Abstract
Chronic dislocation of the elbow is an exceedingly disabling condition associated with severe instability, limitation of elbow function and significant pain. Due to the potentially conflicting goals of restoring elbow stability and regaining a satisfactory arc of motion, successful treatment is a challenge for the experienced trauma surgeon. We report our treatment strategy in three patients suffering from chronically unreduced fracture-dislocations of the elbow. The treatment protocol consists of in situ neurolysis of the ulnar nerve, distraction and reduction of the joint using unilateral hinged external fixation and repair of the osseous stabilizers. A stable elbow was achieved in all patients, without the need of reconstruction of the collateral ligaments. At final follow-up, the average extension/flexion arc of motion was 107° (range, from 100° to 110°). The average MEPI score at follow-up was 93, and the average DASH score was 19. This is a promising treatment protocol for the treatment of chronically unreduced complex elbow dislocations to restore elbow stability and regain an excellent functional outcome.
Keywords: Chronic elbow dislocation, Hinged external fixation, Elbow distraction, In situ neurolysis of ulnar nerve
Introduction
Dislocation of the elbow is a common orthopaedic injury with an incidence of approximately 20% of all articular dislocations [1]. After the shoulder, the elbow is the second most frequently dislocated major joint in adults [2] and the most frequently dislocated major joint in the paediatric population [3]. At least 80% of elbow dislocations are posterior or posterolateral [4, 5], resulting in most cases from a fall on the outstretched hand with the forearm pronated. Lateral, postero-medial, medial, or anterior and divergent dislocations (characterised by displacement of the radius from the ulna) are much less common. Neurovascular complications occur in 5–13% of elbow dislocations and include injury to the ulnar, median and, less frequently, radial nerves and the brachial artery, in most cases in open dislocations or penetrating injuries [5, 6].
Fortunately most elbow dislocations do not have concomitant fractures, and are termed “simple dislocations” [5]. Dislocations associated with fractures of the coronoid process, radial head or neck, distal humerus, or olecranon are termed “complex dislocations”. These injuries usually require surgery to restore the osseous stabilizers of the elbow joint.
Neglected elbow dislocations, incomplete examination and assessment of elbow instability, or inadequate therapy may lead to chronic dislocation of the elbow. This exceedingly disabling condition is generally associated with severe instability, limitation of elbow function and significant pain. If the elbow is not reduced, arthritic changes may develop rapidly [7]. The main goals of therapy, to restore a stable, concentric joint and regain a satisfactory arc of motion, are apparently conflicting, so successful treatment of chronic elbow dislocations is a challenge.
In the present study, we present a successful treatment protocol in chronically unreduced fracture-dislocations of the elbow, consisting of in situ neurolysis of the ulnar nerve, distraction and reduction of the elbow using unilateral hinged external fixation and repair of the osseous stabilizers of the elbow.
Materials and methods
We report the treatment of three male patients suffering from chronic fracture-dislocation of the elbow. The average age of the patients was 52 years (range, 29–68 years). In all of them the dominant limb was involved. The average duration of unreduced elbow dislocation was 10 weeks (range, from four to 16 weeks).
Patient 1 is a 29-year-old man who fell on his outstretched right arm and sustained a posterior dislocation of the right elbow. He was treated in an emergency department by closed reduction of the elbow joint and immobilisation in a posterior elbow splint, followed by physiotherapy and mobilisation of the elbow. Eighteen months later, the patient fell on to his outstretched right arm again while playing soccer and suffered a posterior dislocation of the elbow, this time associated with a type II fracture of the coronoid process as described by Regan and Morrey [8]. After reduction, the trauma surgeon repaired the medial collateral ligament with a suture anchor system and immobilised the joint in a posterior splint. When the patient first presented in our department 4 months after the index surgery, the arc of motion was limited to 30° (E/F 0/30/60°). Antero-posterior and lateral radiographs and a CT-scan showed a persisting posterior dislocation of the elbow (Figs. 1, 2).
