Abstract
The aim of this study was to determine if volumes of frontotemporal regions associated with language were related to thought disorder in 42 children, aged 5–16 years, with cryptogenic epilepsy, all of whom had complex partial seizures (CPS). The children with CPS and 41 age- and gender-matched healthy children underwent brain MRI scans at 1.5 T. Tissue was segmented, and total brain, frontal lobe, and temporal lobe volumes were computed. Thought disorder measures, IQ, and seizure information were collected for each patient. The subjects with CPS had more thought disorder, smaller total gray matter and orbital frontal gray matter volumes, as well as larger temporal lobe white matter volumes than the control group. In the CPS group, thought disorder was significantly related to smaller orbital frontal and inferior frontal gray matter volumes, increased Heschl’s gyrus gray matter volumes, and smaller superior temporal gyrus white matter volumes. However, significantly larger orbital frontal gyrus, superior temporal gyrus, and temporal lobe gray matter volumes and decreased Heschl’s gyrus white matter volumes were associated with thought disorder in the control group. These findings suggest that thought disorder might represent a developmental disability involving frontotemporal regions associated with language in pediatric CPS.
Keywords: Thought disorder, Complex partial seizures, Development, Brain volumes, Childhood, Language
1. Introduction
Children with a broad range of neurobehavioral disorders including epilepsy [1–3], schizophrenia [4], attention-deficit hyperactivity disorder (ADHD) [5], and high-functioning autism [6], as well as young otherwise healthy children [4], have thought disorder. Compared with their peers, these children have difficulty using language to formulate and organize their thoughts. When speaking, they present their ideas with impaired reasoning (i.e., illogical thinking) and unpredictable change the topic of conversation (i.e., loose associations). They also use few linguistic (i.e., cohesive) devices to connect ideas (e.g., conjunctions) and to refer to people, objects, or events (e.g.., pronouns, the article, demonstratives) within and across sentences. In addition, while they speak, they infrequently monitor and self-repair communication breakdowns or errors in how they organize their thoughts and use syntax, word choice, and reference to express their ideas. These discourse deficits make it difficult for the listener to follow whom and what they are talking about.
Given the importance of social communication in our daily lives, these social communication deficits have functional correlates. Thus, studies in children with epilepsy have demonstrated an association between thought disorder and disruptive disorder diagnoses (i.e., ADHD, oppositional defiant disorder, conduct disorder), high Child Behavior Checklist externalizing factor scores, decreased academic achievement, school problems, and poor peer interaction [1–3]. In children with ADHD, thought disorder is related to cognitive and attentional deficits [5], and in children with high-functioning autism, it is related to impaired cognition [6].
From the developmental perspective, in children with cryptogenic epilepsy with complex partial seizures (CPS) and focal involvement in the temporal and frontal lobes, the severity of thought disorder is related to increased seizure frequency, early age at onset, history of prolonged seizures, and type of antiepileptic drug (AED), as well as younger age, male gender, and lower Verbal IQ scores [3]. These cross-sectional findings, together with significantly more thought disorder in younger compared with older children with CPS, imply that thought disorder might reflect a developmental delay or disability involving the normal maturation of social communication skills in pediatric CPS [3].
Age at onset of CPS, a history of prolonged or febrile seizures, as well as localization and lateralization of epileptic activity, are, however, also associated with frontotemporal volumes in these children [7]. More specifically, earlier onset of CPS is related to smaller gray and white matter orbital frontal gyrus (OFG) volumes and temporal lobe white matter volumes, a history of prolonged seizures is related to increased inferior frontal gyrus (IFG) gray and white matter volumes, and left focal EEG activity is related to reduced total white matter volumes [7].
Recent structural imaging studies describe protracted maturation of frontotemporal regions associated with the integration of language and thought in normal children, with a decrease in gray matter density, but increase in white matter volumes, that continues through adolescence [8,9]. Functional imaging studies demonstrate involvement of Broca’s (i.e., IFG) and Wernicke’s (i.e., STG) areas, their right hemisphere homologs, and the dorsolateral prefrontal cortex (DLPFC) in how typically developing children make sense of the logic and topic of conversation [10].
Yet, these same language-associated brain regions are involved in the thought disorder of adults and youth with schizophrenia who have smaller left superior temporal gyrus (STG) [11,12], right temporal [13], and orbital frontal [14] volumes. Evidence for involvement of the orbital frontal lobe in both semantics [15,16] and seizure propagation [17] suggests that in addition to the previously described “classical” language areas, structural abnormalities in the orbital frontal lobe might also play a role in the thought disorder of children with CPS.
To delineate the mechanism of the thought disorder of children with CPS, we examined the relationship of these deficits to volumes of the previously described language-related brain regions and compared the data with those for age- and gender-matched healthy children. Based on our earlier findings [3,7], we predicted that children with CPS would have significantly more thought disorder and larger temporal lobe white matter volumes than age-and gender-matched healthy children. We also hypothesized that both the control children and those with CPS with thought disorder would have smaller frontal (i.e., IFG, OFG, DLPFC) and temporal (i.e., STG, Heschl’s gyrus (HG)) lobe volumes than those without thought disorder.
2. Methods
2.1. Subjects
The study included 42 children with cryptogenic epilepsy, all of whom had CPS, and 41 children without epilepsy aged 5–16 years (Table 1). The control group had significantly higher IQ scores and exhibited a trend toward more children from families of higher socioeconomic status based on the Hollingshead 2 factor index [18], which is derived from both parent occupational and educational status.
Table 1.
Demographic features of the CPS and normal groups
| CPS group | Normal group | |
|---|---|---|
| N | 42 | 41 |
| Age, mean (SD) | 10.2 (2.55) | 10.7 (2.41) |
| Gender | ||
| Male | 50% | 44% |
| Female | 50% | 56% |
| Socioeconomic statusa | ||
| High (I–III) | 26% | 46% |
| Low (IV–V) | 74% | 54% |
| Ethnicity | ||
| Caucasian | 66% | 54% |
| Non-Caucasian | 34% | 46% |
| Full Scale IQ, mean (SD)b | 94.2 (15.43) | 114.5 (13.20) |
χ2(1) = 3.20, P < 0.09.
t(75) = 0.46, P < 0.0001.
