How can health care reform approach the holy trinity of equitable access, controlled costs, and high value?
How can the sweet spot be found in the midst of the politically charged and personally wrenching trade-offs? The sweet spot is where increasing access to health care creates a sense of commonality rather than division, where choices about the use of services are prioritized based on personalized knowledge rather than crude administrative rationing, and where cost control happens in ways that add value and diminish waste.
Previously, this editorial series examined the problem of fragmentation,1 a generalist solution,2 and the paradox of primary care.3 This fourth piece in the series explores an integrated way of understanding how the components of health care can work together to balance access, cost, and quality. This framework is not so much a cookbook as a way of making sense of the current situation and a guidepost for traveling hopefully to a better future.
CONNECTING THE PARTS AND THE WHOLES
In the summer of 1968 in the Austrian mountain hamlet of Alpbach, author Arthur Koestler convened a scientific symposium intended to challenge “the insufficient emancipation of the life sciences from the mechanistic concepts of nineteenth-century physics and the resulting crudely reductionist philosophy.”4 The participants’ task then is highly relevant to health care today, which is stuck in a similarly old-fashioned worldview that does not fit the reality of how health is lost and created, and how the pieces of health care evolve together to create value.
At the Alpbach Symposium, scientists from a variety of fields, including biologist Paul Weiss, biochemist Holger Hydén, developmental psychologists Jean Piaget and Bärbell Inhelder, psychopharmacologist Sey-mour Kety, humanist psychiatrist Viktor Frankl, evolutionary biologist C. H. Waddington, and the father of general systems theory, Ludwig von Bertalanffy, presented data from vastly diverse experiments and observational studies. The common thread—actually more of a chain of evidence—was that biological and social phenomena, like molecular and physical occurrences, evolve as events with many degrees of freedom, but with “ordering restraints exerted upon them by the integral activity of the ‘whole’ in its patterned systems dynamics.” 5(9)
Symposium participants described life in different ways—observations, scientific experiments, mathematical formulae. But they agreed on the concept that the phenomena of life (as well the physical world) are best understood as both parts and wholes. Koestler called these wholes that simultaneously are parts of other wholes holons.6 The world, be it atoms, cells, or social phenomena, is made up of holons.
Holons are arranged in nested hierarchies that Koestler called holarchies. For example, subatomic particles are included in atoms, which are subsumed by molecules, which make up crystals, and so on. Each higher level transcends and includes the one below.
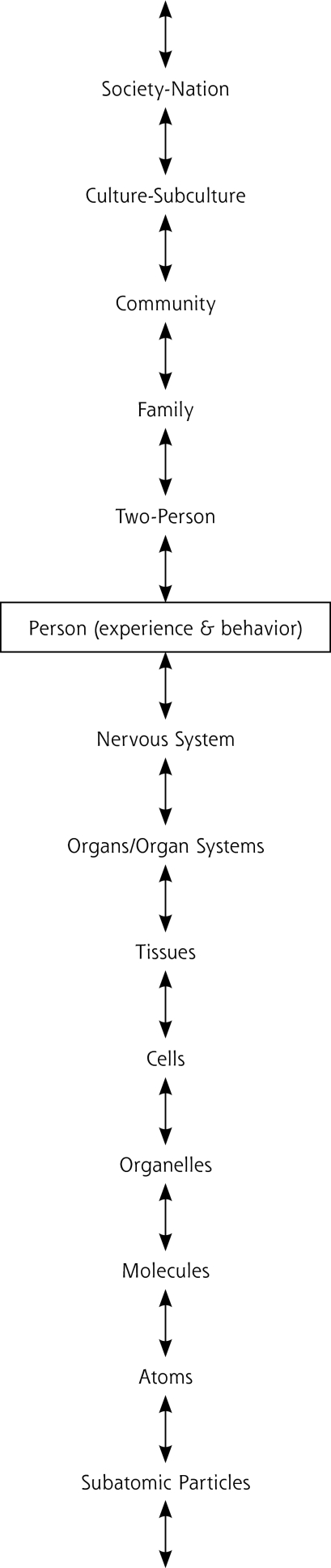
A decade later, psychiatrist George Engel identified similar relationships in health care and health. Seeing that “all of medicine is in crisis” from “adherence to a model of disease no longer adequate for the scientific tasks and social responsibilities of either medicine or psychiatry,”7 Engel8 articulated a similar hierarchy to the one proposed at Alpbach. As displayed in Figure 1 ▶, each higher level in this holarchy (atom, molecule, organelle, cell, and on) transcends but includes the level below.
Figure 1.
Systems hierarchy (levels of organization).
