Abstract
Background
Rescuer fatigue during cardiopulmonary resuscitation (CPR) is a likely contributor to variable CPR quality during clinical resuscitation efforts, yet investigations into fatigue and CPR quality degradation have only been performed in simulated environments, with widely conflicting results.
Objective
We sought to characterize CPR quality decay during actual in-hospital cardiac arrest, with regard to both chest compression (CC) rate and depth during the delivery of CCs by individual rescuers over time.
Methods
Using CPR-recording technology to objectively quantify CCs and provide audiovisual feedback, we prospectively collected CPR performance data from arrest events in two hospitals. We identified continuous CPR “blocks” from individual rescuers, assessing CC rate and depth over time.
Results
135 blocks of continuous CPR were identified from 42 cardiac arrests at the two institutions. Median duration of continuous CPR blocks was 112 sec (IQR 101–122). CC rate did not change significantly over single rescuer performance, with an initial mean rate of 105 ± 11 / min, and a mean rate after 3 min of 106 ± 9 / min (p=NS). However, CC depth decayed significantly starting between 90 sec and 2 min, falling from a mean of 48.3 ± 9.6 mm to 46.0 ± 9.0 mm (p=0.0006) and to 43.7 ± 7.4 mm by 3 minutes (p=0.002).
Conclusions
During actual in-hospital CPR with audiovisual feedback, CC depth decay became evident after 90 sec of CPR, but CC rate did not change. These data provide clinical evidence for rescuer fatigue during actual resuscitations and support current guideline recommendations to rotate rescuers during CC delivery.
Keywords: cardiopulmonary resuscitation, cardiac arrest, quality of care
Introduction
The provision of high quality chest compressions (CC) is a crucial component of cardiopulmonary resuscitation (CPR) and the successful treatment of cardiac arrest. For example, recent work has demonstrated that return of spontaneous circulation (ROSC) from in-hospital cardiac arrest was associated with higher CC rates,1 a finding consistent with earlier out-of-hospital studies of CPR quality. 2–4 Other investigations have revealed improved outcomes associated with greater CC depth. 5,6 Recently, the American Heart Association released a statement endorsing “hands only” CPR for bystanders comprised solely of CC, which highlights the importance of this potentially life-saving skill. 7 However, CCs are physically demanding and it has been generally assumed that rescuer fatigue can lead to degradation in compression quality. 8,9
Over the past several decades, a number of simulation studies have attempted to characterize rescuer fatigue during CPR with widely varying results.10–13 One such investigation among hospital staff found that rescuers fatigue quickly and that CC depth degrades after only one minute of CPR delivery. 10 Another manikin study found CPR quality decay with three minutes of CPR. 11 In stark contrast, a recent paramedic study found that CPR could be performed for as long as 10 minutes without falling below CPR guideline recommendations. 12
Furthermore, in all these studies were conducted in simulated settings using CPR manikins. Therefore, these investigations may not accurately reflect CPR performance during actual cardiac arrests, during which factors such as rescuer stress, motivation and other parameters may directly impact CPR quality. In addition, chest compliance varies both within mannequins and in comparison to people. However, no data exist to date on changes in resuscitation quality over time during actual CPR delivery.
Methods
Using recently developed CPR-sensing technology incorporated into clinical monitor/defibrillators with real-time audiovisual feedback, we conducted a multicenter study of changes in CC quality among individual rescuers over time during actual in-hospital resuscitation efforts. This prospective collection of cardiac arrest data was approved by the Institutional Review Boards (IRBs) of the University of Pennsylvania and the University of Chicago. All data were appropriately collected in a manner compliant with Health Insurance Portability and Accountability Act (HIPAA) regulations.
Data collection
Details of the data collection method have been described previously.14–16 Data were obtained using a commercially available monitor/defibrillator with CPR sensing and recording capabilities (MRx Q-CPR, Philips Healthcare, Andover, MA). The device features a compression-sensing pad consisting of a force transducer and accelerometer that is placed on the patient’s sternum under the hands of the rescuer. This allows for the recording of CC rate and depth, among other parameters. Additionally, the device has an integrated microphone, which allows for audio recording of events. Finally, the MRx provides real-time audiovisual feedback in the form of voice and screen prompts, which alert rescuers when CPR parameters deviate from the recommended guidelines.