To be included in the study, the patients had to have cryptogenic epilepsy and CPS, as defined by the International Classification of Epilepsy [19], and at least one seizure during the year prior to participation in the study. As described in this classification, children with a clinical history of CPS but no EEG evidence of focal epileptic activity were also included in the study sample. We excluded patients with a mixed seizure disorder, a neurological disorder other than CPS, a metabolic disorder, a hearing disorder, past epilepsy surgery, and a structural MRI abnormality other than mesial temporal sclerosis.
We recruited 43% of the patients with CPS from tertiary centers (e.g., UCLA Pediatric Neurology Services, Children’s Hospital of Los Angeles) and 57% from the community (e.g., Kaiser Sunset, Kaiser— Orange County, private pediatric neurologists, Los Angeles chapter of the Epilepsy Foundation). UCLA institutional review board (IRB)-approved recruitment flyers were available for parents of children with CPS at each recruitment site. Parents who decided to enter their children into the study contacted the study coordinator, who provided information about the study and used a UCLA IRB-approved telephone script to determine if the children met the study’s inclusionary but none of the exclusionary criteria. The study coordinator also contacted the child’s pediatric neurologist to confirm the child’s diagnosis and to rule out exclusionary criteria.
Table 2 summarizes seizure frequency during the past year, current AEDs, age at onset, illness duration, as well as the numbers of febrile convulsions and prolonged seizures (i.e., >5 minutes) from the parents and the children’s medical records. Of the 42 patients with CPS, 10 had nonlateralized EEG findings at the time of the initial epilepsy diagnosis, 12 had a left focus, 6 a right focus, and 12 bilateral foci. EEGs were unavailable for 2 patients with CPS. Regarding focal EEG findings, 6 patients had no focal findings, and 14 had interictal spikes in the temporal lobe, 12 in the frontal and temporal lobes, and 8 in other areas. Two patients with CPS had secondary generalization and eight had background slowing. None of the subjects had mesial temporal sclerosis.
Table 2.
Epilepsy-related features of the CPS group
| Seizure frequency | |
| 1/year | 28% |
| 2–10/year | 31% |
| >10/year | 41% |
| Age at onset (years) | 6.6 (3.10) |
| Duration of iIllness (years) | 3.6 (2.51) |
| AEDs | |
| None | 2.4% |
| Monotherapy | 76.2% |
| Polytherapy | 21.4% |
| Prolonged seizures | 44% |
| Febrile convulsions | 15% |
To include children from a wide range of ethnic and socioeconomic backgrounds similar to those of the CPS group, we enrolled the nonepileptic control subjects from four public and two private schools in the Los Angeles community after screening for neurological, psychiatric, language, and hearing disorders through a telephone conversation with a parent. We excluded from the study children manifesting symptoms of these disorders in the past.
2.2. Procedures
This study was conducted in accordance with the policies of the Human Subjects Protection Committees of the University of California, Los Angeles. Informed assents and consents were obtained from all subjects and their parents, respectively.
2.2.1. MRI acquisition
All subjects completed MRI scanning on a 1.5-T GE Signa MRI scanner (GE Medical Systems, Milwaukee, WI, USA). The imaging acquisition protocol used to obtain high-resolution three-dimensional T1-weighted spoiled grass (SPGR) sequences included a sagittal plane acquisition with slice thickness of 1.2 mm, repetition time of 14.6, echo time of 3.3, flip angle of 35, acquisition matrix of 256×192, FOV of 24, and two excitations.
2.2.2. Image preprocessing
Each scan was processed with a series of steps to assess volumes of tissue types. Initially, potential fluctuations in signal resulting from magnetic field inhomogeneities were addressed by applying a radiofrequency correction [20]. Next, an automated brain extraction program (BET) was used to create a brain mask that separates brain tissue from nonbrain tissue (skull and meninges) [21]. This mask was manually modified to ensure accurate separation of tissues. The automated tissue classification method of Shattuck et al. [21] was then used to segment the scans by tissue types to create gray matter, white matter, and cerebrospinal fluid masks. The total intracranial volume was then automatically computed by summing the volumes of these masks.
2.2.3. MRI procedures: Cortical object model methods
2.2.3.1. Prefrontal cortex delineation
The protocol for subparcellating the prefrontal cortex, described in detail in Blanton et al. [22] and Daley et al. [7], can be viewed at http://www.loni.ucla.edu/NCRR/Downloads/Protocols/MaskingRegions.html. Briefly, by use of the cortical object model and all three viewing planes on the T1-weighted slices, the prefrontal cortex was subparcellated into the following regions of interest: IFG, DLPFC (i.e., sum of dorsolateral superior and middle frontal gyrus), and OFG.
