Abstract
Using the Perceived Stress Scale (PSS), perceptions of global stress were assessed in 111 women following breast cancer surgery and at 12 and 24 months later. This is the first study to factor analyze the PSS. The PSS data were factor analyzed each time using exploratory factor analysis with oblique direct quartimin rotation. Goodness-of-fit indices (root mean square error of approximation [RMSEA]), magnitude and pattern of factor loadings, and confidence interval data revealed a two-factor solution of positive versus negative stress items. The findings, replicated across time, also indicate factor stability. Hierarchical factor analyses supported a second-order factor of “perceived stress.” This alternative factor model of the PSS is presented along with observations regarding the measure's use in cancer research.
Keywords: perceived stress, factor analysis, breast cancer
During the past 2 decades, the construct of “stress” has received significant investigative attention as a correlate or predictor of psychological and health outcomes (see Cohen, Kessler, & Gordon, 1995; Dougall & Baum, 2001, for reviews). Stress, often conceptualized within a “stress and coping” framework (Lazarus, 1966; Lazarus & Folkman, 1984), has frequently been measured as perceptions or appraisals (Cohen, Kamarck, & Mermelstein, 1983; Sarason, Johnson, & Siegel, 1978; Vinokur & Selzer, 1975). Within this context, the Perceived Stress Scale (PSS; Cohen et al, 1983) has emerged as a popular choice to assess self-reports of globally perceived stress (i.e., the degree to which life is appraised as “unpredictable, uncontrollable, overloading,” p. 387). Evidence of the PSS's frequent usage comes from more than 385 citations found in the Social Sciences/Science Citation Indexes during the past 6 years. It is particularly common in psychoneuroimmunology/psychoneuroendocrinology studies among both healthy and some medical populations (Cohen, Doyle, & Skoner, 1999; Cruess et al., 1999; Glaser et al., 1999; Stoney, Niaura, Bausserman, & Matacin, 1999).
Rather than stress, psychosocial oncology researchers have emphasized a “quality of life” framework in their studies (Aaronson, 1988; Moinpour et al., 1989), with assessment focused on psychological (depression/anxiety, social support, body image/sexuality) and physical (fatigue/low energy, pain, general health) outcomes related to cancer diagnosis and treatment (Ganz et al., 1996; Maunsell, Brisson, & Deschenes, 1992). On the rare occasions the PSS has been used in adult cancer studies (de Moor et al., 2002; Sandgren, McCaul, King, O'Donnell, & Foreman, 2000; Schulz et al., 1995; Winzelberg et al., 2003), it has been as an outcome measure, much like measures of negative mood. Still, there has been interest in examining the cancer experience within a stress model (adult patients: Chernecky, 1999; pediatric patients: Varni & Katz, 1997; Wallander & Varai, 1992). In at least one model, cancer diagnosis/treatment has been conceptualized as a stressor (Andersen, Kiecolt-Glaser, & Glaser, 1994). The PSS offers one strategy to quantify stress responses among cancer patients. With it, investigators can, for example, test perceived stress as one explanatory mechanism for poorer quality of life outcomes in cancer patients.
For cancer investigators to study the effect of stress on patient outcomes, knowledge of the psychometric properties (i.e., factor solution/s) of stress measures, such as the PSS, is essential. However, there appear to be no factor analytic studies of the PSS. This is surprising because of the popularity of the measure and because factor analysis (FA) provides valuable information for measurement evaluation (construct validation, identification of latent variables; Floyd & Widaman, 1995, p. 286). We did find three studies that used principal components analysis (PCA). Unfortunately, PCA is limited to providing information on correlations between items, whereas FA reveals the relationships between unobservable factors and observable variables (see Fabrigar, Wegener, MacCallum, & Strahan, 1999, for a discussion). The PCA studies did not include cancer patients. One of the studies, conducted by the scale's author (Cohen & Williamson, 1988), used a probability sample of community-dwelling adults, and the other two were conducted with psychiatric samples (adult outpatients: Hewitt, Flett, & Mosher, 1992; adolescent inpatients: Martin, Kazarian, & Breiter, 1995).
Factor analytic data for the PSS is needed. Therefore, the primary research aim of the present study was to determine the factor pattern of the PSS using FA in a sample of women diagnosed with breast cancer. The measure was administered to the sample on three occasions, each 1 year apart, to test the stability of the factor solution and as an opportunity to replicate the findings.
