Abstract
Background
The number of individuals at risk for dementia will probably increase in ageing societies as will the array of preventive and therapeutic options, both however within limited economic resources. For economic and medical purposes valid instruments are required to assess disease processes and the efficacy of therapeutic interventions for different forms and stages of illness. In principal, the impact of illness and success of an intervention can be assessed with biomedical variables, e.g. severity of symptoms or frequency of complications of a disease. However, this does not allow clear judgement on clinical relevance or comparison across different diseases.
Discussion
Outcome model variables such as quality of life (QoL) or health care resource utilization require the patient to appraise their own well-being or third parties to set preferences. In Alzheimer's disease and other dementias the evaluation process performed by the patient is subject to the disease process itself because over progress of the disease neuroanatomical structures are affected that mediate evaluation processes.
Summary
Published research and methodological considerations thus lead to the conclusion that current QoL-instruments, which have been useful in other contexts, are ill-suited and insufficiently validated to play a major role in dementia research, decision making and resource allocation. New models integrating biomedical and outcome variables need to be developed in order to meet the upcoming medical and economic challenges.
Background
Prevalence of Alzheimer's disease and other dementias increase in the aging societies of the Western hemisphere. This puts an ever increasing burden on the health care systems. Considering increasing treatment options over almost the whole spectrum of diseases effective spending of the resources of health care systems is warranted to provide a fair if not comprehensive care. Hence payers, physicians and patients will need to weigh costs and benefits of future interventions much more carefully. The "burden of illness" and "quality of life" convey greater meaning and more direct relevance across a wide spectrum of diseases and illnesses than abstract clinical or scientific parameters, and such dimensions will gain greater appeal for a larger community involved in future decisions.
Biomedical measures are appropriate to determine the consequences of disease on specific medically relevant symptoms. For oncological diseases this may include the size of the tumor or the number and region of metastases. In order to assess the impact on the patient's everyday life these biomedical measures need to be supplemented by other measures relating to everyday life such as the quality of life or pain. For dementing disorders specific symptoms of disease such as cerebral atrophy can be measured in much the same way as the size of a tumor. Beyond this, several symptoms of dementia, e.g. the impairment of memory, can be measured with standardized instruments, whose relevance for everyday life is obvious. Over the course of Alzheimer's dementia the burden of disease is not primarily reflected by diminishing cognitive functions of patients, but also by a variety of behavioural problems and physical handicaps. There is, however, a great deal of heterogeneity regarding the manifestation of, and the coping with these non-cognitive symptoms. Therefore more comprehensive instruments are required to take account of such causes and their effects within the context of family or professional care.
Quality of Life (QoL) measurements require the patient's self-assessment of his or her fulfilment and impairment in everyday life. Sometimes seemingly negligible causes lead to major handicaps, and severe changes regarding the quality of life and resource usage, whereas severe medical problems need not be associated with apparent subjective consequences. These observations suggest that data on subjective relevance and economic outcomes should be included in clinical studies in order to prepare the ground for future cost-effectiveness models which will need to include the subjective and social impact of illness and interventions. [1].
We will address several moot points regarding the use of "quality of life" and other concepts and instruments, which have been developed for other target groups, but are now employed in the context of dementia. We hope to prevent premature conclusions based on the uncritical administration of such scales in patients with dementia, and we argue for the development of adequate tools.
Discussion
Biomedical instruments for assessing dementia
Dementia is a frequent disorder in the elderly and its prevalence increases with age [2]. The most frequent cause is AD. At onset of AD the medial temporal lobe is affected [3] resulting in episodic memory deficit as the early clinical hallmark [4]. As the disease spreads, other brain regions are affected as well. The parietal cortex mediates functions such as spatial orientation and visuospatial functions [5,6], the frontal cortex executive functions, planning, attention, and working memory [7-9]. Spread of AD beyond the temporal lobe thus is characterized in functional terms by accruing deficits of spatial orientation, attention and executive functions as well as working memory and language [4] beyond initial temporal lobe type memory deficits. This can be visualized using advanced imaging methods [10,11].
For Clinical Study purposes test batteries are used, most commonly the Mini Mental Status Examination (MMSE) [12,13] and the Alzheimer's Disease Assessment Scale (ADAScog). Cognitive scales such as the MMSE or the cognitive sub-scale of the ADAScog mingle the results of several cognitive functions into one composite score. While any of the assessed symptoms might be present at one time point or the other during the course of an individual's disease they will not be present all at once at any given stage of disease. Moreover, the dynamic range for observation of change is not the whole band of the scale but a small margin centered around the observed score. Unfortunately, the sensitivity to change of these scores is not linear over the course of disease. As recently reviewed [14] it often is argued that a certain score difference, e.g. a 4-point difference in the ADAScog score, represents a meaningful clinical outcome. However, this judgement remains arbitrary and does not reflect clinical observations of large score differences with hardly any differences in everyday life and vice versa.
