Abstract
Objectives
To compare the efficacy and tolerability of Hypericum perforatum (St John's wort extract) with imipramine in patients with mild to moderate depression.
Design
Randomised, multicentre, double blind, parallel group trial.
Setting
40 outpatient clinics in Germany.
Participants
324 outpatients with mild to moderate depression.
Intervention
75 mg imipramine twice daily or 250 mg hypericum extract ZE 117 twice daily for 6 weeks.
Main outcome measures
Hamilton depression rating scale, clinical global impression scale, and patient's global impression scale.
Results
Among the 157 participants taking hypericum mean scores on the Hamilton depression scale decreased from 22.4 at baseline to 12.00 at end point; among the 167 participants taking imipramine they fell from 22.1 to 12.75. Mean clinical global impression scores at end point were 2.22 out of 7 for the hypericum group and 2.42 for the imipramine group. On the 7 point self assessments of global improvement completed by participants (score of 1 indicating “very much improved” and 7 indicating “very much deteriorated”) mean scores were 2.44 in the hypericum group and 2.60 in the imipramine group. None of the differences between treatment groups were significant. However, the mean score on the anxiety-somatisation subscale of the Hamilton scale (3.79 in the hypericum group and 4.26 in the imipramine group) indicated a significant advantage for hypericum relative to imipramine. Mean scores on the 5 point scale used by participants to assess tolerability (score of 1 indicating excellent tolerability and 5 indicating very poor tolerability) were better for hypericum (1.67) than imipramine (2.35). Adverse events occurred in 62/157 (39%) participants taking hypericum and in 105/167 (63%) taking imipramine. 4 (3%) participants taking hypericum withdrew because of adverse events compared with 26 (16%) taking imipramine.
Conclusions
This Hypericum perforatum extract is therapeutically equivalent to imipramine in treating mild to moderate depression, but patients tolerate hypericum better.
Introduction
Hippocrates, Pliny, and Galen described the use of Hypericum perforatum (St John's wort) as a treatment against demonic possession in ancient Greece.1–3 Hypericum extracts are licensed in continental Europe for the treatment of depression and anxiety.4,5 In the United Kingdom, hypericum is available over the counter.
The efficacy of hypericum in depression has been evaluated over several decades; some reviews have identified as many as 23 published trials.6 Recently, direct comparative studies have been conducted against amitriptyline, imipramine, and placebo.7–11 Comparisons with maprotiline in patients with moderate to severe depression and with imipramine in severely depressed patients have also been published.12,13 However, the design of the studies, the methodology used, and the statistical analyses have often been criticised.6,14 A meta-analysis concluded that hypericum was more effective than placebo but that further studies were required to establish whether hypericum is as effective as other antidepressants.6
The aim of this study was to evaluate the clinical efficacy of hypericum extract and compare it with the recommended dose (150 mg) of imipramine, one of the most commonly used tricyclic antidepressants.15
Particular attention was paid to the design and methodology of the study, including using a sufficiently large sample size to allow robust statistical analyses. The study was performed in accordance with the principles of the Declaration of Helsinki on human rights in clinical research and European Union guidelines on good clinical practice.16,17
Participants and methods
Trial structure
The study took place in 40 psychiatric, internal medicine, and general medicine practices in Germany between June 1997 and April 1998. Only outpatients were recruited.
Participants were treated with either hypericum extract standardised to 0.2% hypericin extracted in ethanol 50% w/w (250 mg film coated tablet taken twice daily) (Remotiv, hypericum extract ZE 117, Bayer Vital, Leverkusen, Germany) or imipramine (75 mg tablet twice daily). To ensure that participants could tolerate imipramine, the dose was increased from 25 mg twice daily (3 days) to 50 mg twice daily (4 days) and then to the final dose from the eighth day. Blinding to treatment was assured by using a “double dummy” design—that is, all participants received one of the two active treatments plus placebos of the comparison treatment.
All physicians had experience using the psychopathological rating scales. The scales used included the Hamilton depression rating scale—completed by the physician—which measures 17 items including mood, guilt, sleep disturbance, work activities, anxiety, somatic symptoms, and suicidal ideation.18,19 A score of 14-20 is associated with mild depression, a score of 21-25 with moderate depression. The Hamilton scale was completed during the screening visit and at the time the participant was allocated to treatment. It was also completed at the third visit (week 1), fourth visit (week 3), and fifth visit (week 6).
