Abstract
Transcutaneous electrical nerve stimulation (TENS) is a commonly utilized non-pharmacological, non-invasive treatment for pain. GABA is a neurotransmitter in the dorsal horn of the spinal cord that mediates analgesia locally, and also through activation of supraspinal sites. TENS reduces hyperalgesia through activation of receptor-mediated pathways at the level of the spinal cord, and supraspinally. The current study tested the hypothesis that either high or low frequency TENS applied to the inflamed knee joint increases GABA in the spinal cord dorsal horn and activates GABA receptors spinally. We utilized microdialysis to sample the extracellular fluid before, during and after TENS and analyzed GABA in dialysates with high performance liquid chromatography. We analyzed the extracellular GABA concentrations in animals with and without knee joint inflammation induced by intra-articular injection of kaolin and carrageenan. We further tested if spinal blockade of GABA receptors prevents the antihyperalgesia produced by TENS in rats with joint inflammation. We show that high frequency TENS increases extracellular GABA concentrations in the spinal cord in animals with and without joint inflammation. The increases in GABA do not occur in response to low frequency TENS, and there are no increases in glycine in response to low or high frequency TENS. However, the reduction in primary hyperalgesia by both high and low frequency TENS is prevented by spinal blockade of GABAA receptors with bicuculline. Thus, high frequency TENS increases release of GABA in the deep dorsal horn of the spinal cord, and both high and low frequency TENS reduce primary hyperalgesia by activation of GABAA receptors spinally.
Keywords: Pain, Electrical stimulation, Microdialysis, Bicuculline, Hyperalgesia
1. Introduction
Transcutaneous electrical nerve stimulation (TENS) is the application of surface electrodes to the skin for pain relief. Clinically, TENS is applied at varying frequencies of stimulation, high (>50 Hz) or low (<10 Hz). Previously, we show different mechanisms of action for the ability of low and high frequency TENS to reduce hyperalgesia. Specifically, low frequency TENS activates mu-opioid, serotonin, and cholinergic receptors in the spinal cord and mu-opioid receptors supraspinally (Sluka et al., 1999; Kalra et al., 2001; Radhakrishnan and Sluka, 2003; Radhakrishnan et al., 2003). On the other hand, antihyperalgesia produced by high frequency TENS activates delta-opioid receptors and cholinergic receptors spinally, and delta-opioid receptors suprapspinally (Sluka et al., 1999; Kalra et al., 2001; Radhakrishnan and Sluka, 2003; Radhakrishnan et al., 2003).
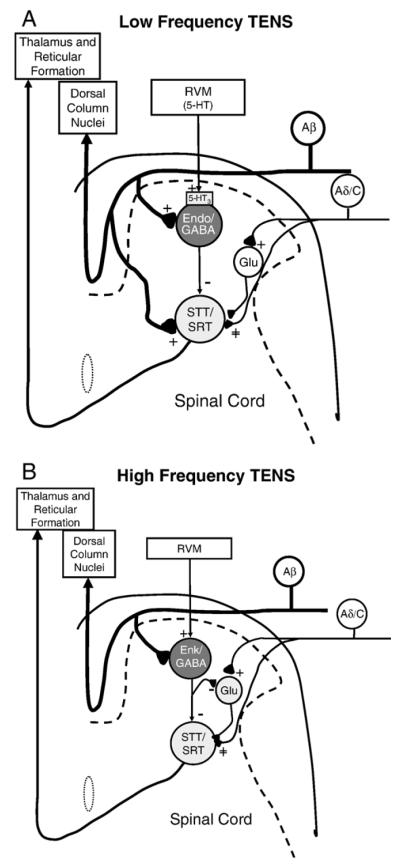
Activation of descending inhibitory pathways from the periaqueductal gray relays through the RVM and utilizes opioids to produce analgesia (see Fields and Basbaum, 1999). Stimulation of the PAG inhibits spinothalamic tract cells through activation of GABAA receptors in the spinal cord (Lin et al., 1994). Supraspinal activation of mu-opioid receptors increases release of GABA in the spinal cord that is prevented by 5-HT3 receptor antagonists (Kawamata et al., 2002). Indeed, dorsal column stimulation at high frequency (100 Hz), which would activate large diameter sensory afferents like TENS, also increases spinal release of GABA in normal animals and those with nerve injury (Linderoth et al., 1994; Stiller et al., 1996), and reduces glutamate release through activation of GABAB receptors (Cui et al., 1997). These data suggest that analgesia mediated by supraspinal μ-opioid receptors releases serotonin in the spinal cord that in turn activates 5-HT3 receptors on GABAergic neurons resulting in release of GABA. We suggest a similar pattern for effects of low frequency TENS: supraspinal μ-opioid receptors releases serotonin in the spinal cord that in turn activates 5-HT3 receptors on GABAergic neurons resulting in release of GABA that subsequently decreases activity of dorsal horn neurons (Fig. 1A). We suggest that high frequency TENS activates supraspinal delta-opioid receptors that releases GABA and enkephalins in the spinal cord resulting in decreased release of glutamate and decreased activity of dorsal horn neurons (Fig. 1B). We are therefore testing the hypothesis that either high or low frequency TENS applied to the inflamed knee joint increases GABA in the spinal cord dorsal horn and activates GABA receptors spinally. The hypothesis will be tested by 1) using in vivo microdialysis of the dorsal horn to examine the time course of neurotransmitter release in response to TENS and 2) using behavioral tests to examine if blockade of GABAA receptors spinally prevents the antihyperalgesia produced by TENS.