2.2.3.2. Temporal lobe delineation
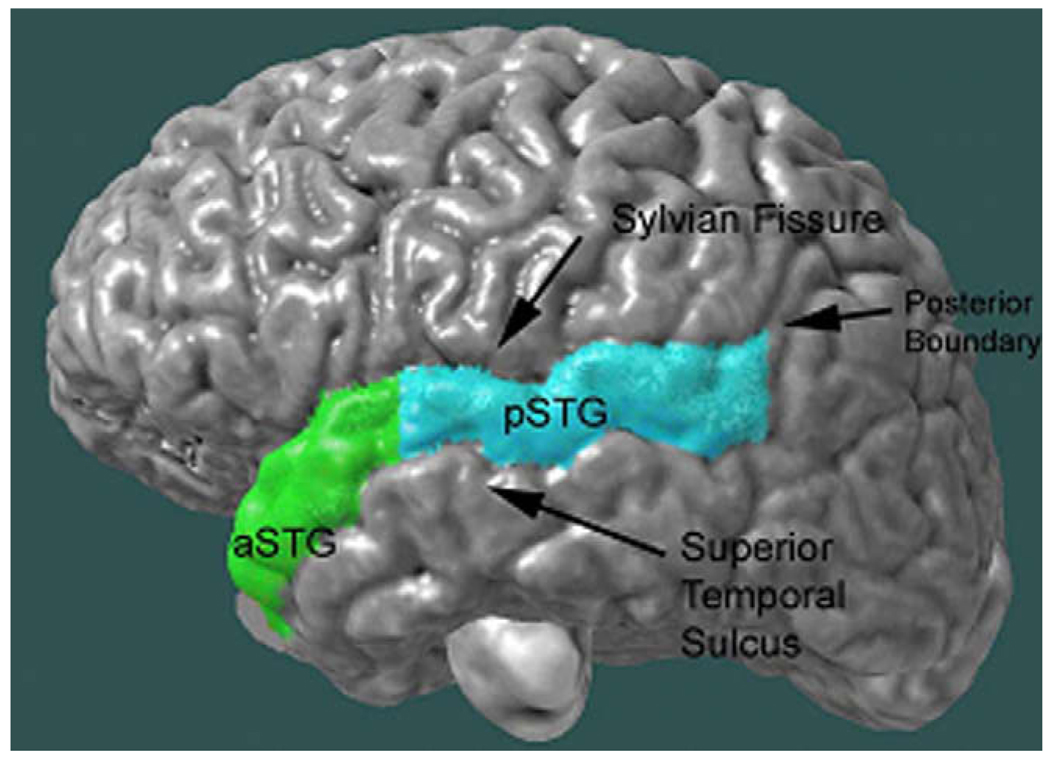
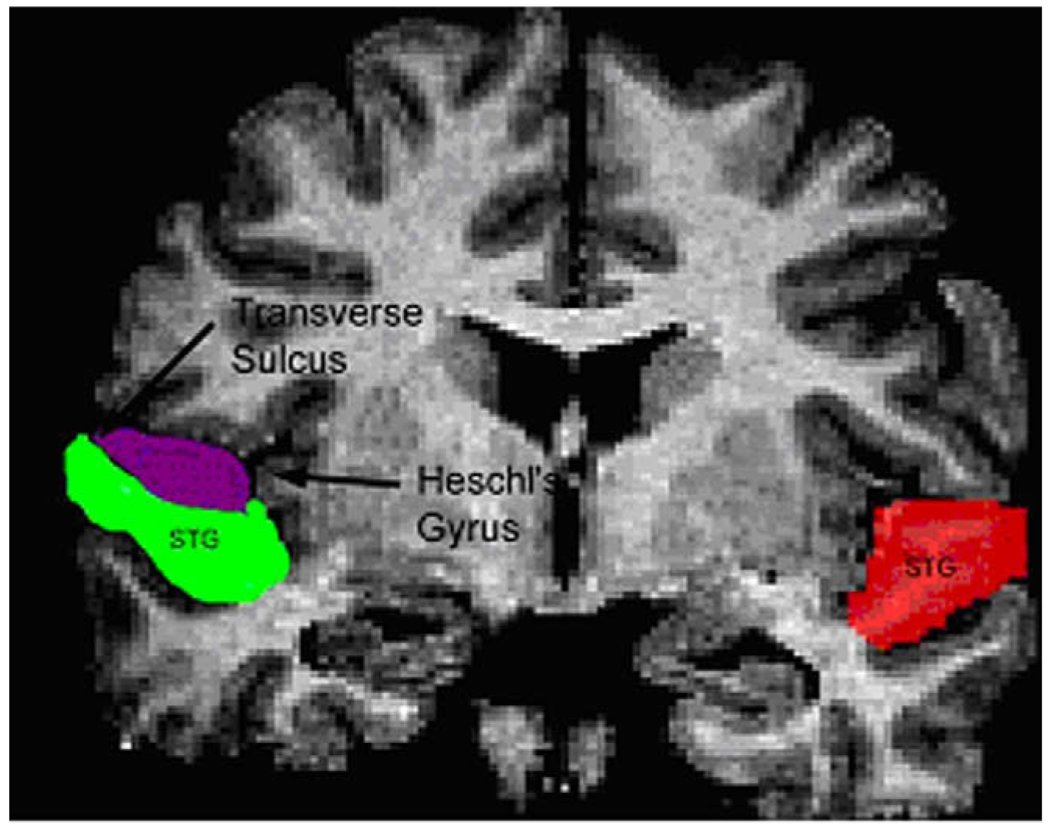
With all three viewing planes and the cortical object model, the temporal lobe was drawn in the sagittal plane as described by Daley et al. [7]. With the sylvian fissure and superior temporal sulcus as landmarks, the STG was delineated according to Taylor et al. [23] and parcellated into the anterior and posterior STG (Fig. 1) and HG (Fig. 2).
Fig. 1.
Three-dimensional view of STG and boundaries. The colors identify regions of the STG: green = left anterior STG, light blue = left posterior STG.
Fig. 2.
Heschl’s gyrus. The colors identify regions of the STG: green = left anterior STG, red = left posterior STG, purple = left HG.
2.2.4. Reliability
The drawings were made by one rater and checked by a second rater, both blind to the children’s diagnosis. A consensus drawing was then determined by agreement of the two raters about the boundaries of the regions of interest. The rater delineated the region of interest on the left hemisphere of 10 brains, and interclass correlation coefficients (ICCs) were calculated between these delineations and the gold standard. A rater was deemed reliable after achieving an ICC of 0.9 or higher. On brain regions examined in this study, the ICCs were 0.94 for IFG, 0.96 for middle frontal cortex, 0.95 for OFG, 0.90 for superior frontal cortex, 0.94 for temporal lobe, 0.83 for anterior STG, 0.88 for posterior STG, and 0.96 for HG.
2.2.5. Thought disorder
The Story Game [24] was used to elicit speech samples from children. Two raters with no knowledge of the children’s neurological diagnoses coded videotapes of the Story Game with the Kiddie Formal Thought Disorder Rating Scale (K-FTDS) [24] and transcriptions of the Story Game with Caplan and colleagues’ modifications [25,26] of Halliday and Hassan’s analysis of cohesion [27] and Evans’ [28] guidelines for repair (Table 3).