METHOD
Participants
The participants were part of a prospective longitudinal study of women with breast cancer. Eligibility criteria included a confirmed diagnosis of regional (Stage 2 or 3) breast cancer, no previous cancer diagnoses, aged between 20 and 85 years, no refusal of cancer treatment prior to accrual, and no adjuvant treatment (e.g., chemotherapy, radiation) prior to accrual. Women with mental retardation, severe untreated psychopathology (e.g., schizophrenia, bipolar disorder), a current neurological disorder, dementia, chronic fatigue syndrome, or other immunologic conditions/diseases (e.g., rheumatoid arthritis) were excluded.
The accrual rate was 52%, which is higher than similar longitudinal studies (Cunningham et al., 1998; Goodwin et al., 2001). There were no significant differences (allps > .05) between participants versus nonparticipants in demographics (age, race, partner status), disease and prognostic characteristics (menopausal status, estrogen/progesterone receptor status, stage of disease, and number of positive lymph nodes), or treatment variables (extent of surgery, receipt of radiotherapy, type of adjuvant chemotherapy recommended). One- and 2-year retention rates were excellent at 89% and 86%, respectively. More detailed information regarding recruitment and accrual are available elsewhere (Golden-Kreutz & Andersen, 2004).
The subjects were 111 women; 87% were diagnosed with Stage 2 disease (Stage 3 = 13%). At the time of the initial assessment, all had been surgically treated (lump-ectomy=41 %; mastectomy = 59%) within the preceding 3 months and were awaiting the start of adjuvant treatment (e.g., chemotherapy, radiation). By the 12-month assessment, all had finished their adjuvant treatment, and at 24-months, all remained disease free. Demographic description of the sample was as follows: age (M = 51 years, SD = 10, range 31 to 84), racial group membership (Caucasian = 93%; African American = 6%; Hispanic = 1%), marital/partner status (76% with a partner), and years of education (M = 15.41; SD = 2.66; Mode = 16.00). Distribution of annual family income was < $15,000 = 7%; $15,000 to $29,000 = 15%; $30,000 to $49,000 = 23%; $50,000 to $79,000 = 24%; and >80,000 = 31%.
Procedure
Informed consent was obtained prior to the initial assessment. Reassessments occurred 12 and 24 months later. All assessments were conducted in person by research, assistants/nurses at the university's General Clinical Research Center or breast cancer clinic. Data included psychological, behavioral, and medical/treatment information from interviews, questionnaires, medical records, and when necessary, physician consultation. Women were paid $25.00 per assessment.
Measure
The PSS (10-item version; Cohen et al., 1983) is a standardized self-report questionnaire of globally perceived stress. The psychometric characteristics (internal reliability, “factor structure”) of the 10-item version are regarded by the authors as stronger in comparison to those of a 14-item version (Cohen & Williamson, 1988). Six of the items are negative (e.g., “How often have you felt nervous or stressed?”), and the remaining 4 are positive (e.g., “How often have you felt that things were going your way?”). Each item is rated for the past month on a 5-point Likert-type scale (1 = never to 5 = very often). In scoring the measure, the 4 positive items are reversed scored, and then all the items are summed (range from 0 to 40). A higher total score indicates greater stress. The measure has demonstrated adequate validity (Cohen et al., 1983). The 10 items are invariant with respect to race, sex, and education (Cole, 1999). Reliability coefficients, using Cronbach's alpha, ranged from .86 to .92, consistent with previous studies (range from .75 to .91; Cohen et al., 1983; Cohen & Williamson, 1988; Glaser et al., 1999). Although a 12-month test-retest interval is longer than that typically used, estimates from this sample ranged from .53 to .61, values similar to those reported by Cohen and colleagues (.55 for 6 weeks; 1983).
Analytic Strategy
Although the FA data of the PSS was of primary interest in the current study, descriptive analyses (i.e., means at each time-point) were also conducted. This included examining change in perceived stress across time using repeated analysis of variance (ANOVA).
For the FA, one has the choice between exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). CFA forces certain factor loadings to be zero. If there are any errors as to the prespecification of zero factor loadings, CFA does not readily indicate the exact positions of misspecified loadings. On the other hand, EFA does not force any factor loadings to be zero. Consequently, specification errors are more readily detected. EFA was chosen, therefore, as it avoids imposing preconceived ideas on the analysis and is able to detect any possible changes in factorial composition in time. The Comprehensive Exploratory Factor Analysis (CEFA) program (Browne, Cudeck, Tateneni & Mels, 1998) was used.
