Abstract
Purpose
To compare the streams of expenses and revenues associated with investment in a cohort of basic science investigators at the University of Rochester School of Medicine & Dentistry over seven years.
Method
The authors evaluated a medical school's financial investment in 25 basic science faculty who were hired between 1999 and 2004 to expand basic science research. The authors compared direct and indirect costs with the extramural grant support generated by these investigators through 2006. To facilitate a comparison of investments made and grants generated, the authors calculated present value (in 2006 dollars) of revenues and expenses using the school's approximate cost of capital.
Results
Of the 25 faculty members hired, 24 (96%) remained at the school through 2006. From 1999 to 2006, the school invested a total of $69.0 million ($33.1 million in start-up costs and $35.9 million in indirect costs) to support the faculty members. Through 2006, these faculty members generated $99.7 million in extramural grant revenue ($70.7 million in direct grant revenue and $29.1 million in indirect grant revenue). While the faculty generated $1.45 in total grant revenue per dollar invested, start-up expenses and incomplete recovery of indirect costs required the school to add 40 cents to every grant dollar generated to achieve financial equilibrium.
Conclusions
Investments in basic science research, even when successful, may require significant financial subsidies from academic health centers.
The financial resources of academic health centers are finite and are likely to become more challenged by constraints on reimbursement for clinical services1 and on the National Institutes of Health (NIH) budget.2 Among the key uses of funding streams available to medical schools is investment in new faculty that serve the research mission.3
Investments in research faculty can be substantial, frequently in the range of $500,000 to $1,000,000 for the start-up package of a basic scientist4. These investments draw upon scarce resources from medical school endowments, faculty practice plans,5 hospitals,6 and other sources.3 Despite the size of these investments, however, published quantitative efforts to track their outcome are limited7 and often rely on modeled outcomes and estimates of investments, opposed to actual outcomes and investments.3, 8 Moreover, these reports have not evaluated the outcomes of focused strategic planning efforts by medical centers to expand their basic science presence. We, therefore, sought to evaluate the grant revenue (direct and indirect) generated by a newly recruited cohort of basic science faculty in relationship to the financial investment made by a medical school as part of a medical center's strategic plan.
Method
Study cohort
Beginning in 1999, as part of a strategic plan for the University of Rochester Medical Center, the University of Rochester School of Medicine & Dentistry invested substantially to build its basic science faculty in three new centers: the Center for Aging and Developmental Biology, the Center for Biomedical Genetics, and the Center for Vaccine Biology. We evaluated the financial impact of the financial investment made in basic science faculty hired into these three centers between 1999 and 2004. For this analysis, we restricted our analysis to faculty members who received start-up packages (n=25) and excluded those who did not (n=4).
Financial analysis
For each new basic science faculty member, we calculated the financial investment made by the school in the investigator and the extramural grant revenues generated by him or her from the first year of hire through the end of fiscal year (July to June) 2006. The school's investment (start-up packages) included salary and benefits provided to the faculty member (including salary above the NIH cap) that was not supported by external funding, support for additional laboratory personnel, capital equipment expenses (which the school generally expensed in the year the cost was incurred), and other expenses (e.g., lab supplies). In addition, we estimated indirect costs expended by the school to support the centers that housed these newly hired faculty from 1999 to 2006. Indirect costs consisted of facility and administrative expenses. Facility costs included utilities and housekeeping (accounting for approximately 50% of the total) and depreciation on buildings and equipment (20% of the costs). Administrative expenses included those associated with our offices of research project administration, research accounting and cost standards, animal resources, the vivarium, human research protection, libraries, and other related expenses. These expenses were generally incremental and, when incremental data were not available (e.g., library and security), the expenses represented the medical school's share of university-wide indirect costs associated with these faculty members (30%). Unlike the start-up packages, the indirect costs were assigned to the center and not to the individual investigator. We excluded these indirect costs when we calculated the return on investment per individual investigator.
To facilitate comparisons of investment made and revenue generated at different time points, we calculated the present value of all investments and revenue as of the end of fiscal year 2006. To do this, we used the approximate cost of capital of the school (8%) to calculate the present value of either expenses (investments) or revenue generated. The cost of capital reflects the approximate borrowing cost of the school (e.g., the interest rate the school must pay its bond holders). We assumed that all investments and grants generated occurred at the end of the year.
