | 0.57** | ||
| 11 | AC Agg 8 years | 0.22* | 0.23* | 0.11 | 0.21* | 0.51** | 0.59** | 0.62** | 0.60** | 0.60** | 0.56** | |
| 12 | AC Agg 10 years | 0.31** | 0.264** | 0.18* | 0.20* | 0.20* | 0.39** | 0.40** | 0.57** | 0.45** | 0.56** | 0.59** |
p<0.05
p<0.01
Table 3.
Study variable correlations
| Variable | Maternal depression | Boys’ ASB | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| 1 | Dep 10 years | |||||||
| 2 | Dep 11 years | 0.64** | ||||||
| 3 | Dep 12 years | 0.61** | 0.63** | |||||
| 4 | Dep 15 years | 0.52** | 0.51** | 0.56** | ||||
| 5 | ASB 10 years | 0.11 | 0.07 | 0.17* | 0.05 | |||
| 6 | ASB 11 years | 0.10 | 0.14* | 0.23** | 0.05 | 0.60** | ||
| 7 | ASB 12 years | 0.19** | 0.22** | 0.20** | 0.18** | 0.62** | 0.62** | |
| 8 | ASB 15 years | 0.20** | 0.17* | 0.26** | 0.19** | 0.26** | 0.28** | 0.38** |
p<0.05
p<0.01
Second, following the estimation of separate unconditional models for maternal depression and sons’ aggressive behavior, we also investigated whether or how changes in each were associated with the other over time by estimating parallel processing models (Muthén 2002; Singer and Willett 2003). This type of modeling permits researchers to understand whether two correlated behaviors develop without influencing each other over time (e.g., whether they are parallel processes) or whether they develop conditionally or interdependently with each other (e.g., whether change in one behavior can be attributed to changes in the other behavior). We estimated two parallel processing models, one using maternal reports of child aggressive behavior and the second model using AC reports of child aggressive behavior. Third, we also wanted to reveal when sons’ aggressive behavior and mothers’ depression were related to one another over time. As this question could not be addressed through latent growth modeling, this involved estimating an autoregressive path model with cross-lagged associations between maternal depression and boys’ aggressive behavior. We controlled for the stability of each construct by simultaneously regressing temporally-later scores on earlier ones (e.g., maternal depressive symptoms at boys’ age 10 were regressed upon depressive symptoms at boys’ age 8). Paths from boys’ prior aggressive behavior were estimated to mothers’ depressive symptoms at each timepoint, and vice versa. Significant cross-lagged paths indicate the timing of child effects on maternal symptoms, and maternal effects on child aggressive behavior.
Fourth, these first three steps were repeated with AC reports of boys’ aggressive behavior problems and mothers’ depression scores from boys’ ages 5 to 10. Separate unconditional models of boys’ aggressive behavior and maternal depression were estimated in this subsample prior to fitting the parallel process model. As in the primary analyses, time was centered at boys’ age 5. These were followed by the examination of cross-lagged associations in an autoregressive path model.
Finally, these first three steps were repeated with boys’ reported antisocial behavior and mothers’ depression scores from boys’ ages 10 to 15. Separate unconditional models were estimated prior to the parallel process model. For all of the replication analyses, time was centered at boy’s age 10. These were followed by the examination of cross-lagged associations via the autoregressive path model.
LGCM and SEM analyses were conducted in M-Plus version 4.0 (Muthén and Muthén 2004). Nested LGCMs were compared using Akaike Information Criterion (AIC) and sample-size adjusted Bayesian Information Criterion (BIC) values. Smaller BIC and AIC values indicate better fit (Singer and Willett 2003). Linear models were retained when quadratic models’ quadratic variances were not significant, regardless of fit indices. The minimal requirements for adequate SEM model fit included RMSEA and SRMR values smaller than 0.10, and CFI values larger than 0.90 (Kline 1998). The chi-square statistic is also reported for all models.
Results
Fit statistics for all unconditional LGCMs are included in Table 4, and fixed effects, variances, and parameter correlations are included in Table 5. Only the best-fitting models are described here to conserve space.
Table 4.
Unconditional latent growth model fit statistics
| Model | (df) χ2 fit | CFI | RMSEA (90% CI) | SRMR | BIC | AIC |
|---|---|---|---|---|---|---|
| Maternal depression 6–10 years (full sample) | ||||||
| Linear | (8) 19.25* | 0.97 | 0.07 (0.03–0.11) | 0.07 | 5,894.46 | 5,891.68 |
| Quadratic | (4) 7.61 | 0.99 | 0.06 (0.00–0.12) | 0.04 | 5,892.68 | 5,888.04 |
| Boys’ aggression 6–10 years (maternal report) | ||||||
| Linear | (8) 25.73** | 0.96 | 0.09 (0.05–0.13) | 0.08 | 5,914.21 | 5,911.43 |
| Quadratic | (1) 3.99* | 0.99 | 0.10 (0.01–0.22) | 0.02 | 5,909.72 | 5,903.69 |
| Maternal depression 6–10 years (limited sample) | ||||||
| Linear | (8) 17.37* | 0.97 | 0.07 (0.02–0.12) | 0.08 | 5,223.18 | 5,221.34 |
| Quadratic | (4) 7.22 | 0.06 (0.00–0.13) | 0.05 | 5,222.25 | 5,219.19 | |
| Boys’ aggression 6–10 years (AC report) | ||||||
| Linear | (5) 20.18** | 0.90 | 0.11 (0.06–0.17) | 0.09 | 3,855.73 | 3,852.94 |
| Quadratic | (4) 16.74** | 0.12 (0.06–0.17) | 0.11 | 3,857.61 | 3,851.50 | |
| Maternal depression 10–15 years | ||||||
| Linear | (8) 15.95* | 0.98 | 0.06 (0.01–0.10) | 0.06 | 5,661.15 | 5,658.58 |
| Quadratic | (4) 5.35 | 0.04 (0.00–0.10) | 0.04 | 5,660.26 | 5,655.98 | |
| Boys’ ASB 10–15 years | ||||||
| Linear | (8) 49.67 | 0.84 | 0.14 (0.10–0.18) | 0.10 | 4,957.10 | 4,954.51 |
| Quadratic | (4) 2.77 | 0.00 (0.00–0.08) | 0.03 | 4,919.92 | 4,915.61 | |
p<0.05
p<0.01
p<0.001
Table 5.