Three separate maximum likelihood FAs were conducted for each time point, for a total of nine. As previous PCA studies had reported a two-component solution (Cohen & Williamson, 1988; Hewitt et al., 1992; Martin et al., 1995), a two-factor solution was extracted. For verification purposes, one- and three-factor solutions were also extracted. Oblique direct quartimin rotation (Jennrich & Sampson, 1968) was applied with the two- and three-factor extractions. Oblique rotation allows the factors to become correlated and should improve the quality of the simple pattern of loadings. But as factors are not forced to be correlated, one has the choice to interpret the factors as correlated after inspection of the loadings. As evidence of stability, we expected the factor solution(s) to replicate (Byrne, Shavelson, & Muthen, 1989) across the three time points.
As a recommended guideline for using FA, the ratio of items to the number of cases was greater than 1:10 (Nunnally, 1978). No reverse scoring of items was done. The directionality of factors was chosen so as to yield preponderantly positive factor loadings. The correlations between the negative and positive items were then allowed to be negative, simplifying interpretation.
RESULTS
Preliminary Analyses
PSS descriptives
The total mean score at the initial assessment was 17.55 (SD = 6.72). Follow-up mean scores were lower (12 months: M = 14.13, SD = 6.46; 24 months: M = 14.04, SD = 7.07). Perceived stress significantly decreased overtime, F(2,105) = 18.78,p<.0001. Pairwise comparisons indicated that mean differences were only significant when comparing the initial time point with the later assessments (all ps < .001). Thus, the measure is capable of detecting change over time in the stress perceptions of cancer patients.
Primary Analyses
Factor solution and stability
Root mean square error of approximation (RMSEA; Steiger, 1989; see also Browne & Cudeck, 1993) was used as a quantitative means of assessing goodness of fit for each, model, with three models for each time point. Guidelines for RMSEA values are as follows: Close fit < .05; reasonable close fit = .05 to .07; mediocre fit = .07 to .10; and unsatisfactory fit > .10.
Considering the one-factor solution, the RMSEA values were between .10 and .12, suggesting an “unsatisfactory fit” of the data at each time point. Further, inspection of the residual matrix for the single-factor solutions (data not provided) showed a pattern of unacceptably large residuals, in the range from . 10 to .22. These results indicated that a one-factor solution is insufficient in representing the relationships between the items adequately and further factors were necessary.
RMSEA data for the two-factor solution indicated a “close fit” (all values < .05). Table 1 displays the solution, loadings, and confidence interval results. To interpret the factor loading data, confidence intervals were provided. If a confidence interval for a loading overlaps zero, it indicates that the associated significance test for a zero population loading will give a result that is not significant at the 10% level. Alternatively, if the confidence interval does not overlap zero, the associated significance test will yield a significant result. All the confidence intervals for both Factor 1 and Factor 2 loadings indicated significant differences from zero, with the only exception of Item F at 12 months. The two-factor solution fit the data well. Additionally, the two-factor solution was stable, as evidenced by the factor-loading pattern changing very little across the three time points.
TABLE 1.
Items, Factor Loadings, and Confidence Intervals for the Two-Factor Solution of the Perceived Stress Scale (PSS), Replicated Across Three Assessments
| Factor 1b |
Factor 2 |
|||||
|---|---|---|---|---|---|---|
| PSS Itemsa | Initial | 12-Month | 24-Month | Initial | 12-Month | 24-Month |
| A. ...angered because of things that happened that were outside of your control? | .90 (83, .99) | .44 (.20, .68) | .65 (.46, .84) | .15 (.10, .20) | -.31 (-.55, .06) | -.12 (-.33, .02) |
| B. ...unable to control the important things in your life? | .64 (.45, .82) | .32 (.09, .55) | .69 (.52, .87) | -.13 (-.34, .08) | -.47 (-.69, .24) | -.17 (-.37, .03) |
| C. ...nervous or "stressed"? | .60 (.41, .78) | .65 (.42, .86) | .64 (.44, .82) | -.20 (-.40, .01) | -.18 (-.42, .06) | -.19 (-.39, .02) |
| D. ...difficulties piling up so high that you could not overcome them? | .57 (.38, .75) | .76 (.55, .98) | .70 (.53, .87) | -.25 (-.46, .05) | -.08 (-.31, .16) | -.18 (-.37, .02) |
| E. ...that you could not cope with all the things that you had to do? | .56 (.36, .75) | .82 (.71, .94) | .97 (.91, 1.03) | -.12 (-.34, .09) | .13 (.05, .20) | .16 (.13, .19) |
| F. ...upset because of something that happened unexpactedly? | .45 (.25, .65) | .17 (-. 08, .42) | .38 (.15, .61) | .3[(-.52,-.10) | -.43 (-.67,-.20) | -.23 (-.47, .00) |
| G. ...confident abort your ability to handle your personal problems? | -.08 (-23, .07) | -.03 (-.19, .13) | .01 (-.09, .12) | .79 (.65, .93) | .83 (.68, .98) | .89 (.78, 1.00) |
| H. ...that things were going your way? | -.08 (-.24, .09) | -.02 (-.20, .17) | -.02 (-.17, .13) | .72 (.57, .88) | .73 (.56, .91) | .79 (.64, .94) |
| I. ...able to control irritations in your life? | .14 (.02, .27) | .05 (-.12, .21) | -.05 (-.26, .16) | .69 (.55, .84) | .75 (.59, .92) | .60 (.39, .80) |
| I. ...that you were on top of things? | -.07 (-.27, .12) | .03 (-.16, .23) | -.09 (-.26, .08) | .57 (.38, .75) | .70 (.51, .88) | .73 (.57, .89) |
All items begin with the stem, "How often have you been/felt..."