Fig. 1.
Schematic diagram representing potential pathways involved in low (A) or high (B) frequency TENS antihyperalgesia. RVM=rostra ventral medulla; Endo=endomorphin-2; Glu=glutamate; STT=spinothalamic tract; SRT=spinoreticular path; 5-HT=serotonin.
2. Results
2.1. GABA
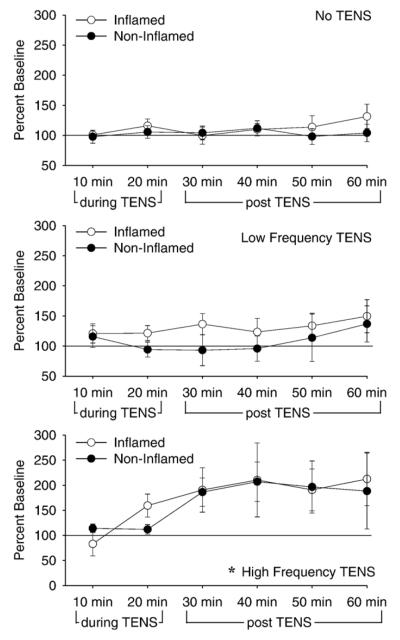
Baseline concentrations for GABA in the spinal cord were 2.9 pg/ml ± 0.3 (mean ± S.E.M.). GABA concentrations increased in the dorsal horn of the spinal cord in the sample beginning after the termination of high frequency TENS but not during application of high frequency TENS. For the changes in GABA concentrations there was a significant effect for time (F5,115 =4.6, p=0.001, repeated ANOVA) and for frequency (F2,23=4.1, p=0.03, repeated ANOVA). The high frequency TENS group was significantly higher than the no TENS group (p=0.02; Tukey’s post hoc) (Fig. 2). However, there was no significant difference between the inflamed and the non-inflamed groups with similar increases in GABA occurring in response to high frequency TENS for both the inflamed and the non-inflamed groups. For analysis of the area under the curve, there was an overall effect for time for the period after TENS (F5,41=4.3, p=0.03), but not during TENS with increases in concentrations of GABA in the group treated with high frequency TENS (p=0.01) when compared to the animals that did not receive TENS (Fig. 3).
Fig. 2.
Time course of changes in extracellular concentrations of GABA during (10–20 min) and after (30–60 min) treatment with low frequency (middle panel), high frequency (bottom panel), or no TENS (top panel) for animals with (open circles) and without (closed circles) knee joint inflammation. Increases in GABA in the extracellular fluid were delayed beginning immediately after removal of TENS and continuing through 60 min. The increases were similar between the group with joint inflammation and the group without joint inflammation. No changes in GABA were observed in the group that received low frequency TENS, or the group that did not receive TENS. Data are expressed as a percent of baseline with baseline set at 100% as the mean±S.E.M. *, P <0.05, significantly different than no TENS.
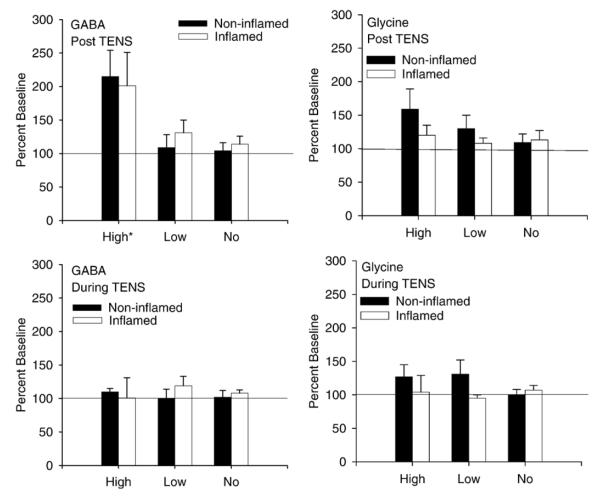
Fig. 3.
Summary of the responses during and after TENS for changes in GABA and glycine. The average increase after treatment with high frequency TENS was signicantly greater than the group that did not receive TENS or the group that received low frequency TENS. There was no change in GABA during TENS, and no change in glycine either during or after TENS. Data are the mean±S.E.M. *, P <0.05.