Study protocol
Hospital staff members at both institutions were trained in the use of the MRx Q-CPR system prior to its implementation. The MRx Q-CPR devices were put into service in May 2007 at the Hospital of the University of Pennsylvania (HUP) in the Medical Intensive Care Unit (MICU), the Cardiac Care Unit (CCU), and on two general medicine floors. The same device was implemented throughout the University of Chicago Medical Center (UCMC) in February 2006.
Consecutive in-hospital cardiac arrests that occurred between May 2007 and May 2008 were included in analysis, provided that an MRx Q-CPR device was used during the arrest. Cardiac arrests were excluded if the MRx Q-CPR sensor was not used, if no CCs were provided, or if the resuscitation episode lasted less than two minutes. Cardiac arrest episodes were analyzed for continuous “blocks” of CCs after initial tracheal intubation, such that 30:2 compression:ventilation was replaced by continuous CC delivery. A block was defined as a segment of continuous CCs with a minimum duration of 90 sec, and no more than one sec between any two compressions. This definition was established in order to ensure the data were from a single rescuer, after it was determined from audio recordings that the rescuers providing CCs were occasionally switching during pauses as short as one sec.
Data analysis
CPR parameters were analyzed using proprietary software designed specifically for the MRx Q-CPR system (Q-CPR Review 2.0.0, Laerdal Medical Corporation, Stavanger, Norway). Each single rescuer block was broken down into consecutive 30-sec segments, which were sequentially analyzed to obtain the mean CC rate and depth of each segment.
Clinical data, such as patient demographics, initial rhythms, and outcomes were abstracted from the clinical record, including patient charts and written resuscitation transcripts.
Statistical analysis
Initial compilation of CPR data and clinical information was performed using spreadsheet software(Excel, Microsoft Corp, Redmond, WA). Statistical evaluation of CC data was performed using a statistical software package (STATA 10, Statacorp, College Station, TX). Continuous variables were described by means with standard deviations (SD), or medians with interquartile ranges (IQR), for highly skewed data. Changes in compression rate and depth over time were determined by comparing mean values of subsequent 30-sec segments within each block to the first 30-sec segment of that block. An additional analysis was done comparing subsequent mean values of the first 30 sec of compression depth in each block within a resuscitation to assess for changes in compliance, that could confound the results. All statistical analyses were conducted using two-sided paired student’s t-tests, with p<0.05 considered statistically significant.
Results
A total of 135 uninterrupted blocks of CCs with duration > 90 sec were identified from the cohort of 42 arrest episodes. The combined baseline characteristics of patients are shown in Table 1. Resuscitation characteristics of cardiac arrest episodes and continuous blocks of CCs are summarized in Table 2, analyzed individually for each hospital to evaluate for differences in CPR performance between institutions. The median (IQR) arrest duration was very similar for both institutions (18.3 (8.4 – 23.7) min at HUP versus 17.9 (8.5 – 30.0) min at UCMC), however UCMC yielded more blocks of uninterrupted CCs compared to HUP (85 versus 50), suggesting less frequent pauses in CPR or less frequent rescuer switching occurred at UCMC, which may relate to local resuscitation culture and training. Regardless, the duration of uninterrupted CC blocks was similar at both institutions, a median (IQR) of 110.1 (101.9 – 125.6) sec at HUP compared to 112.8 (103.0 – 122.2) sec at UCMC.
Table 1.
Patient demographic data (n=42).
| Patient age (yrs), mean ± SD: | 59.5 ± 19.5 |
| Gender, n (%): | |
| Female | 19 (46) |
| Male | 22 (54) |
| Time of event, n (%): | |
| 7:00am – 6:59pm | 24 (57) |
| 7:00pm – 6:59am | 18 (43) |
| Event Location, n (%): | |
| ICU | 32 (76) |
| non-ICU | 10 (24) |
| Initial arrest rhythm, n (%): | |
| VF/VT | 7 (17) |
| PEA | 30 (73) |
| Asystole | 4 (10) |
| ROSC, n (%): | 20 (49) |
| Survival to discharge, n (%): | 5 (12) |
The demographic data from one patient were unobtainable. ICU: intensive care unit; VF/VT: ventricular fibrillation/ventricular tachycardia; PEA: pulseless electrical activity; ROSC: return of spontaneous circulation.