Factor loadings are in bold. 90% confidence intervals for the factor loadines are provided in parentheses.
All three RMSEA values for the three-factor solution were .05 or less, suggesting a “close fit.” The third factor consisted of two items. However, either the specific items comprising this factor or the magnitude of the item loadings changed across time. Specifically, the items and their loadings on the third factor included the following: Initial items, “could not cope with all the things you had to do?” (.98) and “control irritations in your life?” (.08); 12-month items, “difficulties piling up so high that you could not overcome them?” (.93) and “angered because of things that happened that were outside of your control?” (.36); and 24-month items, “difficulties piling up so high that you could not overcome them?” (.65) and “could not cope with all the things you had to do?” (.30). Although including an additional (third) factor yielded a better fit (and, therefore, a lower RMSEA value), the third factor was unstable.
DISCUSSION
The present study is the first to provide an FA of the PSS. Calculating one-, two-, and three-factor solutions enabled the evaluation of alternative factor models for the PSS. The RMSEA values, the magnitude and pattern of the factor loadings, and the associated confidence interval (CI) data showed that the one-factor solution had poor fit and the three-factor solution was unstable. In contrast, the two-factor solution provided the best fit and was stable across time. Factor 1 was composed of six negative items, whereas Factor 2 was composed of four positive items. Importantly, the longitudinal design allowed for a replication of the findings, providing a strong basis for our conclusions.
While the two-factor solution found with EFA is consistent with the previous PCA results (Cohen & Williamson, 1988; Hewitt et al., 1992; Martin et al., 1995), the PCA studies used an orthogonal rotation that restricted the correlation coefficient between the two factors to zero. In the present study, the oblique rotation employed not only resulted in a clearer pattern of loadings after rotation but, more important, consistently showed significant negative interfactor correlation coefficients of -.60 (CI = -.73, -.44), -.71 (CI = -.82, -.55), and -.72 (CI = -.82, -.60) at the three respective time points. These correlations would have been obscured if an orthogonal rotation had been used. Thus, the current data suggest that the two factors share a significant inverse relationship.
Examination of the PSS items comprising the two factors illustrates the authors' strategy of including “items that were negatively worded” (see Table 1, Items A through F) and “positively phrased statements” (Items G through J; Cohen & Williamson, 1988, p. 45). However, the authors consider any distinctions between the factors as “irrelevant” in the measurement of perceived stress (p. 45). Use of item keying for the same criterion response (i.e., inclusion of both “true” and “false” answers for items scored in the direction of the criterion) is a psychometric strategy to reduce acquiescence bias, presumably the intent of Cohen and colleagues (1983). However, close inspection of the four positive items of Factor 2 is important. Only one of the items (I:“... able to control the irritations in your life”) has a similar content to that of a negative item (B: “ ... unable to control the important things in your life”). The remaining items (G, H, and J) do not share similar content with any of the Factor 1 items. Indeed, the content of the Factor 2 items appear to tap positive emotions, feelings of confidence, things “going your way,” and being “on top of things.” Thus, keying (i.e., reverse scoring) is confounded with content for three of the four Factor 2 items.
These factor differences may be important. We suggest that the Factor 2 items can be understood as emotions/feelings counter to stress or those capable of undoing stressful, negative emotions (see Fredrickson, 2001, for a relevant discussion). One might even predict that the positive feelings sampled by Factor 2 are incompatible with the stress (i.e., negative) feelings of Factor 1, an explanation consistent with the high negative conelation coefficient found between the factors. Articulate cases have been offered for the view that “positive” constructs are more than the flip side of “negative” constructs (Fredrickson, 2001; Russell & Carroll, 1999). An alternative model of the perceived stress construct, as measured by the PSS, could reflect these potentially important positive and negative distinctions.
