Abstract
Background
Effective interventions are needed for women long overdue for screening mammography.
Purpose
To pilot test an intervention for motivating overdue women to receive a mammogram.
Methods
Subjects age 45–79 without a mammogram in >=27 months and enrolled in study practices were identified from claims data. The intervention included a mailed, educational booklet, computer-assisted barrier-specific tailored counseling and motivational interviewing and facilitated, short-interval mammography scheduling.
Results
Of 127 eligible women, 45 (35.4%) agreed to counseling and data collection. Most were >=3 years overdue. Twenty-six (57.8%) of counseled women got a mammogram within 12 months. Thirty-one (72.1%) of 43 counseled women moved >=1 stage closer to screening, based on a modified Precaution Adoption Process Model.
Conclusion
It is feasible to reach and counsel women who are long overdue for a mammogram and to advance their stage of adoption. The intervention should be formally evaluated in a prospective trial comparing it to control or to proven interventions.
Keywords: mammogram, overdue, screening, telephone counseling
Introduction
Receipt of a screening mammogram every 1–2 years has been shown to reduce breast cancer mortality (1, 2). But at any given time about 15 million women aged 50–74 in the United States are overdue for a mammogram (3–5). Breen et al. (6) have reported a significant drop in the percent of women up to date with screening from 78.6% to 71.8% between 2000 and 2005. The fall has been most pronounced among women with higher incomes, private insurance and a usual source of care (6). For some women access to mammography is a critical barrier to regular screening, but for the majority women in the United States a host of other correlates of nonadherence likely affect utilization: failure of providers to recommend mammograms (7, 8), limited knowledge, low perceived vulnerability, and several psychological factors (9–12). Mailed and telephone reminders, face to face and telephone counseling have been shown to modestly improve mammography utilization (13), Although combined mail and telephone interventions have shown promise (14), research has not yet identified the optimum, most cost effective approach, or a counseling model that is effective among women who may have significant resistance to mammography.
We report the results of a pilot study of stage-based, tailored, computer-assisted telephone counseling intervention to promote screening among women long overdue for a mammogram and especially for those who might be resistant to screening. The intervention was enhanced with print materials, motivational interviewing, and facilitated scheduling so we could measure the effectiveness of a maximally intensive intervention in this challenging population.
Method
The study was approved by the University of Massachusetts Medical School Human Subjects Committee and was conducted between 2003–2006 in UMass Memorial Health Care (UMMHC) primary care practices in central Massachusetts. We used claims data from a large statewide health plan to identify 325 women aged 45–79 cared for by UMMHC primary care providers (PCPs) who had no claim for a mammogram within the prior 27 months. Eighty-four community-based PCPs with >=5 eligible patients and university-based PCPs with >=2 eligible patients were contacted. Fifty-seven (67.9%) agreed to participate, were sent a list of eligible women, and were asked to exclude those with a history of breast cancer and those for whom they did not recommend screening mammograms (e.g. because of limited life expectancy). All subjects had health insurance that covered screening mammograms.
Theoretical Basis of the Intervention
The Precaution Adoption Process Model (PAPM) (15) and the Transtheoretical Model (TTM) (16) are stage-based theories with roots in social learning theory and the health belief model. Both assert that the adoption of a health behavior proceeds through distinct stages. The PAPM stages are: 1) Unaware (never heard of the risk/screening test), 2) Unengaged (aware of and acknowledges others’ risks), 3) Undecided/Deciding (acknowledges personal risk and is deciding), 4) Decided No, 5) Decided Yes/Planning, 6) Acting (adopts the behavior), and 7) Maintenance (repeats the behavior). The TTM combines the PAPM stages 1–4 into a single stage (precontemplation). We have found that the greater specificity of the PAPM facilitates more precise tailoring of counseling to precontemplators, so we used it in developing our intervention.