2.2. Glycine
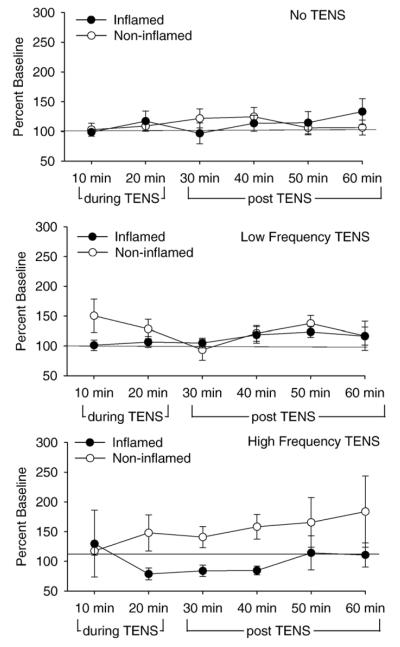
Baseline concentrations for glycine in the spinal cord were 46.8±2.4 pg/ml. No significant differences in glycine either during or after treatment with either high or low frequency TENS, in inflamed or non-inflamed animals (Figs. 3 and 4).
Fig. 4.
Extracellular concentrations for glycine during and after high frequency (bottom panel), low frequency (middle panel) or no TENS (top panel) treatment in animals with (closed circles) and without (open symbols) inflammation. No changes in glycine were observed in the group that received low frequency TENS, high frequency TENS or the group that did not receive TENS. Data are expressed as a percent of baseline with baseline set at 100% as the mean±S.E.M.
2.3. Primary hyperalgesia
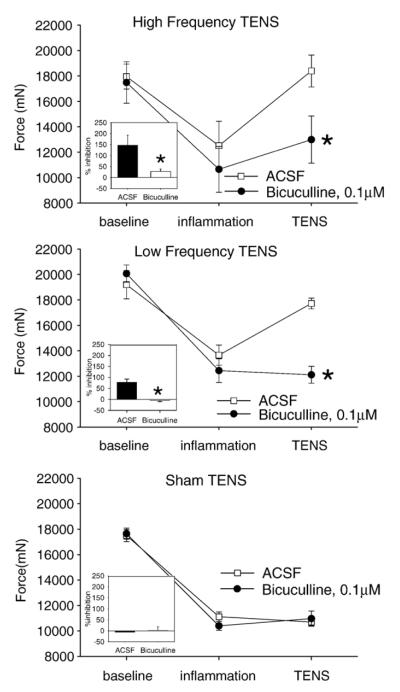
Induction of knee joint inflammation reduced the compression withdrawal threshold of the knee on the side of inflammation 24 h later. Application of high (p=0.001) or low (p=0.004) frequency TENS, with ACSF infusion, increased the compression withdrawal threshold of the knee joint when compared to ACSF infusion with sham TENS (Fig. 5). Pretreatment with bicuculline prior to either high or low frequency TENS significantly prevented the reduction in hyperalgesia by both high and low frequency TENS (F10,42=7.8, p=0.0001, time*group effect). Post hoc testing showed that the high frequency TENS+bicuculline group was significantly less than the high frequency TENS+ACSF group (p=0.02; Tukey’s test) and the low frequency+bicuculline group less than the low frequency+ACSF group (p=0.03, Tukey’s test). The sham TENS+ACSF group was not different with the sham TENS+bicuculline group. The percent inhibition by TENS was also significantly different between groups (F5,26=7.1, p=0.001, one-way ANOVA) with the high frequency+bicuculline group less than the high frequency+ACSF group (p=0.01; Tukey’s test) and the low frequency+bicuculline group less than the low frequency+ACSF group (p=0.03, Tukey’s test). There was no difference between the rats treated with ACSF and sham TENS when compared to ACSF and bicuculline. There were no changes for the compression withdrawal threshold of the contralateral hindlimb after inflammation, or after TENS with ACSF or TENS with bicuculline.
Fig. 5.
Graphs represent the compression withdrawal threshold for groups of rats that received high frequency TENS or low frequency TENS with ACSF (open squares) or with bicuculline (closed circles). Twenty-four hours after inflammation there was a decrease in the compression withdrawal threshold when compared to baseline. In the groups treated with ACSF as a control, TENS increased the compression withdrawal threshold back toward baseline. In contrast the groups treated with bicuculline TENS did not increase the compression withdrawal threshold. The insets show the percent inhibition of hyperalgesia such that 0% is no change, 100% is complete reversal, and >100% is analgesia. *, P <0.05, significantly different from ACSF group.
3. Discussion
3.1. GABA and high frequency TENS
The current study shows that high frequency TENS increases extracellular concentrations of GABA in the L3/L4 spinal segments, and these increases in extracellular concentration of GABA begin after removal from the stimulus. The current study also shows that blockade of GABAA receptors in the spinal cord prevents the antihyperalgesia produced by high frequency TENS. Similarly, prior studies show increased extracellular concentrations of GABA in the spinal cord during dorsal column stimulation, at high frequency, also begins after removal of the stimulation and utilizes GABA receptors in the spinal cord to produce analgesia (Linderoth et al., 1994; Stiller et al., 1996). Dorsal column stimulation, delivered at sensory intensity and high frequency, would activate large diameter afferent fibers similar to TENS delivered at sensory intensity and high frequency (Radhakrishnan and Sluka, 2005). Thus, high frequency stimulation at intensities that activate large diameter afferents results in increases in GABA in the spinal cord dorsal horn.