Adapted, with permission, from: Engel G. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137:535-544. Engel’s original diagram included “Biosphere” at the top and did not have arrows at either end indicating that the holarchy continues on in both directions.
More recently, understanding of complex adaptive systems has further evolved9–21 in ways that put the useful concepts of holons and holarchies into a richer context for understanding how health care can be improved. Ken Wilber has synthesized much of this evolved understanding,22,23 including the following principles24:
Reality is composed “of wholes that are simultaneously parts of other wholes, with no upward or downward limit.”
Holons can be understood both horizontally and vertically. At the horizontal level, they balance self-preservation and adaptation, conserving themselves with time, while adjusting to other holons at their level. Vertically, they balance the possibility of self-dissolution to a lower level, and transcendency— becoming part of another holon—at a higher level. Extensive pathologies can appear when these balances are not right.
Emergent holons transcend but include their predecessors. As they do so, new properties emerge that are more than the sum of the properties that came before. Furthermore, each higher level of evolution produces greater depth (but smaller numbers of holons). Thus, lower level holons are more fundamental; higher levels are more evolved.
Holarchies coevolve with other holons and holarchies in their environment, but each level continues to depend on a network of relationships with other holons at the same level.
Evolution of holons moves toward greater differentiation, variety, complexity, and organization.
How can these concepts help us understand the provision of high-value health care?
A HOLARCHY OF HEALTH CARE
The components of health care, much as the phenomena of the natural world, also can be understood as both parts and wholes—as holons. The holons of health care, such as services, structures, and relationships, are more than isolated commodities to be delivered, bought, and sold. They are related to each other in observable ways that include hierarchies of holons, ie, holarchies.
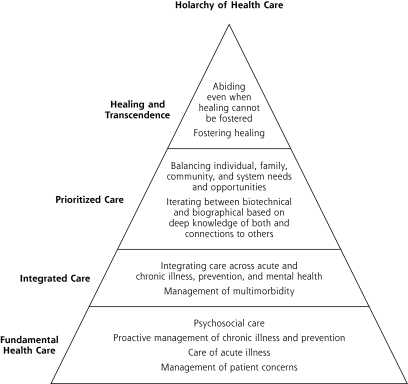
Figure 2 ▶ depicts 4 levels of health care, ranging from fundamental to healing and transcendence. The lower, more fundamental, holons in this holarchy enable higher-order functions, such as integrating, prioritizing, and personalizing. The higher-order functions of health care transcend but include the lower—adding new emergent properties that build on, but are more than, the sum of those below.
Figure 2.
Holarchy of health care.
As in any holarchy, there are other levels above and below. Levels lower than those depicted likely relate to instrumental factors (such as scheduling and record keeping) that enable health care. Higher levels likely relate to spiritual dimensions of care.
The holons of health care in the 4 related levels in Figure 2 ▶ are described below.
Fundamental Health Care
Fundamental health care relates to addressing patient concerns, acute and chronic illnesses, prevention, and mental health. The reasons patients seek health care services have been empirically classified as desire for medical information, psychological assistance, therapeutic listening, general health advice, and biomedical treatment.25 Addressing the reasons for the visit obviously is fundamental to meeting patients’ needs.
More than one-third of all outpatient visits26 and nearly two-thirds of visits to family physicians27 are for care of acute illness. In such specialties as dermatology or cardiology, the top 6 diagnosis clusters account for 70% to 90% of patient visits.28,29 In primary care, reasons for visits are so diverse that only one-half can be classified in the top 20 diagnosis clusters.27–29 Many of these acute illnesses are self-limited and thus require medical care only to the degree to which they cause patient concern or have symptoms that the patient needs help managing. Instrumentally, care of such conditions may be well managed by allied health professionals or in urgent care settings. What is not known is the degree to which providing acute illness care in a single medical home or with a personal clinician fosters the trust and interpersonal relationships that are needed to fully perform higher-order health care functions.