Based on findings from focus groups we conducted with women overdue for mammograms, we created sub-classifications for women in PAPM Stages 4, and 5 (17). We classified women in Stage 4 (Decided No) as either Stage 4a (Definite No: would never get a mammogram) or Stage 4b (Qualified No: would consider getting a mammogram if their perceived risk increased). We created 3 subgroups within Stage 5 (Decided Yes/Planning): Stage 5a (Decided Yes: plan to get mammograms at greater than 2 year intervals and/or no plans to get one in the next 3 months); Stage 5b (Decided Yes: plan to get a mammogram in next 3 months but unwilling to commit to a specific date) and Stage 5c (Decided Yes: ready to schedule a mammogram) (17). We used this revised staging in the counseling protocol for this study.
Procedures
Developing the Intervention
We used a computer-assisted telephone interviewing (CATI) technique to maximize fidelity to the counseling protocol. The technique involves: 1) prompting the interviewer with the text of statements and queries on a computer screen, 2) interviewer entry of the subject’s responses into the computer and 3) display of the next appropriate screen based on an algorithm.
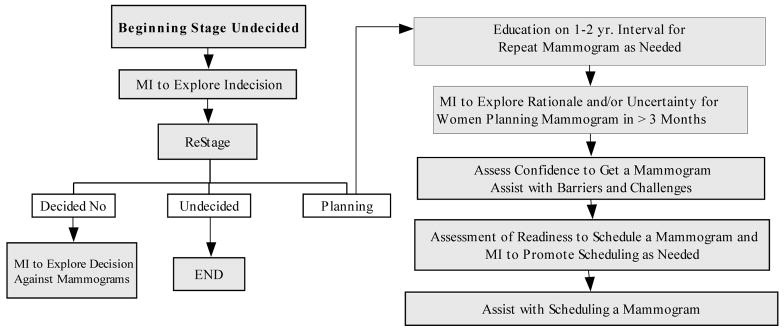
To address the resistance to screening we anticipated among women long overdue for a mammogram, we added a motivational interviewing (MI) component. Developed by addiction specialists seeking to change behaviors in individuals with alcoholism (18), MI has been adapted for use with smoking, drug abuse, diabetes management, diet, exercise and other health related behaviors (19–21). MI is a patient-centered counseling approach that emphasizes a collaborative relationship between patient and counselor and exploration of concerns, of ambivalence and of reasons and resources for change, as well as building self-efficacy while attempting to minimize resistance. We used MI principles (18) to develop counseling modules that focused on exploration of the importance the subject attaches to screening, assessment of a woman’s confidence in her ability to get a mammogram, and on the concerns of women who had decided against screening or were undecided. The counseling script and protocol were also informed by a barrier-specific counseling script that we had used in a previous mammography screening study (22), and our previous work on a colon cancer counseling CATI system (23). A simplified CATI algorithm for women in Stage 3 (Undecided/Deciding) is shown in Figure 1.
Figure 1. CATI algorithm for stage 3 women: undecided/deciding*.
MI = motivational interviewing
Others have demonstrated that printed materials can augment the effect of a counseling call (24). We developed and pre-tested a booklet with sections on the nature of breast cancer, breast cancer risk, screening guidelines, mammograms and several graphics, one illustrating the size of cancers detectable by mammography compared to the much larger size usually identified by clinical breast exam. Women received the booklet before the call, and counselors referenced it during the call. Others have shown that scheduling a mammogram during a counseling call improves the likelihood of completion (25) so counselors were prepared to facilitate scheduling. Because wait time can influence completion rate, we arranged to have appointments available within 2 weeks rather than the usual wait times of 3 to 6 months.
Intervention Implementation
All provider-approved women were sent a letter signed by their PCP explaining the study, recommending a mammogram, and encouraging participation in the study. One week after a letter was sent the study assistant called the recipient, confirmed eligibility, obtained consent, administered a baseline survey, made an appointment for the woman to talk with the counselor and sent the mammography booklet. Up to 10 call attempts were made. Subsequently, because getting women to answer the initial call was time-consuming, we condensed the eligibility, consent and baseline survey call and the counseling call into one call.