The time course of changes in extracellular GABA differs from that observed in prior studies examining the release of neurotransmitters and TENS (Sluka et al., 2005, 2006). For high frequency TENS, decreases in glutamate occur during TENS and return to baseline concentrations after removal of TENS (Sluka et al., 2005). Further the inhibition of extracellular glutamate by TENS only occurs in animals with joint inflammation, and not those without (Sluka et al., 2005). Since GABA increases are delayed in relation to the time of stimulation in the current study, GABA is likely not increased in direct response to the stimulation, but rather indirectly as a result of other long-lasting neurotransmitter and/or cellular mechanisms.
The current study also shows equivalent increases in extracellular GABA during high frequency TENS in animals with and without joint inflammation that begins after removal of TENS. It is thus, unlikely that the increases in GABA are responsible for the decreases in glutamate by high frequency TENS observed in a prior study (Sluka et al., 2005). Further, we show that the decreases in glutamate are prevented by prior treatment with naltrindole, a delta-opioid receptor antagonist, suggesting that endogenous opioid release mediates the decreases in glutamate (Sluka et al., 2005). We hypothesize that the increases in extracellular GABA are a parallel, spinal inhibitory system that enhances the antihyperalgesia produced by TENS. In support, early work shows that spinal transection reduces, but does not eliminate, the analgesic effects of TENS in animals without tissue injury (Woolf et al., 1980). Approximately 50% of the analgesic effect of high frequency TENS remains after spinal transection. The delayed increases in extracellular GABA in the spinal cord in response to TENS parallel the timing of TENS antihyperalgesia testing in prior studies (Sluka et al., 1998). In addition to antihyperalgesia occurring after removal of TENS, inhibition of dorsal horn neuron sensitization also continues after removal of TENS (Ma and Sluka, 2001). Thus, delayed increases in GABA follow the time course of effectiveness of high frequency TENS for reduction in hyperalgesia and thus likely represent one mechanism by which TENS reduces pain.
3.2. GABA and low frequency TENS
In the current study we show that low frequency TENS, unlike the results with high frequency TENS, had no effect on extracellular GABA concentrations in the L3/L4 dorsal horn of the spinal cord, which does not support our initial hypothesis. However, in the current study, blockade of GABAA receptors in the spinal cord reduced the antihyperalgesia produced by low and high frequency TENS, supporting our initial hypothesis. One explanation for this discrepancy between release and behavior data for low frequency TENS could be that there was an increase in GABA extracellularly in animals with joint inflammation in other spinal segments such as the L5 or L6 segments. Alternatively, increases in GABA could occur in the superficial dorsal horn that we were unable to measure in the deep dorsal horn by microdialysis. Bicuculline, delivered by microdialysis, is expected to diffuse at least 2–4 mm in the rostrocaudal direction and dorsoventral directions. Thus, while sampling the extracellular environment is restricted to the area surrounding the microdialysis fiber, drug delivery would encompass multiple spinal sections and the superficial dorsal horn. Further the release studies were performed while the rat was anesthetized with sodium pentobarbital. The behavioral studies, on the other hand, were performed with the animal awake except for the short duration when TENS was applied under light halothane anesthesia (1–2%). Thus, the effects of blockade of GABA receptors spinally during low frequency TENS could be to reduce the binding to GABAA receptors in the L5/L6 spinal cord and/or superficial dorsal horn, or related to use of anesthetic during collection.
Prior studies support a role for GABA in analgesia that involves suprspinal stimulation and serotonin. Specifically, these prior data show 1) electrical stimulation of supraspinal sites (PAG) decreases dorsal horn neuron activity through activation of GABA receptors (Lin et al., 1994; Peng et al., 1996; Lin et al., 1996a), 2) the analgesia and reduction in dorsal horn neuron activity as a result of stimulation of supraspinal sites (PAG and RVM) utilizes serotonin (Lin et al., 1996b; Cui et al., 1999; Hammond et al., 1985, 1998; Sorkin et al., 1993; Bowker and Abhold, 1990), 3) activation of 5-HT3 receptors in the spinal cord increases the release of GABA in the spinal cord (Kawamata et al., 2002), and 4) low frequency TENS increases release of serotonin and activates 5-HT2 and 5-HT3 receptors in the spinal cord (Sluka et al., 2006; Radhakrishnan et al., 2003).
3.3. Neurotransmitter mechanisms of TENS
The differential changes in extracellular GABA concentrations in response to low and high frequency TENS has been shown previously for other neurotransmitters and receptors (Sluka et al., 1999; Kalra et al., 2001; Radhakrishnan et al., 2003; Sluka et al., 2005, 2006). Specifically, in the spinal cord serotonin is increased in response to low frequency TENS, but not high frequency TENS. The reduction in hyperalgesia by low frequency TENS is prevented by spinal blockade of mu-opioid, or 5-HT2 and 5-HT3 receptors, and supraspinal blockade of mu-opioid receptors. Spinal blockade of delta-opioid or serotonin receptors has no effect on the reduction in hyperalgeisa by high frequency TENS. In contrast, for high frequency TENS we previously show that there is a reduction in glutamate release in the spinal cord, and the antihyperalgesia is prevented by spinal or supraspinal blockade of delta-opioid receptors, but not mu-opioid receptors. Thus, different frequencies of stimulation produce antihyperalgesia through distinct mechanisms in the spinal dorsal horn and supraspinal pathways.