Table 3.
Definition and examples of thought disorder
| Thought disorder | Definition | Example |
|---|---|---|
| Formal thought disorder | ||
| Illogical thinking | Inappropriate or inadequate reasoning or contradiction | “I left my hat in her room because her name is Mary.” |
| Loose association | Unpredicted topic change to an unrelated topic | I: “Why’s that not Tim?” S: “I call my mom sweetie.” |
| Cohesion | ||
| Cohesion conjunctions | Ties together contiguous clauses (sentences) | The witch gets burned and that’s the end of story. |
| Referential cohesion | Pronoun, demonstrative, definite article, or comparative referring to person/object in the preceding spoken text | A boy called Peter saw a ghost. He was scared. |
| Unclear reference | Pronoun, demonstrative, definite article, or comparative referring to person/object unmentioned in prior text | I went and looked at the guy to see what they did. |
| Ambiguous reference | Referent that can apply to more than one person or object | Her mother made a costume and she was happy. |
| Exophora | Reference to immediate environment during conversation | I: Did you like that story? S: Open this toy. |
| Lexical cohesion | Ties between ideas by word repetition, synonym, antonym | The kids were bad. Tim was bad too. |
| Repair of the organization of thoughts | ||
| Repetition | Clarifies what was said by repeating word(s) | ‘Cause he wants… ‘cause he wants to play with him. |
| Postponement | Adds background information to clarify referent | And she knew when she found the kitten she knew that was what was making the girl happier. |
| False starts | Starts, but does not complete an idea | And um I don’t … Manniken said but I want to play. |
| Fillers | Word(s) that fills pauses without changing the meaning | Well, like, I don’t know, it’s just scary. |
| Revision of linguistic elements | ||
| Referential | Clarifies the referent | She would have Anne would have to take care of her. |
| Word choice | Modifies word choice | Play with him and make give him some wishes. |
| Syntactic | Corrects syntactic error | The picture you’re drawing you drew looks funny. |
The K-FTDS scores were frequency counts of illogical thinking and loose association ratings divided by the number of sentences (clauses) made by the child. The generalizability coefficient for illogical thinking and j for loose associations were 0.75 (SD = 0.15) and 0.66 (SD = 0.01), respectively, in a subsample of 39 epileptic and healthy subjects.
The cohesion scores, measuring the frequency with which the child used linguistic ties that connect ideas and referents across sentences, included: conjunctions, referential cohesion, lexical cohesion, ellipsis, unclear reference, ambiguous reference, and exophora. The interrater agreement (intraclass correlation) of these scores among a subsample of 31 children was 0.97 for conjunctions, 0.96 for referential cohesion, 0.97 for lexical cohesion, 0.99 for ellipsis, 0.99 for unclear/ambiguous reference, and 0.99 for exophora.
The repair scores are frequency measures of how often the child corrects errors in the organization of thoughts (e.g., fillers, false starts, repetition) or linguistic errors (e.g., syntax, semantics, reference) while speaking [28]. Interrater reliability (ICC) for the repair scores was 0.92 in a subsample of 45 children.
2.2.6. Cognition
The Wechsler Intelligence Scale for Children III [29] administered to the children generated Full Scale, Verbal, and Performance IQ scores.
2.2.7. Psychiatric diagnosis
We determined the presence/absence and type of DMS-IV diagnosis based on the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present and Lifetime Version (K-SADS-PL) [30], administered separately to each child and parent by R.C. or a research assistant trained in administration of the interview, as described in [31].
2.3. Statistical analyses
We compared total brain, gray matter, and white matter volumes between the CPS and normal groups using ANCOVAs. To compare frontal and temporal gray and white matter volumes in the CPS and normal groups, we estimated mixed models using repeated measures with group (CPS, normal) as the intersubject and hemisphere (left, right) as the intrasubject classification variable for IFG, OFG, DLPFC, and temporal lobes separately. Demographic (i.e., age, gender, socioeconomic status, and ethnicity) variables were used as covariates in all these analyses. Total brain volume was also included as a covariate for all analyses of volumes other than total brain volume.
Four categories of thought disorder, namely, formal thought disorder (illogical thinking, loose associations, exophora), cohesion (conjunction, referential cohesion, lexical cohesion, substitution, ellipsis), repair of errors in the organization of thinking (fillers, repetition, false starts, postponement), and revision of linguistic errors (word choice revision, syntactic revision, referential revision) were hypothesized (Table 1). Summary measures for each of these four categories of thought disorder were derived as described by Caplan et al. [3].
Within the CPS group, we examined the relationship of volumes to thought disorder scores with seizure, cognitive, demographic, and linguistic variables in the model. To decrease the number of seizure-related variables to include in the analyses, a principal component analysis (PCA) of seizure variables including subjects with CPS from all our studies (N = 105) was performed, as described by Caplan et al. [3]. This PCA revealed four components with the following loadings: a duration (0.89)/onset (−0.88) component; an EEG localization (0.87)/lateralization (0.87) component; a prolonged seizures (0.92)/febrile convulsions (0.79) component; and a seizure frequency (0.87)/number of AEDs (0.78) component. These four components were then used as the seizure-related variables when investigating their relationship to volumes in the CPS group.
In investigating the association of volumes with thought disorder, seizure, cognitive, and demographic variables, we computed general linear models for gray and white matter volumes for the frontal and temporal lobes and for the following parcellations: IFG, DLPFC, and OFG for the frontal lobe and STG (sum of anterior and posterior STG) and HG in the temporal lobe. Thought disorder scores (formal thought disorder, cohesion, repair revision), age, gender, ethnicity, socioeconomic status, the seizure components, and Full Scale IQ were used as predictors. We used the following model-building strategy to determine which of these variables were predictive of the volumetric measures. We first included all these variables as predictors in a stepwise regression model and determined a subset of predictors that contributed significantly (P < 0.1) to the variance. Then, following the fit of the model from stepwise selection, the importance of each variable included in the model was verified. We also checked for variables whose coefficients change markedly in magnitude when other variables were excluded. We then computed general linear models with this subset of predictors. Total brain volume was used as a covariate in these analyses. All tests were two-tailed, and an α level of 0.05 was adopted for all inferences.