The general formula for calculating present value is the following:
where C is the value of the initial investment, r is the cost of capital, and t is the time (in years) since the investment was made. For example, the present value (in 2006) of $1000 invested in 1999 would be $1000 × (1+0.08)^7 or $1714. The present value of investments made early in the faculty member's time at the school are thus weighed more heavily than more recently generated grant revenue.
We performed a sensitivity analysis, which evaluates the variance of a model's output (in this case the present value calculation) with a key input, to determine how the results changed with different assumptions on the school's cost of capital (range: 3% to 13%).
Statistical analysis
We summarized data using descriptive statistics and compared distributions of financial outcomes among various subgroups using a non-parametric test (the exact Wilcoxon rank sum test) due to distributions that were not normal. We used inferential statistics to allow a generalization of our results to the broader population of basic science researchers. We conducted all statistical tests at the two-sided significance level of 5%, and did not make any correction for multiple testing.
Results
Baseline characteristics
From 1999 to 2004, the school hired 25 faculty members into the three centers examined. Of these, 24 (96%) remained at the University of Rochester through fiscal year 2006 (Table 1). The average age of the cohort at time of hire was 40.5 years, and seven (28%) of the faculty members hired were women. Sixteen (64%), including five of the seven women, had a faculty rank of assistant professor at the time of hiring. We had financial data for all 25 faculty members hired.
Table 1.
Baseline Characteristics of the Faculty Members Hired Between 1999 and 2004 into Three New Basic Science Centers at the University of Rochester Medical Center
| Characteristic | Number (% out of 25) |
|---|---|
| Faculty hired | 25 |
| Faculty hired from outside the university | 23 (92) |
| Faculty remaining at the university through 2006 | 24 (96) |
| Women faculty | 7 (28) |
| Faculty with terminal degree of | |
| PhD | 22 (88) |
| MD, PhD | 3 (12) |
| Faculty hired in fiscal year | |
| 1999 | 5 (20) |
| 2000 | 7 (28) |
| 2001 | 8 (32) |
| 2002 | 1 (4) |
| 2003 | 3 (12) |
| 2004 | 1 (4) |
| Faculty rank upon hire | |
| Assistant Professor | 16 (64) |
| Professor | 9 (36) |
| Faculty rank as of 2006* | |
| Assistant Professor | 10 (40) |
| Associate Professor | 5 (20) |
| Professor | 10 (40) |
Includes rank at the time of the departure of the one faculty member who left the University
Financial results
The school invested (principally from its endowment, philanthropy, royalty streams, transfers from the clinical enterprise, and other unrestricted funds) a total of $25.9 million in start-up expenses from 1999 through 2006 in the 25 faculty members hired and an additional $27.8 million in indirect expenses to support the three newly created centers that housed the new faculty (Table 2). The present value of that total investment in 2006 was $69.0 million—$33.1 million in start-up costs and $35.9 million in indirect costs.
Table 2.
Investments in and Grant Revenues Generated by a Recently Hired Basic Science Faculty Cohort at the University of Rochester Medical Center (in U.S. dollars), 1999-2006
| Expense or revenue | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | Total |
|---|---|---|---|---|---|---|---|---|---|
| School of Medicine & Dentistry Investments | |||||||||
| Start-up package | |||||||||
| Salary and benefits: Faculty | 538,679 | 394,723 | 417,252 | 1,951,901 | 1,911,234 | 1,970,540 | 1,753,804 | 1,689,814 | 10,627,947 |
| Salary and benefits: Other personnel | 46,914 | 6,387 | 255,502 | 698,318 | 759,016 | 572,172 | 557,889 | 407,419 | 3,303,617 |
| Other expenses | 90,806 | 728,165 | 1,015,703 | 1,337,801 | 949,070 | 1,129,504 | 820,549 | 972,636 | 7,044,234 |
| (Total operating expenses*) | (676,399) | (1,129,275) | (1,688,457) | (3,988,021) | (3,619,320) | (3,672,215) | (3,132,241) | (3,069,870) | (20,975,798) |
| Capital equipment | 166,907 | 969,605 | 1,343,307 | 380,737 | 760,569 | 1,110,658 | 79,426 | 100,347 | 4,911,556 |
| [Total start-up package]† | [843,306] | [2,098,880] | [3,031,764] | [4,368,758] | [4,379,889] | [4,782,873] | [3,211,667] | [3,170,217] | [25,887,354] |
| Indirect costs | 2,650,823 | 2,873,076 | 3,285,834 | 3,433,499 | 3,827,363 | 3,903,402 | 3,840,854 | 3,955,655 | 27,770,506 |
| Total | 3,494,129 | 4,971,956 | 6,317,598 | 7,802,257 | 8,207,251 | 8,686,275 | 7,052,521 | 7,125,872 | 53,657,860 |
| Faculty-generated grant revenues | |||||||||
| Direct grant revenue | 606,789 | 2,076,100 | 4354,544 | 5,933,283 | 8,448,424 | 11,544,785 | 14,968,793 | 11,583,655 | 59,516,374 |
| Indirect grant revenue | 336,436 | 458,255 | 1,098,594 | 2,809,335 | 4,005,517 | 5,046,941 | 5,856,478 | 5,070,729 | 24,682,287 |
| Total | 943,225 | 2,534,355 | 5,453,138 | 8,742,619 | 12,453,941 | 16,591,726 | 20,825,272 | 16,654,385 | 84,198,660 |
The items in this line are a sum of the salaries and benefits of the faculty and other personnel and other expenses.