3.4. Extracellular GABA release mechanisms
The increased extracellular concentrations of GABA that occur in response to TENS could be a result of increased neuronal release, decreased reuptake, and/or increased glial release (see del Arco et al., 2003; Timmerman and Westerink, 1997). Basal concentrations of GABA likely reflect metabolic or glial release since these basal concentrations are independent of calcium mechanisms and tetrototoxin-insensitive (Timmerman and Westerink, 1997). However, increased extracellular concentrations evoked by peripherally applied electrical stimulation are less clear. Traditionally, it was thought that extracellular GABA was supplied by spillover from the synaptic cleft. However, GABAergic synapses are surrounded a large number of high and low affinity transporters in both neurons and glia. These GABA transporters tightly regulate GABA and blockade of these transporters increases extracellular GABA as measured by microdialysis (Schousboe, 2003). Further, glia can release GABA into the extracellular fluid, and increases in GABA concentrations extracellularly are likely to effect both neurons and glia though receptors located on astrocytes and extrasynaptically on neurons (Sykova, 2004). This general increase in GABA in the extracellular fluid has been hypothesized to modulate neuronal excitability and gene expression by modifying membrane potential and intracellular cascades through extrasynaptic receptors (del Arco et al., 2003).
4. Summary
In summary, increases in extracellular GABA in the L3/L4 spinal cord occur in response to high frequency TENS, but not low frequency TENS. The increases in extracellular GABA occur in both the inflamed and the non-inflamed animals. These increases in GABA are delayed in onset with respect to the time of application of TENS, and parallel the time in which antihyperalgesia occurs in response to TENS. In parallel, blockade of GABAA in the spinal cord reduced the antihyperalgesia produced by both low and high frequency TENS. Thus, these data suggest that increased spinal release of GABA activates GABAA receptors in the spinal cord to reduce hyperalgesia.
5. Experimental procedures
All experiments were approved by the Animal Care and Use Committee at the University of Iowa. A total of 69 male Sprague—Dawley rats (Harlan, St. Louis, MO, 250–350 g) were used for this study.
5.1. Injection of kaolin and carrageenan into the knee joint
Male Sprague—Dawley rats were injected with a mixture of 3% kaolin and 3% carrageenan (0.1 ml in sterile saline, pH 7.2–7.4) into the knee joint while the rat was anesthetized with halothane, 2–5% (Sluka and Westlund, 1993). For release of neurotransmitters knee joints were injected bilaterally since the microdialysis fiber encompasses both dorsal horns. For the behavioral studies, one knee joint was injected.
5.2. Measurement of compression withdrawal threshold of the knee
The compression withdrawal threshold of the knee was measured as previously described (Skyba et al., 2005). Rats were acclimated to the restraining device for 5 min 3 times per day for 2 consecutive days. On the day of testing, the experimenter extended one hind limb and the knee joint was compressed using measuring device. The measuring device consists of two strain gauges attached to the inner arm of a forceps. Compression was stopped when the animal withdrew the limb forcefully or when the animal vocalized. The maximum force applied at withdrawal was recorded as the threshold in grams as an average of 3 trials for each time period. A reduction in withdrawal threshold of the knee is interpreted as primary hyperalgesia.
5.3. Application of TENS
TENS was applied to the inflamed knee(s) for 20 min while the rat was anesthetized with 1–2% halothane (Sluka et al., 1999). Electrodes were placed on the medial and lateral aspects of the joint and high frequency (100 Hz), low frequency (4 Hz), or placebo TENS was applied. All other parameters were kept constant as follows: pulse width, 100 μs; amplitude/intensity, sensory level (just below motor contraction). Previously we demonstrated that reduction of secondary mechanical or heat hyperalgesia was equivalent with high or low frequency TENS at sensory intensity (Sluka et al., 1999; King and Sluka, 2001).
The TENS units used in these studies are utilized clinically (EMPI Eclipse+). The waveform is a balanced asymmetrical biphasic square wave. Amplitude is adjustable from 0–60 mA; pulse width is adjustable from 30 to 250 μs; pulse rate (frequency) is adjustable from 2–125 Hz. Electrodes are 0.5″ diameter round pregelled and used clinically for TENS treatment (of small areas such as the hand/fingers). The size of electrodes used in these experiments compares to the area of tissue that would be covered by electrodes in human subjects receiving TENS to the knee joint.
5.4. Placement of microdialysis fibers
Microdialysis fibers (200 μm o.d., Hospal Filtral AN69) were covered with epoxy except for a 2 mm gap (Sluka and Westlund, 1992) and placed the day before the experiment while the rat was anesthetized with halothane (2–4%). Specifically, the T13 vertebra was cleared of muscle and small holes drilled into the lateral aspect on each side to expose a small portion of the spinal cord. Microdialysis fibers were inserted transversely across the dorsal horn of the spinal cord through the two holes and then fixed to the bone with dental cement. The free ends of the microdialysis fiber were inserted into PE20 tubing and the connection secured with epoxy. The incision was sutured closed and animals recovered for 24 h.