3. Results
3.1. Between-group differences in thought disorder and volumes
Table 4 and Table 5 summarize mean thought disorder scores and volumes, respectively, for the study groups. ANCOVAs of the thought disorder scores with demographic variables in the model revealed higher formal thought disorder, cohesion, and revision scores in the CPS group compared with the normal group. Compared with the normal group, the CPS group had significantly smaller total gray matter and orbital frontal gray matter volumes and larger temporal white matter volumes, and exhibited a trend to-ward smaller white matter STG volumes.
Table 4.
Mean (SD) thought disorder scores in the CPS and normal groups
| Thought disorder | CPS group | Normal group |
|---|---|---|
| Formal thought disordera | 0.49 (0.26) | 0.33 (0.19) |
| Cohesionb | 0.43 (0.31) | 0.36 (0.22) |
| Repair | 0.39 (0.16) | 0.37 (0.17) |
| Revisionc | 0.47 (0.13) | 0.42 (0.12) |
F(1,77) = 8.0, P < 0.006.
F(1,77) = 7.22, P < 0.009.
F(1,77) = 3.52, P < 0.06.
Table 5.
Mean volumes in the CPS and normal groups
| Volume | CPS group | Normal group |
|---|---|---|
| Total | 0.43 (0.31) | 0.36 (0.22) |
| Gray mattera | 0.39 (0.16) | 0.37 (0.17) |
| White matter | 0.47 (0.13) | 0.42 (0.12) |
| Inferior frontal gyrus gray matter | 21.42 (3.43) | 22.61 (4.00) |
| Inferior frontal white matter | 9.95 (2.08) | 10.76 (2.74) |
| Orbital frontal gyrus gray matterb | 34.72 (5.52) | 36.14 (4.53) |
| Orbital frontal white matter | 16.12 (3.28) | 15.40 (3.21) |
| Dorsolateral prefrontal gyrus gray matter | 118.00 (17.25) | 121.41 (11.70) |
| Dorsolateral prefrontal gyrus white matter | 55.12 (9.65) | 55.08 (8.001) |
| Temporal lobe gray matter | 152.72 (11.84) | 155.85 (15.88) |
| Temporal lobe white matterc | 70.41 (12.27) | 66.35 (11.41) |
| Superior temporal gyrus gray matter | 38.05 (3.00) | 40.17 (3.81) |
| Superior temporal white matterd | 11.98 (1.38) | 13.24 (3.00) |
| Heschl’s gyrus gray matter | 2.73 (0.66) | 2.89 (0.61) |
| Heschl’s gyrus white matter | 1.03 (0.31) | 1.16 (0.30) |
F(1,77) = 4.89, P < 0.03.
F(1,75) = 3.83, P < 0.05.
F(1,74) = 5.26, P < 0.03.
F(1,62) = 2.99, P < 0.09.
3.2. Association between thought disorder and volumes
In the CPS group (Table 6), general linear models of brain volumes with thought disorder scores, seizure variables, and demographic variables as predictors demonstrated that higher formal thought disorder scores were significantly associated with smaller OFG gray matter volumes, DLPFC white matter volumes, and STG white matter volumes. Underuse of cohesion was related to smaller OFG gray matter volumes and increased HG gray matter volumes. However, smaller IFG gray matter volumes, increased temporal lobe white matter volumes, and larger HG gray matter volumes were significantly associated with underuse of repair. Impaired revision was also related to increased gray matter volumes of HG.
Table 6.
Thought disorder and brain volumes in the CPS and normal groups
| CPS group | Normal group | |||||||
|---|---|---|---|---|---|---|---|---|
| F | df | P | Directiona | F | df | P | Directiona | |
| Formal thought disorder | ||||||||
| Orbital frontal gyrus GMb | 4.34 | 1.27 | 0.04 | ↓ | 5.07 | 1.31 | 0.02 | ↑ |
| Dorsolateral prefrontal gyrus WM | 4.30 | 1.33 | 0.04 | ↓ | ||||
| Superior temporal gyrus WM | 4.50 | 1.20 | 0.04 | ↓ | ||||
| Cohesion | ||||||||
| Orbital frontal gyrus GM | 4.95 | 1.34 | 0.03 | ↓ | ||||
| Heschl’s gyrus GM | 11.92 | 1.22 | 0.002 | ↑ | ||||
| Superior temporal gyrus GM | 5.33 | 1.28 | 0.02 | ↑ | ||||
| Temporal lobe GM | 4.54 | 1.30 | 0.04 | ↑ | ||||
| Repair | ||||||||
| Inferior frontal gyrus GM | 5.81 | 1.34 | 0.02 | ↓ | ||||
| Temporal lobe GM | 5.21 | 1.30 | 0.02 | ↑ | ||||
| Temporal lobe WM | 5.95 | 1.25 | 0.02 | ↑ | ||||
| Heschl’s gyrus GM | 15.91 | 1.24 | 0.005 | ↑ | ||||
| Revision | ||||||||
| Heschl’s gyrus GM | 5.49 | 1.24 | 0.02 | ↑ | ||||
| Heschl’s gyrus WM | 9.01 | 1.28 | 0.005 | ↓ | ||||
↑(↓) indicates that higher thought disorder scores were associated with increased (decreased) volumes.
GM, gray matter; WM, white matter.
With demographic variables in the model for the normal group (Table 6), formal thought disorder scores were associated with increased OFG gray matter volumes. Larger gray matter STG and temporal lobe volumes were related to impaired cohesion (i.e., higher cohesion scores). Increased temporal lobe gray matter volumes were also associated with increased repair scores (i.e., under use of repair). Smaller HG white matter volumes were significantly related to impaired revision.