Outcome Measures
Using our amended PAPM staging, the counselor staged women at the beginning of the counseling call and at the end. Receipt of a mammogram within 12 months of the first attempt to reach the patient was determined based on claims data from the HMO. Change in stage and receipt of a mammogram were the primary outcomes.
Statistical Analysis
For all eligible women receipt of a mammogram was compared by counseled status. Fisher’s exact test was used to statistically test differences in the distribution of characteristics across stages, in the proportions of women receiving mammograms and in rates of counseling and mammography across PCPs. Ninety-five percent confidence intervals were calculated without continuity correction using the VassarStats statistics calculator (26), which is based on the procedure outlined by E. B. Wilson (27).
Results
Sample Selection and Characteristics
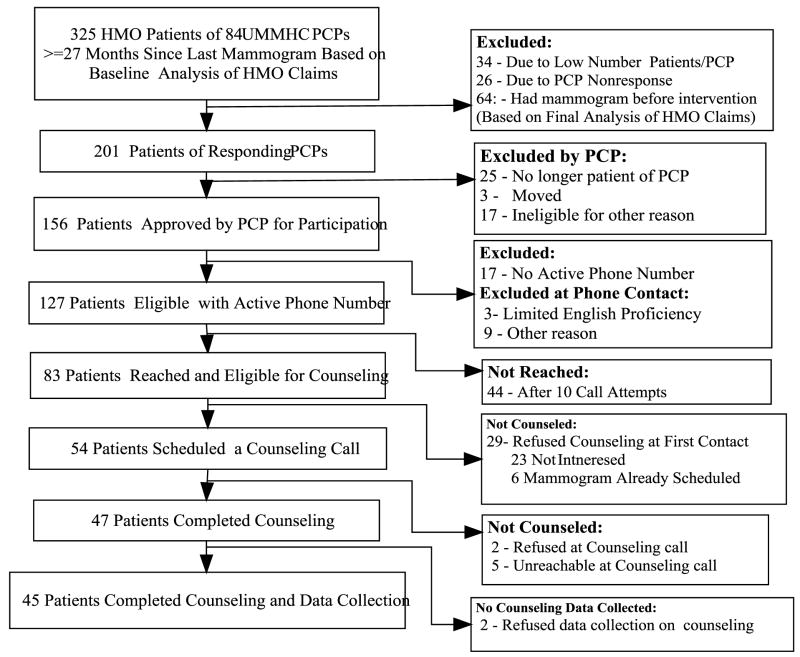
Figure 2 shows the exclusions, failures to contact patients, and the refusals that led to a final counseled sample of 45 patients with complete data. These 45 counseled women were distributed relatively evenly across providers with eligible patients. The association between PCP and percent of eligible patients counseled was statistically insignificant (p=0.247). Selected characteristics of the 45 counseled women included age: 24.4% were aged 45–49, 28.9% were aged 50–59 and 46.6% were 60 and older. Time since last mammogram varied from 35 to > 60 months: 20% of the women had had a mammogram between 35 and 47 months, 6.7% between 48–59 months and 62.2% had not had a mammogram for 60 or more months. There were 11.1% who had never had a mammogram. Regarding education level, 9.3% of them reported less than a high school education, 30.2% no education beyond high school, 20.9% some college, and 39.6% a college or post-graduate degree. Of those who had received a mammogram (n=40), 55% reported that they usually tried to get a mammogram every 2 years while 20% endorsed an interval of 3–5 years and the rest (25%) reported getting a mammogram only if they had a breast problem or when recommended by their physician. Most (67.4%) reported that they got regular medical check-ups. The annual household income ranged from less than $25,000 (12.9%) to greater than $65,000 (41.6%), with the rest (46.2%) reporting incomes from $25,000–64,999.
Figure 2.
