Abstract
We evaluated the efficacy of an interactive, computer-based behavioral therapy intervention, grounded in the community reinforcement approach (CRA) plus voucher-based contingency management model of behavior therapy. Our randomized, controlled trial was conducted at a university-based research clinic. Participants comprised 135 volunteer adult outpatients who met DSM-IV criteria for opioid dependence. All participants received maintenance treatment with buprenorphine and were randomly assigned to one of three treatments: (1) therapist-delivered CRA treatment with vouchers, (2) computer-assisted CRA treatment with vouchers, or (3) standard treatment. The therapist-delivered and computer-assisted CRA plus vouchers interventions produced comparable weeks of continuous opioid and cocaine abstinence (mean = 7.98 and 7.78, respectively) and significantly greater weeks of abstinence than the standard intervention (mean = 4.69; p<.05), yet participants in the computer-assisted CRA condition had over 80% of their intervention delivered by an interactive computer program. The comparable efficacy obtained with computer-assisted and therapist-delivered therapy may enable more widespread dissemination of the evidence-based CRA plus vouchers intervention in a manner that is cost-effective and ensures treatment fidelity.
Keywords: Computerized treatment, opioid dependence, buprenorphine, cognitive-behavior therapy, controlled trial
Introduction
A reevaluation of the current drug abuse treatment system may be required to positively and substantively impact the problem of substance use disorders. Despite numerous important scientific advances in the treatment of drug dependence over the last decade, such a reassessment may be necessary because of the many serious challenges facing the treatment system. The current system has difficulty recruiting and retaining treatment staff, inadequate financing for the provision of treatment, treatment availability insufficient to meet demand, and a slow adoption of research-based treatment innovations (Bickel & McLellan, 1996; McLellan, Carise, & Kleber, 2003). Moreover, the growing problem of dependence disorders in rural communities presents additional challenges for the provision of treatment.
These challenges may be partially addressed by applying computer-based interactive technologies to deliver aspects of substance abuse treatment. Computer-based interactive technologies refer to “computer-based media that enables users to access information and services of interest, control how the information is presented, and respond to information and messages in the mediated environment (e.g., answer questions, send a message, take an action in a game, receive feedback, or make a response to previous actions)” (Street & Rimal, 1997). Two central features of this technology are interactivity and modularity (Street & Rimal, 1997). Interactivity refers to the responsiveness of the program to the behavior of the user such that the user may modify or control the presentation of material (Rafaeli, 1988; Steuer, 1992). Modularity refers to the user’s ability to move from one portion of a program to another (Dede & Fontana, 1995; Street & Rimal, 1997). Types of interactive, computer-based technology that have been employed in providing treatment or promoting health behaviors include desktop computers (Selmi, Klein, Greist, Sorrell, & Erdman, 1990), e-mail (Murphy & Mitchell, 1998), hand-held devices (Newman, Kenardy, Herman, & Taylor, 1997), telephone-accessed computer systems (Osgood-Hynes et al., 1998), video-disc training (Thorkildsen, Bickel, & Williams, 1979)), virtual reality systems (North, North, & Coble, 1997) and Web-based interventions (Wantland, Portillo, Holzemer, Slaughter, & McGhee, 2004). The number of computer-delivered therapeutic interventions or health promotion programs is growing and applicable to an ever-increasing array of disorders (Taylor & Luce, 2003; Wantland et al., 2004).
The most widely developed computerized treatments for psychiatric disorders have been for anxiety and depressive disorders (Buglione, Devito, & Mulloy, 1990; Newman, Consoli, & Taylor, 1997; Newman, Kenardy, Herman, & Taylor, 1996; Selmi, Klein, Greist, Sorrell, & Erdman, 1991). One factor making development of computer-based treatments of these disorders more feasible may be the fact that manuals have been developed for non-computer-based cognitive-behavioral interventions for these disorders; that is, manual-driven treatments that specify the use of certain sequences of procedures may be readily adapted for computer-based interventions (Selmi et al., 1990). Interestingly, comparable outcomes have generally been reported when computer-delivered and therapist-delivered treatments have been compared (Buglione et al., 1990; Carr, Ghosh, & Marks, 1988).