Unconditional models’ fixed effects, variances, and parameter correlations
| Model | Fixed effects | Random effects | |||
|---|---|---|---|---|---|
| Variances | Correlation | ||||
| Intercept | Linear | rI, L | |||
| Maternal report 5–10 years | |||||
| Maternal depression | 7.28*** | −0.24** | 28.60*** | 0.27* | −0.46* |
| Boys’ aggression | 11.23*** | −0.74*** | 33.55*** | 0.89*** | −0.52*** |
| AC report 5–10 years | |||||
| Maternal depression LS | 7.09*** | −0.21** | 27.66*** | 0.30* | −0.42* |
| Boys’ aggression | 10.31*** | −0.30** | 24.70*** | 0.42 | −0.01 |
| Ages 10–15 | |||||
| Maternal depression | 6.56*** | 0.07 | 22.69*** | 0.66*** | −0.06 |
| Boys’ ASB | 3.07*** | 0.38*** | 8.71*** | 0.99*** | −0.31** |
LS limited sample. Subscripts refer to model parameters: I intercept, L Linear
p<0.05
p<0.01
p<0.001
Childhood Models: Maternal Report
Unconditional Maternal Depression
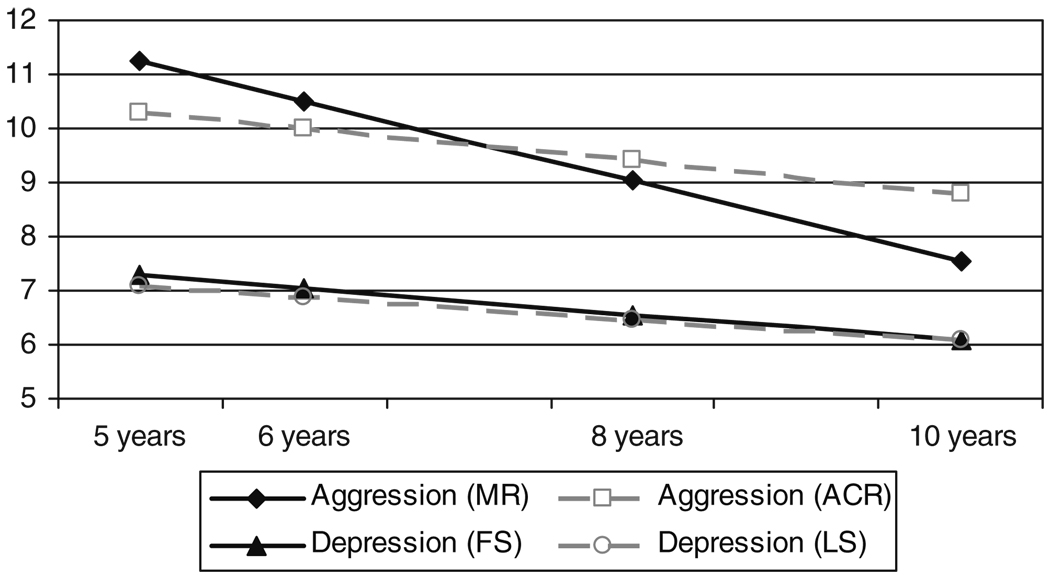
Linear and quadratic unconditional models were estimated to chart the course of maternal depression from boys’ ages 5 to 10 years. The quadratic unconditional model provided a better fit to the data than the linear model (see Table 4); however, the slope and quadratic variances generated by the quadratic model were not significantly different from zero. Average initial status and linear growth in maternal depression were significantly different from zero (see Table 5), so the linear model was selected. Overall, mothers initially reported moderate levels of depression, which declined very gradually to boy’s age 10 (see Fig. 1). The intercept and linear growth terms were negatively correlated, which suggests that a high intercept was associated with slower declines over time.
Fig 1.
Unconditional latent growth in maternal depression and boys’ aggression from boys’ ages 5 to 10 years. Plotted values were estimated values derived from the unconditional growth models. MR maternal report, ACR alternate caregiver report, FS full sample, LS limited sample
Unconditional Boys’ Aggressive Behavior
Linear and quadratic models were estimated to examine growth in mothers’ perceptions of boys’ aggressive behavior from ages 5 to 10 years. An unconditional linear model provided the best fit to growth in maternal-reported boys’ aggressive behavior (see Table 4); as with maternal depression, the slightly better fit provided by the quadratic model was negated by its non-significant linear and quadratic variances. On average, boys followed gradual declines in aggressive behavior from ages 5 to 10 (see Fig. 1). Intercept was negatively correlated with linear growth (see Table 5), which suggests that high initial levels of aggressive behavior were associated with slower declines over time.
Parallel Processing Model
To determine how initial status and growth were related in maternal depression and maternal perception of sons’ aggressive behavior, we estimated a parallel processing model. In this model, the growth parameters of the linear aggressive behavior and maternal depression models were estimated simultaneously and allowed to correlate. This model adequately fit the data, χ2 fit (28)=64.68, p<0.001, RMSEA=0.07, 90% CI=0.05–0.09, SRMR=0.06, CFI=0.96, BIC=11,747.51, AIC=11,740.09. There were several correlations between growth components describing maternal depression and maternal-reported boys’ aggressive behavior, in addition to the correlations already described in each unconditional model. Higher levels of maternal depression at boys’ age 5 were associated with a higher intercept (r=0.57, p<0.001) and linear growth (r=−0.45, p<0.01) in maternal perception of boys’ aggressive behavior. High levels of maternal depressive symptoms at boys’ age 5 were indicative of high levels of maternal-reported aggressive behavior at age 5, and slower declines in boys’ aggressive behavior between ages 5 to 10. Likewise, linear growth in maternal depression was positively correlated with linear growth in maternal-reported aggressive behavior (r=0.75, p<0.001), indicating that maternal reports of depression and sons’ aggressive behavior declined at similar speeds. In all, these correlations suggest that the rates of decline for maternal depression and perception of sons’ aggressive behavior are correlated, such that reductions in maternal depression correspond to declines in her perceptions of her sons’ aggressive behavior. Significant variance remained in maternal depression intercepts and slopes after accounting for intercept and slope in maternal-reported aggressive behavior; like-wise, significant variance also remained in boys’ aggressive behavior after accounting for maternal depression ( both ps<0.001).