The clinical global impression scale was completed by the clinicians. It is a 7 point scale: a score of 1 indicates that a patient is “very much improved” and a score of 7 indicates that a patient is “very much worse.” It was completed during the third, fourth, and fifth visits.20
Participants completed a global impression scale the first time they were seen while taking drug treatment (third visit) and at the fifth visit. This scale consists of two items. The first item mirrors the clinical global impression scale: a score of 1 indicates that a participant is “very much improved” and a score of 7 indicates that a participant's condition is “very much deteriorated.” The second item assesses tolerability. Scores range from 1 (tolerability is excellent) to 5 (tolerability is very poor). Thus, lower scores on these scales indicate improvement.
Investigators were trained before the study to use the scales to ensure consistency in ratings both within and between centres. All assessments were made by the same individual in each clinic.
Selection of participants
Men and women were included if they were aged 18 or older and presented with mild to moderate depression without increased suicidal ideation and if they fulfilled ICD-10 (international classification of diseases, 10th revision) criteria for a depressive episode or recurrent depressive disorder (ICD-10 codes F32.0 or F33.0 and F32.1 or F33.1). All participants gave written, informed consent before entering the study.
Participants had to score ⩾18 on the 17 item Hamilton depression rating scale on two consecutive visits to be included in the study.18,19 Participants were excluded if they were pregnant or breast feeding, if they were premenopausal and not using contraception, were known to be allergic to the drugs being studied, or had a serious disease that in the investigator's opinion should preclude their entry to the study. They were also excluded if they had abnormal thyroid function or other relevant abnormalities on laboratory testing, or if they had bipolar disorder, previous serious psychiatric disease, or misused alcohol or drugs. Participants who had taken any of the following medications within the past 14 days were also excluded: monoamine oxidase inhibitors, antidepressant drugs, lithium, antipsychotic drugs, neuroleptic drugs, cimetidine, oral corticosteroids, anticonvulsants, theophylline, or thyroid hormones. Owing to the 50% chance of receiving imipramine in the study, benzodiazepines were allowed at a maximum daily dose of 10 mg diazepam for not longer than three consecutive days on not more than three occasions over the six weeks of the study.
Statistical analysis
The main variable measuring efficacy was the change in scores from baseline on the Hamilton scale. The end point was the final visit at six weeks or the last observation carried forward if the participant withdrew earlier. The sample size was calculated assuming that if hypericum was not the inferior treatment this would be indicated by a difference in improvement between the groups of >3.5 points on the Hamilton scale favouring imipramine; the assumed difference between the two treatments was 0, with a standard deviation of 9 points. The null hypothesis was that hypericum was the inferior treatment. To reject the null hypothesis (one sided) with a power of 90% and an α of 5%, a minimum sample size of 114 participants per group was required. If a withdrawal rate of 25% was assumed then a minimum of 152 participants per group was required. The computer generated randomisation sequence was balanced in blocks of six.
All efficacy analyses were done on an intention to treat basis and on the basis of compliance with protocols—that is, only data from those participants who were treated for a minimum of 35 days were analysed. Safety was evaluated using the intention to treat analysis.
An analysis of covariance for the main efficacy variable used baseline scores on the Hamilton scale as a covariate and used end point as the dependent variable; the treatment and centre were factored into the model. Calculations of 95% confidence intervals were based on differences between the least square means of the general linear model. Significance tests of secondary variables were exploratory and not adjusted for multiple testing. Thus, for the secondary parameters (the clinical global impression scale and the patient's global impression scale), P values were regarded as an indication of the plausibility of the effect rather than true differences.20
Results
Both the intention to treat analysis and the analysis of data from participants who complied with the protocol were planned prospectively; the latter is preferred by some statisticians in equivalence studies.21 Both types of analyses yielded almost identical results. Therefore, whenever results are presented they relate to the intention to treat population unless otherwise stated.