Table 2.
Cardiac arrest episode and continuous CC block data.
| HUP | UCMC | |
|---|---|---|
| Cardiac arrest episodes included, n: | 23 | 19 |
| Episode duration (min), median (IQR): | 18.3 (8.4 – 23.7) | 17.9 (8.5 – 30.0) |
| Continuous CC blocks >90 sec, n: | 50 | 85 |
| Block duration (sec), median (IQR): | 110.1 (101.9–125.6) | 112.8 (103.0–122.2) |
| Pause time before block (sec), median (IQR): |
7.5 (2.9–16.6) | 8.7 (6.6 – 13.9) |
| Blocks with audible rescuer switches during pause prior to blocks, n (%): |
13 (26) | 25 (29) |
| Pause time of audible rescuer switches, median (IQR): |
3.4 (2.6–6.7) | 8.5 (6.3–12.7) |
CC: chest compression; HUP: Hospital of the University of Pennsylvania; UCMC: University of Chicago Medical Center.
Additionally, we analyzed the pause time before each individual rescuer CC block, during which rescuers may have switched, and/or pulse and rhythms may have been checked. At HUP the median (IQR) pre-block pause time was 7.5 (2.9 – 16.6) sec and at UCMC it was 8.7 (6.6 – 13.9) sec. Rescuer switches were definitively identified in 26% and 29% of the pauses, respectively, based on listening to audio recordings of each CC block. The median (IQR) pre-block pause times for the definitive rescuer switches was 3.4 (2.6 – 6.7) sec for HUP and 8.5 (6.3 – 12.7) sec for UCMC.
Each block of uninterrupted CCs was divided into 30 sec segments over which the mean CC rate and depth was calculated. Table 3 shows the average rate and depth for all compression periods during the first three minutes of CPR. The average change in compression rate and depth from baseline (the first 30 sec segment) by block is presented graphically in Figure 1 and Figure 2, respectively. With regard to rate, there was no significant change over six 30 sec segments (three min total elapsed time). Meanwhile, there was no significant change in compression depth over the first 90 sec but a linear decrease of 6.6 ± 4.9 mm (p=0.002) over the subsequent 90 sec, representing a 12.1% decay in compression depth during that time. When the first 30 sec mean compression depths of each block in any given resuscitation were analyzed, there was no significant change over time, suggesting that changes in chest wall compliance did not contribute to our findings (data not shown).
Table 3.
CC rate and depth over consecutive 30 sec segments within a block of continuous CPR.
| Segment (sec) | blocks, n | rate (/min) | depth (mm) |
|---|---|---|---|
| 0–30 | 135 | 105.2 ± 11.5 | 48.3 ± 9.6 |
| 31–60 | 135 | 105.8 ± 10.0 | 48.5 ± 9.1 |
| 61–90 | 135 | 105.8 ± 8.6 | 47.9 ± 8.9 |
| 91–120 | 116 | 106.3 ± 9.3 | 46.0 ± 9.0 |
| 121–150 | 32 | 102.9 ± 7.6 | 44.0 ± 8.4 |
| 151–180 | 10 | 106.6 ± 8.8 | 43.7 ± 7.4 |
CC: chest compression; CPR: cardiopulmonary resuscitation. Note that each continuous CC block was of different duration, thus the later segments are represented in a decreasing number of blocks. No p values are shown, as statistical evaluation was only performed on paired CC data (see Figure 1 and Figure 2).
Figure 1.