Flow diagram of subject eligibility, PCP approval, participation and counseling
Outcomes
At the beginning of the call, 13 women (28.9%) were in Stages 2–4 (Not Planning), with 5 decided against screening (Stage 4) and 7 undecided (Stage 3). 32 (71.1%) of the women were in Stage 5 (Decided Yes/Planning) with 7 planning in >3 months (Stage 5a) 13 planning within 3 months (Stage 5b) and 2 already scheduled for a mammogram (Stage 5c). Those not planning a mammogram were more likely to be 60 years old or older compared to those planning (69.2% vs. 36.7%, p=.066). Those not planning were also more likely to have limited education (less than high school) (23.1% vs. 3.5% p=.063), and to have never had a mammogram (23.1% vs. 6.7%, p=.153).
At the end of the counseling call, 72%, (95% CI 57.3, 83.3) of the 43 women with no mammogram scheduled at the beginning moved at least one stage higher in the direction of getting a mammogram. 60% (95% CI 45.6, 73.6) of these 43 women scheduled a mammogram and 16.7% (95% CI 13.2, 37.8) more stated a desire to get a mammogram. Of the 13 women not planning a mammogram at the beginning of the call, 7 ((53.9% (95% CI 29.2, 76.8)) moved at least one stage higher towards getting a mammogram, with 3 scheduling a mammogram and another 3 stating the intention to get one.
Regarding mammography completion, of the 32 women planning a mammogram at the beginning of the call, 56.3% (95% CI 37.9, 73.2) received a mammogram. Of the 13 women not planning at the beginning of the call, 38.5% (95% CI 15.1, 67.7) got a mammogram. 23 women were contacted who did not have a mammogram scheduled but refused counseling. Only 2 (8.7%) got a mammogram. Of the 44 women who could not be contacted, 20.5% got a mammogram. Table 1 shows the proportion of women counseled who eventually received a mammogram by their stage at the end of the call. Mammogram completion was assessed at 12 months following the call. Of the 38 women who “Decided Yes” at the end of the call, 60.5% received a mammogram. Of the entire counseled group, 26 ((57.8% (95% CI 43.3, 72.0)) got a mammogram while of the 80 women who appeared eligible but did not receive counseling, only 21.3% received a mammogram (57.8% vs. 21.3%, p<.001). Overall 43 (34.4%) of the 125 eligible women with data received a mammogram over the 12-month follow-up period.
Table 1.
Distribution of Subjects by Revised PAPM Stage at End of Counseling Call And Percent Receiving a Mammogram
| Received Mammogram | ||||
|---|---|---|---|---|
| Stage Number | Stage Name | Stage at End of Call n (%) | (%) | 95% CI |
| 3 | Deciding/Undecided | 6 (13.3) | 3/6 (50) | 18.8, 81.2 |
| 4a | Decided No (Never) | 1 (2.2) | 0/1 (0) | 0, 79.4 |
| 4b | Decided No (Not now) | 0 | -- | -- |
| 5a | Decided Yes (Not within 3mo.) | 0 | -- | -- |
| 5b | Decided Yes (Within 3 mo. but No Specific Date) | 10 (22.2) | 2/10 (20) | 5.7, 51.1 |
| 5c | Decided Yes (Specific Date and Scheduled) | 28 (62.2) | 21/28 (75.0) | 56.6, 88.6 |
| Total | 45 (100) | 26/45 (57.8) | 43.3, 72.0 | |
For 6 of 16 PCPs with counseled patients, all patients counseled received a mammogram. None of the counseled patients of 2 PCPs received a mammogram while for the rest of the PCPs with counseled patients the proportion receiving a mammogram ranged from 33–75%. The association between PCP and proportion of counseled women receiving a mammogram was statistically significant (p=0.048). Women who did not receive counseling were distributed relatively evenly across the PCPs with subjects per PCP ranging from 2 to 8. Mammography rates among those not counseled did not differ significantly by PCP (p=0.189)
Practice Implications
36% of eligible women in this pilot study were reachable and agreeable to counseling, a response rate high enough to make further study of the intervention potentially worthwhile. Most of the counseled women (71.1%), were planning on getting a mammogram “sometime”, but only 2 had already scheduled one, and 13 (40.6%) had no near term date in mind. However 63% of eligible women avoided counseling, by not responding to phone messages, or by refusing participation when contacted. For women who never responded to calls, we cannot be sure about the reasons for nonresponse. Reasons could include failure to receive a voice mail or to remember to return the call as well as explicit avoidance of counseling. We do know that nonresponders had a low follow-up mammography rate (21%), suggesting that they are on the whole reluctant to receive mammograms. Women without a scheduled mammogram who were successfully contacted but refused counseling had a particularly low rate of mammography (9%), suggesting that direct refusal of counseling is a strong marker for resistance to obtaining mammograms. It is difficult to envision a telephone intervention that would be effective for nonresponders and those refusing counseling, although in-person counseling in the context of an office visit could be an option worth exploring.