The items in this line are a sum of the total start-up package, including salaries, benefits, other expenses, and capital equipment costs before indirect costs.
Over the same time period, these 25 faculty members generated $84.2 million in extramural funding, the present value of which in 2006 was $99.7 million—$70.7 million in direct support and $29.1 million in indirect support (Figure 1). For each dollar invested, the faculty cohort generated $1.45 ($99.7 grant support generated/$69.0 million invested) in extramural grants. Most (71% or $70.7 million/$99.7 million) of the grant funding generated was to support the direct costs of the research activities conducted by the investigators. Of the $35.9 million in indirect costs invested by the school from 1999 to 2006, the school was able to recover only $29.1 million (81%) through grants generated by the cohort through 2006. Therefore, the school invested a total of $39.9 million ($33.1 million in start-up packages plus $6.8 million in unrecovered indirect costs) in order to generate $99.7 million in grants (most of which supported the research of the hires). Put differently, the school had to add about 40 cents on every externally generated research dollar to cover all the costs of research. Figure 2 graphically displays the cumulative present value of the total investment by the school and the grant funding generated by the investigators.
Figure 1.
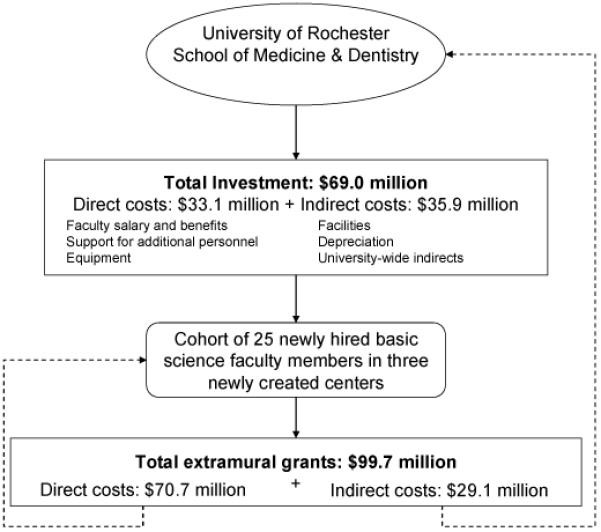
Total Investment Made by University of Rochester School of Medicine & Dentistry and Total Extramural Grant Revenue Generated by a Recently Hired Cohort of Basic Science Faculty, 1999 - 2006. The values in the figure represent the present value in 2006 dollars of the investments made and extramural grant support generated from 1999 - 2006. The present value is calculated as C x (1 + r)^t where C is the value of the investment made or grant generated, r is the cost of capital, and t is the time (in years) since the investment was made or the grant was generated. Of the $35.9 million in indirect costs invested by the school from 1999 to 2006, the school was able to recover only $29.1 million (81%) through grants generated by the cohort through 2006. Therefore, the school invested a total of $39.9 million ($33.1 million in start-up packages plus $6.8 million in unrecovered indirect costs) in order to generate $99.7 million in grants (most of which supported the research of the hires).
Figure 2.