Chronic illnesses account for a substantial and growing proportion of health care—37% of all outpatient visits in the United States in 2006.26 This proportion is increasing substantially as the population ages and as behavioral risk factors and obesity increase the prevalence of chronic diseases, such as diabetes, hypertension, osteoarthritis, and cancer.30 Preventive care is the main focus of 19% of all outpatient visits,26 and in primary care, one-third of visits for illness involve preventive service delivery,31 often tailored to risk factors32–34 or teachable moments.35,36 Both chronic illness management and effective delivery of preventive services require a proactive approach and supportive systems that go beyond reacting to patient concerns and providing acute illness care.37 Thus, much current health care systems research and development is focused on increasing the ability of primary care to prevent and manage chronic illness.38,39
Recent efforts to control costs and increase quality by “carving out” mental health care have led to increasingly fragmented care.40,41 There are, however, great opportunities for both controlling costs and improving care and outcomes by integrating primary medical and mental health care.40,42–44 Psychosocial care also involves helping patients manage life events and the stresses and joys of daily living that do not cross the threshold to a mental health diagnosis.40,45 An ongoing patient-physician relationship developed over time can provide a basis for integrating mental and physical health care.46,47
Integrated Care
Multimorbidity (the co-occurrence of multiple medical conditions) and comorbidity (the co-occurrence of conditions beyond a particular index condition)48 are seen in one-half of all outpatient visits.26 Multimorbidity, particularly common in the aging population49,50 is the rule rather than the exception among primary care patients,48–54 and the typical primary care visit addresses 3 to 4 problems.51,52 Most scientific evidence explicitly excludes people with comorbid conditions, however.49,53 Thus, because of limitations in the current scientific paradigm, the care of multiple conditions, particularly the care of whole people with multiple conditions, is relegated to the art rather than the science of medicine. Evidence-based guidelines are not helpful; in fact, they are potentially harmful for a large proportion of patients seen in primary care.49,53–55
Higher-level health care involves not only attending to multiple chronic medical conditions, but also requires the integration and personalized prioritization of care across acute and chronic illness, prevention, and mental health.2,3,56–58
Prioritized Care
The ability to prioritize and integrate care based on an inclusive view and personal knowledge is a crucial primary care function that is only beginning to be recognized. Although recent research has begun to provide evidence on how preventive services can be prioritized at the level of the population,59 prioritization of care at the level of the person and across acute and chronic illness, prevention, and mental health has received scant attention in medical science.56 Prioritization and integration of care may help explain the paradox3 that primary care–based systems result in better population health and lower costs60,61 and higher (or similar) quality of care62 at lower cost,63,64 despite evidence that evidence-based guidelines are followed at lower rates. At the individual level, prioritization can involve protecting patients from overuse of tests with high false-positive rates that begin a cascade of interventions and procedures of marginal benefit.65 At the system level, prioritizing care may involve efficient care of families66,67 and use of equally effective but lower-cost treatments.68
Primary care benefits the individual and the health care system by balancing biotechnical and biographical care.69,70 This balance is a complex function that results in the personalized application of the best scientific evidence, tempered by the best evidence from personal context.71 Limiting resource use at the system level can only be done crudely, where it is widely seen as rationing. Selective use of resources, however, based on first-contact access, a comprehensive whole-person family and community focus, care integration, and continuous relationships,72,73 results in prioritized care that protects patients from overtreatment.65 Personalized care that is prioritized based on knowledge of the person, family, and community rather than crude system-level rationing is most likely to enhance benefit to the person and the population.
Healing and Transcendence
Healing sometimes involves more than cure. It involves the transcendence of suffering.74–76 For optimal healing, clinicians must identify and develop knowledge of opportunities for cure, the values of the patient, connection with community, and possibilities for transcendence. Sometimes healing cannot be fostered. A difficult and important aspect of health care is to stick with the patient and family even when “success” is not forthcoming. This is a higher, noninstrumental level of caring.
The healing and transcendence level of the holarchy of health care is particularly important during key moments in the life cycle, such as life-threatening illness or a major personal or family event. Death and dying45,77 in particular are poorly handled by the US health care system, both in terms of cost78 and human suffering.79,80 High-order healing functions can be fostered by specific short-term approaches to care81 and by longitudinal relationships and abiding over time.74–76 Patients particularly recognize the value of healing relationships when they include both going through a key event together and abiding over time.46,47
Although much is made of the importance of medical professionalism,82,83 there is a role that surpasses that of clinician or even healer. This role involves being a friend, and when it is appropriate, it represents not a loss of professionalism as much as an expression of unselfish love that is the mark of the healer.2
APPLYING THE HOLARCHY OF HEALTH CARE
A previous article in this series2 told the story of a patient, Jim Bauer. Jim received fundamental care over time, which enabled moving to the higher level of an integrated approach to diagnosis and treatment when he developed a complicated illness. The ongoing relationship helped difficult therapeutic decisions about treatment for 2 cancers and an aortic aneurysm to be prioritized in a way that was congruent with Jim’s values, avoided individual risk, and maximized value for the system. A temporary break in this relationship diminished the opportunity for healing and transcendence during the time immediately before his death. The therapeutic relationship, however, was resumed with the “hidden patient,”45 Jim’s wife, Doris, who received care across the entire continuum of the holarchy of care.