5.5. Analysis of glycine and GABA
Samples from microdialysis experiments were analyzed for glycine and GABA using fluorescent detection after derivitization with o-phthaldialdehyde (OPT; Sigma)(Zahn et al., 2002)4. All samples were stored at −70 °C until analysis. Aliquots of 20 μl of the sample were diluted with 160 μl ACSF, and 20 μl 10 ng/ml of the internal standard homoserine. Samples underwent pre-column derivitization with OPT and injection with an auto-injector. A Supelcosil LC-18 HPLC column (5 μmparticle diameter, 4.6 mm i.d., 15 cm long) and a mobile phase composed of 17% methanol and 0.05 M sodium acetate was used with a pumping rate of 1.0 ml/min. The fluorescence detector was set at 330 nm for excitation and 420 nm for emission. Standards were dispersed through the run so that there were 3 standards at the beginning of the run, one standard every 5 samples, and two standards at the end of the run. The limit of detection for glycine is 0.25 ng/ml, the limit of quantification is 0.77 pg/ml, and precision is 4%. The limit of detection for GABA is 0.01 ng/ml, the limit of quantification is 0.02 ng/ml and precision is 4%. Peak areas were first normalized to the internal standard homoserine and concentrations calculated based on normalized peak areas with external standards run simultaneously. With the current techniques glycine and GABA are well above the levels of detection for samples collected from the spinal cord.
5.6. Experimental protocol
5.6.1. Microdialysis
The day after placement of the microdialysis fiber, rats were anesthetized with sodium pentobarbital (50 mg/kg, i.p.). An intravenous line was inserted to maintain anesthesia throughout the sampling period with sodium pentobarbital (2–4 mg/kg/h, i.v.). TENS electrodes were placed on the knee joint prior to collection of samples. Artificial cerebrospinal fluid (ACSF) was infused through the microdialysis fiber at 5 μl/min. All samples were collected on ice, immediately frozen on dry ice, and stored at −70 °C until analysis. After 1 h of washout, 4, 10 min baseline samples were collected. TENS was then applied for 20 min to the knee joint and 2, 10 min samples collected during TENS treatment. TENS was then stopped and 4, 10 min samples collected.
Animals were divided into the following groups as follows: 1) Inflammation, no TENS (n=6); 2) Inflammation, high frequency TENS (n=4); 3) Inflammation, low frequency TENS (n=10); 4) Normal, no TENS (n=7); 5) Normal, high frequency TENS (n=9); 6) Normal, low frequency TENS (n=6). At the end of the experiment, rats were euthanized with an overdose of sodium pentobarbital, the spinal cord removed, fixed in 10% formalin and analyzed for microdialysis fiber placement. Fifteen animals were removed from the study due to placement in L5 or L6 spinal segments. The animals included in this manuscript had microdialysis fibers were placed in the L3/L4 spinal segments and the deep dorsal horn (laminae III—VI).
5.6.2. Behavior
Prior to placement of microdialysis fibers the compression withdrawal threshold of the knee was measured (baseline, pre-inflammation). After baseline testing one knee joint was injected with a mixture of 3% kaolin and 3% carrageenan under halothane anesthesia (4%) and the rats were returned to their cage. After 2–3 h, the rats were re-anesthetized with halothane (2–4%) and a microdialysis fiber was placed in lumbar enlargement of the spinal cord at the level of the T13 vertebra.
The next day, the compression withdrawal threshold of the knee was assessed after inflammation to ensure development of hyperalgesia (post-inflammation). Rats were then randomly divided into the following groups as follows: 1) ACSF (n=5)+high frequency TENS, 2) bicuculline+high frequency TENS (n=5), 3) ACSF+low frequency TENS (n=4), 4) bicuculline+low frequency TENS (n=4), 5) ACSF+sham TENS (n=4) and 6) bicuculline+sham TENS (n=5). Preliminary experiments in an additional four animals determined that 1 h infusion of 0.1 mM bicuculline blocked the analgesic effects of the GABA agonist muscimol, and thus we utilized 0.1 mM bicuculline to block GABAA receptors in the spinal cord.
ACSF or 0.1 mM bicuculline was infused with the animal awake for 30 min. The rats were then lightly anesthetized with 1–2% halothane and TENS was applied to the inflamed knee joint for 20 min. ACSF or bicuculline was infused throughout the application of TENS for a total infusion time of approximately 1 h. Approximately 10–15 min after application of TENS and recovery from anesthesia the compression withdrawal threshold of the knee joint was re-assessed. Total testing time was 10–15 min. Rats were euthanized and the spinal cord was removed to confirm placement of microdialysis fibers in the lumbar enlargement.
5.7. Statistical analysis
For GABA and glycine data was converted to a percent of baseline. Data were analyzed with a repeated measures ANOVA for time and frequency of stimulation. The area under the curve for the GABA and glycine release data was analyzed for the period during the application of TENS, and for the time period after application of TENS. A one-way ANOVA compared differences between groups. Post hoc testing was done with Tukey’s test. For behavioral experiments, data was analyzed with a repeated measures ANOVA for time and for group. Post hoc testing with a Tukey’s test compared differences between groups. Behavioral data were also converted to a percent of baseline so that 100% inhibition resulted in a full reversal of hyperalgesia, 0% inhibition was no change in hyperalgesia, and >100% was analgesic. Analysis with a one-way ANOVA compared differences between groups.