Impact of disease in terms of Quality of Life (QoL)
The concept of QoL relates to the 1947 definition of 'health' by the World Health Organization (WHO) as being a state of complete physical, mental, and social well-being [15]. In a similar fashion, Lawton characterized five domains pertaining to QoL for subjects with dementing illnesses to comprise the same areas as in people in general (cognitive functioning, ability to perform activities of daily living, being able to engage in meaningful time use, social behavior, as well as a favorable balance between positive emotion and absence of negative emotion) [16]. As QoL refers to all aspects of a patient's life, it can provide complementary and valuable information on the patient's self perception of health and treatment impact. Therefore, QoL is suggested in many disease areas as an important outcome to evaluate new treatments.
Considering the subjective nature of the QoL concept it is generally agreed that any appraisal thereof at best should rely on the perception of the individual to be looked at. The use of proxies (e.g relatives or a nurse) to measure QoL has inherent obstacles, such as personality characteristics of the proxy, the nature of the relationship, the time spent with one another, and the level of impairment. Frequently, proxy appraisal of the patient's QoL are disparate to the patients own evaluation [17]. Moreover, discrepancies between dementia patients' and their caregivers' ratings of the patients' quality of life are associated with increased levels of caregiver burden, rather than lower levels of patients' functioning alone [18,19] and thus are not only related to the disease process in the patient but external and internal factors of the proxy. The proxie's experiences of depression and burden might also negatively affect proxies' assessments of QoL [17]. Despite these observations this procedure has been used when patients are too severely impaired to complete the rating themselves. At best, proxy-ratings can be considered as complementary information for self-ratings but not as a substitute. Despite these difficulties and need for further methodological research [20], QoL has become an important dimension of AD therapeutic research [21] and health economic analyses in this area.
There are different concepts to measure a health-related quality of life (QoL). Rather than qualifying the approaches purely as either medical or economic, a methodological classification would focus on the major components used in describing and valuating QoL of dementia patients (Table 1). For measuring QoL of those who provide care for dementia patients (e.g., relatives) Table 1 without the proxy category would most likely be adequate. All approaches to value QoL require a descriptive element. (The literature mentions valuations based on numerical ratings alone, however, without a descriptive basis their valuation lacks any relation to aspects of the health status).
Table 1.
Classification of approaches to describe and valuate QoL according to the person surveyed
| Person surveyed or person defining | Measures to describe QoL | Procedures to valuate QoL | ||
| Generic | Disease-specific | Externally defined a | Preference-based b | |
| Patient | I | II | - | 1 |
| Proxy | III | IV | - | 2 |
| Scientist | - | - | 3 | - |
| Population | - | - | - | 4 |
a e.g. a sum score
b especially according to the procedures of VAS, TTO and SG, enabling the calculation of QALYs
Quality of Life – Utility Measure in Health Economics
In economic cost-utility studies generic descriptions of QoL are combined with preference-based valuations. From an economic perspective, the preferences of the individual are the key criteria to assess whether goods or services can be considered "efficient"' from the perspective of the consumer (for most consumers, even the most cost-effectively produced shoes would be worth little if it were only left ones). Economists would suggest eliciting the preferences of those individuals affected by an intervention. When looking from a medical point of view, this would definitely be the patient. As in dementia the choice of the approach may be restricted by the capabilities of the patient, one would have to consider surveying a proxy (e.g., a relative) instead of the patient in cases where he would be unable to articulate his preferences but the use of this approach may be limited (cf. above).
Yet there are also other positions in the discussion with respect to the preferences to be used for valuation. When the question is about which services are to be covered in a national or statutory health service, some economists argue that it is the general population which is affected and that, accordingly, their preferences should be used for valuation (which is then typically derived via given pre-defined standardized health states in interviews or surveys). This approach, however, is distorted given the lack of knowledge about Alzheimer's disease in the general population [22-25]. The key problem in valuation, in any case, is to give a summary statement on QoL that integrates all different aspects of health at stake. Any answer to this problem should be scientifically well motivated. A simple solution is to use a pre-defined algorithm instead of preferences, e.g. a sum score across a health profile. Yet, this might only reflect the judgement of the constructor of the sum score. Obviously, constructors, the general population, the proxy or the patient himself may not assess a health state, such as e.g. mild dementia, in the same way. In the end, the choice of the method to integrate all health aspects will also depend on the type of decision that waits to be supported by the QoL data but proceeding in such a way somewhat forecloses a later result. Furthermore, the methodological usefulness of the approach used to describe and valuate QoL must be critically considered. The most important criteria for psychometric testing include reliability, validity and responsiveness [26]. For any measurement of QoL that claims to rely on scientific grounds it is necessary to show that the instrument used is psychometrically appropriate for the target group of patients or population analyzed – the foundation of what is being measured, and how well this is being achieved, is lacking otherwise. Accordingly, respective methodological pilot studies are required as long as the respective properties of the measurement instrument cannot be quoted from the literature.