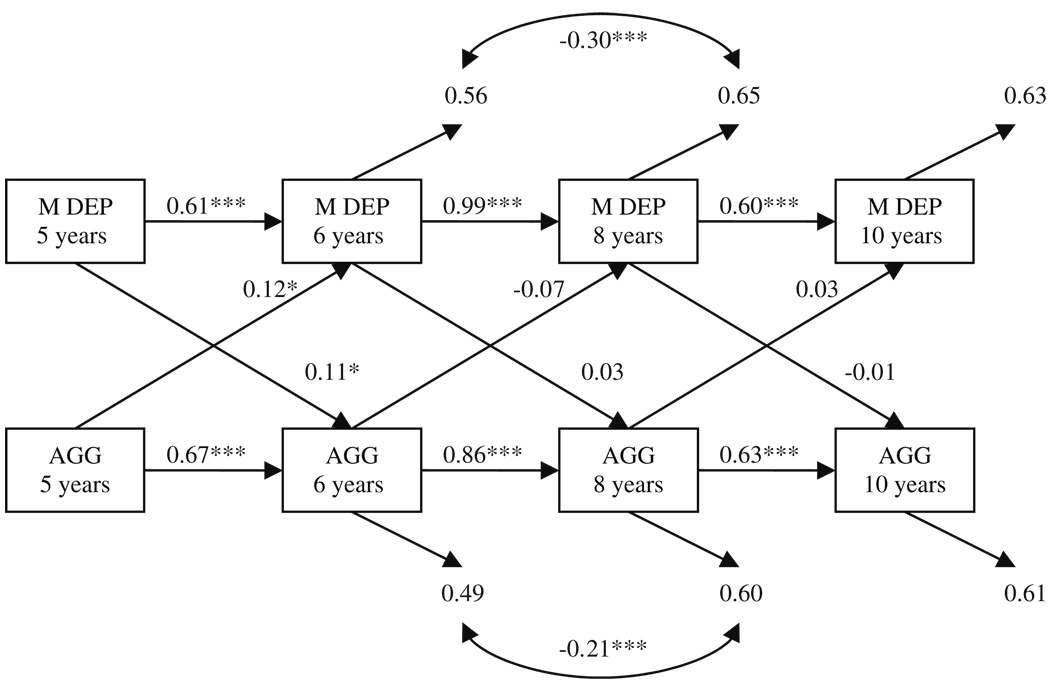
Autoregressive Model
An autoregressive path model was fitted to examine the timing of child effects on maternal depression and of maternal effects on her sons’ aggressive behavior. In this model, we examined the cross-lagged associations between maternal depression and maternal-reported child aggressive behavior while controlling for the stability of each construct and for correlations within each timepoint. Model fit was initially not entirely adequate, χ2 fit (12)=79.91, p<0.001, RMSEA=0.14, 90% CI=0.11–0.17, SRMR=0.06, CFI=0.93, but significantly improved through the addition of two residual correlations. This indicates that other underlying causes of depression or aggressive behavior are shared at boys’ ages 6 and 8, and are not represented by this model, χ2 fit (10)=33.00, p<0.001, Δχ2 fit (2)=46.91, p<0.001, RMSEA=0.09, 90% CI=0.06–0.13, SRMR=0.04, CFI=0.97 (see Fig. 2).
Fig 2.
Mother-report autoregressive model (boys’ ages 5 to 10 years). All coefficients are standardized. Within-timepoint correlations were estimated but omitted from the figure (respectively, rs were 0.38, 0.08, 0.08, and 0.15; all ps<0.05). *p<0.05, **p<0.01, ***p<0.001
Maternal depression was stable from sons’ ages 5 to 10 years (β range=0.61–0.99), and the same was also true of sons’ aggressive behavior during the same time period (β range=0.63–0.86). One of three paths from maternal depression to boys’ subsequent aggressive behavior was significant. Mothers with higher levels of depression when their boys were age 5 reported higher levels of boys’ aggressive behavior at age 6. There was also evidence of a child effect on maternal depression during the same time period, such that higher levels of boys’ age 5 aggressive behavior predicted higher levels of maternal depression when the boys were 6.
Replication with Alternate Caregiver Reports of Boys’ Aggressive Behavior
Unconditional Maternal Depression
Unconditional models of maternal depression were re-estimated in the subsample with AC data. This model was essentially identical to the unconditional model estimated in the full sample (see Table 4). The quadratic model provided a slightly better fit to the data, but the linear and quadratic slope variance components were not significantly different from zero. Consequently, the linear model was retained. Average initial status and linear growth in maternal depression were significantly different from zero (see Table 5). Overall, mothers initially reported moderate levels of depression, which declined very gradually to boys’ age 10 (see Fig. 1). The intercept and linear growth terms were negatively correlated, which suggests that a high intercept was associated with slower declines over time.
Unconditional Boys’ Aggressive Behavior
Linear and quadratic models were estimated to examine growth in ACs’ perceptions of boys’ aggressive behaviors from ages 5 to 10 years. An unconditional linear model provided the best fit to growth in AC-reported boys’ aggressive behavior (see Table 4). On average, boys initially had rather high levels of AC-reported aggressive behavior at age 5, followed by gradual declines to age 10 (see Fig. 1). Intercept was not correlated with linear growth (see Table 5), which suggests that declines in AC-reported aggressive behavior over time were not associated with boys’ starting points.
Parallel Processing Model
To determine how initial status and growth were related in maternal depression and AC-reported boys’ aggressive behavior, we estimated a parallel processing model. In this model, the growth parameters of the linear aggressive behavior and maternal depression models were estimated simultaneously and allowed to correlate. This model adequately fit the data, χ2 fit (25)=47.62, p<0.01, RMSEA=0.06, 90% CI=0.03–0.09, SRMR=0.07, CFI= 0.96, BIC=9,071.06, AIC=9,065.15. Higher levels of maternal depression at boys’ age 5 were associated only with a higher intercept (r=0.30, p<0.01) of age 5 AC-reported boys’ aggressive behavior. Significant variance remained in maternal depression intercepts and slopes after accounting for intercept and slope in AC-reported aggressive behavior. Significant variance also remained in boys’ initial status but not slope in AC-reported aggressive behavior after accounting for maternal depression .
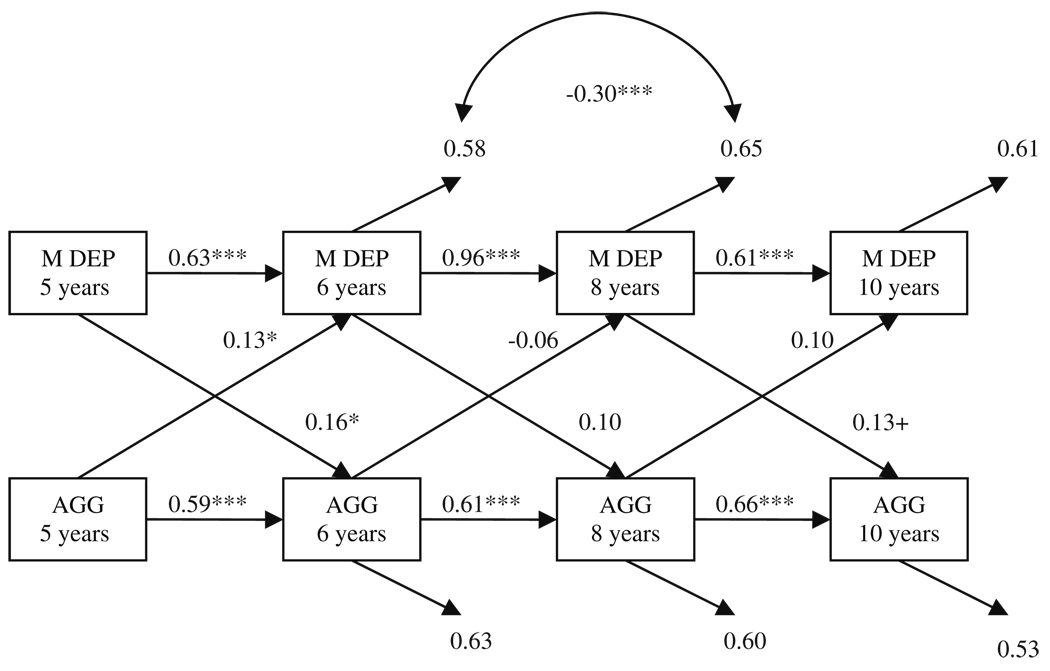
Autoregressive Model
An autoregressive path model was fitted to examine the timing of child effects on maternal depression and of maternal effects on AC-reported boys’ aggressive behavior. In this model, we examined the cross-lagged associations between maternal depression and child aggressive behavior while controlling for the stability of each construct. No within-timepoint correlations were estimated. Model fit was not entirely adequate, χ2 fit (16)=63.67, p<0.001, RMSEA=0.11, 90% CI=0.08–0.14, SRMR=0.08, CFI =0.91, but significantly improved through the addition of one residual correlation. This indicates that other underlying causes of depression are shared at boys’ ages 6 and 8, and are not represented by this model, χ2 fit (15)= 41.95, p<0.001, Δχ2 fit (1)=21.72, p<0.001, RMSEA=0.09, 90% CI=0.06–0.12, SRMR=0.07, CFI=0.95 (see Fig. 3).