3.3. Secondary analyses
The study’s CPS findings were unrelated to the presence of EEG slowing (N = 8 CPS), a psychiatric diagnosis (3 ADHD, 7 affective/anxiety disorder, 7 both ADHD and affective/anxiety disorder, 1 tic disorder), and type of psychiatric diagnosis (i.e., ADHD vs affective/ anxiety/other vs no diagnosis). For those regions with volumes significantly associated with thought disorder, we also conducted additional analyses to determine how these findings were related to lateralization and localization of EEG done at the time of the child’s CPS diagnosis. We found a significant interaction of EEG lateralization with formal thought disorder scores for OFG gray matter volumes (F(3,19) = 3.66, P < 0.03). In the 12 children with left lateralization of epileptic activity, higher formal thought disorder scores were associated with smaller gray matter OFG volumes (t(19) = 3.16, P < 0.005). In contrast, in the 6 children with right lateralization of epileptic activity, high formal thought disorder scores were related to increased gray matter OFG volumes (t = 1.90, P < 0.07).
4. Discussion
The study’s findings demonstrate that thought disorder in the CPS group was related to reduced OFG and IFG gray matter volumes, increased HG gray matter volumes, smaller white matter DLPFC volumes, and increased temporal lobe white matter volumes, above and beyond the effects of seizure variables. These findings suggest that thought disorder might reflect the neuropathology underlying CPS. However, the association of age at onset, history of prolonged seizures, and left focal EEG findings with both thought disorder [1–3] and OFG, IFG, and temporal lobe volumes [7] also implies a seizure-related developmental vulnerability of both these higher-level linguistic skills and the associated brain regions in children with CPS. Supporting this conclusion, Ben Ari and Holmes [32] hypothesize that in the young animal, recurrent seizures might affect the ongoing construction of cortical networks or lead to displaced cells and migration disorders.
In contrast, thought disorder in young normal children during middle childhood and prepuberty [4] and its association with increased OFG and STG gray matter volumes but reduced HG white matter volumes might reflect a delay in the normal age-related decrease [9] in gray matter density and volumes and increase in white matter volumes in brain regions associated with language. The process of gray matter loss begins first in dorsal parietal cortices, particularly the primary sensorimotor areas near the inter-hemispheric margin, and then spreads rostrally over the frontal cortex and caudally and laterally over the parietal, occipital, and, finally, temporal cortex, particularly the posterior superior temporal gyrus [8]. This process is thought to reflect synaptic pruning together with trophic glial and vascular changes and/or cell shrinkage [8].
In parallel, children’s higher-level linguistic and discourse skills begin in the toddler period, undergo accelerated maturation during middle childhood, and continue to mature through the teenage years [see review in 33]. Thus, younger normal children have thought disorder compared with older normal children. They are illogical, make topic changes without preparing the listener for the topic change, use a narrow range of linguistic devices to connect ideas across sentences and to make reference to people, objects, or events, and also underuse linguistic devices to monitor and clarify communication breakdowns that occur while they speak.
The developmental implications of our findings are also supported by evidence that HG with its central role in processing speech, language, and rapid acoustic changes [34] has the highest concentration of white matter compared with other temporal lobe subregions [35]. Thus, reduced HG white matter volumes in the control subjects with impaired use of revision but increased HG gray matter volumes in the CPS subjects with impaired cohesion, repair, and revision might represent abnormalities in the parallel processes of increased myelination and decreased gray matter volumes that occur with age [8,9].
Interestingly, different brain regions were associated with the individual thought disorder components in the subjects with CPS compared with the control subjects. However, in both the CPS and control groups, the frontotemporal network involved in how children organize, monitor, and repair the coherence of their speech includes brain regions participating in language [36–38], the integration of linguistic function with semantic knowledge [39], and executive functions [40]. The consistent relationship of thought disorder with the OFG supports recent findings in schizophrenic adults whose thought disorder was associated with smaller left middle orbital frontal gyrus volumes [14]. It is also possible that the OFG findings reflect inclusion of Brodmann area (BA) 47, which contributes to semantic processing and control of semantic information [36,37], in the lateral boundaries of OFG. We defined the OFG as the cortex inferior to the frontal marginal sulcus, inferior and anterior to the lateral orbital sulcus, and lateral to the olfactory sulcus. The circular insular sulcus served as the most posterior boundary of the OFG [22].
Of relevance to epilepsy, the lateral OFG is also vulnerable to the propagation of mesial temporal seizures from the epileptogenic region to distant areas mediated by fiber tracts connecting the mesial temporal structures with ipsilateral lateral temporal, via the subicular cortex, the enthorhinal cortex, and perirhinal/parahippocampal cortices [17]. Thus, as suggested by our secondary analysis findings in the subjects with left CPS, the association of reduced OFG volumes with thought disorder might also represent effects of seizure propagation. The relationship of increased gray matter OFG volumes to thought disorder in the subjects with right CPS, similar to that in the control children with thought disorder, implies that the thought disorder of children with left and right CPS might involve different processes.
Formal thought disorder, which involves abnormal use of language to formulate, organize, and process thoughts, was related to DLPFC volumes. Yet, underuse of cohesion and repair, more basic linguistic functions, was associated with IFG, STG, HG, and temporal lobe volumes. These findings can be understood in light of the role of the DLPFC in executive functions [see review in 40] and thought disorder [41], whereas the STG and HG are implicated in semantics, syntax, phonology, and sentence processing [see review in 38]. As children with CPS have deficits in both executive [42] and basic linguistic [43] functions, we are currently studying how impaired executive function and language might mediate the impact of pediatric CPS on both thought disorder and frontotemporal volumes.
Study limitations include multiple, albeit hypothesis-driven statistical comparisons, retrospective rather than current EEG data, the relatively small sample size, particularly of children with right CPS, and the cross-sectional design of the study. Nevertheless, the findings suggest that thought disorder might represent a developmental disability involving decreased frontotemporal volumes of brain regions involved in language in pediatric CPS. They also add to the growing evidence of smaller IFG and OFG gray matter volumes in children with temporal lobe epilepsy with impaired executive function [44], reduced left posterior hemisphere gray matter volumes with poor academic performance in new-onset pediatric epilepsy [45], lower language and IQ scores in children with new-onset epilepsy with MRI evidence of structural abnormalities [46], and widespread decreased gray matter density that includes the left and right superior temporal gyrus in intractable pediatric temporal lobe epilepsy [47].