Acknowledgments
Funded by the Arthritis Foundation, National Institutes of Health K0202201.
REFERENCES
- Bowker RM, Abhold RH. Evoked changes in 5-hydroxytryptamine and norepinephrine release: in vivo dialysis of the rat dorsal horn. Eur. J. Pharmacol. 1990;175:101–106. doi: 10.1016/0014-2999(90)90159-4. [DOI] [PubMed] [Google Scholar]
- Cui J-G, O’Connor WT, Ungerstedt U, Linderoth B, Meyerson BA. Spinal cord stimulation attenuates augmented dorsal horn release of excitatory amino acids in mononeuropathy via a GABAergic mechanism. Pain. 1997;73:87–95. doi: 10.1016/s0304-3959(97)00077-8. [DOI] [PubMed] [Google Scholar]
- Cui M, Feng Y, McAdo DJ, Willis WD. Periaqueductal gray stimulation-induced inhibition of nociceptive dorsal horn neurons in rats is associated with the release of norepinephrine, serotonin, and amino acids. J. Pharmacol. Exp. Ther. 1999;289:868–876. [PubMed] [Google Scholar]
- del Arco A, Segovia G, Fuxe K, Mora F. Changes in dialysate concentrations of glutamate and GABA in the brain: an index of volume transmission mediated actions? J. Neurochem. 2003;85:23–33. doi: 10.1046/j.1471-4159.2003.01692.x. [DOI] [PubMed] [Google Scholar]
- Fields HL, Basbaum AI. Central nervous system mechanisms of pain modulation. In: Wall PD, Melzack R, editors. Textbook of Pain. Churchill Livingstone; New York: 1999. pp. 243–257. [Google Scholar]
- Hammond DL, Tyce GM, Yaksh TL. Efflux of 5-hydroxytryptamine and noradrenaline into spinal cord superfusates during stimulation of the rat medulla. J. Physiol. (London) 1985;359:151–162. doi: 10.1113/jphysiol.1985.sp015579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond DL, Nelson V, Thomas DA. Intrathecal methysergide antagonizes the antinociception, but not the hyperalgesia produced by microinjection of baclofen in the ventromedial medulla of the rat. Neurosci. Lett. 1998;244:93–96. doi: 10.1016/s0304-3940(98)00142-6. [DOI] [PubMed] [Google Scholar]
- Kalra A, Urban MO, Sluka KA. Blockade of opioid receptors in rostral ventral medulla prevents antihyperalgesia produced by transcutaneous electrical nerve stimulation (TENS) J. Pharmacol. Exp. Ther. 2001;298:257–263. [PubMed] [Google Scholar]
- Kawamata T, Omote K, Toriyabe M, Kawamata M, Namiki A. Intracerebroventricular morphine produces antinociception by evoking gamma-aminobutyric acid release through activation of 5-hydroxytryptamine 3 receptors in the spinal cord. Anesthesiology. 2002;96:1175–1182. doi: 10.1097/00000542-200205000-00022. [DOI] [PubMed] [Google Scholar]
- King EW, Sluka KA. The effect of varying frequency and intensity of transcutaneous electrical nerve stimulation on secondary mechanical hyperalgesia in an animal model of inflammation. J. Pain. 2001;2:128–133. doi: 10.1054/jpai.2001.19963. [DOI] [PubMed] [Google Scholar]
- Lin Q, Peng YB, Willis WD. Glycine and GABA(A) antagonists reduce the inhibition of primate spinothalamic tract neurons produced by stimulation in periaqueductal gray. Brain Res. 1994;654:286–302. doi: 10.1016/0006-8993(94)90491-x. [DOI] [PubMed] [Google Scholar]
- Lin Q, Peng YB, Willis WD. Role of GABA receptor subtypes in inhibition of primate spinothalamic tract neurons: difference between spinal and periaqueductal gray inhibition. J. Neurophysiol. 1996a;75:109–123. doi: 10.1152/jn.1996.75.1.109. [DOI] [PubMed] [Google Scholar]
- Lin Q, Peng YB, Willis WD. Antinociception and inhibition from the periaqueductal gray are mediated in part by spinal 5HT1A receptors. J. Pharmacol. Exp. Ther. 1996b;276:958–967. [PubMed] [Google Scholar]
- Linderoth B, Stiller CO, Gunasekera L, O’Connor WT, Ungerstedt U, Brodin E. Gamma-aminobutyric acid is released in the dorsal horn by electrical spinal cord stimulation: an in vivo microdialysis study in the rat. Neurosurgery. 1994;34:484–488. doi: 10.1227/00006123-199403000-00014. [DOI] [PubMed] [Google Scholar]
- Ma YT, Sluka KA. Reduction in inflammation-induced sensitization of dorsal horn neurons by transcutaneous electrical nerve stimulation in anesthetized rats. Exp. Brain Res. 2001;137:94–102. doi: 10.1007/s002210000629. [DOI] [PubMed] [Google Scholar]
- Peng YB, Lin Q, Willis WD. Effects of GABA and glycine receptor antagonists on the activity and PAG-induced inhibition of rat dorsal horn neurons. Brain Res. 1996;736:189–201. doi: 10.1016/0006-8993(96)00668-3. [DOI] [PubMed] [Google Scholar]