Fig 3.
Alternate caregiver-report autoregressive model (boys’ ages 5 to 10 years). All coefficients are standardized. Within-timepoint correlations were constrained to zero. p<0.10, *p<0.05, **p<0.01, ***p<0.001
Maternal depression was stable from sons’ ages 5 to 10 years (β range=0.61–0.96), and the same was also true of AC-reported sons’ aggressive behavior during the same time period (β range=0.59–0.66). One of three paths from maternal depression to boys’ subsequent AC-reported aggressive behavior was significant. Higher levels of maternal depression when boys were 5 were significantly related to higher levels of AC-reported aggressive behavior at boys’ age 6 years. There was also evidence of a trend-level association; higher levels of maternal depression when boys were 8 were indicative of higher levels of AC-reported, age 10 aggressive behavior. Finally, one child effect on maternal depression was observed, such that higher levels of AC-reported aggressive behavior at age 5 were predictive of higher levels of maternal depression when boys were 6.
Replication in Adolescence
Unconditional Maternal Depression
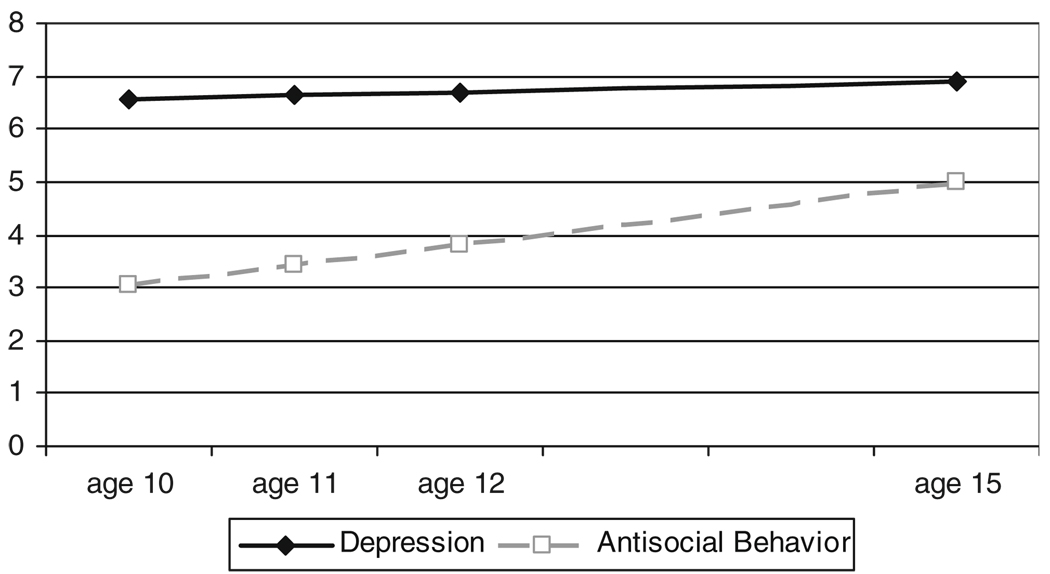
The course of maternal depression during boys’ adolescence was examined in a linear unconditional model, which provided the best fit to the data with significant growth variances (see Table 4). The average intercept in maternal depression at boys’ age 10 was significantly different from zero (see Table 5). The average slope was in a positive direction but was not significantly different from zero, and there was significant individual variability in intercepts and slopes (see Table 5). This suggests that mothers’ depression was stable from boys’ ages 10 to 15 years (see Fig. 4).
Fig 4.
Unconditional latent growth in maternal depression and boys’ antisocial behavior from boys’ ages 10 to 15 years. Plotted values were estimated values derived from the unconditional growth models
Unconditional Boys’ Antisocial Behavior
A linear unconditional model provided the best fit to the boys’ reports of antisocial behavior (ASB) in early adolescence (see Table 4). On average, initial status and slope of ASB at age 10 were significantly different from zero (see Table 5). Boys’ average initial ASB was low and increased steadily until age 15 (see Fig. 4). High levels of initial ASB were predictive of slower growth between ages 10 and 15.
Parallel Processing Model
We replicated the parallel processing model with the adolescent data waves to examine how initial status and growth in maternal depression and sons’ reported ASB were associated in early to mid-adolescence. In this model, the growth parameters of the linear ASB model and the linear maternal depression model were modeled simultaneously and allowed to correlate. This model adequately fit the data, χ2 fit (28)=76.94, p<0.001, RMSEA=0.08, 90% CI=0.06–0.10, SRMR=0.07, CFI=0.92, BIC=10,608.16, AIC=10,601.26. Unlike the childhood model, the intercept in maternal depression was only associated with the intercept in ASB (r=0.22, p<0.05). Higher levels of initial maternal depression were associated with higher levels of initial ASB. High initial levels of ASB remained negatively correlated with growth (r=0.31, p<0.01). No other model parameters were correlated. Significant variance remained in maternal depression intercepts and slopes (;both ps<0.001) after accounting for boys’ ASB. Significant variance also remained in boys’ intercepts and slopes of self-reported ASB after accounting for maternal depression (;both ps<0.001).