In clinical research, one of the important differences of different QoL measures is measuring health status or utility of different health states. Health status measures describe functioning and the impact of illness on health. They are generally subdivided into generic and disease-specific measures. The generic measures are intended for general use and suitable for wide range of patient groups. Measuring general health status is important because it shows the extent to which interventions really make a difference to a patient's overall life and helps to quantify the relative effects of different interventions for patients with different diseases. The SF-36 and the EQ-5D instruments are the most frequently used generic QoL measures worldwide, while only for the EQ 5D broadly acknowledged valuation procedures are available to elicitate corresponding utilities. Typically one of these generic measures in clinical research is combined with one or more disease-specific measures. The latter aim at emphasizing problems specific to patients with the disease in question (e.g. EORTC QLQ-C30 or FACT-G in cancer research or the QOL-AD focusing on Alzheimer's disease). Compared with generic measures, disease-specific measures normally are more sensitive and responsive to the changes in the assessment of QoL of specific patient groups.
Utilities measures describe utilities or quality-of-life weights to health states derived by either direct or indirect utility measures. Direct utility measures include visual analogue scales (VAS), standard gamble (SG), and time trade-off (TTO) techniques. VAS asks patients to indicate on an e.g. 10 cm Likert scale the position of their current state, and also to mark positions corresponding to various scenarios. SG attempts to estimate patient's preferences under uncertainty, where the uncertainty involves a risk of death or some other outcome. On the other hand, TTO measures patients' preferences under certainty. The patients are asked to indicate whether they would choose one year in perfect health or one year with impaired health. SG and TTO have been found to be practical on most populations with TTO being a commonly used substitute for the SG method and vice versa. Some QoL instruments were developed to produce a series of health utilities, such as the Quality of Well-Being scale (QWB), the Health Utilities Index (HUI) and the EQ-5D from the EuroQoL group. They are referred to as being generic or indirect utility measures and in practice the generic utility measures are widely used mainly due to their ease in use: The answers of only few questions result in a QoL-utility. For example using the EQ-5D patients have to answer five questions, one question for one dimension of QoL (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), and give an expression of their current state of QoL via the VAS.
These utility measures assign values or utilities for health states from 0.0 to 1.0, where 0 is defined as death and 1 is defined as the best possible health state. The health state utilities are used to calculate quality-adjusted life-years (QALYs) which are applied in cost-utility or cost-effectiveness analysis. Based on health-related quality of life and survival for the patient, QALYs can assess the extent of the benefits gained from interventions. During that approach not only gained life time but also quality of that time gained is combined and it is defined that there exists the possibility of trade off between these two aspects. When the QALY is used in different indications and/or interventions, cross-comparisons can be made to describe the relative benefit for patients. When combined with the costs of providing the interventions, decision makers can understand the relative cost-effectiveness of different interventions. When resources are scarce one can argue that those interventions should be reimbursed which provide the best incremental cost-effectiveness ratio.
Regardless of whether a method is used that asks for a direct appraisal by the patient or that assesses of preferences these approaches implicitly assume that the patient is in a position to perform a valid appraisal of his or her own situation and that a sufficient knowledge about the disease is at hand.
Deficits of judgement and decision-making in patients with dementia
Competent choices require awareness of competences and restrictions and a deliberate judgement on well- or ill-being despite present and future deficits. Lesions or malfunctioning of the frontal and prefrontal cortex foster a lack of awareness of deficits and impairments and ultimately the inability of formulating a free will [27]. A recent functional imaging study demonstrated this even in a semi-quantitative fashion. Decreased awareness was positively correlated with perfusion deficits in frontal regions [28]. It is unclear yet, whether impairment of deficit awareness is predominantly associated with frontal cortex malfunction or overall severity of central nervous system disease. While some studies suggest that the former is true [29] other studies suggest the latter [30-33]. Impaired awareness of deficits has been associated with malfunctions of the right hemisphere [34], the temporo-parietal junction [35], the right prosubiculum of the hippocampus [34], the parietal cortex [36], and the anterior cingulate gyri [37]. Thus a widespread network is involved in the awareness of deficits. This network is affected early on during progressing AD or other dementias although the pattern is unpredictable and subject to the specific disease and other internal and external factors in the patient, e.g. comorbidities.
Patients with mild dementia [27,34,38-42] and even those with Mild Cognitive Impairment (MCI) [43] frequently demonstrate decreased awareness of their cognitive impairments and change of behaviour. In particular, decreased awareness of deficits manifests as poor awareness of deficits in activities of daily living (ADL) [30]. Compared to their proxies, AD and MCI patients underestimate their deficits [36,44]. Moreover, however, family informants may also fail to recognize memory problems in subjects subsequently found to have dementia [45]. Patients' awareness of deficits is associated positively or negatively with age, gender, pre-morbid education and socioeconomic status in a complex fashion [31,46]. In general, awareness of deficits seems to decrease with an increased severity of dementia [30-32]. Awareness of deficits is modulated by even sub-syndromal depression, anxiety, psychosis, and apathy [28,31,47]. This modulation is subject to pre-morbid capacities as depressive symptoms and awareness were found to be positively related in high, but not low, cognitive reserve groups [48].