Understanding the holarchy of health care can help us organize health care more effectively. For example, if information systems, which currently function at the fundamental level, were expanded to include information on patient preferences and individual medical risks, reminder systems would better enable care integration, personalization, and prioritization across multiple illnesses and domains. Systems that balance convenience of access with enhancing access to a personal clinician and health care team during key transitions and life events could change health care from an isolated commodity into a relationship-centered continuum that maximizes integration, prioritization, and when needed, healing and transcendence. If we take seriously the need for time to develop person-focused relationships that are required for development up the health care holarchy, we would minimize the unhelpful distraction of disease-specific coding and incentives for fundamental primary care,84–86 reimbursing instead for accessibility, comprehensiveness, integration, and personalization functions that provide the added value of primary care.58,73,87 A holarchy-informed system would engage primary care clinicians as a first contact and an ongoing resource for integrating and prioritizing care, engaging specialty care selectively when it can be most effective.62,88–90 An effective system to enable individuals, families, and communities to evolve along the holarchy would have at least a 50-50 mix of generalists and specialists, rather than the current and worsening imbalance found in the United States.
LIMITATIONS
The holarchy of health care displayed in Figure 2 ▶ interacts with other holarchies and evolves with time. Thus, an accurate depiction of the holarchical system of health care needs to consider its interactions with other systems. The biological and social processes that cause health and illness (some of which are included in Figure 1 ▶) are an important factor in how health care works, just as economic and environmental systems affect both health care and health.
In addition, the levels of the holarchy of health care proceed to both higher and lower levels of development beyond those levels that are shown. Higher levels likely involve spiritual dimensions. Lower levels likely involve factors that enable fundamental health care. A full depiction of these multiple holons, interactions, and levels defies simple visual representation.
Further, although the holarchy hypothesized here meets most of Wilber’s tenets,24 it is not clear that destroying lower holons would obliterate all of the holons above. It may be possible to provide abiding, transcendent health care without addressing all of the lower levels of care. A similar critique has been leveled against Maslow’s hierarchy of need,91,92 namely, that higher levels sometimes are possible without having achieved the lower levels.93 This limitation likely results from the coevolution of this holarchy with other related holons and hierarchies that are not depicted.
Thus, the holarchy of health care depicted here is a simplification of the true complexity of effective levels of health care. Recognizing these additional interactions, however, does not negate the simple usefulness of understanding that phenomena in health care and the natural world are both parts and wholes (holons), and that hierarchies of these holons (holarchies) can be recognized. Recognizing the interaction of these and other holons and holarchies can help explain surprises94,95 and reconcile silos of understanding that misrepresent the world in ways that block advancement. For example, Glass and McAtee recently have used systems concepts and their evolution to try to reconcile the fields of sociobehavioral science and public health.96 Others have called for both vertical and horizontal integration to achieve high-value health care.97–101
IMPLICATIONS
The holarchy presented here leads to a number of useful implications and hypotheses for understanding the nature of health care and for organizing and improving care.
Since the phenomena of health care and health are context dependent, it is helpful to understand their nature as holons—part/wholes that are simultaneously part of other wholes that coevolve over time.
Understanding the components of health care as related holons rather than isolated commodities can help us to develop systems that foster care which is more relationship centered, less fragmented, and of greater value.
Lower-level tasks, done faithfully over time, can build relationships that enable higher-level tasks.
Higher-level tasks in the holarchy provide an important frame and boundary for lower-level tasks. Lower-level tasks set the possibilities from which higher-order health care holons can emerge.65
Even within levels of the health care holarchy, integration is possible and desirable, eg, at the fundamental level, integrating mental health with other basic care rather than carving it out.
With most current crude quality assessment tools and information systems, we know how to measure only the fundamental holons of health care.102
Measuring and incentivizing only the lowest level of the holarchy may unintentionally disincentivize and block progression toward higher levels.
Even though the higher level tasks are less instrumental and therefore less easily specified, they could be enabled by systems and information technology (IT). For example, IT could prioritize prompts based on epidemiological data, thus using the fundamental care level to enable the integrated care level. IT could prioritize prompts based on information on patient preferences and societal costs or benefits, thus enabling the next level of prioritized care. IT could provide a mechanism for ongoing self-reflection about patients’ evolving preferences, thus moving from our current static approach to living wills to an evolutionary approach that better reflects the reality of how patient’s preferences work, and preventing us from getting locked into health care approaches that push technology in the final days of life way beyond what people want, and that drain our coffers with unwanted, unneeded, unhelpful, and sometimes cruel care that is done to people rather than provided in partnership with them.
Care organized to foster development along the holarchy may help to reframe health as more than the absence of disease,103 but as a foundation for achievement,104 and as relationships and the meaning derived from them.105,106
Primary care often is thought to be simple; however, the holarchy of health care reveals increasing complexity. Lower-order functions are the building blocks that develop the relationships necessary to accomplish higher-order functions. Lower-order functions relate to managing individual problems based on various kinds of evidence. Higher-order functions involve more sophisticated prioritizing, personalizing, integrating, and abiding.