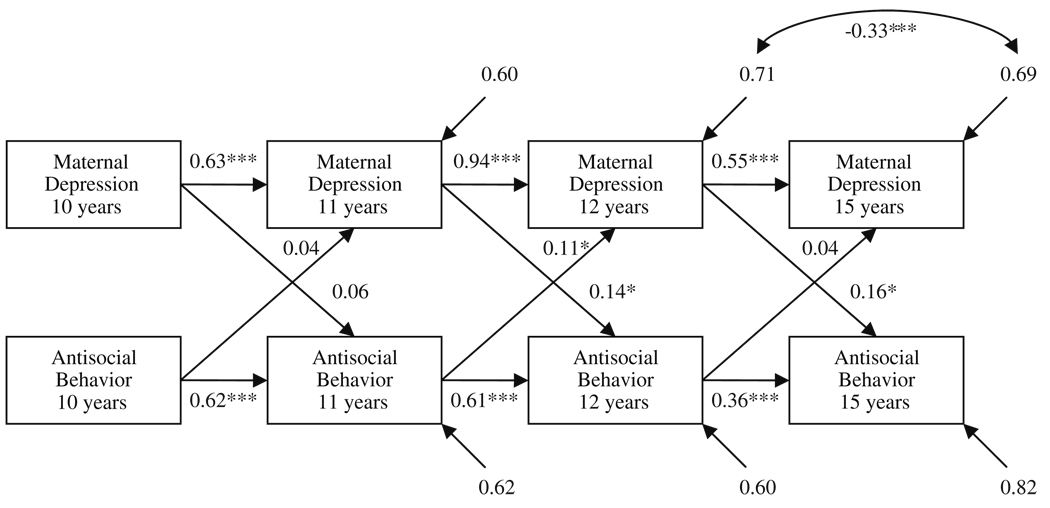
Autoregressive Model
We also replicated the autoregressive model to further examine the timing of effects. Within-timepoint correlations were constrained to zero. Fit of this model approached acceptability, χ2 fit (16)=89.71, p<0.001, RMSEA=0.13, 90% CI=0.11–0.16, SRMR=0.08, CFI=0.88, and improved by including one residual correlation. This indicates that other underlying causes of depression are shared at boys’ ages 12 and 15, and are not represented by this model, χ2 fit (15)=65.19, p<0.001, Δχ2 fit (1)=24.00, p<0.001, RMSEA=0.11, 90% CI=0.08–0.14, SRMR=0.07, CFI=0.92 (see Fig. 5). Boys’ ASB (β range=0.36–0.62) and maternal depression (β range=0.63–0.94) showed moderate stability from boys’ ages 10 to 15. Two paths from maternal depression to boys’ reported ASB were significant, indicating that higher levels of maternal depression at boys’ ages 11 and 12 were associated with higher levels of boys’ ASB at ages 12 and 15, respectively. In keeping with the prior model, there was evidence of child effects on maternal depression. Higher levels of boys’ ASB at age 11 were indicative of higher levels of maternal depression when boys were 12.
Fig 5.
Autoregressive model (replication from boys’ ages 10 to 15 years). All coefficients are standardized. Within-timepoint correlations were constrained to zero. *p<0.05, **p<0.01, ***p<0.001
Discussion
This study tested a transactional model of parent–child effects to explore reciprocal relations between child disruptive and antisocial behaviors, and maternal depressive symptoms. We examined a parallel processing model and cross-lagged associations to analyze the interrelations among maternal depression and boys’ disruptive and antisocial behavior (as reported by mother, an alternate caregiver, and youth), specifically looking for the presence and the timing of these effects. Overall model fit of the parallel processing models for both age periods suggests the presence of reciprocal effects between parent and child. When we examined the autoregressive paths to look at the timing of effects, we found significant parent and child effects from boys’ ages 5 to 6 in the middle childhood middle using both maternal and AC report of child aggressive behavior. The adolescent model found consistent effects from maternal depression to youth-reported ASB (i.e., two out of three paths significant), and some evidence for boys’ ASB being related to later levels of maternal depression (i.e., one out of three paths significant, boys’ ages 11 to 12).
A methodological strength of this study was the use of different informants to report on maternal depression and child disruptive problems. In middle childhood, the pattern of child and parent effects found using maternal report of aggressive behavior was corroborated using AC reports. We found that both models fit the data well and showed the strongest parent and child effects from ages 5 to 6. In the adolescent model, we used youth reports of ASB. By using different informants, we were able to show that the reciprocal effects found in the middle childhood model were not simply attributable to cognitive distortions by the mother. Past research has suggested that depressed mothers are overly negative in their perception of their children’s behavior (Fergusson et al. 1993; Goodman and Gotlib 1999). As these negative, cognitive distortions about their children may increase the likelihood of elevated depression symptoms, it was therefore critical to corroborate our results with a second informant reporting on child disruptive problems.
Timing of Effects
Overall, our hypothesis that parent and child effects would occur more often during periods of physical and/or social transitions was supported by the data. In the middle childhood models, maternal depression was most strongly related to subsequent increases in child disruptive problems during the transition to school (boys’ ages 5 to 6). In the adolescent model, we found associations between maternal depression and boys’ ASB throughout this period of transition (from boys’ ages 11 to 12 and 12 to 15), despite the minimal degree of change in maternal depression during the adolescent period. Child effects were significant during the early part of this transition, when the boys were ages 11 to 12.
As mentioned previously, the transition to school may encompass a period of vulnerability not typically emphasized in the extant literature. In addition to being a critical social transition for children, a child’s formal school entry can also affect parents and families. There is a growing body of literature that advises the use of ecological approaches (including children, schools, and families) in understanding the transition to school (Petriwskyj et al. 2005; Tudge et al. 2003). Challenges during this time can be distressing for parents. For example, if a child exhibits behavioral difficulties during this transition, a parent may receive negative feedback about her child from school staff and other parents in the classroom. Moreover, parents may have to adjust to changing involvement in their children’s lives as they typically become less familiar with peers and adults their children spend most of their day with and have less control over their children’s activities (Pianta et al. 1999).
Whereas children typically adjust to this transition in adaptive ways, for a subset of children, the transition to school may serve as a catalyst for the initiation or maintenance of externalizing trajectories (Reid 1993; Silver et al. 2005). In some cases, exposure to the features of the classroom environment may introduce risk for children who did not show prior risk for behavioral problems (Silver et al. 2005). For children previously at-risk for behavior problems, the transition to school may expand their “domains of risk” (Reid 1993); adverse early school experiences, such as peer rejection, struggles with academic work, coercive interactions with school staff, and teacher-child conflict, provide additional risk factors that are associated with externalizing behaviors and could result in increased challenges at both home and school. Moreover, rates of teachers’ perceptions of problems during this transition were higher in schools that had a high minority composition and a greater percentage of low-income families. A substantial number of participants in our study would have attended these types of schools.
Issues Raised
While the parallel processing model demonstrates bidirectional effects across 1- to 2-year periods, the current results do not address the specific mechanisms by which symptoms of maternal depression and child disruptive behavior and ASB affect one another. Such mechanisms may be evident by examining moment-by-moment observations of parent–child behavior. A number of investigators have found support for the notion that associations between parental depression and child adjustment are mediated by parenting, specifically tendencies for depressed mothers to be negative, critical, unresponsive, helpless, and low on positivity towards offspring (Goodman and Gotlib 1999; Zahn-Waxler et al. 1990). More intensive examinations of this process also provide some support for this idea. For example, a recent study by Shaw et al. (2006b) explored mothers’ contingent responses to their children’s expression of emotions. They found that mothers with a history of childhood-onset depression (COD) showed less contingent responsivity to their child’s expression of sadness and distress than non-COD mothers. Additional research is needed to more intensively uncover the processes by which parent-to-child and child-to-parent effects affect child externalizing symptoms and maternal well-being, respectively.
Another question raised by these findings is whether there are other child behaviors or problems besides disruptive behavior that are related to increases in maternal depression. For example, the Jaffee and Poulton (2006) study found boys’ symptoms of anxiety and depression to be related to maternal internalizing symptoms, rather than disruptive problems. The current study was initiated in an attempt to better understand the development of ASB in at-risk boys, and thus is not ideal for investigating questions of comorbidity. Other unexplored child characteristics that may affect maternal well-being and warrant investigation include medical or pervasive developmental disorders (e.g., mental retardation, autism), and child academic and peer-related difficulties. Future studies should consider these and other child characteristics.