Standard approaches to judge the future impact of deficits on subjective well-being are also impaired in AD. AD patients perform less well in gambling tasks than elderly controls and show impairments in cognitive estimation [49]. Psychopharmacological and pathological evidence supports the concept of a 'cholinergic component' of conscious awareness [50]. In AD, a cholinergic deficit has been established many years ago [51] so that for this disease in particular the ability of the patient to undertake a deliberate choice is questioned.
On these grounds it can be expected that patients with mild AD have difficulties in taking decisions in every-day life situations, both in cases of ambiguity (information on probability is missing or conflicting, and the expected utility of the different options is incalculable) and in cases of risk (outcomes can be predicted by well-defined or estimable probabilities) [52]. Moreover, AD patients frequently change between strategies so that decisions are given in a random fashion which precludes the development of a consistent response pattern over time [53].
Where to go?
In a summary recommendation aiming at patients after reviewing studies for dementia drugs, The American College of Physicians & The American Academy of Family Physicians concluded that outcomes related to QoL were studied (and hence, captured) less frequently than other outcome measures, and did not show consistent improvements attributable to drugs analyzed. Considering that dementia studies do not use survival as endpoint but rather employ intermediate surrogate endpoints, this is a remarkable statement. This enhances the need to elaborate on difficulties in accurately measuring QoL for this patient group [54]. Methodological problems are pinpointed when it comes to measuring the impact of drug treatment on QoL of dementia patients in terms of QALYs (Table 2).
Table 2.
Appraisal of the internal validity of the QALY-endpoint in six cost-utility studies in the HTA on dementia drugs [56]
| Product assessed (study) | Internal validity | Comment on generation of QALYs |
| Donepezil [58] | Unacceptable | Based on the Index of Health Related Quality of Life (IHQL) which was not validated for valuing cognitive impairment, and no rationale was given for the IHQL values used |
| Donepezil [59] | Unclear or unknown | Not stated |
| Rivastigmine [60] | Unacceptable | Based on the IHQL (see above) |
| Galantamine [61,62] | Unclear or unknown | Derived from [63] (pre – full time care at 0.60, full time care at 0.34) |
| Memantine [64] | Unclear or unknown/unacceptable | Insufficient detail found in the study |
A few key questions which type of studies might be able to answer some questions appropriately can be taken from a current British consensus paper on good health economic modelling standards [55]: "Are the utilities incorporated into the model weights (utilities) appropriate? Is the source for the utility weights referenced? Are the methods of derivation for the utility weights justified?"
In their health technology assessment report on dementia drugs for the U.K. National Institute for Health and Clinical Excellence (NICE) Loveman et al [56] have evaluated the use of the QALY-endpoint in six cost-utility studies. Not one of the studies investigated achieved the label of being internally valid at this point, some of them lacking transparency, some lacking appropriate measurement instruments, and others using too simple assumptions (table 2). Next to the published literature, the industry submissions on the drugs investigated in this study were evaluated according to the quoted Philips et al. (2006) standards [55] with respect to the utility measurement. Again, no classification as 'internally valid' could be achieved.
It can thus be concluded that large gaps exist between published measurements of QoL in terms of utility and the quality standards required by guidelines. This conclusion is further supported by a consensus statement on measuring treatment benefits in dementia, in which the International Psychogeriatric Association has stated that health utility measures are not validated satisfactorily in dementia and that this calls into question previous health economic analyses [57].
These sobering findings on QALY measurements in dementia patients would further worsen if the guidelines' requirements were extended for the above claimed need to show the usefulness of the measurement instruments used according to the usual psychometric testing criteria which were not met by the quoted studies. Future research, [56] concluded accordingly, should include information on the quality of the outcome measures used as well as the need to establish QoL instruments for dementia patients.
Summary
We conclude that current outcome model variables, especially quality of life measures, are well suited and established for non-dementing diseases but at present are not fully suited to be rested upon in medical or health economic analyses of disease impact or therapeutic interventions in the dementias. The function of representation of objective measures as obtained by biomedical assessments or proxy measures in their relation to everyday life or instruments of quality of life assessments is elusive, yet (Figure 1). In consideration of the increasing prevalence of Alzheimer's disease and other dementias in old age an integrative model of biomedical and outcome model variables is warranted to face the upcoming medical and health economic challenges.
Figure 1.