Participants' characteristics at entry
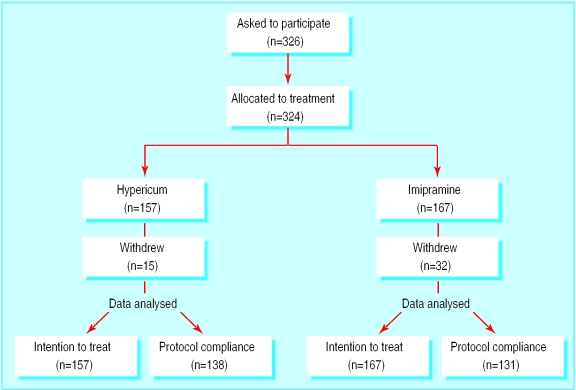
The demographic characteristics of participants are shown in table 1 and the randomisation of treatment is shown in the figure. Altogether 326 patients were asked to participate; two were excluded. Of these, 157 were randomly assigned to treatment with hypericum extract and 167 to imipramine. The two treatment groups were balanced at entry with regard to the main demographic variables and measures of depression.
Table 1.
Characteristics of patients at time of entering the study. Values are means (SD) unless indicated otherwise
| Treatment
|
||
|---|---|---|
| Hypericum (n=157) | Imipramine (n=167) | |
| No (%) women | 112 (71) | 119 (71) |
| Age (years) | 46.5 (12.7) | 45.4 (12.8) |
| Weight (kg) | 72.1 (14.2) | 72.3 (13.6) |
| Height (cm) | 168.9 (8.2) | 168.2 (7.9) |
| Score on Hamilton depression rating scale | 22.4 (3.4) | 22.1 (2.9) |
| Score on anxiety subscale of Hamilton scale | 7.14 (2.21) | 7.06 (2.06) |
| Score on clinical global impression scale | 4.06 (0.61) | 4.04 (0.53) |
More participants (189/324) were classed as having mild depression (ICD-10 F32.0 or F33.0) than moderate (135/324; F32.1 or F33.1). The mean age at onset, presence of concomitant disease, and mean duration of current depressive episode were similar between the groups (data not shown). Six participants had previously been treated in psychiatric hospitals (five in the hypericum group and one in the imipramine group). Altogether, 81/324 (25%) of participants had a family history of depression and 96/324 (30%) had had antidepressant treatment in the previous two years (data not shown). The distribution of these characteristics was similar between the two groups.
Efficacy
The main efficacy results are shown in table 2. The two treatments were therapeutically equivalent with regard to overall effect on depression. All secondary analyses of efficacy supported the conclusions of the primary analysis, although in one exploratory parameter (the anxiety-somatisation subscale of the Hamilton scale) hypericum had a significant advantage. Rates of response to treatment were essentially similar (table 3).
Table 2.
Effects of treatment at six weeks. Analyses are on an intention to treat basis unless indicated otherwise. Values are least square means unless indicated otherwise
| Treatment
|
Difference of least square means (95% CI)* | P value† | |||
|---|---|---|---|---|---|
| Hypericum (n=157) | Imipramine (n=167) | ||||
| Primary variable | |||||
| Hamilton depression rating scale:‡ | |||||
| Change from baseline score | 12.00 | 12.75 | −0.75 (−1.90 to 0.40) | 0.20 | |
| Change from baseline score (analysis of data from patients who complied with protocol) | 11.53 | 11.21 | 0.32 (−0.72 to 1.36) | 0.55 | |
| Secondary variables | |||||
| Hamilton depression scale: | |||||
| Score on anxiety-somatisation subscale | 3.79 | 4.26 | −0.48 (−0.91 to −0.04) | 0.03 | |
| Score on depression subscale | 4.33 | 4.57 | −0.24 (−0.74 to 0.26) | 0.35 | |
| Score on clinical global impression scale‡ | 2.22 | 2.42 | −0.20 (−0.42 to 0.02) | 0.08 | |
| Score on patient's global impression scale‡ | 2.44 | 2.60 | −0.16 (−0.40 to 0.09) | 0.20 | |
| Score of patient's assessment of tolerability | 1.67 | 2.35 | −0.68 (−0.88 to −0.49) | 0.00 | |
Least square means are derived from the general linear model (analysis of covariance). The means are adjusted (end points reflect changes corrected for baseline values).