Limitations
There are a few significant methodological limitations to the study. First, participants were primarily low-income European and African American boys. Some research suggests that there are gender differences in how children are affected by maternal depression. For example, Leve et al. (2005) found that the association between maternal depressive symptoms and later outcomes varied by gender, with elevated maternal depressive symptoms uniquely predicting increases in internalizing symptoms for girls and increases in boy’s disruptive symptoms when boys’ impulsivity was low. Similarly, child effects on maternal depression may vary by gender. Steinberg (2001) found that in adolescence, parental distress from parent–child conflict is more intense for parents whose adolescent is the same sex. Jaffee and Poulton (2006) found that in middle childhood and early adolescence, girls’ ASB predicted increases in maternal depression but boys’ ASB did not. Thus, we recommend that future work in this area be conducted on boys and girls from diverse socioeconomic strata and ethnic backgrounds to replicate or disconfirm our results.
Finally, these results should be interpreted with caution, as the fit of path models just attained commonly-accepted standards. We prudently permitted correlations between concurrent variables’ residuals, which were identified via model modification indices. The presence of these correlations indicates that variables’ measurement errors are correlated (Loehlin 2004), or that an underlying common cause is not represented in the model (Kline 1998), such as maternal ASB (e.g., Kim-Cohen et al. 2006). The addition of multiple measurements and omitted causes may potentially reduce the magnitude of residual correlations and improve model fit. Additionally, the significant path coefficients in all autoregressive models were fairly small in magnitude, ranging from 0.11 to 0.16. This indicates that while each process in the models (i.e., maternal depression and the corresponding child behavior) contributes to the other in a meaningful way, the amount of variance and growth explained by these constructs alone is small.
Clinical Implications
The results of this study are consistent with the robust finding in the existing literature that higher levels of maternal depressive symptoms are associated with poor outcomes in children. This finding, coupled with the relatively high stability of maternal depressive symptoms, indicates the need for early identification and preventive interventions (Olds 2002; Shaw et al. 2006a). In addition, the significant effects of disruptive behavior on maternal depressive symptoms during the transitions to school (boys’ ages 5 to 6) and adolescence (boys’ ages 11 to 12), suggest that clinicians working with depressed mothers include an assessment of child behavior and its impact on maternal well being. The significant parent effect findings also suggest the need for clinicians working with children to reduce or prevent behavior problems to focus explicitly on factors such as caregiver mood and affect. Developers of child intervention programs may want to explicitly focus on maternal depression as a target of change, particularly procedures with a proven track record of success in reducing depressive symptomatology (e.g., cognitive behavior therapy, interpersonal therapy). At a broader level, the findings are consistent with an ecological approach to treat child- and parent-identified issues (Dishion and Stormshak 2006), in that change of context can address multiple family mental health problems that tend to be etiologically linked and clustered (e.g., maternal depression, child problem behavior). In this sense, a family-centered approach may be preferred for the treatment of common adult mental health problems, especially when factors such as depression are embedded within a relationship and/or family context (Shaw et al., submitted for publication).
In sum, these findings provide novel information about the reciprocal associations between child behavior and maternal depression. The use of parallel processing analysis allowed us to examine parent and child influences over short spans of time (e.g., on a year-to-year basis) and over the course of 10 years. The results shed new light on transactional processes in a sample of mothers who showed above average rates of depressive symptoms and boys who exhibited elevated rates of disruptive and antisocial behaviors throughout childhood and adolescence.
Acknowledgements
The research reported in this paper was supported by grants to Dr. Daniel Shaw from the National Institute of Mental Health (MH 46925, MH 50907, and MH 01666). We are grateful to the staff of the Pitt Mother & Child Project for their years of service and to our study families for making the research possible.
Appendix
SRD Items Used in Analysis
For each item, respondents report if they engaged in behavior, never, once or twice, or more often.
Cheated on school tests or assignments
Skipped school without an excuse
Sent home from school for bad behavior
On purpose broken or damaged or destroyed something belonging to your parents or other people in your family
On purpose broken or damaged or destroyed something belonging to a school
On purpose broken or damaged or destroyed other things that did not belong to you, not counting things that belong to your family or school
Written things or sprayed paint on walls or sidewalks or cars, where you were not supposed to be
Purposely set fire to a building, a car, or something or tried to do so
Stolen or tried to steal a bicycle or skateboard
Taken something from a store without paying for it
Taken some money at home that did not belong to you, like from your mother’s purse of from your parents’ dresser
Taken anything else at home that did not belong to you
Taken anything at school from the teacher or other kids that did not belong to you
Taken something out of somebody’s house or yard or garage that did not belong to you
Taken something from a car that did not belong to you
Gone or tried to go into a building to steal something
Avoided paying for things such as movies, bus, or subway rides or food
Snatched someone’s purpose or wallet or picked someone’s pocket
Hit a teacher or another grown-up at school
Hit other students or gotten into physical fights with them
Hit one of your parents
Hit your brother or sister or gotten into a physical fight with him/ her
Carried a hidden weapon other than a plain pocket knife
Thrown rocks or bottles at people
Secretly taken a sip from a glass or bottle of beer
Secretly taken a sip from a glass or bottle of wine
Secretly taken a sip from a glass or bottle of liquor
Secretly smoked a cigarette, smoked a pipe, or chewed tobacco
Smoked Marijuana
Sniffed glue
Gone into someone’s garden, backyard, house, or garage when you were not supposed to be there
Run away form home
Been loud, rowdy, or unruly in a public place so that people complained about it or got you in trouble
References
- Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Baker BL, Heller TL. Preschool children with externalizing behaviors: Experience of fathers and mothers. Journal of Abnormal Child Psychology. 1996;24:513–532. doi: 10.1007/BF01441572. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bell RQ. A reinterpretation of the direction of effects in studies of socialization. Psychological Review. 1968;75:81–95. doi: 10.1037/h0025583. [DOI] [PubMed] [Google Scholar]
- Bell RQ, Harper LV. Child effects on adults. Hillsdale, NJ: Lawrence Erlbaum; 1977. [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley-Interscience; 2006. [Google Scholar]