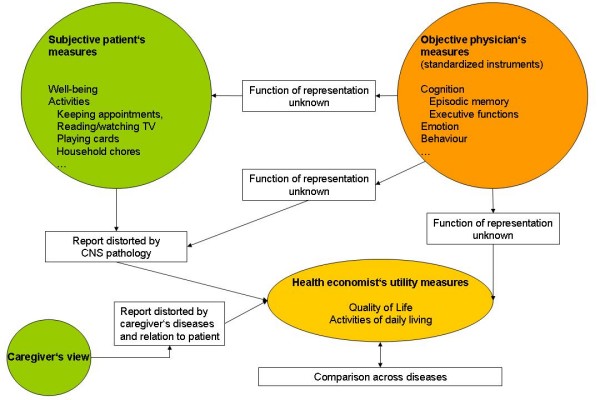
Measures relevant for dementias.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MWR was involved in drafting the manuscript, interpretation of the literature and critical revision. TM was involved in drafting the manuscript, interpretation of the literature and critical revision. HF was involved in drafting the manuscript, interpretation of the literature and critical revision. LF was involved in interpretation of the literature and critical revision. MH was involved in interpretation of the literature and critical revision. RL was involved in drafting the manuscript, interpretation of the literature and critical revision. CV was involved in interpretation of the literature and critical revision. MVDS was involved in interpretation of the literature and critical revision. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Matthias W Riepe, Email: matthias.riepe@uni-ulm.de.
Thomas Mittendorf, Email: tm@ivbl.uni-hannover.de.
Hans Förstl, Email: Hans.Foerstl@lrz.tu-muenchen.de.
Lutz Frölich, Email: lutz.froelich@zi-mannheim.de.
Martin Haupt, Email: m.haupt@alzheimer-praxis-duesseldorf.de.
Reiner Leidl, Email: leidl@bwl.lmu.de.
Christoph Vauth, Email: cv@ivbl.uni-hannover.de.
Matthias Graf von der Schulenburg, Email: jms@ivbl.uni-hannover.de.
References
- Vellas B, Andrieu S, Sampaio C, Wilcock G. Disease-modifying trials in Alzheimer's disease: a European task force consensus. Lancet Neurol. 2007;6:56–62. doi: 10.1016/S1474-4422(06)70677-9. [DOI] [PubMed] [Google Scholar]
- Erkinjuntti T, Ostbye T, Steenhuis R, Hachinski V. The effect of different diagnostic criteria on the prevalence of dementia. N Engl J Med. 1997;337:1667–1674. doi: 10.1056/NEJM199712043372306. [DOI] [PubMed] [Google Scholar]
- Hyman BT, Van Horsen GW, Damasio AR, Barnes CL. Alzheimer's disease: cell-specific pathology isolates the hippocampal formation. Science. 1984;225:1168–1170. doi: 10.1126/science.6474172. [DOI] [PubMed] [Google Scholar]
- Hodges JR. Memory in the dementias. In: Tulving E, Craik FIM, editor. The Oxford Handbook of Memory. Oxford, New York: Oxford University Press; 2000. pp. 441–459. [Google Scholar]
- Marshall JC, Fink GR. Spatial cognition: where we were and where we are. Neuroimage. 2001;14:S2–S7. doi: 10.1006/nimg.2001.0834. [DOI] [PubMed] [Google Scholar]
- Save E, Poucet B. Hippocampal-parietal cortical interactions in spatial cognition. Hippocampus. 2000;10:491–499. doi: 10.1002/1098-1063(2000)10:4<491::AID-HIPO16>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Godefroy O, Cabaret M, Petit-Chenal V, Pruvo JP, Rousseaux M. Control functions of the frontal lobes. Modularity of the central-supervisory system? Cortex. 1999;35:1–20. doi: 10.1016/S0010-9452(08)70782-2. [DOI] [PubMed] [Google Scholar]
- Nagahama Y, Okada T, Katsumi Y, Hayashi T, Yamauchi H, Oyanagi C, et al. Dissociable mechanisms of attentional control within the human prefrontal cortex. Cereb Cortex. 2001;11:85–92. doi: 10.1093/cercor/11.1.85. [DOI] [PubMed] [Google Scholar]
- Rowe JB, Toni I, Josephs O, Frackowiak RS, Passingham RE. The prefrontal cortex: response selection or maintenance within working memory? Science. 2000;288:1656–1660. doi: 10.1126/science.288.5471.1656. [DOI] [PubMed] [Google Scholar]
- Gron G, Bittner D, Schmitz B, Wunderlich AP, Riepe MW. Subjective memory complaints: Objective neural markers in patients with Alzheimer's disease and major depressive disorder. Ann Neurol. 2002;51:491–498. doi: 10.1002/ana.10157. [DOI] [PubMed] [Google Scholar]
- Gron G, Riepe MW. A neural basis of the cognitive continuum in episodic memory from health to Alzheimer's Disease. Am J Geriatr Psychiatry. 2004;12:648–652. doi: 10.1176/appi.ajgp.12.6.648. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Robins LN, Helzer JE. The Mini-Mental State Examination. Arch Gen Psychiatry. 1983;40:812. doi: 10.1001/archpsyc.1983.01790060110016. [DOI] [PubMed] [Google Scholar]
- Ashford JW, Kolm P, Colliver JA, Bekian C, Hsu LN. Alzheimer patient evaluation and the mini-mental state: item characteristic curve analysis. J Gerontol. 1989;44:139–146. doi: 10.1093/geronj/44.5.p139. [DOI] [PubMed] [Google Scholar]
- Molnar FJ, Man-Son-Hing M, Fergusson D. Systematic Review of Measures of Clinical Significance Employed in Randomized Controlled Trials of Drugs for Dementia. J Am Geriatr Soc. 2009;57:536–546. doi: 10.1111/j.1532-5415.2008.02122.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Constitution of the World Health Organization Geneva, Switzerland. 1947.