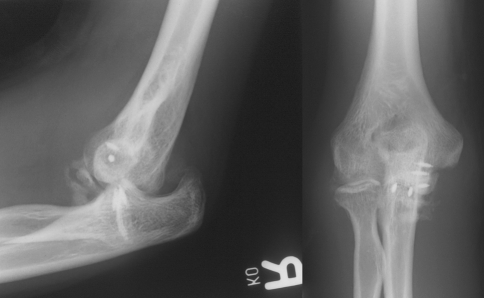
Fig. 1.
Antero-posterior and lateral radiographs of patient 1 demonstrating chronic elbow dislocation 12 weeks after the index operation
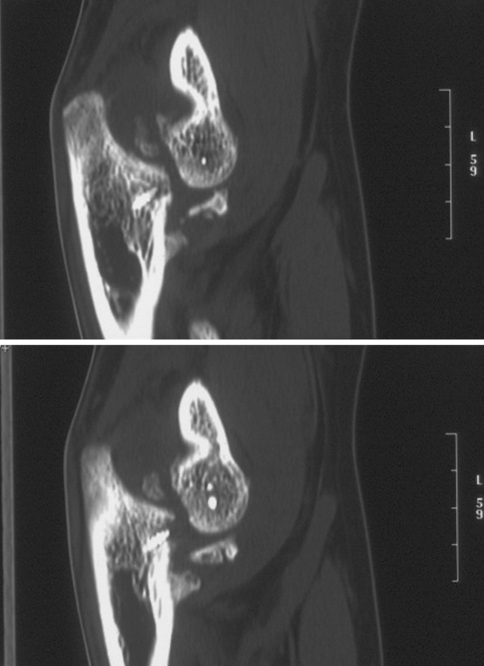
Fig. 2.
CT-scan of patient 1 12 weeks after the index operation
Patient 2 is a 68-year-old man who fell on his outstretched right arm and sustained a complex posterior dislocation of the right elbow associated with a type III fracture of the coronoid process [8]. He was treated in an emergency department by reduction and immobilisation of the elbow joint in a posterior splint for 2 weeks, followed by physiotherapy. Ten weeks after the injury the patient presented at our department with a contracture of the elbow in 20° of flexion. Radiographs and a CT-scan showed a chronic posterior dislocation of the elbow.
Patient 3 is a 59-year-old labourer who fell on his right arm and suffered a complex medial dislocation of the elbow associated with a type II fracture of the coronoid process. The receiving surgeons performed an indirect screw osteosynthesis of the coronoid fracture to restore the osseous stabilizer of the elbow. When the patient presented at our department 4 weeks after surgery, the elbow was stiff with an arc of motion of 30°. Radiographs and the CT-scan displayed chronic medial dislocation of the elbow and extensive heterotopic ossification. Therefore, prophylactic radiation was performed immediately before and after surgery.
Our surgical treatment of the three patients was the same and comprises the following procedures:
Initially, in situ neurolysis of the ulnar nerve was performed between the arcade of Struthers and the Osborne fascia, using a curved incision over the cubital tunnel. The wound was left open to allow observation of the tension in the ulna nerve during distraction and reduction of the elbow. Closed reduction (pat. 1, 2) was carried out by distraction of the elbow and application of the hinged humero-ulnar fixator with motion capacity (Elbow fixator Orthofix Srl, Bussolengo, VR, Italy). Patient 3 required an open reduction due to heterotopic fibrous tissue and ossification, using a limited lateral approach as described previously [9, 10]. The elbow was positioned horizontally with the medial side down and a true lateral view of the elbow was obtained with fluoroscopy, showing the ring structures of the trochlea as a perfect circle. The tip of a 2.0 mm K-wire was placed on the proximal border of the circle and drilled through the lateral epicondyle. The part of the K-wire protruding out of the skin was bent if necessary to be parallel to the axis of rotation, appearing as a dot on the lateral view. The fixator was slid over the K-wire and used as its own template for positioning of the humeral and ulnar screws [11]. It was then removed and two temporary screws inserted into the lateral aspect of the olecranon for mounting the T-clamp of the distraction fixator. Using a standard Orthofix fixator and a standard compression–distraction unit, distraction of the humero-ulnar joint was performed twice over a period of 10 min upto a distraction distance of 15 mm confirmed by fluoroscopy. After the second distraction, the temporary olecranon screws were removed and the hinged elbow fixator mounted using a standard protocol [11]. The fixator was used to reduce the elbow in all cases. The definite and concentric distractions of the joint-space were adjusted using small in-built distractors on the humeral and ulnar links of the fixator. If there was impingement of the coronoid process or persisting subluxation, distraction along the ulnar fixator link was performed for perfect congruency. The fixator was locked in flexion while monitoring the tension of the ulnar nerve by direct vision.