Although current incentives and systems often obstruct development toward the higher levels in the holarchy of health care, high-quality primary care need not be limited to fundamental functions; with support it can incorporate the higher levels of integrating and prioritizing and thereby foster healing.
Knowing this holarchy can help in the design of flexible, personalized health care delivery systems that foster the most developed care necessary for a given situation while providing cost-effective simple care when appropriate.
Both specialist and generalist approaches are needed for effective health care. The broader scope of generalists can help focus the more narrowly construed work of specialists.
Ongoing care based on understanding and acting on this holarchical organization of health care is likely to lead to lower costs, less waste, greater personalization, greater effectiveness, and greater value in health care.
Understanding and acting on this holarchy may lead to less emphasis on health care and more emphasis on related holarchies of health and the social determinants of health107 that are not about the health care industry.
Understanding and acting on this holarchy is likely to lead to health care that involves greater caring, and serves as a force for greater personal development and interpersonal and societal solidarity.
JOIN THE EXCHANGE OF IDEAS
We invite readers from diverse fields to comment on and provide examples that challenge or support the concept of holons and the holarchical organization of physical, biological, and social systems. We encourage readers to consider and comment on the implications of this knowledge for understanding and improving health care and health. Please join the discussion at: http://www.AnnFamMed.org.
Acknowledgments
Paul Thomas and William Miller provided substantial input on earlier drafts of this manuscript. I regret that I was not able to fully incorporate their important ideas on this topic. Robin Gotler, Robert Phillips, Andrew Bazemore, Martey Dodoo, Frank deGruy, Larry Green also provided helpful comments.
Funding support: Dr Stange is supported in part by a Clinical Research Professorship from the American Cancer Society.
REFERENCES
- 1.Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7(2):100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stange KC. The generalist approach. Ann Fam Med. 2009;7(3): 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stange KC, Ferrer RL. The paradox of primary care. Ann Fam Med. 2009;7(4):293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koestler A, Smythies JR, eds. Beyond Reductionism: New Perspectives on the Life Sciences. Boston, MA: Houghton Mifflin Co; 1971.
- 5.Weiss PA. The living system: determinism stratified. In: Koestler A, Smythies JR, eds. Beyond Reductionism: New Perspectives on the Life Sciences. New York, NY: Beacon Press; 1969.
- 6.Koessler A. The Ghost in the Machine. New York, NY: The Macmillan Company; 1967.
- 7.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. [DOI] [PubMed] [Google Scholar]
- 8.Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137:535–544. [DOI] [PubMed] [Google Scholar]
- 9.Stacey RD. Complexity and Creativity in Organizations. San Francisco, CA: Berrett-Koehler Publishers; 1996.
- 10.Goldberger AL. Non-linear dynamics for clinicians: chaos theory, fractals, and complexity at the bedside. Lancet. 1996;347(9011): 1312–1314. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths F, Byrne D. General practice and the new science emerging from the theories of ’chaos’ and complexity. Br J Gen Pract. 1998;48(435):1697–1699. [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmerman B, Lindberg C, Plsek P. Edgeware: Insights From Complexity Science for Health Care Leaders. Irving, TX: VHA, Inc; 1998.
- 13.Miller WL, McDaniel RR, Jr, Crabtree BF, Stange KC. Practice jazz: Understanding variation in family practices using complexity science. J Fam Pract. 2001;50(10):872–878. [PubMed] [Google Scholar]
- 14.Sturmberg JP. Systems and complexity thinking in general practice. Part 2: application in primary care research. Aust Fam Physician. 2007;36(4):273–275. [PubMed] [Google Scholar]
- 15.Sweeney K, Griffiths F, eds. Complexity and Healthcare: An Introduction. Abingdon, UK: Radcliffe Medical Press; 2002.
- 16.Holt TA, ed. Complexity for Clinicians. San Francisco, CA: Radcliffe; 2004.
- 17.Borrell-Carrio F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med. 2004;2(6):576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berkes F, Colding J, Folke C. Navigating Social-Ecological Systems: Building Resilience for Complexity And Change. Cambridge, MA: Cambridge University Press; 2008.
- 19.Wilson T, Holt T, Greenhalgh T. Complexity science: complexity and clinical care. BMJ. 2001;323(7314):685–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plsek PE, Greenhalgh T. Complexity science: The challenge of complexity in health care. BMJ. 2001;323(7313):625–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sturmberg JP. Systems and complexity thinking in general practice: part 1—clinical application. Aust Fam Physician. 2007;36(4):170–173. [PubMed] [Google Scholar]
- 22.Wilber K. Sex, Ecology, Spirituality: The Spirit of Evolution. Boston, MA: Shambhala Publications; 1995.