The use of computers in substance abuse treatment is a small but growing research area. Several studies have demonstrated the effective use of computer-generated personalized messages and feedback to users in promoting smoking cessation, encouraging movement of smokers along the stages of change, or promoting nicotine fading procedures (Burling, Seidner, & Gaither, 1994; Curry, McBride, Grothaus, Louie, & Wagner, 1995; Dijkstra, DeVries, & Roijackers, 1998; Prochaska, Velicer, Guardagnoli, & Rossi, 1991; Schneider, Schwartz, & Fast, 1995; Schneider & Tooley, 1986; Strecher et al., 1994; Velicer et al., 1993). To our knowledge, three controlled clinical trials have examined the efficacy of interactive computer-delivered therapy during drug abuse or alcohol treatment. The first study demonstrated that a computerized version of a behavioral self-control training program produced significant reductions in drinking among heavy drinkers (Hester & Delaney, 1997). The second study demonstrated that a computer-based, brief motivational intervention promoted a reduction in the quantity and frequency of drinking and associated problems among problem drinkers (Hester, Squires, & Delaney, 2005). A third study, that compared computer-delivered to therapist-delivered HIV/AIDS education among opioid-dependent, injection drug-users (IDUs) receiving buprenorphine treatment (Marsch & Bickel, 2004), found that participants who received computer-based instruction learned significantly more information, retained more of that information at a 3-month follow-up, liked the teaching medium better, and requested more supplemental information about HIV/AIDS relative to those in the therapist-delivered program. Additional research on computer-based technology in the treatment of substance abuse is necessary because of its potential to address the challenges of the current treatment system. Indeed, adoption of such technology may play a critical role in improving community-based substance abuse treatment in a manner that enables rapid diffusion and adoption of evidence-based interventions (See Bickel & Marsch, 2007 for a discussion of the application of computer technology to substance abuse prevention and treatment; Carise, Ozge, McLellan, Dugosh, & Kendig, 2005).
This article reports on the application of computer-based interactive technology to the treatment of opioid dependence. Specifically, we computerized the cognitive behavior therapy package referred to as the community reinforcement approach (CRA) with contingency management (Budney & Higgins, 1998). We selected to develop a computer-based therapeutic intervention theoretically grounded in the CRA intervention because this intervention has been shown repeatedly to be effective in treating substance use disorders, including opioid dependence (Abbott, Weller, Delaney, & Moore, 1998; Bickel, Amass, Higgins, Badger, & Esch, 1997; Higgins, Budney, & Bickel, 1993; Higgins et al., 1994; Higgins, Delaney, & al., 1991; Higgins, Sigmon, Wong, & al., 2003). In this research program, we have adopted a similar approach to prior evaluations of CRA with vouchers, which first demonstrated the efficacy of the treatment package and then examined the efficacy of the components of the package. Thus, in the present study we will examine whether there is an overall difference between the replacement of counselor delivered therapy with computer delivered therapy as part of the treatment package as compared to the treatment package with counselor delivered therapy. To ensure that the two treatment packages each have efficacy a usual treatment condition is also used as a comparator. Thus, to evaluate this computer-delivered intervention, opioid-dependent outpatients were randomly assigned to one of three treatments in a randomized, controlled trial: (1) therapist-delivered CRA behavioral treatment with vouchers, (2) computer-assisted CRA behavioral treatment with vouchers, or (3) standard treatment (typical counseling offered at methadone treatment clinics) (Ball & Ross, 1991). Note that this standard treatment has been employed as a comparator in other studies (Bickel et al., 1997; Gross, Marsch, Badger, & Bickel, 2006). All participants received maintenance treatment with the partial opioid agonist buprenorphine as a background therapy (see Bickel & Amass, 1995, for a review). To our knowledge, the interactive, computer-delivered intervention described in this report is the only computer-based intervention that is based on the community reinforcement approach for individuals with opioid dependence and that has been evaluated in a controlled study.
Methods
Participants
One-hundred and eighty-one (181) individuals were assessed for eligibility for this study, and 57 of these participants were excluded (35 of these 57 participants did not return during the medication induction period and the remaining 11 were excluded for various other reasons), thus resulting in 135 opioid-dependent adults who participated in this study’s 23-week, outpatient maintenance treatment phase. Participants were recruited over a 2-year period by newspaper, radio, and television advertisements, word of mouth, and various referral sources (e.g., physicians, alcohol, and drug abuse clinics). All participants (a) met DSM-IV opioid dependence criteria; (b) met FDA methadone treatment qualification criteria; (c) were ≥ 18 years of age; (d) were void of active psychiatric disorders (e.g., psychosis, manic-depressive illness) and significant medical illnesses (e.g., cardiovascular disease); and (e) were not pregnant as determined by urinary pregnancy tests conducted at intake and at weekly intervals throughout the study. All patients provided written informed consent prior to study participation. This study was conducted at an outpatient research clinic at the University of Vermont and was approved by the University’s Institutional Review Board.