As biomechanical studies have emphasized the important role of the coronoid process for posterior, posterolateral and varus stability of the elbow [12], reconstruction of the coronoid process in chronic posterior dislocation of the elbow is of considerable importance [13]. In a second operation 10 days after reduction and fixator application, the coronoid fracture was repaired through a ventral muscle splitting approach using a custom-made plate osteosynthesis, after corrective osteotomy of the displaced and/or deformed coronoid process (pat. 1 and 2; Fig. 3). The elbow fixator maintained distraction of the joint and was covered by sterile towels during the operation. After the second surgery, the fixator was locked in flexion for another 4 days. Thereafter elbow motion was started by unlocking the central unit of the fixator; extension was limited to 30° for 3 weeks by incorporating a extension limit block into the fixator. Physiotherapy exercises were carried out twice a day. Using the compression/distraction unit of the fixator, the fixator was locked at night in maximum flexion and extension alternately. Pin site care was performed with a proprietary antiseptic (Octenisept®, Schülke and Mayr GmbH, Norderstedt, Germany) and dry wound dressing on a weekly basis; to avoid heterotopic ossification and to reduce pain, indomethacin was prescribed 50 mg bid with gastric protection for 6 weeks after surgery. The fixator was removed 8 weeks after the index procedure as an outpatient procedure.
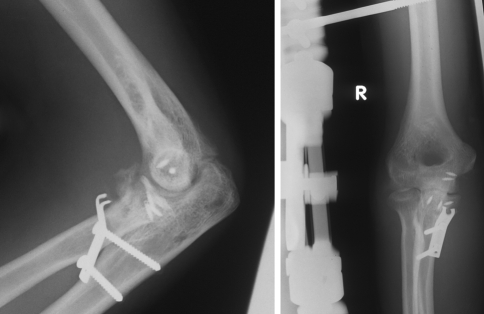
Fig. 3.
Antero-posterior and lateral radiographs of patient 1 after distraction and reduction of the elbow using hinged external fixation and repair of the coronoid process, demonstrating a concentric joint-space
At follow-up, the arc of motion of the elbow was recorded and the stability of the elbow joint tested on examination. Radiographs in two planes were taken to assess articular alignment and post-traumatic arthrosis. Patients were evaluated using the Mayo Elbow Performance Index (MEPI) [14] and the Disabilities of the Arm, Shoulder, and Hand (DASH) instrument [15] before the index operation and at final follow-up.
Results
No peri- or postoperative complications were recorded. No pin-site infections occurred. No re-dislocation was recorded. The average period of follow-up was 32 months (range 12–64). Clinical examination at follow-up revealed no evidence of elbow instability. The average range of motion at follow-up was 107° with regard to extension/flexion (range 100–110°); forearm rotation was not restricted in any patient. No ulnar nerve dysfunction was observed.
Radiographs at follow-up revealed concentric reduction and anatomic alignment of the ulno-humeral and the radio-capitellar joints in all patients. Radiographs of two patients showed mild heterotopic ossification near the collateral ligaments; in one patient, additional heterotopic ossification of the ventral and dorsal capsule was detected. Radiographs of two patients showed moderate joint-space narrowing and osteophyte formation. The results of the evaluation at follow-up using the MEPI-score [14] and the DASH-score [15] are given in Table 1.
Table 1.