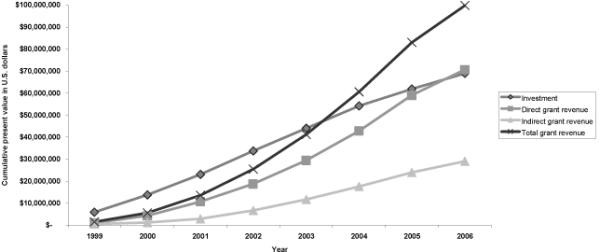
Cumulative Present Value of Investment in and Grant Revenue Generated by a Recently Hired Basic Science Faculty Cohort at the University of Rochester Medical Center, 1999 - 2006.
As mentioned above, the financial analysis by faculty member excluded the indirect costs ($35.9 million) borne by the school to support the new centers because these costs could not be assigned to an individual hire. With that caveat, faculty hired as professors tended to generate more grant dollars ($3.71) per dollar invested than did faculty hired as assistant professors ($2.18) (Table 3) although this difference did not reach statistical significance (p=0.12). Women generated similar grant revenues per dollar invested as men overall ($2.48 versus $2.83, respectively; p=0.75) and after controlling for rank at time of hire ($1.95 for female assistant professors versus $2.28 for male assistant professors; p=0.83).
Table 3.
Amount of Grant Support Generated per Dollar Invested in a Recently Hired Cohort of Basic Science Faculty at University of Rochester School of Medicine & Dentistry, 1999 - 2006
| Total grant support generated* | Direct grant support generated* | Indirect grant support generated* | |||||
|---|---|---|---|---|---|---|---|
| Population | Number | Average | Range | Average | Range | Average | Range |
| All investigators | 25 | 2.73 | 0 -- 7.07 | 1.90 | 0 -- 4.90 | 0.83 | 0 -- 2.17 |
| Women | 7 | 2.48 | 0 -- 5.33 | 1.72 | 0 -- 3.51 | 0.75 | 0 --1.82 |
| Men | 18 | 2.83 | 0.46 -- 7.07 | 1.97 | 0.36 -- 4.90 | 0.85 | 0.10 -- 2.17 |
| Assistant professors† | 16 | 2.18 | 0 --7.07 | 1.51 | 0 -- 4.90 | 0.67 | 0 -- 2.17 |
| Professors† | 9 | 3.71 | 0.67 -- 6.62 | 2.61 | 0.42 -- 4.77 | 1.10 | 0.25 -- 1.85 |
The ratio of grant support generated per dollar invested reflects the present value in 2006 of the dollars invested in the past and the grant support generated in the past. The present value is calculated as Cx (1 + r)^t where C is the value of the investment made or grant generated, r is the cost of capital, and t is the time (in years) since the investment was made or the grant was generated. Values greater than 1.00 indicate that more grant support was generated than dollars invested. Values less than 1.00 indicate that less grant support was generated than dollars invested. [Alternatively, a value of 2.73 indicates that the present value of grant support generated was $2.73 for every $1.00 invested.]
Rank at time of hire
Increasing the school's cost of capital from 8% to 13% gives greater relative weight to cash outlays that occurred further in the past (e.g., initial investments in the faculty). Using this higher cost of capital, each dollar invested by the school generated $1.37 of total ($0.97 direct, and $0.40 indirect) grant support. When the cost of capital is decreased to 3%, each dollar invested generated $1.52 of total ($1.08 direct, and $0.45 indirect) grant support.
Conclusions
Successful expansion of basic science research comes at a financial cost to academic health centers. Despite the success of the studied cohort of 25 basic science investigators in obtaining research grants, the school was unable to recover fully its indirect cost support and did not recover any of its investment in start-up packages. In the end, the school had to contribute 40 cents from other financial sources for each extramural grant dollar generated.
These results, generated largely during a time of rapid growth in biomedical research funding,9 highlight the value that investments by medical schools can create in advancing basic science research. The findings also support the view that medical schools are unable to recover investments made in expanding basic research. A RAND study,3, 10 using different methodology, suggested that universities do not fully recover their indirect costs. The results from that study suggested the research institutions contribute $0.15 to $0.20 to every indirect dollar received to support their scientific research mission.