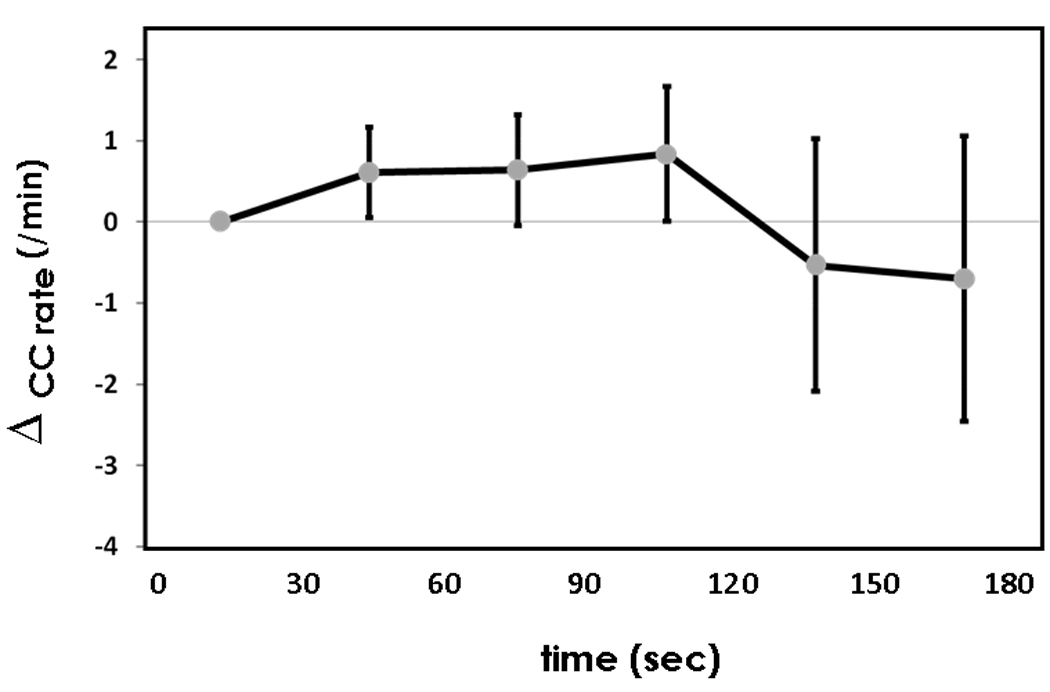
Change in mean CC rate over consecutive 30 sec segments compared to baseline CC rate during first 30 sec segment. There is no statistically significant change over time during measured continuous CPR.
Figure 2.
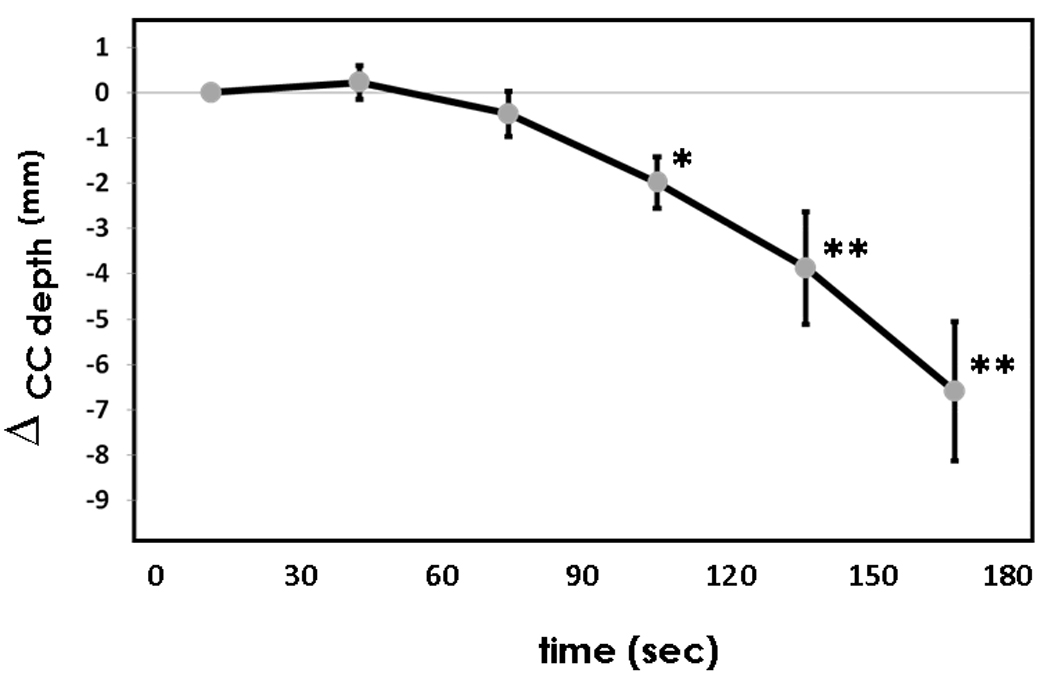
Change in mean CC depth over consecutive 30 sec segments compared to baseline CC depth during first 30 sec segment. * p<0.001; ** p<0.01.