Data of three patients with chronically unreduced complex elbow dislocations
| Type of injury | Duration of dislocation | Range of motion at FU | MEPI-score pre/post operation | DASH-score pre/post operation | |
|---|---|---|---|---|---|
| Pat. 1 (m, 29 years) | Complex posterior dislocation with type II fracture of coronoid process | 16 weeks | 110° (E/F 0/20/130°) |
45/95 | 72/20 |
| Pat. 2 (m, 68 years) | Complex posterior dislocation with type III fracture of the coronoid process | 10 weeks | 100° (E/F 0/15/115°) |
25/90 | 78/16 |
| Pat. 3 (m, 59 years) | Complex medial dislocation with type II fracture of the coronoid process | 4 weeks | 110° (E/F 0/20/130°) |
20/95 | 70/20 |
Discussion
Due to the apparently conflicting goals of restoring elbow stability and regaining a satisfactory arc of motion, treatment of chronic elbow dislocation is still a challenge for the experienced trauma surgeon. Prolonged dislocation of the elbow causes contracture and fibrosis of the joint capsule and ligaments and shortening of the triceps muscle, leading to consolidation of the dislocation. The standard treatment of chronic elbow dislocations has consisted of open reduction, v-y-muscleplasty of the triceps and temporary arthrodesis and/or cast immobilisation (Table 2; for review: Lyons et al. (2008) [16]). However, prolonged postoperative immobilisation is problematic as it may lead to elbow stiffness. In 2001, Ruch and Triepel [17] reported successful treatment of five patients suffering from recurrent or chronically persisting elbow dislocations after failure of the initial operative or non-operative treatment, using hinged external fixation as an alternative to complete osseous and ligamentous reconstruction. Subsequently, several reports have been published of successful treatment of chronic elbow dislocations using hinged external fixation with or without repair or reconstruction of the collateral ligaments [7, 18–22] (Table 2). While preserving mobility of the elbow, hinged humero-ulnar fixation provides guided stability to the joint. The soft tissues heal in a directed mode and lead to re-establishment of the ligament apparatus, and repaired or reconstructed collateral ligaments are protected [11].
Table 2.
Literature overview: treatment strategies of chronic elbow dislocations
| Author | Number of patients, duration of elbow dislocation | Treatment |
|---|---|---|
| Balchandani et al. (1969) [23] | 19 patients, duration unclear | Open reduction |
| Ashby et al. (1974) [24] | Three patients, duration 3–18 months | Open reduction |
| Krishnamoorthy et al. (1976) [25] | 26 patients, duration 2 weeks–8 months (average 7 weeks) | Open reduction |
| Billett (1979) [26] | Six patients, duration 1–3 months | Open reduction, v-y-muscleplasty, temporary arthrodesis |
| Dryer et al. (1980) [27] | Four patients, duration unclear | Open reduction |
| Naidoo (1982) [28] | 23 patients, duration 1 month–2 years | Open reduction, v-y-muscleplasty, temporary arthrodesis |
| Fowles et al. (1984) [29] | 15 patients, duration 3 weeks–3 years | Open reduction, v-y-muscleplasty, temporary arthrodesis, decompression of ulnar nerve |
| Martini et al. (1984) [30] | 47 patients, duration 1 month–25 years | Open reduction, v-y-muscleplasty, temporary arthrodesis, transposition of ulnar nerve |
| Arafiles (1987) [31] | 11 patients, duration 1–48 months (average 9 months) | Open reduction, tendon graft stabilisation |
| di Schino et al. (1990) [32] | 81 patients, duration 1–>12 months | Open reduction, v-y-muscleplasty, resection of distal humerus, decompression of ulnar nerve |
| Bruce et al. (1993) [33] | One patient, duration 5 weeks | Open reduction, temporary humero-radial arthrodesis, decompression of ulnar nerve |
| Moritomo et al. (1998) [34] | Two patients, duration 4–6 months | Open reduction, reattachment of the medial collateral ligament, reconstruction of the coronoid |
| Ruch et al. (2001) [17] | Five patients, duration at least 6 weeks | Hinged external fixation |
| Jupiter et al. (2002) [7] | Five patients, duration 6–30 weeks (average 11 weeks) | Open reduction, hinged external fixation, reattachment of the lateral soft tissue envelope, anterior subcutaneous transposition of ulnar nerve |
| Devnani et al. (2004) [35] | Nine patients, duration 1, 5–30 months (average 8 months) | Open reduction, excision of collateral ligaments, temporary arthrodesis, anterior transposition of ulnar nerve |
| Lo et al. (2004) [19] | One patient, duration 1 month | Open reduction, hinged external fixation, decompression of ulnar nerve |