- Radhakrishnan R, Sluka KA. Spinal muscarinic receptors are activated during low or high frequency TENS-induced antihyperalgesia in rats. Neuropharmacology. 2003;45:1111–1119. doi: 10.1016/s0028-3908(03)00280-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radhakrishnan R, Sluka KA. Deep tissue afferents, but not cutaneous afferents, mediate TENS-induced antihyperalgesia. J. Pain. 2005;6:673–680. doi: 10.1016/j.jpain.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Radhakrishnan R, King EW, Dickman J, Richtsmeier C, Schardt N, Spurgin M, Sluka KA. Blockade of spinal 5-HT receptor subtypes prevents low, but not high, frequency TENS-induced antihyperalgesia in rats. Pain. 2003;105:205–213. doi: 10.1016/s0304-3959(03)00207-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schousboe A. Role of astrocytes in the maintenance and modulation of glutamatergic and GABAergic neurotransmission. Neurochem. Res. 2003;28:347–352. doi: 10.1023/a:1022397704922. [DOI] [PubMed] [Google Scholar]
- Skyba DA, Radhakrishnan R, Sluka KA. Characterization of a method for measuring primary hyperalgesia of deep somatic tissue. J. Pain. 2005;6:41–47. doi: 10.1016/j.jpain.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Sluka KA, Westlund KN. An experimental arthritis in rat: dorsal horn aspartate and glutamate increases. Neurosci. Lett. 1992;145:141–144. doi: 10.1016/0304-3940(92)90006-s. [DOI] [PubMed] [Google Scholar]
- Sluka KA, Westlund KN. Behavioral and immunohistochemical changes in an experimental arthritis model in rats. Pain. 1993;55:367–377. doi: 10.1016/0304-3959(93)90013-F. [DOI] [PubMed] [Google Scholar]
- Sluka KA, Bailey K, Bogush J, Olson R, Ricketts A. Treatment with either high or low frequency TENS reduces the secondary hyperalgesia observed after injection of kaolin and carrageenan into the knee joint. Pain. 1998;77:97–102. doi: 10.1016/S0304-3959(98)00090-6. [DOI] [PubMed] [Google Scholar]
- Sluka KA, Deacon M, Stibal A, Strissel S, Terpstra A. Spinal blockade of opioid receptors prevents the analgesia produced by TENS in arthritic rats. J. Pharmacol. Exp. Ther. 1999;289:840–846. [PubMed] [Google Scholar]
- Sluka KA, Vance CGT, Lisi TL. High, but not low, frequency transcutaneous electrical nerve stimulation (TENS) reduces aspartate and glutamate release in the spinal cord dorsal horn. J. Neurochem. 2005;95:1794–1801. doi: 10.1111/j.1471-4159.2005.03511.x. [DOI] [PubMed] [Google Scholar]
- Sluka KA, Lisi TL, Westlund KN. Increased release of serotonin in the spinal cord during low, but not high, frequency TENS. Arch. Phys. Med. Rehabil. 2006 doi: 10.1016/j.apmr.2006.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin LS, Mcadoo DJ, Willis WD. Raphe magnus stimulation induced antinociception in the cat is associated with release of amino acids as well as serotonin in the lumbar dorsal horn. Brain Res. 1993;618:95–108. doi: 10.1016/0006-8993(93)90433-n. [DOI] [PubMed] [Google Scholar]
- Stiller C-O, Cui J-G, O’Conner WT, Brodin E, Meyerson BA, Linderoth B. Release of y-aminobutyric acid in the dorsal horn and suppression of tactile allodynia by spinal cord stimulation in mononeuropathic rats. Neurosurgery. 1996;39:367–374. doi: 10.1097/00006123-199608000-00026. [DOI] [PubMed] [Google Scholar]
- Sykova E. Extrasynaptic volume transmission and diffusion parameters of the extracellular space. Neuroscience. 2004;129:861–876. doi: 10.1016/j.neuroscience.2004.06.077. [DOI] [PubMed] [Google Scholar]
- Timmerman W, Westerink BHC. Brain microdialysis of GABA and glutamate: what does it signify? Synapse. 1997;27:242–261. doi: 10.1002/(SICI)1098-2396(199711)27:3<242::AID-SYN9>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Woolf CJ, Mitchell D, Barrett GD. Antinociceptive effect of peripheral segmental electrical stimulation in the rat. Pain. 1980;8:237–252. doi: 10.1016/0304-3959(88)90011-5. [DOI] [PubMed] [Google Scholar]
- Zahn PK, Sluka KA, Brennan TJ. Excitatory amino acid release in the spinal cord caused by plantar incision in the rat. Pain. 2002;100:65–76. doi: 10.1016/s0304-3959(02)00241-5. [DOI] [PubMed] [Google Scholar]