Discussion
We demonstrated a decrease in CC depth over time for a single rescuer starting at 90 sec of CPR, without any change in CC rate, during actual in-hospital resuscitations during which real-time audiovisual feedback was provided. To our knowledge, this study represents the first to evaluate decay in CC quality (commonly associated with rescuer fatigue) during actual in-hospital cardiac arrest resuscitation efforts.
Our results stand in contrast to some of the previous studies on rescuer fatigue during simulated CPR. Hightower et al. reported a drastic drop in compression adequacy (a combined metric including depth and rate analysis) from 93% of compressions to 67% after only one min of CPR.13 After five min they found that only 18% of the delivered CCs were adequate. Conversely, in another manikin study Bjørshol et al. found no significant degradation in CC performance over 10 min of continuous efforts.12
Although we measured average CC depth rather than percentage of adequate compressions, our results suggest that the decrease in depth over time—and therefore the decrease in compression adequacy—is more gradual during actual cardiac arrest than demonstrated by Hightower et al., but does indeed occur as a real phenomenon of continuous CPR delivery. These differences could be attributed to differences in chest wall compliance between humans and mannequins or to the varied settings and participants in the simulation studies, where many of the psychological and physiological factors such as a sense of urgency, preparedness, and anxiety, as well as room crowding, noise levels, and team dynamics, are likely quite different from the actual cardiac arrest environment.
It should also be noted that although our findings were statistically significant, the magnitude of the decay in CC depth was moderate and the clinical significance of remains uncertain. However, based on prior work evaluating the accuracy of the CPR sensing technology utilized, it is likely that the measured compressions overestimate actual compression depth by as much as 28–40%, which would decrease subsequent compression depths below resuscitation guideline recommendations of 38–51 mm.17,18
The importance of this topic is additionally relevant to CPR in the out-of-hospital cardiac arrest setting, where bystanders and Emergency Medical Services personnel often perform CPR for more prolonged periods of time before arriving at the hospital. The investigation of such out-of-hospital CPR would allow for evaluation of CPR decay over longer durations of continuous CC delivery.
Our study is not without limitations. First, we were unable to gather the rescuers’ demographic data to assess whether any CC provider factors were linked to CPR quality. One might expect such characteristics as physical size and age, as well as experience, to play a role in an individual rescuer’s ability to deliver compressions; recent simulation work has highlighted such factors in CPR delivery.19 In previous studies of CPR decay and fatigue, Ochoa et al. reported that an observed decrease in compression quality did not depend on gender, age, height, weight or the rescuer’s profession. However, Ashton et al. found in their study that females achieved significantly fewer adequate compressions over a three minute period of CPR, and that this discrepancy was correlated with height and weight differences. Further work in which rescuers are identified during actual resuscitation efforts and linked to CPR performance will be required to further elucidate this issue. Other factors may play a role as well, such as presence or absence of a backboard, or the mattress compliance. These factors were unmeasured in our current study.
A second limitation was that these results were obtained using real-time audiovisual feedback during resuscitation and may not be generalizable to systems where feedback is not used. However, several prior clinical investigations have demonstrated that use of real-time feedback improves CPR quality.20–22 Therefore, our results likely underestimate the actual CPR decay from rescuer fatigue, as some fraction of rescuers may have maintained CPR quality despite initial fatiguing in response to feedback messages. In a similar limitation to the broad applicability of our work, the majority of resuscitations evaluated in this cohort took place in critical care settings, not on the general wards or Emergency Department. It is unclear whether parameters of CC decay and fatiguing would be different, however, based on location of event or local staffing. One might expect less CC decay in critical care settings, where staff are more experienced with CPR delivery, although future work will be required to test this hypothesis.
Conclusion
In this multicenter clinical investigation, we demonstrated a moderate but statistically significant decay in chest compression depth over three minutes of in-hospital CPR from a cohort of individual rescuers, starting after 90 sec, under conditions of automated CPR audiovisual feedback. Further work will be required to determine the clinical significance of this decay. However, these data provide clinical evidence for rescuer fatigue during actual resuscitations and support the need to rotate rescuers frequently during CPR as currently recommended by consensus resuscitation guidelines.