The alternative model, provided below, uses a second-order factor analysis model (Gorsuch, 1983, Ch. 11).This model is mathematically equivalent to the first-order model previously presented and fits the data to exactly the same extent. On the other hand, it is not conceptually the same, as it explicitly includes a single second-order “perceived stress” factor that accounts for the substantial negative correlation between the two first-order factors. This second-order factor influences all the measured variables through the first-order factors. A path diagram of the model is provided in Figure 1. Conventions specified by McArdle (1988, Section 2.2) are used. For simplicity of representation, only one dominant path per manifest variable is shown, and small loadings are disregarded. The 10 measured variables are shown in squares, and common and unique factors are shown in circles. Single-headed arrows represent the influence of factors on other variables in the system. Curved double-headed arrows represent common and unique factor variances or, equivalently, the sources of the variation and covariation in the measured variables.
FIGURE 1.
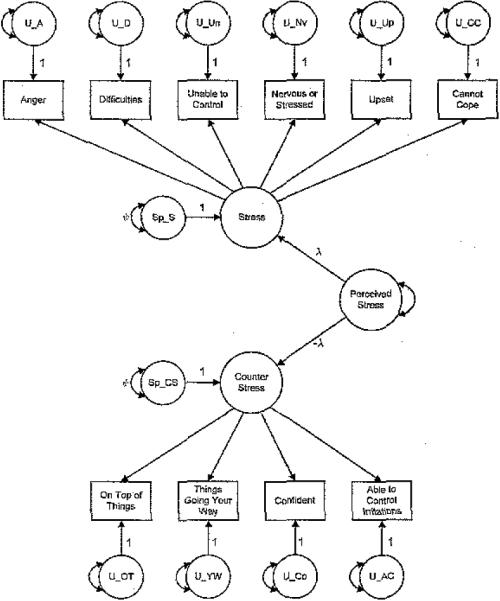
Conceptual Path Diagram of the Second-Order Factor Analysis Model for the Perceived Stress Scale (PSS)
As shown in Figure 1, a single second-order factor, Perceived Stress, influences the 2 first-order factors (Stress Emotions/Feelings [S] and Counter Stress Emotions/Feelings [CS]) equally but in different directions. As Perceived Stress increases, S increases and CS decreases. S is also affected by a specific factor, Sp_S. Similarly, CS is also affected by a specific factor, Sp_CS. The first 6 items are influenced directly by the first-order factor, S, and consequently, indirectly by Perceived Stress and Sp_S. CS has a direct influence on the last 4 items. Consequently, these are influenced indirectly by Perceived Stress and Sp_CS. Thus, the common second-order factor, Perceived Stress, influences all 10 items and is the main source of covariation among them. A further source of covariation amongst the first 6 items is the second-order specific factor, Sp_S. The other second-order specific factor, Sp_CS, is a further source of covariation: for the last 4 items. Second-order factor loadings, represented by λ and -λ in the diagram are ±.77, ±.85, and ±.84 for each of the three time points. The unique variances, represented by Ψ, all range from .38 to .40.
In sum, the hierarchical factor analytic model of the PSS, as presented in Figure 1, accounts for the presence of two factors (Stress and Counter Stress) as highly related manifestations of a single factor (Perceived Stress). This is consistent with the modified theoretical “stress and coping” model of Lazarus and Folkman (original 1966; 1984), which now includes the role of positive psychological states in coping with stress (Folkman, 1997). The revised model proposes that positive and negative psychological states “co-occur” during stress, and both have roles in the coping process (as opposed to earlier theories emphasizing the role of distress in coping outcomes). In particular, positive states (e.g., counter stress feelings/ emotions) influence individuals' appraisal or perceptions of a stressor/event as threatening (primary appraisal) as well as how they judge their ability to cope with the stressor/event (secondary appraisal). Thus, we propose that perceived stress, as measured by the PSS, may be composed of two dimensions, one positive (Factor 2/ Counter Stress) and the other negative (Factor 1/ Stress). Although Hewitt and colleagues (1992) named Factor 1 “perceived distress”and Factor 2 “perceived coping” and, more recently, Sandgren and McCaul (2003) identified Factor 2 as a measure of “perceived control,” none have placed these factors within the context of a theoretical model. Future research will need to test the construct validity of the two factors and make recommendations about their use as subscales.