- 23.Wilber K. The Integral Vision. Boston, MA: Shambhala Publications; 2007.
- 24.Wilber K. The pattern that connects. In: Sex, Ecology, Spirituality: The Spirit of Evolution. Boston, MA: Shambala Publications; 1995:40–85.
- 25.Like R, Zyzanski SJ. Patient requests in family practice: a focal point for clinical negotiations. Fam Pract. 1986;3(4):216–228. [DOI] [PubMed] [Google Scholar]
- 26.Cherry DK, Hing E, Woodwell DA, Rechsteiner EA. National Ambulatory Medical Care Survey: 2006 Summary. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed]
- 27.Stange KC, Zyzanski SJ, Jaén CR, et al. Illuminating the ’black box’. A description of 4454 patient visits to 138 family physicians. J Fam Pract. 1998;46(5):377–389. [PubMed] [Google Scholar]
- 28.Schneeweiss R, Cherkin DC, Hart LG, et al. Diagnosis clusters adapted for ICD-9-CM and ICH-2. J Fam Pract. 1986;22(1):69–72. [PubMed] [Google Scholar]
- 29.Schneeweiss R, Rosenblatt RA, Cherkin DC, Kirkwood CR, Hart G. Diagnosis clusters: a new tool for analyzing the content of ambulatory medical care. Med Care. 1983;21(1):105–122. [DOI] [PubMed] [Google Scholar]
- 30.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. [DOI] [PubMed] [Google Scholar]
- 31.Stange KC, Flocke SA, Goodwin MA. Opportunistic preventive services delivery. Are time limitations and patient satisfaction barriers? J Fam Pract. 1998;46(5):419–424. [PubMed] [Google Scholar]
- 32.Jaén CR, Crabtree BF, Zyzanski SJ, Goodwin MA, Stange KC. Making time for tobacco cessation counseling. J Fam Pract. 1998;46(5): 425–428. [PubMed] [Google Scholar]
- 33.Podl TR, Goodwin MA, Kikano GE, Stange KC. Direct observation of exercise counseling in community family practice. Am J Prev Med. 1999;17:207–210. [DOI] [PubMed] [Google Scholar]
- 34.Eaton CB, Goodwin MA, Stange KC. Direct observation of nutrition counseling in community family practice. Am J Prev Med. 2002;23:174–179. [DOI] [PubMed] [Google Scholar]
- 35.Flocke SA, Stange KC, Goodwin MA. Patient and visit characteristics associated with opportunistic preventive services delivery. J Fam Pract. 1998;47:202–208. [PubMed] [Google Scholar]
- 36.Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns. 2009;76:25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q. 2001;79:579–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 39.Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27:63–80. [DOI] [PubMed] [Google Scholar]
- 40.deGruy F. Mental health care in the primary care setting. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. Washington, DC: National Academy Press; 1996:285–311. [PubMed]
- 41.Nease DE, Jr., Aikens JE, Schwenk TL. Mental health disorders and their descriptive criteria in primary care: clarifying or confounding? Primary Care Companion J Clin Psychiatry. 2005;7:89–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care—making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006;189:484–493. [DOI] [PubMed] [Google Scholar]
- 43.Bower P, Rowland N. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database Syst Rev. 2006;3: CD001025. [DOI] [PubMed] [Google Scholar]
- 44.Harkness EF, Bower PJ. On-site mental health workers delivering psychological therapy and psychosocial interventions to patients in primary care: effects on the professional practice of primary care providers. Cochrane Database Sys. Rev. 2009;21(1):CD000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medalie JH. Family Medicine: Principles and Applications. Baltimore, MD: Williams & Wilkins; 1978.