- Lawton MP. Quality of life in Alzheimer disease. Alzheimer Dis Assoc Disord. 1994;8:138–150. doi: 10.1046/j.1532-5415.2001.49210.x. [DOI] [PubMed] [Google Scholar]
- Karlawish JH, Casarett D, Klocinski J, Clark CM. The relationship between caregivers' global ratings of Alzheimer's disease patients' quality of life, disease severity, and the caregiving experience. J Am Geriatr Soc. 2001;49:1066–1070. doi: 10.1046/j.1532-5415.2001.49210.x. [DOI] [PubMed] [Google Scholar]
- Zanetti O, Geroldi C, Frisoni GB, Bianchetti A, Trabucchi M. Contrasting results between caregiver's report and direct assessment of activities of daily living in patients affected by mild and very mild dementia: the contribution of the caregiver's personal characteristics. J Am Geriatr Soc. 1999;47:196–202. doi: 10.1111/j.1532-5415.1999.tb04578.x. [DOI] [PubMed] [Google Scholar]
- Sands LP, Ferreira P, Stewart AL, Brod M, Yaffe K. What explains differences between dementia patients' and their caregivers' ratings of patients' quality of life? Am J Geriatr Psychiatry. 2004;12:272–280. doi: 10.1159/000051197. [DOI] [PubMed] [Google Scholar]
- Gauthier S. Update on diagnostic methods, natural history and outcome variables in Alzheimer's disease. Dement Geriatr Cogn Disord. 1998;9:2–7. doi: 10.2165/00019053-200624010-00004. [DOI] [PubMed] [Google Scholar]
- Dixon S, Walker M, Salek S. Incorporating carer effects into economic evaluation. Pharmacoeconomics. 2006;24:43–53. doi: 10.1177/1533317508317818. [DOI] [PubMed] [Google Scholar]
- Lundquist TS, Ready RE. Young adult attitudes about Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2008;23:267–273. doi: 10.1177/1533317508317818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwalen S, Forstl H. [Alzheimer's disease: knowledge and attitudes in a representative survey] Neuropsychiatr. 2008;22:35–37. doi: 10.1097/WAD.0b013e3181461740. [DOI] [PubMed] [Google Scholar]
- Connell CM, Scott RJ, McLaughlin SJ. Public opinion about Alzheimer disease among blacks, hispanics, and whites: results from a national survey. Alzheimer Dis Assoc Disord. 2007;21:232–240. doi: 10.1097/WAD.0b013e3181461740. [DOI] [PubMed] [Google Scholar]
- McLaughlin KJ, Harden PN, Ueda S, Boulton-Jones JM, Connell JM, Jardine AG. The role of genetic polymorphisms of angiotensin-converting enzyme in the progression of renal diseases. Hypertension. 1996;28:912–915. doi: 10.1007/BF00422218. [DOI] [PubMed] [Google Scholar]
- Hays RD, Anderson R, Revicki D. Psychometric considerations in evaluating health-related quality of life measures. Qual Life Res. 1993;2:441–449. doi: 10.1136/jnnp.2004.053157. [DOI] [PubMed] [Google Scholar]
- Eslinger PJ, Dennis K, Moore P, Antani S, Hauck R, Grossman M. Metacognitive deficits in frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2005;76:1630–1635. doi: 10.1002/(SICI)1099-1166(199912)14:12<1019::AID-GPS61>3.0.CO;2-F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derouesne C, Thibault S, Lagha-Pierucci S, Baudouin-Madec V, Ancri D, Lacomblez L. Decreased awareness of cognitive deficits in patients with mild dementia of the Alzheimer type. Int J Geriatr Psychiatry. 1999;14:1019–1030. doi: 10.1136/jnnp.57.7.805. [DOI] [PubMed] [Google Scholar]
- Michon A, Deweer B, Pillon B, Agid Y, Dubois B. Relation of anosognosia to frontal lobe dysfunction in Alzheimer's disease. J Neurol Neurosurg Psychiatry. 1994;57:805–809. doi: 10.1136/jnnp.2005.085373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starkstein SE, Jorge R, Mizrahi R, Robinson RG. A diagnostic formulation for anosognosia in Alzheimer's disease. J Neurol Neurosurg Psychiatry. 2006;77:719–725. doi: 10.1017/S1041610205002772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aalten P, van VE, de Vugt ME, Lousberg R, Jolles J, Verhey FR. Awareness and behavioral problems in dementia patients: a prospective study. Int Psychogeriatr. 2006;18:3–17. doi: 10.1017/S1041610207005492. [DOI] [PubMed] [Google Scholar]