In addition to presenting a second-order factor analysis of the PSS, several observations regarding its use with cancer patients are warranted. Measuring cancer patients' appraisals of stress with a measure such as the PSS is important as the cancer experience does not occur in isolation but rather in the context of the patient's daily living (family, social, and occupational responsibilities) and other ongoing stressors (financial difficulties; Golden-Kreutz & Andersen, 2004). For patients in tihe current study, perceived stress declined with time. The initial PSS scores appear to reflect the stress of the women's recent breast cancer diagnosis, surgery, and apprehension that often precedes adjuvant treatment. The significantly lower follow-up scores (p < .0001) likely reflect some resolution of stress after adjuvant treatments had ended. This is consistent with other studies reporting a significant decline in distress (mood, anxiety) from diagnosis onward for women with breast cancer (Edgar, Rosberger, & Nowlis, 1992; Lee et al., 1992).
Even though perceived stress may decline with time, data suggest that clinical interventions remain necessary and beneficial (see Andersen, 2002, for a discussion). For example, if quality of life outcomes are to be improved, the best time to offer psychological/behavioral interventions should be when stress is high—at the time of initial diagnosis and treatment. Despite any decline that occurs with time, it is the magnitude of initial stress that predicts later quality of life outcomes (increased negative affect: Varni & Katz, 1997; lower self-esteem/self-efficacy: Koopman et al., 2002; Varni, Katz, Colgrove, & Dolgin, 1994; and poorer physical health and sleep quality: Jacobsen et al., 1998). The PSS can provide clinical information regarding the degree to which cancer patients appraise their lives, in general, as stressful. When used within the context of a stress model, the measure has the potential to identify the role of perceived stress in important cancer outcomes, such as patients' quality of life and adherence to treatment.
Acknowledgments
This study was supported by the American Cancer Society (PBR-89), the Longaberger Company-American Cancer Society Grant for Breast Cancer Research (PBR-89A), the U.S. Army Medical Research Acquisition Activity Grants (DAMD17-94-J-4165; DAMD17-96-1-6294; DAMD17-97-1-7062), National Institute of Mental Health (RO1MH51487), National Cancer Institute (RO1CA92704; P30CA16058), and General Clinical Research Center (MO1-RR0034). The authors wish to thank the patients for their dedicatedparticipation and the research staff for subject recruitment and data collection. Thanks also to Tim Crespin, Ph.D., for helpful comments regarding the manuscript.
Biographies
Deanna M. Golden-Kreutz is a clinical health psychologist and research associate in the Department of Psychology at Ohio State University. She received an M.A. in counseling psychology from the University of Notre Dame (1987) and a Ph.D. in clinical psychology from Ohio State University (1993). Her primary clinical and research interests include the effect of cancer on mood, stress, and coping.
Michael W.Browne is a professor in the Department of Psychology at Ohio State University. He received his M.Sc. from the University of Witwatersrand (1958) and a Ph.D. from the University of South Africa (1969). His research interests have included the statistical modeling of multivariate psychological data and, more currently, the modeling of longitudinal data using nonlinear latent curve models and time series models.
Georita M.Frierson is a postdoctoral fellow in clinical psychology at Brown University Medical School. She received her Ph,D. in clinical psychology from Ohio State University (2003). Her primary research interests include sexual functioning among cancer patients and minority health issues.
Barbara L. Andersenis a professor in the Department of Psychology at Ohio State University. She graduated with a Ph.D. in clinical psychology from the University of Illinois (1980). She has published in the area of psychological and sexual outcomes for cancer patients. Currently, her research interests include investigating the role of stress, immunity, and survival in cancer patients.