Of the counseled women planning but not scheduled, 76.7% went on to schedule a mammogram by the end of counseling and of these 79% completed the mammogram. Fourteen of the 26 (53.8%) mammograms completed by counseled women occurred within 4 weeks. The modest success of this short interval scheduling for some counseled women provides some of the strongest evidence that our intervention may reduce the time to next mammogram, because only women in this study could schedule a mammogram within 4 weeks, compared to 4 months or longer for others. However, without a true control group we could not directly measure the reduction in time to mammogram attributable to the intervention or determine if it is clinically meaningful.
Of the women who at the end of the call said they were “planning” but refused to schedule, only 20% got a mammogram. This suggests that stated intention when not coupled with scheduling belies an underlying ambivalence or persistent procrastination. It remains to be seen if any kind of intervention can be effective in this group but further study of this group is warranted. While only 13 women who received counseling were “not planning” at the start of counseling, these women were key targets of the study. Two of the 13 reported a decision to never get a mammogram, and 1 of these moved to the deciding stage. Of the other 11 women, 6 moved to “planning”, 3 scheduled one, and 5 received a mammogram. Despite the small sample size, our findings suggest that some women explicitly ambivalent about and/or resistant to mammography can be engaged by telephone counseling and moved to accept mammography. All women, counseled or not, who scheduled a mammogram had about the same rate of completing it, (79% for counseled women vs. 83% for those not counseled). This suggests that making the commitment to be screened strongly predicts completion.
Given the association between PCP and proportion of counseled women receiving a mammogram, it is conceivable that there could be an interaction between the effect of counseling and PCP. That is, counseling might be more effective among patients of some PCPs, possibly because the PCP is more supportive of mammography or because the PCP attracts women more likely to respond to counseling. However, it does not appear that a particular PCP behavior is required for counseling to have an impact, since counseled women who received a mammogram could be found in 15 of 17 PCPs with counseled subjects in their practices.
This intervention has not been yet been evaluated in a prospective randomized intention-to-treat study. Nonetheless, health systems may wish to implement it in some way. For example, a cost-effective stepwise outreach strategy could cull those not resistant to screening from those more reluctant or resistant and needing more attention. Some of those who were long overdue could undoubtedly be moved to mammography completion by simpler interventions such as a reminder letter or a reminder call that included scheduling possibilities. The complex counseling intervention described in this pilot study could then be saved for the non-responders. This type of outreach system (reminders followed by counseling) could be adopted and maintained as a centralized service provided to multiple primary care practices linked through information systems. The most likely early adopters of this type of service would be large integrated health care networks (IHN). Financial support for the service could come from several sources: revenue generated by additional mammograms and follow-up studies and from incentive payments from managed care organizations (MCO) for high levels of patient compliance with mammography. We are currently implementing a centralized mammography reminder and counseling system in an IHN that serves 34,000 women age 40 and older and will be working with IHN leadership and MCOs to develop a strategy for ongoing financial support of the system.
