Summary
OBJECTIVE
To assess differences of HIV risk between ethnicities in northwestern China.
METHOD
Cross-sectional serosurvey and structured questionnaire interview of 383 injection drug users of either Han or Uigur ethnicity in Urumqi, Xinjiang.
RESULTS
Both Uigur minority ethnicity and residence in a Uigur or mixed Uigur/Han community were independently associated with higher HIV risk.
CONCLUSION
HIV prevention programs should give special focus on minority ethnic drug users and their communities.
Keywords: injection drug users, HIV, risk environment, China
Introduction
Injection drug use is the most frequent mode of HIV transmission in China (Lu et al. 2006). Illicit drugs such as heroin and opium are mainly trafficked from China’s neighbouring regions ‘Golden Triangle’ and ‘Golden Crescent’, into its southwestern and northwestern parts and then further to inland provinces (Beyrer et al. 2000; Qian et al. 2006).
Provinces in southwestern and northwestern China, such as Yunnan, Xinjiang and Guangxi, have the heaviest epidemics of IDU and related HIV/AIDS (Qian et al. 2005, 2006; Xiao et al. 2007). These provinces also have high proportion of minority ethnic residents, for example, 30% in Yunnan, 60% in Xinjiang, and 38% in Guangxi. On national average, 8% of China’s total population are minorities belonging to 55 ethnic groups; the vast majority (92%) of the population are Han.
Compared to eastern coastal provinces, these remote regions are less developed economically and have fewer resource for public health programs, particularly in rural areas (Henderson et al. 1995; Liu et al. 2007). One important public health question is: how do drug injection and equipment sharing practices affect HIV risk among minority ethnic drug users in these regions? We conducted a cross-sectional survey in Xinjiang in 2005 to evaluate whether minority ethnic people have higher drug-related HIV risk than Han.
Methods
This study was conducted in Urumqi, the capital city of Xinjiang in northwestern China, where Uigur is a dominant minority ethnicity. Participants were recruited using community outreach and snowballing strategies. Those who were 18 years or older, had injected drugs at least once in the last 3 months, and were willing to provide written informed consent, were eligible for enrolment in this study. All eligible subjects were interviewed using a structured questionnaire that included questions regarding the study participant’s demographics, drug use and sexual history. A blood sample was collected to test HIV antibody using both enzyme immunoassay and Western blot. Informed consent was obtained from each participant. The Institutional Review Board of Chinese National Center for AIDS/STD Control and Prevention approved this study.