Acknowledgements
The authors wish to thank the dedicated housestaff and nurses at the University of Pennsylvania and University of Chicago for their dedication to the care of cardiac arrest patients and their willingness to participate in our research efforts.
This study was funded by Philips Healthcare, which had no role in the design and conduct of the study, analysis of the findings, or the drafting of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
This study was funded by Philips Healthcare, which had no role in the design and conduct of the study or analysis of the findings. In addition to research funding, Drs. Edelson, Abella, and Becker have received honoraria and consulting fees from Philips Healthcare. Dr. Abella has additionally received consulting fees from Cardiac Science Corporation; Dr. Becker has received research funding from Laerdal Medical Corporation. Drs. Edelson and Abella have received research funding from the American Heart Association. for CPR investigations.
References
- 1.Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 2.Wik L, Steen PA, Bircher NG. Quality of bystander cardiopulmonary resuscitation influences outcome after prehospital cardiac arrest. Resuscitation. 1994;28:195–203. doi: 10.1016/0300-9572(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher EJ, Lombardi G, Gennis P. Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA. 1995;274:1922–1925. [PubMed] [Google Scholar]
- 4.Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. Belgian Cerebral Resuscitation Study Group. Quality and efficiency of bystander CPR. Resuscitation. 1993;26:47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- 5.Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71:137–145. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Sayre MR, Berg RA, Cave DM, et al. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- 8.Heidenreich JW, Berg RA, Higdon TA, et al. Rescuer fatigue: standard versus continuous chest-compression cardiopulmonary resuscitation. Acad Emerg Med. 2006;13:1020–1026. doi: 10.1197/j.aem.2006.06.049. [DOI] [PubMed] [Google Scholar]
- 9.Steen PA, Kramer-Johansen J. Improving cardiopulmonary resuscitation quality to ensure survival. Curr Opin Crit Care. 2008;14:299–304. doi: 10.1097/MCC.0b013e3282f827d3. [DOI] [PubMed] [Google Scholar]
- 10.Ochoa FJ, Ramalle-Gómara E, Lisa V, Saralegui I. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–152. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 11.Ashton A, McCluskey A, Gwinnutt CL, Keenan AM. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 2002;55:151–155. doi: 10.1016/s0300-9572(02)00168-5. [DOI] [PubMed] [Google Scholar]
- 12.Bjørshol CA, Søreide E, Torsteinbø TH, Lexow K, Nilsen OB, Sunde K. Quality of chest compressions during 10min of single-rescuer basic life support with different compression: ventilation ratios in a manikin model. Resuscitation. 2008;77:95–100. doi: 10.1016/j.resuscitation.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Hightower D, Thomas SH, Stone CK, Dunn K, March JA. Decay in quality of closed-chest compressions over time. Ann Emerg Med. 1995;26:300–303. doi: 10.1016/s0196-0644(95)70076-5. [DOI] [PubMed] [Google Scholar]
- 14.Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 15.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 16.Losert H, Sterz F, Köhler K, et al. Quality of cardiopulmonary resuscitation among highly trained staff in an emergency department setting. Arch Intern Med. 2006;166:2375–2380. doi: 10.1001/archinte.166.21.2375. [DOI] [PubMed] [Google Scholar]
- 17.Perkins GD, Smith CM, Augre C, et al. Effects of a backboard, bed height, and operator position on compression depth during simulated resuscitation. Intensive Care Med. 2006;32:1632–1635. doi: 10.1007/s00134-006-0273-8. [DOI] [PubMed] [Google Scholar]
- 18.Nishisaki A, Nysaether J, Sutton R, et al. Effect of mattress deflection on CPR quality assessment for older children and adolescents. Resuscitation. 2009 doi: 10.1016/j.resuscitation.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Verplancke T, De Paepe P, Calle PA, et al. Determinants of the quality of basic life support by hospital nurses. Resuscitation. 2008;77:75–80. doi: 10.1016/j.resuscitation.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 21.Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Boyle AJ, Wilson AM, Connelly K, et al. Improvement in timing and effectiveness of external cardiac compressions with a new non-invasive device: the CPR-Ezy. Resuscitation. 2002;54:63–67. doi: 10.1016/s0300-9572(02)00049-7. [DOI] [PubMed] [Google Scholar]