Study Limitations and Strengths
The comparisons between mammography outcomes among the counseled and not counseled groups must be interpreted cautiously because this is a non-randomized small pilot study. Women who can be contacted and agree to counseling are different from those who cannot be contacted or refuse counseling. However, we did exclude the possibility that there was clustering of patients who were seen by the same provider, that is, that patients of one provider were more (or less) likely to be counseled or to get mammograms than patients of another provider. This is key as PCP recommendation is a known predictor of patient behavior and mammography adherence. Nonetheless, we cannot conclude that the relatively high mammography rate in the counseled women was due to counseling. The study sample was small and included a homogenous group of women, mostly middle class and Caucasian, so the findings suffer from statistical imprecision and may not be generalizable to women from other racial/ethnic groups or socioeconomic strata.
Strengths of the study include the initial identification of only those women with mammogram coverage from their health insurance and who had received a recommendation from their PCP to get a mammogram. Another strength is the selection of a sample reasonably representative of middle class white women in the health care network studied. While it is possible there are important differences between women in Central Massachusetts and other parts of the country it seems reasonable to cautiously generalize our findings to white, middle class, insured American women long overdue for a mammogram.
Conclusions
It is feasible to deliver a complex telephone counseling intervention to a substantial number of women who are long overdue for a mammogram, although many women will likely passively or actively refuse this type of intervention. It is probable that the intervention will reduce the time to next mammogram for some of those counseled, but further study is needed to confirm this finding and to determine if it is clinically meaningful. To advance the goal of identifying the most cost-effective means of reducing time to next mammogram among overdue women, a large randomized trial is needed that compares the effectiveness of our enhanced intervention to selected less intense, less costly, and less complex interventions (e.g. a simple reminder and scheduling calls, with/without short-interval scheduling) and to controls.
Acknowledgments
This work was supported by National Institutes of Health, National Cancer Institute Grant: R21 100286. We thank Amin Vidal for his technical expertise in developing the CATI system. All patient/personal identifiers have been removed or disguised so the participants described are not identifiable. All participants gave their informed consent to data collection and, if appropriate, to telephone counseling.
References
- 1.Nystrom L, Rutquist LE, Wall S, et al. Breast cancer screening with mammography: An overview of Swedish randomized trials. Lancet. 1993;341:973–978. doi: 10.1016/0140-6736(93)91067-v. [DOI] [PubMed] [Google Scholar]
- 2.Jonsson H, Tornberg S, Nystrom L, Lenner P. Service screening with mammography of women aged 70–74 years in Sweden: Effects on breast cancer mortality. Cancer Detection and Prevention. 2003;27(5):360–369. doi: 10.1016/s0361-090x(03)00131-4. [DOI] [PubMed] [Google Scholar]
- 3.Rakowski W, Breslau ES. Perspectives on behavioral and social science research on cancer screening. Cancer. 2004;1(5 Suppl):1118–1130. doi: 10.1002/cncr.20503. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Use of mammograms among women aged >/= 40 years—United States, 2000–2005. MMWR – Morbidity and Mortality Weekly Report. 2007;56(3):49–51. [PubMed] [Google Scholar]
- 5.U.S. Census Bureau. Statistical abstract of the United States: 2001.