P values are exploratory; they are derived from the statistical analyses conducted to construct confidence intervals.
Lower scores indicate greater improvement.
Table 3.
Response to treatment as measured by decrease in scores on Hamilton depression rating scale. Lower scores indicate greater improvement. Values are numbers (percentages) unless indicated otherwise
| Change in score on Hamilton depression rating scale | Treatment
|
Relative risk (95% CI) | |
|---|---|---|---|
| Hypericum (n=157) | Imipramine (n=167) | ||
| ⩾50% decrease | 68 (43) | 67 (40) | 1.08 (0.83 to 1.40) |
| ⩾20% decrease | 115 (73) | 109 (65) | 1.12 (0.97 to 1.30) |
| ⩾10 point decrease | 77 (49) | 75 (45) | 1.09 (0.87 to 1.38) |
Safety and tolerability
The incidence of adverse events in each group is shown in table 4. Participants tolerated hypericum better than imipramine (P<0.01). Adverse events were reported by more participants treated with imipramine than with hypericum (105/167 (63%) v 62/157 (39%)). Four (3%) patients on hypericum stopped treatment because of adverse events. Conversely, 1 in 6 participants on imipramine withdrew from treatment because of adverse events.
Table 4.
Number (percentage) of adverse events and withdrawals from treatment caused by adverse events
| Treatment
|
||
|---|---|---|
| Hypericum (n=157) | Imipramine (n=167) | |
| Patients reporting adverse events | 62 (39) | 105 (63) |
| Total No adverse events | 121/359 (34) | 238/359 (66) |
| All adverse events possibly or probably related to drug treatment | 50/202 (25) | 152/202 (75) |
| Treatment withdrawals caused by adverse events | 4 (3) | 26 (16) |
| Most common adverse events possibly or probably related to drug treatment: | ||
| Dry mouth | 13 (8) | 41 (25) |
| Headache | 3 (2) | 6 (4) |
| Sweating | 2 (1) | 13 (8) |
| Asthenia | 2 (1) | 11 (7) |
| Nausea | 1 (<1) | 12 (7) |
| Dizziness | 0 | 12 (7) |
The most common adverse events reported in the imipramine group were dry mouth (41 participants (25%)), sweating, dizziness, nausea, asthenia, and headache. Dry mouth was also the most commonly reported adverse event in the hypericum group (13 participants (8%)). All other adverse events occurred in fewer than three participants in the hypericum group.
Discussion
The efficacy and safety of herbal remedies is often not subjected to the systematic testing required of conventional drugs. The safety and efficacy of hypericum has been questioned in editorials, and two recent comprehensive overviews of the literature highlighted the importance of controlled trials and strict methodology in evaluating hypericum. 4,6,22 Additionally, further studies comparing the use of hypericum extracts with standard antidepressants were needed. Thus, this study was planned to be the largest randomised controlled study of hypericum. Other large and methodologically robust comparative trials of hypericum have recently been published by Wheatley (165 patients),7 by Vorbach et al (209 patients),13 and by Philipp et al (263 patients).23 In contrast to most published studies the dose of imipramine used in this study (150 mg per day) is considered to be a full therapeutic dose.15
The results of this study support the conclusion that the two treatments are therapeutically equivalent. There was some evidence to suggest that hypericum may be better than imipramine in relieving anxiety associated with depression although there were no differences in any of the measures of efficacy.
Herbal remedies are reputed to be well tolerated, and we monitored adverse events systematically, using the double dummy technique of double blinding to avoid any biases. The results confirmed both the expected side effects of imipramine and those of hypericum. The 8% incidence of dry mouth occurring with hypericum treatment highlights the fact that both participants and doctors were aware that participants had a 50% chance of being treated with imipramine; a similar finding has been reported in other studies using tricyclic antidepressants as controls.7,8,12,13 Hypericum was better tolerated; this was confirmed by the results of participants' self assessments (P<0.01) (data not shown) and by the difference in withdrawal rates for adverse effects between the groups (3% for hypericum v 16% for imipramine). In this study no interactions were observed; reports of possible interactions of hypericum with other drugs are few but must be borne in mind when treating patients, particularly those receiving concomitant ciclosporin,24 digoxin,25 indinavir,26 and theophylline.27
Treating patients with mild to moderate depression can be a challenge. The mild nature of the disorder often precludes the treatments commonly used in severe depression, such as tricyclic antidepressants or selective serotonin reuptake inhibitors. This is particularly relevant in general practice where the milder forms of depression are more commonly encountered. Patients seen in general practice frequently prefer to bear the symptoms of depression rather than sustain the side effects of treatment with antidepressants.11 In these situations, an effective antidepressant with no (or comparatively few) side effects, which is acceptable to patients, would be an optimal treatment. Hypericum seems to meet these criteria.