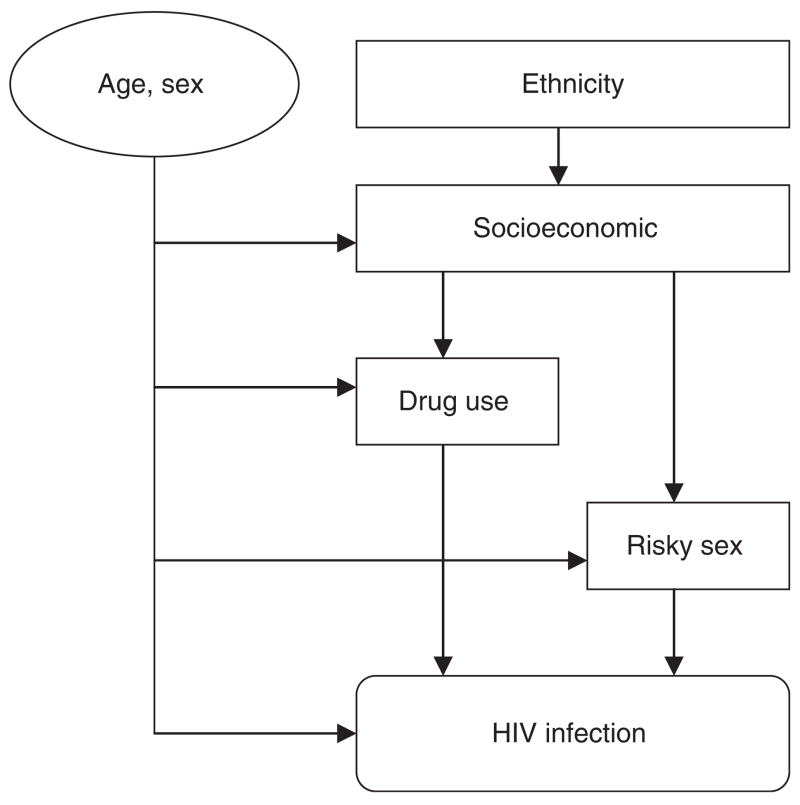
Data were analysed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA). Multivariate logistic regression analyses were used to take into account the hierarchical relationship between the proposed risk factors and the outcome (Victora et al. 1997). According to our conceptual model (Figure 1), ethnicity may constitute a predictor for HIV infection through a hierarchical chain from socioeconomic factors to drug using or risky sexual behaviours, while age and sex may determine all these intermediate variables and the outcome. As univariate analysis showed a significant relationship between ethnicity and HIV infection, the first multivariate model (Model 1) included ethnicity. Age and sex were forced into the first model as well all subsequent models. The second model (Model 2) added to Model 1 all socioeconomic variables such as marital status, income, education, owning a house/apartment and community of residence which were significant at a level of P = 0.05. Again, all variables in Model 2 were forced into Model 3 plus the drug use and risk sex variables which were statistically significant.
Figure 1.
Conceptual framework of risk factors for HIV infection among IDUs in Xinjiang, China.
Results
A total of 401 injection drug users (IDUs) were tested for HIV infection; 18 were excluded because they were neither Han nor Uigur. Thus 383 subjects were included in the analyses, comprising 103 (26.9%) Han and 280 (73.1%) Uigur individuals. The median age was 30 (range 18–48) years; 89% were male; 62.1% were unemployed; 23.2% were married. 21% of IDUs reported residing in a Han community and 79.1% in a Uigur or mixed Han/Uigur community. The median number of years of injecting drugs was 5.0 (range 0.1–15.4) years. A total of 68.4% reported having ever shared injection equipments with other drug users. Eighteen percent of IDUs reported involving in commercial sex in the last 6 months.
Thirty-seven percent (142/383) of IDUs were HIV seropositive, 12.6% among Han and 46.1% among Uigur participants. Three multivariate logistic regression models were fitted, and seven variables were identified as independent predictors for HIV seropositivity (Table 1): Uigur ethnicity (adjust odds ratio (AOR): 9.2; 95% confidence intervals (CI): 4.2–19.7), residing in an Uigur or mixed community (AOR: 4.2; 95% CI: 1.8–9.5), older age (≥30 years) (AOR: 2.4; 95% CI: 1.3–4.3), female sex (AOR: 3.7; 95% CI: 1.6–8.3), being married (AOR: 2.6; 95% CI: 1.4–4.8), ≥5 years of injecting drugs (AOR: 3.7; 95% CI: 2.1–6.4), and ≥2 lifetime partners sharing injection equipment (AOR: 2.3; 95% CI: 1.4–3.9).
Table 1.