| Ring et al. (2004) [21] | 13 patients, duration 1–5 months (average 2 months) | Open reduction, preservation or reconstruction of coronoid process and radiocapitellar contact, repair or reconstruction of lateral collateral ligament, hinged external fixation, anterior subcutaneous transposition of ulnar nerve |
| Mahaisavariya et al. (2005) [36] | 24 patients, duration 1–60 months (average 8 months) | Open reduction, repair of collateral ligaments, v-y-muscleplasty, temporary arthrodesis |
| Mighell et al. (2005) [37] | Six patients, duration 5–52 weeks (average 17 weeks) | Primary semi-constrained total elbow arthroplasty |
| Ohno et al. (2005) [20] | One patient, duration 2 years | Open reduction, reconstruction of collateral ligaments, decompression of ulnar nerve, hinged external fixation |
| Sunderamoorthy et al. (2005) [22] | One patient, recurrent dislocations, duration 3 weeks and 2 weeks | External fixation and transolecranon pin |
| Degreef et al. (2007) [18] | One patient, duration 11 weeks | Open reduction, repair of collateral ligaments, hinged external fixation |
| Majima et al. (2007) [38] | Three patients, duration 3–4 months | Open reduction, reconstruction of collateral ligaments, anterior subcutaneous transposition of ulnar nerve |
As reported here our treatment strategy consists of initial in situ neurolysis of the ulnar nerve. Prolonged dislocation of the elbow leads to extensive fibrosis around the nerve, and significant tension is applied to it during reduction and flexion. We prefer in situ neurolysis as in vivo rabbit studies have demonstrated that transposition of the nerve leads to a significant loss of nerve conduction velocity and a deleterious change of the elastic properties of the ulnar nerve (unpublished data). Subsequently closed or, if not possible, open reduction of the elbow is performed after closed mechanical distraction. Recent biomechanical studies of the forces acting on the elbow joint during distraction have shown that at least 1000 Newton act on the joint and fixator construct and that distraction of 15 mm (for two times during the index operation) does not lead to any disruption of the ligaments or joint capsule. In agreement with recent reports [7, 17, 19], we do not reconstruct the collateral ligament complex, as it becomes re-established during healing restoring stability to the elbow joint with no need of formal ligament reconstruction. This is especially true when a hinged fixator is used, because it has been shown to modulate and re-establish a biomechanically stable ligament complex [11]. At follow-up none of our patients showed evidence of joint instability. As post-traumatic elbow stiffness is a common problem in reconstructive elbow surgery, a mechanical distraction technique was established using a hinged humero-ulnar fixator to distract the articular surfaces and contracted joint capsule and ligamentous structures [9, 10]. The elbow fixator enables distraction to be maintained along the humeral and ulnar fixator links, withstands the forces tending to redislocate the joint and controls the intraarticular surface pressure of the ulno-humeral and radio-capitellar joints. If there is a deficit in flexion or extension, a compression–distraction unit can be used to increase flexion and extension stepwise, whereas pronation and supination are not affected by the fixator. In a second step and after a definitive relaxation period, with the elbow fixator maintaining reduction and distraction of the joint, repair of the coronoid process as an osseous contributor to elbow stability was performed as described above.
At follow-up all patients achieved an excellent functional outcome with an average arc of motion of 107° with respect of flexion/extension and no residual elbow instability. Our results are in line with recent reports demonstrating that hinged humero-ulnar external fixation is a promising tool in the treatment of chronic elbow dislocations to restore stability and to regain a satisfactory arc of motion. In addition, the monolateral hinged elbow fixator enables mobilisation of the elbow under continuous joint distraction to improve the functional outcome. Successful treatment of chronic elbow dislocations remains a challenge, and treatment of acute elbow dislocations, including skilled examination and assessment of elbow instability should be performed by experienced personnel to avoid this painful and disabling complication.