- Dourado M, Marinho V, Soares C, Engelhardt E, Laks J. Awareness of disease in Alzheimer's dementia: description of a mild to moderate sample of patient and caregiver dyads in Brazil. Int Psychogeriatr. 2007;19:733–744. doi: 10.1159/000117056. [DOI] [PubMed] [Google Scholar]
- Lopez OL, Becker JT, Somsak D, Dew MA, DeKosky ST. Awareness of cognitive deficits and anosognosia in probable Alzheimer's disease. Eur Neurol. 1994;34:277–282. doi: 10.1136/jnnp.2003.030007. [DOI] [PubMed] [Google Scholar]
- Marshall GA, Kaufer DI, Lopez OL, Rao GR, Hamilton RL, DeKosky ST. Right prosubiculum amyloid plaque density correlates with anosognosia in Alzheimer's disease. J Neurol Neurosurg Psychiatry. 2004;75:1396–1400. doi: 10.1002/hbm.20203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon E, Perani D, Herholz K, Marique P, Kalbe E, Holthoff V, et al. Neural correlates of anosognosia for cognitive impairment in Alzheimer's disease. Hum Brain Mapp. 2006;27:588–597. doi: 10.1097/00002093-199601020-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott BR, Lafleche G, Whelihan WM, Buongiorno GW, Albert MS, Fogel BS. Impaired awareness of deficits in Alzheimer disease. Alzheimer Dis Assoc Disord. 1996;10:68–76. doi: 10.1159/000119594. [DOI] [PubMed] [Google Scholar]
- Hanyu H, Sato T, Akai T, Shimizu S, Hirao K, Kanetaka H, et al. Neuroanatomical correlates of unawareness of memory deficits in early Alzheimer's disease. Dement Geriatr Cogn Disord. 2008;25:347–353. doi: 10.1007/s11065-005-9026-7. [DOI] [PubMed] [Google Scholar]
- Ecklund-Johnson E, Torres I. Unawareness of deficits in Alzheimer's disease and other dementias: operational definitions and empirical findings. Neuropsychol Rev. 2005;15:147–166. doi: 10.1097/00002093-199509020-00007. [DOI] [PubMed] [Google Scholar]
- McDaniel KD, Edland SD, Heyman A. Relationship between level of insight and severity of dementia in Alzheimer disease. CERAD Clinical Investigators. Consortium to Establish a Registry for Alzheimer's Disease. Alzheimer Dis Assoc Disord. 1995;9:101–104. doi: 10.1016/j.bandc.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Banks S, Weintraub S. Self-awareness and self-monitoring of cognitive and behavioral deficits in behavioral variant frontotemporal dementia, primary progressive aphasia and probable Alzheimer's disease. Brain Cogn. 2008;67:58–68. doi: 10.1093/brain/awl367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Keeffe FM, Murray B, Coen RF, Dockree PM, Bellgrove MA, Garavan H, et al. Loss of insight in frontotemporal dementia, corticobasal degeneration and progressive supranuclear palsy. Brain. 2007;130:753–764. doi: 10.1136/jnnp.2004.042879. [DOI] [PubMed] [Google Scholar]
- Rankin KP, Baldwin E, Pace-Savitsky C, Kramer JH, Miller BL. Self awareness and personality change in dementia. J Neurol Neurosurg Psychiatry. 2005;76:632–639. doi: 10.1159/000076354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel A, Stokholm J, Gade A, Andersen BB, Hejl AM, Waldemar G. Awareness of deficits in mild cognitive impairment and Alzheimer's disease: do MCI patients have impaired insight? Dement Geriatr Cogn Disord. 2004;17:181–187. doi: 10.1177/1533317506292454. [DOI] [PubMed] [Google Scholar]
- Onor ML, Trevisiol M, Negro C, Aguglia E. Different perception of cognitive impairment, behavioral disturbances, and functional disabilities between persons with mild cognitive impairment and mild Alzheimer's disease and their caregivers. Am J Alzheimers Dis Other Demen. 2006;21:333–338. doi: 10.1001/jama.277.10.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross GW, Abbott RD, Petrovitch H, Masaki KH, Murdaugh C, Trockman C, et al. Frequency and characteristics of silent dementia among elderly Japanese-American men. The Honolulu-Asia Aging Study. JAMA. 1997;277:800–805. doi: 10.1016/j.acn.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Spitznagel MB, Tremont G. Cognitive reserve and anosognosia in questionable and mild dementia. Arch Clin Neuropsychol. 2005;20:505–515. doi: 10.1016/j.acn.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Starkstein SE, Petracca G, Chemerinski E, Kremer J. Syndromic validity of apathy in Alzheimer's disease. Am J Psychiatry. 2001;158:872–877. doi: 10.1176/appi.ajp.158.6.872. [DOI] [PubMed] [Google Scholar]