Acknowledgments
This study was supported by Grants NS32070 (R.C.) and MH067187 (R.C.). We appreciate the technical assistance of Amy Mo, Erin Lanphier, Ph.D., Pamela Vona, Lesley Stahl, and Ronald Seese.
References
- 1.Caplan R, Guthrie D, Komo S, Chayasirisobhon S, Mitchell W, Shields WD. Conversational repair in pediatric epilepsy. Brain Lang. 2001;78:82–93. doi: 10.1006/brln.2000.2447. [DOI] [PubMed] [Google Scholar]
- 2.Caplan R, Guthrie D, Komo S, et al. Social communication in pediatric epilepsy. J Child Psychol Psychiatry. 2002;43:245–253. doi: 10.1111/1469-7610.00017. [DOI] [PubMed] [Google Scholar]
- 3.Caplan R, Siddarth P, Bailey CE, et al. Thought disorder: a developmental disability in pediatric epilepsy. Epilepsy Behav. 2006;8:726–735. doi: 10.1016/j.yebeh.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Caplan R, Guthrie D, Komo S, Tang B, Asarnow R. Thought disorder in childhood schizophrenia: replication and update of concept. J Am Acad Child Adolesc Psychiatry. 2000;39:771–778. doi: 10.1097/00004583-200006000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Caplan R, Guthrie D, Tang B, Nuechterlein KH, Asarnow RE. Thought disorder in attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2001;40:965–972. doi: 10.1097/00004583-200108000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Van der Gaag RJ, Caplan R, van Engeland H, Loman F, Buitelaar JK. A controlled study of formal thought disorder in children with autism and multiple complex developmental disorders. J Child Adolesc Psychopharmacol. 2005;15:465–476. doi: 10.1089/cap.2005.15.465. [DOI] [PubMed] [Google Scholar]
- 7.Daley M, Levitt J, Siddarth P, et al. Frontal and temporal volumes in children with complex partial seizures. Epilepsy Behav. 2007;10:470–476. doi: 10.1016/j.yebeh.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 8.Ben-Ari Y, Holmes GL. Effects of seizures on developmental processes in the immature brain. Lancet Neurol. 2006;5:1055–1063. doi: 10.1016/S1474-4422(06)70626-3. [DOI] [PubMed] [Google Scholar]
- 9.Sowell ER, Peterson BS, Thompson PM, Welcome SE, Henkenius AL, Toga AW. Mapping cortical change across the human life span. Nat Neurosci. 2003;6:309–315. doi: 10.1038/nn1008. [DOI] [PubMed] [Google Scholar]
- 10.Dapretto M, Caplan R. Making sense: an fMRI study of discourse coherence in typically developing children. NeuroReport. 2005;16:1661–1665. doi: 10.1097/01.wnr.0000183332.28865.11. [DOI] [PubMed] [Google Scholar]
- 11.Shenton ME, Dickey CC, Frumin M, McCarley RW. A review of MRI findings in schizophrenia. Schizophr Res. 2001;49:1–52. doi: 10.1016/s0920-9964(01)00163-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holinger DP, Shenton ME, Wible CG, et al. Superior temporal gyrus volume abnormalities and thought disorder in left-handed schizophrenic men. Am J Psychiatry. 1999;156:1730–1735. doi: 10.1176/ajp.156.11.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsumoto H, Simmons A, Williams S, et al. Superior temporal gyrus abnormalities in early-onset schizophrenia: similarities and differences with adult-onset schizophrenia. Am J Psychiatry. 2001;158:1299–1304. doi: 10.1176/appi.ajp.158.8.1299. [DOI] [PubMed] [Google Scholar]
- 14.Nakamura M, Nestor PG, Levitt JJ, et al. Orbitofrontal volume deficit in schizophrenia and thought disorder. Brain. 2008;131:180–195. doi: 10.1093/brain/awm265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duffau H, Gatignol P, Mandonnet E, Peruzzi P, Tzourio-Mazoyer N, Capelle L. New insights into the anatomo-functional connectivity of the semantic system: a study using cortico-subcortical electrostimulations. Brain. 2005;128:797–810. doi: 10.1093/brain/awh423. [DOI] [PubMed] [Google Scholar]
- 16.Mandonnet E, Nouet A, Gatignol P, Capelle L, Duffau H. Does the left inferior longitudinal fasciculus play a role in language? A brain stimulation study. Brain. 2007;130:623–629. doi: 10.1093/brain/awl361. [DOI] [PubMed] [Google Scholar]
- 17.Gloor P. The temporal lobe and the limbic system. New York: Oxford University Press; 1997. [Google Scholar]
- 18.Hollingshead A. Medical sociology: a brief review. Milbank Mem Fund Q Health Soc. 1973;51:531–542. [PubMed] [Google Scholar]
- 19.Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia. 1989;30:389–399. doi: 10.1111/j.1528-1157.1989.tb05316.x. [DOI] [PubMed] [Google Scholar]
- 20.Sled J, Pike G. Standing-wave and RF penetration artifacts caused by elliptic geometry: an electrodynamic analysis of MRI. IEEE Trans Med Imaging. 1998;17:653–662. doi: 10.1109/42.730409. [DOI] [PubMed] [Google Scholar]
- 21.Shattuck D, Sandor-Leahy S, Schaper K, Rottenberg D, Leahy R. Magnetic resonance image tissue classification using a partial volume model. NeuroImage. 2001;13:856–876. doi: 10.1006/nimg.2000.0730. [DOI] [PubMed] [Google Scholar]
- 22.Blanton R, Levitt J, Peterson J, Fadale D, Porty M, Lee M. Gender differences in the left inferior frontal gyrus in normal children. NeuroImage. 2004;22:626–636. doi: 10.1016/j.neuroimage.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 23.Taylor JL, Blanton RE, Levitt JG, Caplan R, Nobel D, Toga AW. Superior temporal gyrus differences in childhood-onset schizophrenia. Schizophr Res. 2005;73:235–241. doi: 10.1016/j.schres.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 24.Caplan R, Guthrie D, Fish B, Tanguay PE, David-Lando G. The Kiddie Formal Thought Disorder Rating Scale: clinical assessment, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1989;28:408–416. doi: 10.1097/00004583-198905000-00018. [DOI] [PubMed] [Google Scholar]