Previous meta-analyses have concluded that hypericum is more effective than placebo, and this and other studies have shown it to be as efficacious as standard antidepressants.6,14 Placebo controlled studies of hypericum have found a low incidence of adverse events; this study confirms that patients tolerate hypericum better than imipramine.
Conclusions
Hypericum is therapeutically equivalent to imipramine, but is better tolerated by patients. These results taken with conclusions from recent overviews6,14 and other large comparative trials7,13 provide compelling evidence that hypericum is therapeutically equivalent to standard antidepressants. In view of the mounting evidence of hypericum's comparable efficacy to other antidepressants and its safety record, hypericum should be considered for first line treatment in mild to moderate depression, especially in the primary care setting.
What is already known on this topic
Hypericum perforatum extracts are licensed in continental Europe for the treatment of depression and anxiety
The design and methodology of studies evaluating the efficacy of hypericum have often been criticised
What this study adds
This is the largest controlled trial of hypericum for treating depression
After six weeks of treatment, hypericum and imipramine are therapeutically equivalent in patients with mild to moderate depression
Patients with anxiety associated with depression may derive more benefit from treatment with hypericum than with imipramine
Patients treated with hypericum seem to tolerate it better and have fewer adverse events than those treated with imipramine
Hypericum should be considered for treating mild to moderate depression especially in primary care
Supplementary Material
Figure.
Recruitment of patients and randomisation of treatment
Footnotes
Funding: Bayer AG supplied the study medication and sponsored the study through the clinical research organisation Beromed, Berlin, Germany.
Competing interests: None declared. The interpretation of the results was entirely the prerogative of the principal investigator and the study group.
A full list of members of the study group can be found on the BMJ's website
References
- 1.Fernie WT. Herbal simples. Bristol: John Wright; 1897. [Google Scholar]
- 2.Pratt A. Wild flowers. London: Society for Promoting Christian Knowledge; 1853. [Google Scholar]
- 3.Pickering C. Chronological history of plants. Boston: Little Brown; 1879. [Google Scholar]
- 4.Commission Nationale de Pharmacopée France. Pharmacopée française. 10th ed. Paris: Adrapharm; 1982. [Google Scholar]
- 5.Kommission Deutscher Arzneimittel-Codex. Johanniskraut—Hyperici herba. DAC; 1986. [Google Scholar]
- 6.Linde K, Ramirez G, Mulrow C D, Pauls A, Weidenhammer W, Melchart D. St John's wort for depression—an overview and meta-analysis of randomised clinical trials. BMJ. 1996;313:253–258. doi: 10.1136/bmj.313.7052.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wheatley D. LI160, an extract of St John's wort versus amitriptyline in mildly to moderately depressed outpatients—a controlled 6-week clinical trial. Pharmacopsychiatry. 1997;30(suppl):77–80. doi: 10.1055/s-2007-979523. [DOI] [PubMed] [Google Scholar]
- 8.Vorbach EU, Hübner WD, Arnoldt KH. Effectiveness and tolerance of the hypericum extract LI160 in comparison with imipramine: randomised double-blind study in 135 outpatients. J Geriat Psychiatry Neurol. 1994;7(suppl 1):19–23S. doi: 10.1177/089198879400700107. [DOI] [PubMed] [Google Scholar]
- 9.Hänsgen KD, Vesper J, Ploch M. Multicentre double-blind study examining the antidepressant effectiveness of the hypericum extract LI160. J Geriat Psychiatry Neurol. 1994;7(suppl 1):15–8S. doi: 10.1177/089198879400700106. [DOI] [PubMed] [Google Scholar]