Factors associated with HIV infection in 383 injection drug users in Xinjiang, China
| Factors | No. of participants | No. of HIV positives (%) | Unadjusted odds ratio (95% CI)* | P-value | Adjusted odds ratio (95% CI)* | P-value |
|---|---|---|---|---|---|---|
| Age*(years) | ||||||
| <30 | 184 | 61 (33.2) | 1.0 | 0.13 | 1.0† | <0.01 |
| ≥30 | 199 | 81 (40.7) | 1.4 (0.9–2.1) | 2.4 (1.3–4.3) | ||
| Sex | ||||||
| Male | 339 | 122 (36.0) | 1.0 | 0.22 | 1.0† | <0.01 |
| Female | 44 | 20 (45.5) | 1.5 (0.8–2.8) | 3.7 (1.6–8.3) | ||
| Ethnicity | ||||||
| Han | 103 | 13 (12.6) | 1.0 | <0.01 | 1.0† | <0.01 |
| Uigur | 280 | 129 (46.1) | 5.9 (3.2–11.1) | 9.2 (4.2–19.7) | ||
| Place of residence | ||||||
| Han community | 80 | 11 (13.8) | 1.0 | <0.01 | 1.0‡ | <0.01 |
| Uigur or mixed community | 303 | 131 (43.2) | 4.8 (2.4–9.4) | 4.2 (1.8–9.5) | ||
| Married | ||||||
| No | 299 | 93 (31.1) | 1.0 | <0.01 | 1.0‡ | <0.01 |
| Yes | 84 | 49 (58.3) | 3.1 (1.9–5.1) | 2.6 (1.4–4.8) | ||
| Duration of drug injection | ||||||
| <5 years | 189 | 44 (23.3) | 1.0 | <0.01 | 1.0 § | <0.01 |
| ≥5 years | 194 | 98 (50.5) | 3.4 (2.2–5.2) | 3.7 (2.1–6.4) | ||
| Number of lifetime partners sharing injection equipments | ||||||
| <2 | 190 | 44 (23.2) | 1.0 | <0.01 | 1.0 § | <0.01 |
| ≥2 | 193 | 98 (50.8) | 3.4 (2.2–5.3) | 2.3 (1.4–3.9) | ||
CI, confidence interval.
Model 1: age, sex, and ethnicity.
Model 2: model 1 plus place of residence and marital status.
Model 3: model 2 plus duration of drug injection and number of lifetime partners sharing injection equipments.
Discussion
Our study showed that the HIV prevalence among Uigur IDUs was nearly three times as high as among Han IDUs. This phenomenon has been also observed in HIV/AIDS surveillance and other epidemiologic studies. Uigur ethnic residents accounted for 45% of the total population in Xinjiang but they contributed 84% of cumulatively reported HIV/AIDS cases by 2005. A previous prospective 12-month cohort study in Urumqi city found HIV incidence among Uigur IDUs (11%) to be nearly twice that among Han IDUs (6%) (Zhang et al. 2007). In Yunnan province in southwestern China, the Jingpo minority accounted for 9% of all new HIV infections in 2004 but only 0.3% of the general population; the Dai minority accounted for 7% of all new HIV infections and 2.5% of the population (Lu et al. 2005). In Xichang City of Sichuan Province, Yi minority IDUs also showed higher HIV risk (Ruan et al. 2004). However, a study in another south-western Guangxi province heavily affected by an IDU-associated HIV epidemic found that Zhuang minority ethnicity was not associated with elevated HIV risk, but the sample size of the Han IDUs comparison group was small (Lai et al. 2001).
The booming drug smuggling activities in minority ethnic communities along southwestern and northwestern border provinces may partially explain the disproportionate distribution of reported HIV/AIDS cases among Uigur people in Xinjiang and Jingpo and Dai people in Yunnan. However, other reasons may account for the ethnic difference of HIV risk in our study as all participants were IDUs. Uigur IDUs were more likely to share equipment probably because of their social customs, lower awareness of injection safety and HIV risk, or inability to obtain clean needles. In our study, 71.4% of Uigur participants had ever shared equipment compared to 60.2% of Han participants (P < 0.05); and 55.7% of Uigur participants had ever shared equipments with two or more partners compared to 35.9% of Han participants (P < 0.001). Studies in Yunnan province also showed that Jingpo male drug users were twice as likely to initiate drug use (Wu et al. 1999) and that Jingpo ethnic men were six times as likely to share syringes as other ethnic groups (Wu et al. 1996). Although several drug use variables were adjusted for in assessing the association between ethnicity and HIV risk and ethnicity, residual confounding due to drug use practices was still possible.
Another important finding of this study was that residence in an Uigur or mixed community was an independent risk factor for HIV infection, while there was no significant interaction between ethnicity and residence. The place of residence reflects the role of the social and physical environment with regard to vulnerability and exposure to risk among drug users (Latkin et al. 1995; Rhodes et al. 2003). Qualitative ethnographic and social network research is needed to better understand the relationship. Our study suggests that drug abuse and HIV prevention intervention programs should be specially tailored to minority ethnic people and communities in these border regions of China.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (10501052), the Ministry of Health of China (WA2003-13) and the Ministry of Science and Technology of China (2004BA719A01). HZQ received support from the Vanderbilt- UAB AIDS International Training and Research Program grant (NIH 3D43 TW001035).