Part of the explanation for the low recovery of the investment made in this study was the need for significant start-up costs for brand new faculty in newly created centers. Many of the faculty were junior (16 of the 25 were hired as assistant professors) upon hire and most (23 of the 25) were new to the school. Consequently, as shown in Table 2 and Figure 2, the bulk growth in extramural grants did not occur until 2003-2004 when the majority of the new hires were in place for at least two years. At steady state with established investigators, the net investment required by the school decreases substantially. For example, starting in 2003 the annual indirect costs generated by the investigators' grants exceeded the estimated indirect costs borne by the school. However, this incremental gain is insufficient, at least through 2006, to recover the total indirect costs invested by the school. Over longer periods, the school may be able to recover this investment in indirect costs. In the foreseeable future, however, the school will likely recover little, if any, of its substantial ($33.1 million) investment in direct start-up expenses to help the investigators start their new research careers. The shortfalls must be funded from other sources, such as the school's endowment, philanthropy, royalties, or transfers from other revenue centers (e.g., teaching hospital). Consistent with our findings, previous investigators have also found that investments in basic science faculty do not generate sufficient positive cash flow to the medical school to recover the initial investment even over ten years.3
At the faculty member level, senior members who were full professors at the time of their hire generated more grant support per dollar invested than did junior faculty members. This difference reflects the larger magnitude of extramural grants that senior faculty obtain and underscores the importance of retaining successful faculty.3 Grant support per dollar invested was very similar among women and men. While the numbers are small, the data highlight the success that women are increasingly experiencing in academic medicine.11, 12
While helpful, the financial metrics used in this analysis are incomplete. Our cost data allocated indirect costs to each of the newly created centers that housed the new faculty hires. An alternative analysis could compare all costs (including indirect ones) to each faculty hire and compare that to the “revenue” generated by each. Unfortunately, allocating all costs (e.g., utilities and security) to an individual faculty member is not always practical or accurate. Another potential analysis would solely look at the incremental costs and revenue associated with each new hire. In analysis of incremental costs and revenue, one may exclude fixed costs, such as the library; however, even “fixed” costs are increasingly variable (e.g., electronic library journals are often priced per head). In addition, an analysis solely of incremental costs would never cover the fixed costs associated with a university.
These financial metrics also do not account for all sources of economic value generated by the faculty. The exclusive reliance on extramural grant support excludes the value generated by faculty for teaching,13 clinical activities, royalties, and gifts. In this cohort, the teaching activities were likely limited in scope as the investigators devoted the vast majority of their time to research and administrative efforts (the latter was also not included in the financial analysis). Clinical activities, which can result in cash flows to the medical school (e.g., through a dean's tax), were virtually nonexistent in this cohort, as only three of the 25 investigators are physicians, and their clinical activity was limited. The magnitude of revenue generated from royalties, while occasionally large,14 is extremely erratic, usually associated with a small number of highly successful inventions.3 In this cohort, no royalties have resulted to date, and only two patents have been issued. Finally, gifts to support research in this cohort have been limited; the largest gift thus far has been $30,000. Our metrics also do not account for the non-financial returns that faculty generate in terms of contributions to the school's mission and reputation, to the local economy (e.g., job creation), or to society (e.g., the advancement of knowledge).
The results of this study also may not be readily generalizable as they come from one private medical school and only evaluate investments made in basic (not clinical) research. The results, however, are generally consistent with previous research done at a public medical school.3 These results extend that analysis by including the actual investments made by a medical school in hiring new faculty and by focusing on a specific cohort of individuals hired as part of a strategic plan.
Despite the limitations, the results of this study are valuable in planning research programs and in highlighting the research investment medical schools make. The metrics used are meaningful as they reflect both financial and academic (grants are generally rewarded post a peer-review process) outcomes. In addition, the results are complete for a sizeable cohort of faculty members, the vast majority of whom have remained at the medical school. The analyses conducted are relatively straightforward and deans and other administrators can use them to track investments made in the past retrospectively and future ones prospectively. With larger cohorts and additional data, administrators can use these analyses to identify factors associated with the financial and academic success of investigators, which is especially important given the wide range of research grant productivity found in this cohort. Further, administrators can employ these factors, once identified, in successfully recruiting and developing current and future faculty members. For example, administrators can more effectively set budgets and target an appropriate mix (e.g., by seniority) of recruits for departments or divisions.
Finally, as this study indicates, academic health centers contribute significantly to the research that is conducted at their institutions. According to the National Science Foundation, the contribution of academic institutions to science and engineering has grown from $5.4 billion in 1999 to $9.1 billion in 2006.15 This extraordinary growth in financial support for research by academic institutions highlights the increasingly important role played by endowment, philanthropy, and other private sources of support for such work, alongside stalwart governmental sources such as the NIH. With the constraints on the NIH budget2 and the transition of industry support from basic to clinical research,9 the role of academic health centers in supporting basic science research is likely to continue to grow.