REFERENCES
- Aaronson N. Quality of life: What is it? How should it be measured? Oncology. 1988;2:69–74. [PubMed] [Google Scholar]
- Andersen BL. Biobehavioral outcomes following psychological interventions for cancer patients. Journal of Consulting and Clinical Psychology. 2002;70:590–610. doi: 10.1037//0022-006X.70.3.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Kiecolt-Glaser JK, Glaser R. A bio-behavioral model of cancer stress and disease course. American Psychologist. 1994;49:389–404. doi: 10.1037//0003-066x.49.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–161. [Google Scholar]
- Browne MW, Cudeck R, Tateneni K, Mels G. CEFA: Comprehensive exploratory factor analysis. 1998 WWW document and computer program]. Retrieved from http://quantrm2.psy.ohio-state.edu/browne/
- Byrne BM, Shavelson RJ, Muthen B. Testing for partial measurement invariance. Psychological Bulletin. 1989;105:456–466. [Google Scholar]
- Chernecky C. Temporal differences in coping, mood, and stress with chemotherapy. Cancer Nursing. 1999;22:266–276. doi: 10.1097/00002820-199908000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle W, Skoner D. Psychological stress, cytokine production, and Severity of upper respiratory illness. Psychosomatic Medicine. 1999;61:175–180. doi: 10.1097/00006842-199903000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S, Kessler RC, Gordon LU. Measuring stress: A guide for health and social scientists. Oxford; New York: 1995. [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample in the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Sage; Newbury Park, CA: 1988. pp. 31–67. [Google Scholar]
- Cole S. Assessment of differential item functioning in the Perceived Stress Scale-10. Journal of Epidemiology and Community Health. 1999;53:319–320. doi: 10.1136/jech.53.5.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craess D, Antoni M, Kumar M, Ironson G, McCabe P, Fernandez J, et al. Cognitive-behavioral stress management buffers decreases in dehydroepiandrosterone sulfate (DHEA-S) and increases in me cortisol/DHEA-S ration and reduces mood disturbance and perceived stress among HIV-seropositive men. Psychoneuroendocrinology. 1999;24:537–549. doi: 10.1016/s0306-4530(99)00010-4. [DOI] [PubMed] [Google Scholar]
- Cunningham AJ, Edmonds CV, Jenkins GP, Pollack H, Lockwood GA, Warr D. A randomized controlled trial of the effects of group psychological therapy on survival in women with metastatic breast cancer. Psychological Oncology. 1998;7:508–517. doi: 10.1002/(SICI)1099-1611(199811/12)7:6<508::AID-PON376>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- de Moor C, Sterner J, Hall M, Warneke C, Gilani Z, Amato R, et al. A pilot study of the effects of expressive writing on psychological and behavioral adjustment in patients enrolled in a Phase II Trial of vaccine therapy for metastatic renal cell carcinoma. Health Psychology. 2002;21:615–619. doi: 10.1037//0278-6133.21.6.615. [DOI] [PubMed] [Google Scholar]
- Dougall AL, Baum A. Stress, health, and illness. In: Baum A, Revenson TA, Singer J,E, editors. Handbook of health psychology. Lawrence Erlbaum; Manwah, NJ: 2001. pp. 321–337. [Google Scholar]
- Edgar L, Rosberger Z, Nowlis D. Coping with cancer during the first year after diagnosis. Assessment and intervention. Cancer. 1992;69:817–828. doi: 10.1002/1097-0142(19920201)69:3<817::aid-cncr2820690334>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4:272–299. [Google Scholar]
- Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995;7:286–299. [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Social Science Medicine. 1997;45:1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Fredrickson E. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist. 2001;56:218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz P, Coscarelli A, Fred C, Kahn B, Polinsky ML, Petersen L. Breast cancer survivors: Psychosocial concerns and quality of life. Breast Cancer Research and Treatment. 1996;38:183–199. doi: 10.1007/BF01806673. [DOI] [PubMed] [Google Scholar]
- Glaser R, Kiecolt-Glaser J, Marucha P, MacCallum R, Laskowski B, Malarkey W. Stress-related changes in pro-inflammatory cytokrae production in wounds. Archives of General Psychiatry. 1999;56:450–456. doi: 10.1001/archpsyc.56.5.450. [DOI] [PubMed] [Google Scholar]
- Golden-Kreutz DM, Andersen BL. Depressive symptoms after breast cancer surgery: Relationships with global, cancer-related, and life event stress. Psycho-Oncology. 2004;13:211–220. doi: 10.1002/pon.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin PJ, Leszcz M, Ennis M, Koopmans J, Vincent L, Gather H, et al. The effect of group psychosocial support on survival in metastatic breast cancer. New England Journal of Medicine. 2001;345:1719–1726. doi: 10.1056/NEJMoa011871. [DOI] [PubMed] [Google Scholar]