- Brown RT, Borden KA, Clingerman SR, Jenkins P. Depression in attention-deficit-disordered and normal children and their parents. Child Psychiatry and Human Development. 1988;18:119–132. doi: 10.1007/BF00709726. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Development and Psychopathology. 2000;12:467–488. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- Civic D, Holt VL. Maternal depressive symptoms and child behavior problems in a nationally representative normal birthweight sample. Maternal and Child Health Journal. 2000;4:215–221. doi: 10.1023/a:1026667720478. [DOI] [PubMed] [Google Scholar]
- Coyne J, Kahn J, Gotlib I. Depression. In: Jacob T, editor. Family interaction and psychopathology: Theories, methods, and findings. New York: Plenum Press; 1987. pp. 509–533. [Google Scholar]
- Cui M, Donnellan MB, Conger RD. Reciprocal influences between parents’ marital problems and adolescent internalizing and externalizing behavior. Developmental Psychology. 2007;43:1544–1552. doi: 10.1037/0012-1649.43.6.1544. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Trouman BR. Social support, infant temperament, and parenting self-efficacy: A mediational model of postpartum depression. Child Development. 1986;57:1507–1518. [PubMed] [Google Scholar]
- Dahl RE. Adolescent brain development: A period of vulnerabilities and opportunities. Keynote address. Annals of the New York Academy of Sciences. 2004;1021:1–22. doi: 10.1196/annals.1308.001. [DOI] [PubMed] [Google Scholar]
- Danforth JS, Barkley RA, Stokes TF. Observations of parent-child interactions with hyperactive children: Research and clinical implications. Clinical Psychology Review. 1991;11:703–727. [Google Scholar]
- DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders. 2001;3:325–334. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Patterson GR. Handbook of antisocial behavior. New York: Wiley; 1997. [Google Scholar]
- Dishion TJ, Stormshak EA. Intervening in children’s lives: An ecological, family-centered approach to mental health care. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Donenberg G, Baker BL. The impact of young children with externalizing behaviors on their families. Journal of Abnormal Child Psychology. 1993;21:179–186. doi: 10.1007/BF00911315. [DOI] [PubMed] [Google Scholar]
- Eddy JM, Leve LD, Fagot BI. Coercive family processes: A replication and extension of Patterson’s coercion model. Aggressive Behavior. 2001;27:14–25. [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review. 2004;24:441–459. doi: 10.1016/j.cpr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Elliot DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Thousand Oaks, CA: Sage; 1985. [Google Scholar]
- Enders CK. A primer on maximum likelihood algorithms available for use with missing data. Structural Equation Modeling. 2001;8:128–141. [Google Scholar]
- Farmer A, McGuffin P, Williams J. Measuring psychopathology. Oxford: Oxford University Press; 2002. [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. Journal of Abnormal Child Psychology. 1993;21:245–269. doi: 10.1007/BF00917534. [DOI] [PubMed] [Google Scholar]
- Feske U, Shear MK, Anderson B, Cyranowski J, Strassburger M, Matty M, et al. Comparison of severe life stress in depressed mothers and non-mothers: Do children matter. Depression and Anxiety. 2001;13:109–117. doi: 10.1002/da.1026. [DOI] [PubMed] [Google Scholar]
- Field T, Healy B, Goldstein S, Perry S, Bendell D, Shanberg S, et al. Infants of depressed mothers show ‘depressed’ behaviour even with non-depressed adults. Child Development. 1988;59:1569–1579. doi: 10.1111/j.1467-8624.1988.tb03684.x. [DOI] [PubMed] [Google Scholar]
- Fite PJ, Colder CR, Lochman JE, Wells KC. The mutual influence of parenting and boys’ externalizing behavior problems. Journal of Applied Developmental Psychology. 2006;27:151–164. doi: 10.1016/j.appdev.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flavell JH. The development of children’s knowledge about the mind: From cognitive connections to mental representations. In: Astington J, Harris P, Olson D, editors. Developing theories of mind. New York: Cambridge University Press; 1988. pp. 244–267. [Google Scholar]
- Forbes EE, Shaw DS, Fox NA, Cohn JF, Silk JS, Kovacs M. Maternal depression, child frontal asymmetry, and child affective behavior as factors in child behavior problems. Journal of Child Psychology and Psychiatry. 2006;47:79–87. doi: 10.1111/j.1469-7610.2005.01442.x. [DOI] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:320–354. [Google Scholar]
- Ghodsian M, Zajicek E, Wolkind S. A longitudinal study of maternal depression and child behaviour problems. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1984;25:91–109. doi: 10.1111/j.1469-7610.1984.tb01721.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Brumley HE. Schizophrenic and depressed mothers: Relational deficits in parenting. Developmental Psychology. 1990;26:31–39. [Google Scholar]
- Goodman SJ, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry. 2003;60:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Angold A, Harold GT, Sharp D. Pathways to violence in the children ofmothers who were depressed postpartum. Developmental Psychology. 2003;39:1083–1094. doi: 10.1037/0012-1649.39.6.1083. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Poulton R. Reciprocal effects of mothers’ depression and children’s problem behaviors from middle childhood to early adolescence. In: Huston AC, Ripke MN, McCord J, editors. Developmental contexts in middle childhood: Bridges to adolescence and adulthood. New York: Cambridge University Press; 2006. pp. 107–129. [Google Scholar]
- Johnston C, Mash EJ. Families of children with Attention-Deficit/Hyperactivity Disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Wu P. Disentangling mother-child effects in the development of antisocial behavior. In: McCord J, editor. Coercion and punishment in long-term perspectives. New York: Cambridge University Press; 1995. pp. 106–123. [Google Scholar]
- Keenan K, Shaw DS. The development of coercive family processes: The interaction between aversive toddler behavior and parenting factors. In: McCord J, editor. Coercion and punishment in long-term perspective. New York: Cambridge University Press; 1995. pp. 165–180. [Google Scholar]
- Keenan K, Shaw DS. Developmental and social influences on young girls’ early problem behavior. Psychological Bulletin. 1997;121:95–113. doi: 10.1037/0033-2909.121.1.95. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Rutter M, Tomás MP, Moffitt TE. The caregiving environments provided to children by depressed mothers with or without an antisocial history. American Journal of Psychiatry. 2006;163:1009–1018. doi: 10.1176/ajp.2006.163.6.1009. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford; 1998. [Google Scholar]
- Krueger RF, Schmutte PS, Caspi A, Moffitt TE, Campbell K, Silva PA. Personality traits are linked to crime among men and women: Evidence from a birth cohort. Journal of Abnormal Psychology. 1994;103:328–338. doi: 10.1037//0021-843x.103.2.328. [DOI] [PubMed] [Google Scholar]
- Lapalme M, Hodgins S, LaRoche C. Children of parents with bipolar disorder: A metaanalysis of risk for mental disorders. Canadian Journal of Psychiatry. 1997;42:623–631. doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- Leve LD, Kim HK, Pears KC. Childhood temperament and family environment as predictors of internalizing and externalizing trajectories from ages 5 to 17. Journal of Abnormal Child Psychology. 2005;33:505–520. doi: 10.1007/s10802-005-6734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Scaramella LV, Fagot BI. Infant temperament, pleasure in parenting, and marital happiness in adoptive families. Infant Mental Health Journal. 2001;22(5):545–558. [Google Scholar]
- Loeber R, Stouthamer-Loeber M. Development of juvenile aggression and violence: Some common misconceptions and controversies. American Psychologist. 1998;53:242–259. doi: 10.1037//0003-066x.53.2.242. [DOI] [PubMed] [Google Scholar]