Acknowledgements
This publication was made possible by Grant Number KL2 RR024136 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Information on NCRR is available at (http://www.ncrr.nih.gov/). Information on Re-engineering the Clinical Research Enterprise can be obtained from (http://nihroadmap.nih.gov/clinicalresearch/).
Footnotes
Disclaimer The contents of this report are solely the responsibility of the authors and do not necessarily represent the official view of National Center for Research Resources or the National Institutes of Health.
References
- (1).Moses H, 3rd, Thier SO, Matheson DHM. Why have academic medical centers survived? JAMA. 2005;293:1495–500. doi: 10.1001/jama.293.12.1495. [DOI] [PubMed] [Google Scholar]
- (2).Zerhouni EA. Research funding. NIH in the post-doubling era: Realities and strategies. Science. 2006;314(5802):1088–90. doi: 10.1126/science.1136931. [DOI] [PubMed] [Google Scholar]
- (3).Joiner KA, Hiteman S, Wormsley S, Germain P. Timing of revenue streams from newly recruited faculty: Implications for faculty retention. Acad Med. 2007;82:1228–1238. doi: 10.1097/ACM.0b013e318159cfa4. [DOI] [PubMed] [Google Scholar]
- (4).Joiner KA. A strategy for allocating central funds to support new faculty recruitment. Acad Med. 2005;80(3):218–24. doi: 10.1097/00001888-200503000-00005. [DOI] [PubMed] [Google Scholar]
- (5).Jones RF, Sanderson SC. Clinical revenues used to support the academic mission of medical schools, 1992 -93. Acad Med. 1996;71(3):300–7. doi: 10.1097/00001888-199603000-00027. [DOI] [PubMed] [Google Scholar]
- (6).Bowman MA, Rubenstein AH, Levine AS. Clinical revenue investment in biomedical research. Lessons from two academic medical centers. JAMA. 2007;297(22):2521–4. doi: 10.1001/jama.297.22.2521. [DOI] [PubMed] [Google Scholar]
- (7).Holmes EW, Burks TF, Dzau V, et al. Measuring contributions to the research mission of medical schools. Acad Med. 2000;75(3):303–13. doi: 10.1097/00001888-200003000-00027. [DOI] [PubMed] [Google Scholar]
- (8).Joiner KA. Sponsored-research funding by newly recruited assistant professors: Can it be modeled as a sequential series of uncertain events? Acad Med. 2004;79(7):633–43. doi: 10.1097/00001888-200407000-00005. [DOI] [PubMed] [Google Scholar]
- (9).Moses H, 3rd, Dorsey ER, Matheson DHM, Thier SO. Financial anatomy of biomedical research. JAMA. 2005;294(11):1333–42. doi: 10.1001/jama.294.11.1333. [DOI] [PubMed] [Google Scholar]
- (10).Goldman CA, Williams T. Paying for university research facilities and administration. RAND; Santa Monica, CA: 2000. [Google Scholar]
- (11).Jagsi R, Guancial EA, Worobey CC, et al. The “gender gap” in authorship of Academic Medical Literature - A 35-year perspective. New Engl J Med. 2006;355(3):281–7. doi: 10.1056/NEJMsa053910. [DOI] [PubMed] [Google Scholar]
- (12).Nonnemaker L. Women physicians in academic medicine: New insights from cohort studies. New Engl J Med. 2000;342(6):399–405. doi: 10.1056/NEJM200002103420606. [DOI] [PubMed] [Google Scholar]
- (13).Mallon WT, Jones RF. How do medical schools use measurement systems to track faculty activity and productivity in teaching? Acad Med. 2002;77(2):115–23. doi: 10.1097/00001888-200202000-00005. [DOI] [PubMed] [Google Scholar]
- (14).Becker C. Cashing in on royalties. Sloan-Kettering reaps 142 million dollars in deal. Modern Healthcare. 2005;35(35):18–19. [PubMed] [Google Scholar]
- (15).National Science Foundation, Division of Science Resource Statistics . NSF 08-300. Arlington, VA: 2007. Academic Research and Development Expenditures: Fiscal Year 2006. Ronda Britt, project officer. Available at: ( http://www.nsf.gov/statistics/nsf08300/pdf/nsf08300.pdf). Accessed September 22, 2008. [Google Scholar]