References
- Beyrer C, Razak MH, Lisam K, Chen J, Lui W, Yu XF. Overland heroin trafficking routes and HIV-1 spread in south and south-east Asia. AIDS. 2000;14:75–83. doi: 10.1097/00002030-200001070-00009. [DOI] [PubMed] [Google Scholar]
- Henderson G, Jin S, Akin J, et al. Distribution of medical insurance in China. Social Science & Medicine. 1995;41:1119–1130. doi: 10.1016/0277-9536(94)00420-x. [DOI] [PubMed] [Google Scholar]
- Lai S, Liu W, Chen J, et al. Changes in HIV-1 incidence in heroin users in Guangxi Province, China. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2001;26:365–370. doi: 10.1097/00126334-200104010-00014. [DOI] [PubMed] [Google Scholar]
- Latkin C, Mandell W, Oziemkowska M, et al. Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug and Alcohol Dependence. 1995;38:1–9. doi: 10.1016/0376-8716(94)01082-v. [DOI] [PubMed] [Google Scholar]
- Liu M, Zhang Q, Lu M, Kwon CS, Quan H. Rural and urban disparity in health services utilization in China. Medical Care. 2007;45:767–774. doi: 10.1097/MLR.0b013e3180618b9a. [DOI] [PubMed] [Google Scholar]
- Lu L, Jia MH, Lu JY, et al. Analysis of HIV/AIDS prevalence in Yunnan province. Zhongguo Xing Bing Ai Zi Bing Fan Zhi Za Zhi. 2005;11:172–174. [Google Scholar]
- Lu F, Wang N, Wu Z, et al. Estimating the number of people at risk for and living with HIV in China in 2005: methods and results. Sexually Transmitted Infections. 2006;82(Suppl 3):87–91. doi: 10.1136/sti.2006.020404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian HZ, Vermund SH, Wang N. Risk of HIV/AIDS in China: subpopulations of special importance. Sexually Transmitted Infections. 2005;81:442–447. doi: 10.1136/sti.2004.014258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian HZ, Schumacher JE, Chen HT, Ruan YH. Injection drug use and HIV/AIDS in China: review of current situation, prevention and policy implications. Harm Reduction Journal. 2006;3:4. doi: 10.1186/1477-7517-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T, Mikhailova L, Sarang A, et al. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment. Social Science & Medicine. 2003;57:39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- Ruan Y, Chen K, Hong K, et al. Community-based survey of HIV transmission modes among intravenous drug users in Sichuan, China. Sexually Transmitted Diseases. 2004;31:623–627. doi: 10.1097/01.olq.0000140018.24262.4a. [DOI] [PubMed] [Google Scholar]
- Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. International Journal of Epidemiology. 1997;26:224–227. doi: 10.1093/ije/26.1.224. [DOI] [PubMed] [Google Scholar]
- Wu Z, Detels R, Zhang J, et al. Risk factors for intravenous drug use and sharing equipment among young male drug users in Longchuan County, south-west China. AIDS. 1996;10:1017–1024. doi: 10.1097/00002030-199610090-00013. [DOI] [PubMed] [Google Scholar]
- Wu Z, Zhang J, Li Z. Risk factors for initiation of drug use among young males in Longchuan, Yunnan. Zhonghua Liu Xing Bing Xue Za Zhi. 1999;20:15–18. [PubMed] [Google Scholar]
- Xiao Y, Kristensen S, Sun J, Lu L, Vermund SH. Expansion of HIV/AIDS in China: lessons from Yunnan Province. Social Science & Medicine. 2007;64:665–575. doi: 10.1016/j.socscimed.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Shan H, Trizzino J, et al. HIV incidence, retention rate, and baseline predictors of HIV incidence and retention in a prospective cohort study of injection drug users in Xinjiang, China. International Journal of Infectious Diseases. 2007;11:318–323. doi: 10.1016/j.ijid.2006.09.001. [DOI] [PubMed] [Google Scholar]