- 6.Breen N, Cronin KA, Meissner HI, et al. Reported drop in mammography: Is this cause for concern? [Accessed 2007 May 14];Cancer Online. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 7.NCI Breast Cancer Screening Consortium. Screening mammography: A missed clinical opportunity. Results of the NCI breast cancer screening and national health intervew studies. Journal of the American Medical Association. 1990;264(1):54–58. [PubMed] [Google Scholar]
- 8.Costanza ME. The extent of breast cancer screening in older women. Cancer. 1994;74(7 suppl):2046–2050. doi: 10.1002/1097-0142(19941001)74:7+<2046::aid-cncr2820741710>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 9.Clemow L, Costanza ME, Haddad WP, et al. Underutilizers of mammography screening today: Characteristics of women planning, undecided about, and not planning a mammogram. Annals of Behavioral Medicine. 2000;22(1):80–88. doi: 10.1007/BF02895171. [DOI] [PubMed] [Google Scholar]
- 10.Rimer BK, Ross E, Cristinzio CS, King E. Older women’s participation in breast screening. Gerontology. 1992;47:85–91. [PubMed] [Google Scholar]
- 11.Glasgow RE, Whitlock EP, Valanis BG, Vogt TM. Barriers to mammography and pap smear screening among women who recently had neither, one or both types of screening. Annals of Behavioral Medicine. 2000;22(3):223–228. doi: 10.1007/BF02895117. [DOI] [PubMed] [Google Scholar]
- 12.Burton MV, Warren R, Price D, Earl H. Psychological predictors of attendance at annual breast screening examinations. British Journal of Cancer. 1998;77(11):2014–2019. doi: 10.1038/bjc.1998.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yabroff KR, Mandelblatt JS. Interventions targeted towards patients to increase mammography use. Cancer Epidemiology, Biomarkers and Prevention. 1999;8:749–757. [PubMed] [Google Scholar]
- 14.Legler J, Breen N, Meissner H, et al. Predicting patterns of mammography use: A geographic perspective on national needs for intervention research. Health Services Research. 2002;37(4):929–947. doi: 10.1034/j.1600-0560.2002.59.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weinstein ND. The precaution adoption process. Health Psychology. 1988;7:355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- 16.Prochaska JO, DiClemente C. Stages and processes of self-change of smoking: Toward an integrative model. Journal of Consulting and Clinical Psychology. 1983;51:390–393. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 17.LaPelle N, Costanza ME, Luckmann R, et al. Staging mammography non-adherent women: A qualitative study. Journal of Cancer Education. 2008;23(2):114–121. doi: 10.1080/08858190802039094. [DOI] [PubMed] [Google Scholar]
- 18.Miller W, Rollnick S. Motivational interviewing: Preparing people to change addictive behaviors. New York, NY: Guilford Press; 1991. [Google Scholar]
- 19.Rosal MC, Ebbeling CB, Ockene JK, et al. Facilitating dietary change: The patient- centered counseling model. Journal of the American Dietetic Association. 2001;101(3):332–341. doi: 10.1016/S0002-8223(01)00086-4. [DOI] [PubMed] [Google Scholar]
- 20.Emmons KM, Hammond K, Fava JL, et al. A randomized trial to reduce passive smoke exposure in low-income households with young children. Pediatrics. 2001;108(1):18–24. doi: 10.1542/peds.108.1.18. [DOI] [PubMed] [Google Scholar]
- 21.Emmons KM, Rollnick S. Motivational interviewing in health care settings: opportunities and limitations. American Journal of Preventive Medicine. 2001;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 22.Costanza ME, Stoddard AM, Luckmann R, et al. Promoting mammography: Results of a randomized trial of telephone counseling and a medical practice intervention. American Journal of Preventive Medicine. 2000;19(1):39–46. doi: 10.1016/s0749-3797(00)00150-1. [DOI] [PubMed] [Google Scholar]
- 23.White MJ, Stark JR, Luckmann R, et al. Implementing a computer-assisted telephone interview (CATI) system to increase colorectal cancer screening: A process evaluation. Patient Education and Counseling. 2006;61:419–428. doi: 10.1016/j.pec.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Rimer BK, Conaway M, Lyna P, et al. The impact of tailored interventions on a community health center population. Patient Education and Counseling. 1999 Jun;37(2):125–140. doi: 10.1016/s0738-3991(98)00122-0. [DOI] [PubMed] [Google Scholar]
- 25.Taplin SB, Barlow WE, Ludman E, et al. Testing reminder and motivational telephone calls to increase screening mammography: A randomized study. Journal of the National Cancer Institute. 2000;92(3):233–242. doi: 10.1093/jnci/92.3.233. [DOI] [PubMed] [Google Scholar]
- 26. [Accessed 3/24/08]; http://faculty.vassar.edu/lowry/prop1.html.
- 27.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Statistics in Medicine. 1998;17:857–872. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]