- Spitznagel MB, Tremont G, Brown LB, Gunstad J. Cognitive reserve and the relationship between depressive symptoms and awareness of deficits in dementia. J Neuropsychiatry Clin Neurosci. 2006;18:186–190. doi: 10.1007/s00702-007-0752-2. [DOI] [PubMed] [Google Scholar]
- Barabassy A, Beinhoff U, Riepe MW. Cognitive estimation in mild Alzheimer's disease. J Neural Transm. 2007;114:1479–1484. doi: 10.1016/S0166-2236(98)01361-7. [DOI] [PubMed] [Google Scholar]
- Perry E, Walker M, Grace J, Perry R. Acetylcholine in mind: a neurotransmitter correlate of consciousness? Trends Neurosci. 1999;22:273–280. doi: 10.1126/science.7046051. [DOI] [PubMed] [Google Scholar]
- Bartus RT, Dean RL, Beer B, Lippa AS. The cholinergic hypothesis of geriatric memory dysfunction. Science. 1982;217:408–414. doi: 10.1016/j.neuropsychologia.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Sinz H, Zamarian L, Benke T, Wenning GK, Delazer M. Impact of ambiguity and risk on decision making in mild Alzheimer's disease. Neuropsychologia. 2008;46:2043–2055. doi: 10.1016/j.neuropsychologia.2007.01.006. [DOI] [PubMed] [Google Scholar]
- Delazer M, Sinz H, Zamarian L, Benke T. Decision-making with explicit and stable rules in mild Alzheimer's disease. Neuropsychologia. 2007;45:1632–1641. doi: 10.1016/j.neuropsychologia.2007.01.006. [DOI] [PubMed] [Google Scholar]
- Summaries for patients. Drug treatment for patients with dementia: American College of Physicians and American Academy of Family Physicians recommendations. Ann Intern Med. 2008;148:I41. doi: 10.2165/00019053-200624040-00006. [DOI] [PubMed] [Google Scholar]
- Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment: a review and consolidation of quality assessment. Pharmacoeconomics. 2006;24:355–371. doi: 10.2165/00019053-200624040-00006. [DOI] [PubMed] [Google Scholar]
- Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al. The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer's disease. Health Technol Assess. 2006;10:iii–xi. doi: 10.1017/S1041610207005145. [DOI] [PubMed] [Google Scholar]
- Katona C, Livingston G, Cooper C, Ames D, Brodaty H, Chiu E. International Psychogeriatric Association consensus statement on defining and measuring treatment benefits in dementia. Int Psychogeriatr. 2007;19:345–354. doi: 10.1017/S1041610207005145. [DOI] [PubMed] [Google Scholar]
- Stein K. Donepezil in the treatment of mild to moderate senile dementia of the Alzheimer type (SDAT) Bristol: NHS Executive South and West; 1998. [Google Scholar]
- Neumann PJ, Hermann RC, Kuntz KM, Araki SS, Duff SB, Leon J, et al. Cost-effectiveness of donepezil in the treatment of mild or moderate Alzheimer's disease. Neurology. 1999;52:1138–1145. doi: 10.1212/wnl.52.6.1138. [DOI] [PubMed] [Google Scholar]
- Stein K. Rivastigmine (Exelon) in the treatment of senile dementia of the Alzheimer type (SDAT) Bristol: NHS Executive South and West; 1997. [Google Scholar]
- Getsios D, Caro JJ, Caro G, Ishak K. Assessment of health economics in Alzheimer's disease (AHEAD): galantamine treatment in Canada. Neurology. 2001;57:972–978. doi: 10.1159/000064929. [DOI] [PubMed] [Google Scholar]
- Caro JJ, Salas M, Ward A, Getsios D, Mehnert A. Economic analysis of galantamine, a cholinesterase inhibitor, in the treatment of patients with mild to moderate Alzheimer's disease in the Netherlands. Dement Geriatr Cogn Disord. 2002;14:84–89. doi: 10.1097/00005650-199901000-00005. [DOI] [PubMed] [Google Scholar]
- Neumann PJ, Kuntz KM, Leon J, Araki SS, Hermann RC, Hsu MA, et al. Health utilities in Alzheimer's disease: a cross-sectional study of patients and caregivers. Med Care. 1999;37:27–32. doi: 10.2165/00002512-200421090-00005. [DOI] [PubMed] [Google Scholar]
- Jones RW, McCrone P, Guilhaume C. Cost effectiveness of memantine in Alzheimer's disease: an analysis based on a probabilistic Markov model from a UK perspective. Drugs Aging. 2004;21:607–620. doi: 10.2165/00002512-200421090-00005. [DOI] [PubMed] [Google Scholar]