- 46.Mainous AG, III, Goodwin MA, Stange KC. Patient-physician shared experiences and value patients place on continuity of care. Ann Fam Med. 2004;2(5):452–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nutting PA, Goodwin MA, Flocke SA, Zyzanski SJ, Stange KC. Continuity of primary care: to whom does it matter and when? Ann Fam Med. 2003;1(3):149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tinetti ME, Bogardus ST, Jr., Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Eng. J Med. 2004;351(27):2870–2874. [DOI] [PubMed] [Google Scholar]
- 50.Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3(3):223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Beasley JW, Hankey TH, Erickson R, et al. How many problems do family physicians manage at each encounter? A WReN study. Ann Fam Med. 2004;2(5):405–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Flocke SA, Frank SH, Wenger DA. Addressing multiple problems in the family practice office visit. J Fam Pract. 2001;50(30:211–216. [PubMed] [Google Scholar]
- 53.Fortin M, Dionne J, Pinho G, Gignac J, Almirall J, Lapointe L. Randomized controlled trials: do they have external validity for patients with multiple comorbidities? Ann Fam Med. 2006;4(2):104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nutting PA. Why can’t clinical policies be relevant to practice? J Fam Pract. 1997;44(4):350–352. [PubMed] [Google Scholar]
- 55.Schwenk TL. Competing priorities and comorbidities. So much to do and so little time. Arch Fam Med. 1997;6(3):238–239. [DOI] [PubMed] [Google Scholar]
- 56.Woolf SH, Stange KC. A sense of priorities for the health care commons. Am J Prev Med. 2006;31(1):99–102. [DOI] [PubMed] [Google Scholar]
- 57.Stange KC. The paradox of the parts and the whole in understanding and improving general practice. Int J Qual Health Care. 2002;14(4):267–268. [DOI] [PubMed] [Google Scholar]
- 58.Stange KC, Jaén CR, Flocke SA, Miller WL, Crabtree BF, Zyzanski SJ. The value of a family physician. J Fam Pract. 1998;46(5):363–368. [PubMed] [Google Scholar]
- 59.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31(1):52–61. [DOI] [PubMed] [Google Scholar]
- 60.Starfield B. Primary care and health: A cross-national comparison. JAMA. 1991;266(16):2268–2271. [PubMed] [Google Scholar]
- 61.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baicker K, Chandra A. Medicare spending, the physician work-force, and beneficiaries’ quality of care. Health Aff (Millwood). 2004;Suppl Web Exclusives:W184–W197. [DOI] [PubMed]
- 63.Greenfield S, Nelson EC, Zubkoff M, et al. Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992;267(12):1624–1630. [PubMed] [Google Scholar]
- 64.Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin-dependent diabetes mellitus treated by different systems and specialties: results from the medical outcomes study. JAMA. 1995;274(18):1436–1444. [PubMed] [Google Scholar]
- 65.Franks P, Clancy CM, Nutting PA. Gatekeeping revisited—protecting patients from overtreatment. N Engl J Med. 1992;327(6):424–429. [DOI] [PubMed] [Google Scholar]
- 66.Flocke SA, Goodwin MA, Stange KC. The effect of a secondary patient on the family practice visit. J Fam Pract. 1998;46(5):429–434. [PubMed] [Google Scholar]
- 67.Orzano AJ, Gregory PM, Nutting PA, Werner JJ, Flocke SA, Stange KC. Care of the secondary patient in family practice. A report from the Ambulatory Sentinel Practice Network. J Fam Pract. 2001;50(2):113–116. [PubMed] [Google Scholar]
- 68.Hoffman A, Pearson SD. ‘Marginal medicine’: targeting comparative effectiveness research to reduce waste. Health Aff (Millwood). 2009;28(4):w710–w718. [DOI] [PubMed] [Google Scholar]
- 69.Gunn J, Naccarella L, Palmer V, Kokanovic R, Pope C, Lathlean J. What is the Place of Generalism in the 2020 Primary health care team? Australian Primary Health Care Research Institute. 2008. http://www.anu.edu.au/aphcri/Domain/Workforce/Perkins_25_final.pdf. Accessed Jan 12, 2009.
- 70.Heath I, Sweeney K. Medical generalists: connecting the map and the territory. BMJ. 2005;331(7530):1462–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Weiner SJ. Contextualizing medical decisions to individualize care: lessons from the qualitative sciences. J Gen Intern Med. 2004; 19(3):281–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. Rev ed. New York, NY: Oxford University Press; 1998.
- 73.Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care: America’s Health in a New Era. Washington, DC: National Academy Press; 1996. [PubMed]
- 74.Egnew TR. The meaning of healing: transcending suffering. Ann Fam Med. 2005;3(3):255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Egnew TR. Suffering, meaning, and healing: challenges of contemporary medicine. Ann Fam Med. 2009;7(2):170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Scott JG, Cohen D, Dicicco-Bloom B, Miller WL, Stange KC, Crab-tree BF. Understanding healing relationships in primary care. Ann Fam Med. 2008;6(4):315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Farber SJ, Egnew TR, Herman-Bertsch JL. Defining effective clinician roles in end-of-life care. J Fam Pract. 2002;51(2):153–158. [PubMed] [Google Scholar]
- 78.Scitovsky AA. “The high cost of dying”: what do the data show? 1984. Milbank Q. 2005;83(4):825–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. [DOI] [PubMed] [Google Scholar]
- 80.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273–287. [DOI] [PubMed] [Google Scholar]
- 81.Epstein RM, Fiscella K, Lesser C, Stange KC. Defining and achieving patient-centered care: the role of clinicians, patients and healthcare systems. Health Aff (Millwood). In press.