- 25.Caplan R, Guthrie D, Foy JG. Communication deficits and formal thought disorder in schizophrenic children. J Am Acad Child Adolesc Psychiatry. 1992;31:151–159. doi: 10.1097/00004583-199201000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Caplan R, Guthrie D, Komo S. Conversational repair in schizophrenic and normal children. J Am Acad Child Adolesc Psychiatry. 1996;35:950–958. doi: 10.1097/00004583-199607000-00023. [DOI] [PubMed] [Google Scholar]
- 27.Halliday M, Hassan R. Cohesion in spoken and written English. London: Longmans; 1976. [Google Scholar]
- 28.Evans M. Self-initiated speech repairs: A reflection of communicative monitoring in young children. Dev Psychol. 1985;21:365–371. [Google Scholar]
- 29.Wechsler D. Wechsler Intelligence Scale for Children, 3rd ed (WISC-III) San Antonio: Psychological Corp; 1991. [Google Scholar]
- 30.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School Age Children Present and Lifetime version (K SADS PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 31.Caplan R, Sagun J, Siddarth P, et al. Social competence in pediatric epilepsy: insights on underlying mechanisms. Epilepsy Behav. 2005;6:218–228. doi: 10.1016/j.yebeh.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 32.Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caplan R. Discourse deficits in children with schizophrenia spectrum disorder. In: Beichtman JH, Cohen N, Konstantareas M, Tannock R, editors. Language, learning, and behavior disorders. Cambridge: Cambridge University Press; 1996. pp. 156–177. [Google Scholar]
- 34.Sigalovsky IS, Fischl B, Melcher JR. Mapping an intrinsic MR property of gray matter in auditory cortex of living humans: a possible marker for primary cortex and hemispheric differences. NeuroImage. 2006;32:1524–1537. doi: 10.1016/j.neuroimage.2006.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wallace M, Johnston PW, Palmer AR. Histochemical identification of cortical areas in the auditory region of the human brain. Exp Brain Res. 2002;143:499–508. doi: 10.1007/s00221-002-1014-z. [DOI] [PubMed] [Google Scholar]
- 36.Bookheimer S. Functional MRI of language: new approaches to understanding the cortical organization of semantic processing. Annu Rev Neurosci. 2002;25:151–188. doi: 10.1146/annurev.neuro.25.112701.142946. [DOI] [PubMed] [Google Scholar]
- 37.Poldrack RA, Wagner AD, Prull MW, Desmond JE, Glover GH, Gabrieli JDE. Functional specialization for semantic and phonological processing in the left inferior prefrontal cortex. NeuroImage. 1999;10:15–35. doi: 10.1006/nimg.1999.0441. [DOI] [PubMed] [Google Scholar]
- 38.Vigneau M, Beaucousin V, Herve PY, et al. Meta-analyzing left hemisphere language areas: phonology, semantics, and sentence processing. NeuroImage. 2006;30:1414–1432. doi: 10.1016/j.neuroimage.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 39.Hagoort P, Hald L, Bastiaansen M, Petersson KM. Integration of word meaning and world knowledge in language comprehension. Science. 2004;304:438–441. doi: 10.1126/science.1095455. [DOI] [PubMed] [Google Scholar]
- 40.Alvarez J, Emory E. Executive function and the frontal lobes: a meta-analytic review. Neuropsychol Rev. 2006;16:17–42. doi: 10.1007/s11065-006-9002-x. [DOI] [PubMed] [Google Scholar]
- 41.Stirling J, Hellewell J, Blakey A, Deakin W. Thought disorder in schizophrenia is associated with both executive dysfunction and circumscribed impairments in semantic function. Psychol Med. 2006;36:475–484. doi: 10.1017/S0033291705006884. [DOI] [PubMed] [Google Scholar]
- 42.Schoenfeld J, Seidenberg M, Woodard A. Neuropsychological and behavioral status of children with complex partial seizures. Dev Med Child Neurol. 1999;41:724–731. doi: 10.1017/s0012162299001486. [DOI] [PubMed] [Google Scholar]
- 43.Caplan R, Siddarth P, Gurbani S, Ott D, Sankar R, Shields W. Psychopathology and pediatric complex partial seizures: seizure -related, cognitive, and linguistic variables. Epilepsia. 2004;45:1273–1286. doi: 10.1111/j.0013-9580.2004.58703.x. [DOI] [PubMed] [Google Scholar]
- 44.Guimaraes CA, Bonilha L, Franzon RC, Li LM, Cendes F, Guerreiro MM. Distribution of regional gray matter abnormalities in a pediatric population with temporal lobe epilepsy and correlation with neuropsychological performance. Epilepsy Behav. 2007;11:558–566. doi: 10.1016/j.yebeh.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 45.Hermann B, Jones J, Sheth R, Dow C, Koehn M, Seidenberg M. Children with new-onset epilepsy: neuropsychological status and brain structure. Brain. 2006;129:2609–2619. doi: 10.1093/brain/awl196. [DOI] [PubMed] [Google Scholar]
- 46.Byars AW, deGrauw TJ, Johnson CS, et al. The association of MRI findings and neuropsychological functioning after the first recognized seizure. Epilepsia. 2007;48:1067–1074. doi: 10.1111/j.1528-1167.2007.01088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cormack F, Gadian DG, Vargha-Khadem F, Cross JH, Connelly A, Baldeweg T. Extra-hippocampal grey matter density abnormalities in paediatric mesial temporal sclerosis. NeuroImage. 2005;27:635–643. doi: 10.1016/j.neuroimage.2005.05.023. [DOI] [PubMed] [Google Scholar]