- Loeber R, Keenan K, Zhang Q. Boys’ experimentation and persistence in developmental pathways toward serious delinquency. Journal of Child and Family Studies. 1997;6:321–357. [Google Scholar]
- Loehlin JC. Latent variable models. 4th ed. Mahwah, NJ: Erlbaum; 2004. [Google Scholar]
- Luoma I, Tamminen T, Kaukonen P, Laippala P, Puura K, Salmelin R, et al. Longitudinal study of maternal depressive symptoms and child well-being. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1367–1374. doi: 10.1097/00004583-200112000-00006. [DOI] [PubMed] [Google Scholar]
- Lytton H. Child and parent effects in boys’ conduct disorder: A reinterpretation. Developmental Psychology. 1990;26:683–697. [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychology Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Munson JA, McMahon RJ, Spieker SJ. Structure and variability in the developmental trajectory of children’s externalizing problems: Impact of infant attachment, maternal depressive symptomatology, and child sex. Development and Psychopathology. 2001;13:277–296. doi: 10.1017/s095457940100205x. [DOI] [PubMed] [Google Scholar]
- Murray L, Stanley C, Hooper R, King F, Fiori-Cowley A. The role of infant factors in postnatal depression and mother–infant interactions. Developmental Medicine and Child Neurology. 1996;38:109–119. doi: 10.1111/j.1469-8749.1996.tb12082.x. [DOI] [PubMed] [Google Scholar]
- Muthén BO. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 3rd ed. Los Angeles, CA: Muthén & Muthén; 2004. [Google Scholar]
- Nagin D, Tremblay RE. Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Development. 1999;70:1181–1196. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- Nelson K. Memory development from 4 to 7 years. In: Sameroff AJ, Haith MM, editors. The five to seven year shift: The age of reason and responsibility. Chicago: The University of Chicago Press; 1996. pp. 141–160. [Google Scholar]
- Nelson DR, Hammen C, Brennan PA, Ullman JB. The impact of maternal depression on adolescent adjustment: The role of expressed emotion. Journal of Counseling and Clinical Psychology. 2003;71:935–944. doi: 10.1037/0022-006X.71.5.935. [DOI] [PubMed] [Google Scholar]
- Olds D. Prenatal and infancy home visiting by nurses: From randomized trials to community replication. Prevention Science. 2002;3:153–172. doi: 10.1023/a:1019990432161. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Coercive family processes. Eugene, OR: Castalia; 1982. [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, et al. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25:413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Petriwskyj A, Thorpe K, Tayler C. Trends in construction of transition to school in three western regions, 1990–2004. International Journal of Early Years Education. 2005;13:55–69. [Google Scholar]
- Pianta RC, Cox MJ, Taylor L, Early D. Kindergarten teachers’ practices related to the transition to school: Results of a national survey. The Elementary School Journal. 1999;100:71–86. [Google Scholar]
- Pincus HA, Petit AR. The societal costs of chronic major depression. Journal of Clinical Psychiatry. 2001;62:5–9. [PubMed] [Google Scholar]
- Prinzie P, Onghena P, Hellinckx W, Grietens H, Ghesquiére P, Colpin H. Parent and child personality characteristics as predictors of negative discipline and externalizing problem behaviour in children. European Journal of Personality. 2004;18:73–102. [Google Scholar]
- Reid JB. Prevention of conduct disorder before and after school entry: Relating interventions to developmental findings. Development and Psychopathology. 1993;5:243–262. [Google Scholar]
- Rimm-Kaufman S. School transition and school readiness: An outcome of early childhood development. In: Tremblay RE, Barr RG, Peters RDeV, editors. Encyclopedia on Early Childhood Development. Montreal, Quebec: Centre of Excellence for Early Childhood Development; 2004. [Accessed September 21, 2007]. pp. 1–7. [online]2004:Available at: http://www.excellence-earlychildhood.ca/documents/Rimm-KaufmanANGxp.pdf. [Google Scholar]
- Rimm-Kaufman SE, Pianta RC. An ecological perspective on the transition to kindergarten: A theoretical framework to guide empirical research. Journal of Applied Developmental Psychology. 2000;21:491–511. [Google Scholar]
- Rimm-Kaufman SE, Pianta RC, Cox MJ. Teachers’ judgments of problems in the transition to kindergarten. Early childhood Research Quarterly. 2000;15:147–166. [Google Scholar]
- Rutter M, Graham P, Chadwick F, Yule W. Adolescent turmoil: Fact or fiction. Journal of Child Psychology and Psychiatry. 1976;17:35–56. doi: 10.1111/j.1469-7610.1976.tb00372.x. [DOI] [PubMed] [Google Scholar]
- Sameroff A. General systems theories and developmental psychopathology. In: Cichetti D, Cohen D, editors. Developmental psychopathology: Theory and methods. Vol. 1. New York: Wiley; 1995. pp. 659–695. [Google Scholar]
- Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997. [Google Scholar]
- Shaw DS, Dishion TJ, Supplee L, Gardner F, Arnds K. Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-Year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology. 2006a;74:1–9. doi: 10.1037/0022-006X.74.1.1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Schonberg M, Sherrill J, Huffman D, Lukon J, Obrosky D, et al. Responsivity to offspring’s expression of emotion among childhood-onset depressed mothers. Journal of Clinical Child and Adolescent Psychology. 2006b;35:490–503. doi: 10.1207/s15374424jccp3504_1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Winslow EB, Owens EB, Vondra JI, Cohn JF, Bell RQ. The development of early externalizing problems among children from low-income families: A transformational perspective. Journal of Abnormal Child Psychology. 1998;26:95–107. doi: 10.1023/a:1022665704584. [DOI] [PubMed] [Google Scholar]
- Silver RB, Measelle JR, Armstrong JM, Essex MJ. Trajectories of classroom externalizing behavior: Contributions of child characteristics, family characteristics, and the teacherchild relationship during the school transition. Journal of School Psychology. 2005;43:39–60. [Google Scholar]
- Silverberg S, Steinberg L. Psychological well-being of parents at midlife: The impact of early adolescent children. Developmental Psychology. 1990;26:658–666. [Google Scholar]
- Simon G, Katzelnick D. Depression, use of medical services, and cost-offset effects. Journal of Psychosomatic Research. 1997;42:333–344. doi: 10.1016/s0022-3999(96)00367-4. [DOI] [PubMed] [Google Scholar]
- Sinclair DA, Murray L. Effects of postnatal depression on children’s adjustment in school. British Journal of Psychiatry. 1998;172:58–63. doi: 10.1192/bjp.172.1.58. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Steinberg L. We know some things: Parent-adolescent relationships in retrospect and prospect. Journal of Research on Adolescence. 2001;11:1–19. [Google Scholar]
- Steinberg L, Steinberg W. Crossing paths: How your child’s adolescence triggers your own crisis. New York: Simon & Schuster; 1994. [Google Scholar]
- Teti DM, Gelfand DM. Behavioral competence among mothers and infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- Tudge JRH, Odero DA, Hogan DM, Etz KE. Relations between the everyday activities of preschoolers and their teachers’ perceptions of their competence in the first years of school. Early Childhood Research Quarterly. 2003;18:42–64. [Google Scholar]
- Wilkins AJ, O’Callaghan MJ, Najman JM, Bor W, Williams GM, Shuttlewood G. Early childhood factors influencing health-related quality of life in adolescents at 13 years. Journal of Paediatrics and Child Health. 2004;40:102–109. doi: 10.1111/j.1440-1754.2004.00309.x. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Iannotti RJ, Cummings EM, Denham S. Antecedents of problem behaviors in children of depressed mothers. Development and Psychopathology. 1990;2:271–291. [Google Scholar]