- 82.McCullough LB. The physician’s virtues and legitimate self-interest in the patient-physician contract. Mt Sinai J Med. 1993; 60(1):11–14. [PubMed] [Google Scholar]
- 83.Sox HC; ABIM Foundation. American Board of Internal Medicine; ACP-ASIM Foundation. American College of Physicians-American Society of Internal Medicine; European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136(3):243–246. [DOI] [PubMed] [Google Scholar]
- 84.Sandy LG, Schroeder SA. Primary care in a new era: disillusion and dissolution? Ann Intern Med. 2003;138(3):262–267. [DOI] [PubMed] [Google Scholar]
- 85.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Davis K. Paying for care episodes and care coordination. N Engl J Med. 2007;356(11):1166–1168. [DOI] [PubMed] [Google Scholar]
- 87.Starfield B, Shi LY, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB, Weiner JP. Comorbidity: implications for the importance of primary care in ‘case’ management. Ann Fam Med. 2003;1(1):8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Starfield B, Lemke KW, Herbert R, Pavlovich WD, Anderson G. Comorbidity and the use of primary care and specialist care in the elderly. Ann Fam Med. 2005;3(3):215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations’ health: assessing the evidence. Health Aff (Millwood). 2005;(Suppl Web Exclusives):W5-97–W95-107. [DOI] [PubMed]
- 91.Maslow A, ed. Motivation and Personality. New York, NY: Harper; 1954.
- 92.Maslow A. The Farther Reaches of Human Nature. New York, NY: Viking Press; 1971.
- 93.Wahba A, Bridgewell L. Maslow reconsidered: A review of research on the need hierarchy theory. Organ Behav Hum Perform. 1976;14:212–240. [Google Scholar]
- 94.McDaniel RR Jr, Jordan ME, Fleeman BF. Surprise, Surprise, Surprise! A complexity science view of the unexpected. Health Care Manage Rev. 2003;28(3):266–278. [DOI] [PubMed] [Google Scholar]
- 95.Crabtree BF. Primary care practices are full of surprises! Health Care Manage Rev. 2003;28(3):279–283, discussion 289–290. [DOI] [PubMed] [Google Scholar]
- 96.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650–1671. [DOI] [PubMed] [Google Scholar]
- 97.Van der Geest S, Speckmann JD, Streefland PH. Primary health care in a multi-level perspective: towards a research agenda. Soc Sci Med. 1990;30(9):1025–1034. [DOI] [PubMed] [Google Scholar]
- 98.De Maeseneer J, van Weel C, Egilman D, Mfenyana K, Kaufman A, Sewankambo N. Strengthening primary care: addressing the disparity between vertical and horizontal investment. Br J Gen Pract. 2008;58(546):3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stange KC. Polyclinics must integrate health care vertically AND horizontally. Lond J Prim Care. 2008;1:42–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thomas P, Meads G, Moustafa A, Nazareth I, Stange KC. Combined vertical and horizontal integration of health care—a goal of practice based commissioning. Qual Prim Care. 2008;16(6):425–432. [PubMed] [Google Scholar]
- 101.Lawn JE, Rohde J, Rifkin S, Were M, Paul VK, Chopra M. Alma-Ata 30 years on: revolutionary, relevant, and time to revitalise. Lancet. 2008;372(9642):917–927. [DOI] [PubMed] [Google Scholar]
- 102.Stange KC, Nutting PA, Miller WL, et al. Definging and measuring the patient-centered medical home. J Gen Intern Med. In press. [DOI] [PMC free article] [PubMed]
- 103.Declaration of Alma-Ata. International conference on primary health care, Alma-Ata, USSR, 6–12 September 1978. 1978. http://www.who.int/hpr/NPH/docs/declaration_almaata.pdf, Accessed Sept 26, 2008.
- 104.Seedhouse D. Health: The Foundations for Achievement. 2nd ed. New York, NY: Wiley; 2001.
- 105.Berry W. Life Is a Miracle: An Essay Against Modern Superstition. Washington, DC: Counterpoint; 2000.
- 106.Fine M, Peters JW. The Nature of Health: How America Lost, and Can Regain, A Basic Human Value. Abingdon, Oxfordshire: Radcliffe Publishing Limited; 2007.
- 107.World Health Organization. Commission on Social Determinants of Health—Final Report. 2008. http://www.who.int/social_determinants/final_report/en/index.html. Accessed January 30, 2009.