- 10.Witte B, Harrer G, Kaplan T, Podzuweit H, Schmidt U. Treatment of depression with a highly concentrated hypericum preparation: a multicentre, placebo-controlled, double-blind study. Fortschr Med. 1995;113:404–408. [PubMed] [Google Scholar]
- 11.Schrader E, Meier B, Brattström A. Hypericum treatment of mild-moderate depression in a placebo-controlled study. A prospective, double-blind, randomized, placebo-controlled, multicentre study. Hum Psychopharmacol. 1998;13:163–169. [Google Scholar]
- 12.Harrer G, Hübner WD, Podzuweit H. Effectiveness and tolerance of the hypericum extract LI160 compared with maprotiline: a multicentre double-blind study. J Geriat Psychiatry Neurol. 1994;7(suppl 1):24–8S. doi: 10.1177/089198879400700108. [DOI] [PubMed] [Google Scholar]
- 13.Vorbach EU, Arnoldt KH, Hübner WD. Efficacy and tolerability of St John's wort extract LI160 versus imipramine in patients with severe depressive episodes according to ICD10. Pharmacopsychiatry. 1997;30(suppl):81–85. doi: 10.1055/s-2007-979524. [DOI] [PubMed] [Google Scholar]
- 14.Ernst E. St John's wort as antidepressive therapy. Fortschr Med. 1995;113:354–355. [PubMed] [Google Scholar]
- 15.Angst J, Bech P, Boyer P, Bruinvels J, Engel R, Helmchen H. Consensus on the methodology of clinical trials of antidepressants, Zurich, March 1988: report of the Consensus Committee. Pharmacopsychiatry. 1989;22:3–7. [Google Scholar]
- 16.International Conference on Harmonisation, Committee on Proprietary Medicinal Products. Notes for guidance on good clinical practice. London: European Agency for Evaluation of Medicinal Products; 1997. . (ICH/135/95.) [Google Scholar]
- 17.European Union. Good clinical practice for clinical investigation of medicines in the European Community. Vol. 3. London: European Agency for Evaluation of Medicinal Products; 1996. pp. 115–132. [Google Scholar]
- 18.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 20.National Institute of Mental Health. 028 CGI clinical global impressions. In: Guy W, editor. ECD-EU assessment for psychopharmacology. Rev ed. Rockville, MD: National Institute of Mental Health; 1976. pp. 217–222. [Google Scholar]
- 21.Jones B, Jarvis P, Lewis JA, Ebbutt AF. Trials to assess equivalence: the importance of rigorous methods. BMJ. 1996;313:36–39. doi: 10.1136/bmj.313.7048.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeSmet PA, Molen WA. St John's wort as an antidepressant. BMJ. 1996;313:241–242. doi: 10.1136/bmj.313.7052.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Philipp M, Kohnen R, Hiller KO. Hypericum extract versus imipramine or placebo in patients with moderate depression: randomised multicentre study of treatment for eight weeks. BMJ. 1999;319:1534–1538. doi: 10.1136/bmj.319.7224.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruschitzka F, Meier PJ, Turina M, Luescher TF, Noll G. Acute heart transplant rejection due to St John's wort. Lancet. 2000;355:548–549. doi: 10.1016/S0140-6736(99)05467-7. [DOI] [PubMed] [Google Scholar]
- 25.Johne A, Brockmöller J, Bauer S, Maurer A, Langheinrich M, Roots I. Pharmacokinetic interaction of digoxin with an herbal extract from St. John's wort (Hypericum perforatum) Clin Pharmacol Ther. 1999;66:338–345. doi: 10.1053/cp.1999.v66.a101944. [DOI] [PubMed] [Google Scholar]
- 26.Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J. Indinavir concentrations and St John's wort. Lancet. 2000;355:547–548. doi: 10.1016/S0140-6736(99)05712-8. [DOI] [PubMed] [Google Scholar]
- 27.Nebel A, Schneider BJ, Baker RK, Kroll DJ. Potential metabolic interaction between St. John's wort and theophylline. Ann Pharmacother. 1999;33:502. doi: 10.1345/aph.18252. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.