- Gorsuch RL. Factor analysis. 2nd ed Lawrence Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Hewitt PL, Flett GL, Mosher SW. The Perceived Stress Scale: Factor structure and relation to depression symptoms in a psychiatric sample. Journal of Psychopathology and Behavioral Assessment. 1992;14:247–257. [Google Scholar]
- Jacobsen P, Widows M, Hann D, Andrykowski M, Kronish L, Fields K. Post-traumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosomatic Medicine. 1998;60:366–371. doi: 10.1097/00006842-199805000-00026. [DOI] [PubMed] [Google Scholar]
- Jennrich R, Sampson P. Rotation for simple loadings. Psychometrika. 1968;31:313–323. doi: 10.1007/BF02289465. [DOI] [PubMed] [Google Scholar]
- Koopman C, Butler L, Classen C, Giese-Davis J, Morrow G, Westendorf J, et al. Traumatic stress symptoms among women with recently diagnosed primary breast cancer. Journal of Traumatic Stress. 2002;15:277–287. doi: 10.1023/A:1016295610660. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Psychological stress and the coping process. McGraw-Hill; New York: 1966. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- Lee MS, Love SB, Mitchell JB, Parker EM, Reubens RD, Watson JP, et al. Mastectomy or conservation for early breast cancer: Psychological morbidity. European Journal of Cancer. 1992;28A(89):1340–1344. doi: 10.1016/0959-8049(92)90514-3. [DOI] [PubMed] [Google Scholar]
- Martin RA, Kazarian SS, Breiter HJ. Perceived stress, life events, dysfunctional attitudes, and depression in adolescent's psychiatric patients. Journal of Psychopathology and Behavioral Assessment. 1995;17:81–95. [Google Scholar]
- Maunsell E, Brisson J, Deschenes L. Psychological distress after initial treatment of breast cancer. Assessment of potential risk factors. Cancer. 1992;70:120–125. doi: 10.1002/1097-0142(19920701)70:1<120::aid-cncr2820700120>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- McArdle JJ. Dynamic but structural equation modeling of repeated measures data. In: Nesselroade JR, Cattell RB, editors. Handbook of multivariate experimental psychology. 2nd ed. Plenum; New York: 1988. pp. 56l–614. [Google Scholar]
- Moinpour CM, Feigl P, Metch B, Hayden KA, Meyskens FL, Crowley J. Quality of life end points in cancer clinical trials: Review and recommendations. Journal of the National Cancer Institute. 1989;81:485–495. doi: 10.1093/jnci/81.7.485. [DOI] [PubMed] [Google Scholar]
- Nunnally JC. Psychometric theory. 2nd ed. McGraw-Hill; New York: 1978. [Google Scholar]
- Russell J, Carroll J. On the bipolarity of positive and negative affect. Psychological Bulletin. 1999;125:3–30. doi: 10.1037/0033-2909.125.1.3. [DOI] [PubMed] [Google Scholar]
- Sandgren A, McCaul K. Short-term effects of telephone therapy for breast cancer patients. Health Psychology. 2003;22:310–315. doi: 10.1037/0278-6133.22.3.310. [DOI] [PubMed] [Google Scholar]
- Sandgren A, McCaul K, King B, O'Donnell S, Foreman G. Telephone therapy for patients with breast cancer. Oncology Nursing Forum. 2000;27:683–688. [PubMed] [Google Scholar]
- Sarason G, Johnson J, Siegel J. Assessing the impact of life changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Schulz R, Williamson G, Knapp J, Bookwala J, Lave J, Fello M. The psychological, social, and economic impact of illness among patients with recurrent cancer. Journal of Psychosocial Oncology. 1995;13:21–45. [Google Scholar]
- Steiger JH. EzPATH: A supplementary module for SYSTAT and SYGRAPH. SYSTAT; Evanston, IL: 1989. [Google Scholar]
- Stoney C, Niaura R, Bausserman L, Matacin M. Lipid reactivity to Stress: I. Comparison of chronic and acute stress responses in middle-aged airline pilots. Health Psychology. 1999;18:241–250. doi: 10.1037//0278-6133.18.3.241. [DOI] [PubMed] [Google Scholar]
- Varni J, Katz E. Stress, social support and negative affectivity in children with Newly diagnosed cancer: A prospective transactional analysis. Psycho-Oncology. 1997;6:267–278. doi: 10.1002/(SICI)1099-1611(199712)6:4<267::AID-PON277>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Varni J, Katz E, Colegrove R, Dolgin M. Perceived stress and adjustment of long-term survivors of childhood cancer. Journal of Psychosocial Oncology. 1994;12:1–16. [Google Scholar]
- Vinokur A, Selzer M. Desirable versus undesirable life events: Their relationships to stress and mental distress. Journal of Personality and Social Psychology. 1975;32:329–337. doi: 10.1037//0022-3514.32.2.329. [DOI] [PubMed] [Google Scholar]
- Wallander J, Varni J. Adjustment in children with chronic physical disorders: Programatic research on a disability-stress-coping model. In: La Greca AM, Siegel LJ, Wallander JL, Walker CE, editors. Stress and coping in child health. Guilford; New York: 1992. pp. 279–298. [Google Scholar]
- Winzelberg A, Classen C, Alpers G, Roberts H, Koopman C, Adams R, et al. Evaluation of an Internet support group for women with primary breast cancer. Cancer. 2003;97:1164–1173. doi: 10.1002/cncr.11174. [DOI] [PubMed] [Google Scholar]