Conclusion
Due to the apparently conflicting goals of restoring elbow stability and regaining a satisfactory arc of motion, treatment of chronically unreduced elbow dislocations is a challenge for the experienced trauma surgeon. Over time treatment strategies have been modified, and recently, several reports of successful treatment of chronic elbow dislocation using hinged external fixation have been published. Our defined treatment protocol comprises in situ neurolysis of the ulnar nerve, distraction and reduction of the joint using unilateral hinged external fixation enabling continuous joint distraction and repair of the osseous stabilizers; it provides a successful tool to restore elbow stability and regain an excellent functional outcome without the need for collateral ligament reconstruction.
References
- 1.Jupiter JB (1992) Trauma to the adult elbow fractures of the distal humerus. In: Browner BD, Levine AM, Trafton PG (eds) Skeletal trauma, vol 2. Saunders, Philadelphia, p 1141
- 2.King GJW (2007) The complex dislocations of the elbow. In: Celli A, Celli L, Morrey BF (eds) Treatment of elbow lesions. Springer, Milan, p 103
- 3.Kuhn MA, Ross G (2008) Acute elbow dislocations. Orthop Clin North Am 39:155–161 [DOI] [PubMed]
- 4.DeLee JC, Green DP, Wilkins KE (1984) Fractures and dislocations of the elbow. In: Rockwood CA, Green DP (eds) Fractures in adults, 2nd edn. Lippincott, Philadelphia, p 559
- 5.Linscheid RL, Wheeler DK (1965) Elbow dislocations. JAMA 194:113–118 [DOI] [PubMed]
- 6.Endean ED, Veldenz HC, Schwarcz TH, Hyde GL (1992) Recognition of arterial injury in elbow dislocation. J Vasc Surg 16:402–406 [DOI] [PubMed]
- 7.Jupiter JB, Ring D (2002) Treatment of unreduced elbow dislocations with hinged external fixation. J Bone Joint Surg Am 84-A:1630–1635 [DOI] [PubMed]
- 8.Regan W, Morrey BF (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71:1348–1354 [PubMed]
- 9.Mader K, Koslowsky TC, Gausepohl T, Pennig D (2007) Mechanical distraction for the treatment of posttraumatic stiffness of the elbow in children and adolescents. Surgical technique. J Bone Joint Surg Am 89(Suppl 2):26–35 [DOI] [PubMed]
- 10.Mader K, Pennig D, Gausepohl T, Koslowsky TC, Wulke AP (2004) Post-traumatic stiffness of the elbow: arthodiatasis using unilateral hinged external fixation. Scientific exhibit at the 71st AAOS meeting, San Francisco, California, March 10–14
- 11.Pennig D, Gausepohl T, Mader K (2000) Transarticular fixation with the capacity for motion in fracture dislocations of the elbow. Injury 31(Suppl 1):35–44 [DOI] [PubMed]
- 12.O`Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD (2003) Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 52:113–136 [PubMed]
- 13.Terada N, Yamada H, Seki T, Urabe T, Takayama S (2000) The importance of reducing small fractures o the coronoid process in treatment of unstable elbow dislocation. J Shoulder Elbow Surg 9:344–346 [DOI] [PubMed]
- 14.Morrey BF, Adams RA (1992) Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Joint Surg Am 74:479–490 [PubMed]
- 15.Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and hand). The Upper Extremity Collaborative Group. Am J Ind Med 29:602–608 [DOI] [PubMed]
- 16.Lyons RP, Armstrong A (2008) Chronically unreduced elbow dislocations. Hand Clin 24:91–103 [DOI] [PubMed]
- 17.Ruch DS, Triepel CR (2001) Hinged elbow fixation for recurrent instability following fracture dislocation. Injury 32(Suppl 4):70–78 [DOI] [PubMed]
- 18.Degreef I, De Smet L (2007) Chronic elbow dislocation: a rare complication of tennis elbow surgery. Successful treatment by open reduction and external fixator. Chir Main 26:150–153 [DOI] [PubMed]
- 19.Lo CY, Chang YP (2004) Neglected elbow dislocation in a young man: treatment by open reduction and elbow fixator. J Shoulder Elbow Surg 13:101 [DOI] [PubMed]
- 20.Ohno Y, Shimizu K, Ohnishi K (2005) Surgically treated chronic unreduced medial dislocation of the elbow in a 70-year-old man: a case report. J Shoulder Elbow Surg 14:549–553 [DOI] [PubMed]
- 21.Ring D, Hannouche D, Jupiter JB (2004) Surgical treatment of persistent dislocation or subluxation of the ulnohumeral joint after fracture-dislocation of the elbow. J Hand Surg 29A:470–480 [DOI] [PubMed]
- 22.Sunderamoorthy D, Smith A, Woods DA (2005) Recurrent elbow dislocation—an uncommon presentation. Emerg Med J 22:667–669 [DOI] [PMC free article] [PubMed]
- 23.Balchandani RH (1969) Unreduced dislocations of the elbow. Proceedings of the Indian Orthopaedic Association. J Bone Joint Surg Br 51:781
- 24.Ashby ME (1974) Old dislocations of the elbow. J Natl Med Assoc 66:465–467, 471 [PMC free article] [PubMed]
- 25.Krishnamoorthy S, Bose K, Wong KP (1976) Treatment of old unreduced dislocation of the elbow. Injury 8:39–42 [DOI] [PubMed]
- 26.Billett DM (1979) Unreduced posterior dislocation of the elbow. J Trauma 19:186–188 [DOI] [PubMed]
- 27.Dryer RF, Buckwalter JA, Sprague BL (1980) Treatment of chronic elbow instability. Clin Orthop 148:254 [PubMed]
- 28.Naidoo KS (1982) Unreduced posterior dislocations of the elbow. J Bone Joint Surg Br 64:603–606 [DOI] [PubMed]
- 29.Fowles JV, Kassab MT, Douik M (1984) Untreated posterior dislocation of the elbow in children. J Bone Joint Surg Am 66:921–926 [DOI] [PubMed]
- 30.Martini M, Benselama R, Daoud A (1984) Neglected luxations of the elbow. 25 surgical reductions. Rev Chir Orthop Reparatrice Appar Mot 70:305–312 (French) [PubMed]
- 31.Arafiles RP (1987) Neglected posterior dislocation of the elbow. A reconstruction operation. J Bone Joint Surg Br 69:199–202 [DOI] [PubMed]
- 32.di Schino M, Breda Y, Grimaldi FM, Lorthioir JM, Merrien Y (1990) Surgical treatment of neglected elbow dislocations. Report of 81 cases. Rev Chir Orthop Reparatrice Appar Mot 76:303–310 (French) [PubMed]
- 33.Bruce C, Laing P, Dorgan J, Klenerman L (1993) Unreduced dislocation of the elbow: case report and review of the literature. J Trauma 35:962–965 [DOI] [PubMed]
- 34.Moritomo H, Tada K, Yoshida T, Kawatsu N (1998) Reconstruction of the coronoid for chronic dislocation of the elbow. J Bone Joint Surg Br 80:490–492 [DOI] [PubMed]
- 35.Devnani AS (2004) Outcome of longstanding dislocated elbows treated by open reducation and excision of collateral ligaments. Singapore Med J 45:14–19 [PubMed]
- 36.Mahaisavariya B, Laupattarakasem W (2005) Neglected dislocation of the elbow. Clin Orthop Rel Res 431:21 [DOI] [PubMed]
- 37.Mighell MA, Dunham RC, Rommel EA, Frankle MA (2005) Primary semi-constrained arthroplasty for chronic fracture-dislocations of the elbow. J Bone Joint Surg Br 87:191–195 [DOI] [PubMed]
- 38.Majima M, Horii E, Nakamura R (2007) Treatment of chronic dislocated elbows: a report of three cases. J Shoulder Elbow Surg 16:e1–e4 [DOI] [PubMed]