Randomization
Participants were randomly assigned to one of the three maintenance treatment groups using a computer generated stratified randomization procedure in SAS. A separate randomization list was provided by the biostatistician for each of the twelve strata defined by the following three patient characteristics: (1) buprenorphine/naloxone maintenance dose (≤ or > 12 mg); (2) past month cocaine use (y/n); and (3) one-way commute time to clinic (< 30 minutes, 30 – 60 minutes, > 60 minutes).
Urinalysis and Blood Alcohol Level Monitoring
Urine specimens were collected thrice weekly (Mondays, Wednesdays, Fridays) under staff observation and screened immediately on-site using the MIRA semi-quantitative urinalysis machine (Syva Corp., San Jose, CA). All specimens were screened for methadone, opioids, propoxyphene, cocaine, and benzodiazepines (Fridays only). In addition, breath samples were analyzed thrice weekly for blood alcohol levels (ALCO-SENSOR III, Intoximeters, Inc., St. Louis, MO), which had to be less than 0.05 g/ml for patients to receive their medication.
Behavioral Treatment
Therapist-delivered community reinforcement approach (CRA) treatment with contingency management
Participants in this condition received behavioral treatment based on CRA plus voucher-based contingency management (Budney & Higgins, 1998), with modifications as appropriate for an opioid-dependent patient population (e.g., detoxification training). Therapist-delivered CRA and voucher-based contingency management treatment was administered throughout the 23-week maintenance treatment phase. During the first 12 weeks of maintenance treatment, the CRA intervention was implemented in three 30-minute individual counseling sessions per week. During the final 11 weeks, CRA was implemented in one 30-minute and two 20-minute individual counseling sessions per week. Participants were provided with counseling in various life skills through the following training modules: Self-Management Planning, Drug-Refusal Training, Time Management, Social/Recreational Counseling, Problem Solving, Vocational Counseling/Employment, Social Skills Training, HIV/AIDS Prevention, Relationship Counseling, Communications Training, Other Substance Abuse, Depression, Anxiety, Insomnia, Relapse Prevention, Anger Management, Pain Management, Detoxification Training, Finance Management, and Housing Solutions. Participants who tested positive for opioid and/or cocaine use completed two modules, Functional Analysis and Self-Management Planning, with their therapist (see Budney & Higgins, 1998 for specific procedures used).
The voucher schedule used in the current study was similar to the schedule used successfully with opioid-dependent individuals receiving a buprenorphine dose tapering regimen in a prior trial (Bickel et al., 1997). Participants earned voucher points by providing opioid- (i.e., opioids, propoxyphene, methadone) and cocaine-negative samples. Each voucher point was worth $0.25. The first negative sample was worth 29 points or $7.25 ($0.25 * 29). Vouchers increased by one point with each consecutive negative sample (i.e., 30 points for the second, 31 for the third, etc.). In addition, a $10.00 bonus was earned for a week (Monday – Friday) of negative samples. Continuous abstinence throughout the 23-week maintenance phase resulted in voucher earnings of $1,316.75.
Submission of an opioid- and/or cocaine-positive urine sample, or failing to submit a valid, scheduled sample reset the voucher points to the baseline of 29 points. Submission of five consecutive opioid- and cocaine-negative samples returned voucher points to the pre-lapse level. Voucher points, once earned, could not be lost.
A research staff member delivered paper copies of vouchers to participants each day they provided a urine sample, indicating if a given sample was positive or negative for opioids and cocaine, the amount of vouchers earned if negative for both drugs, the total account balance to date and the amount that participants could earn for their next submission of an opioid- and cocaine-negative sample. Vouchers were delivered to participants immediately after urine samples were tested, as described above.
Computer-assisted community reinforcement approach (CRA) with contingency management
Participants in this condition received the CRA plus vouchers intervention delivered via an interactive, self-directed computer-based program throughout the 23-week maintenance phase. The computer-assisted CRA and therapist-delivered CRA treatments were identical with respect to CRA frequency, duration, topics, Functional Analysis and Self-Management Planning completion, and voucher schedule, except that in the computer-assisted CRA condition all of these interventions, as well as the printout of paper copies of vouchers, were delivered via computer. In addition, every other week (biweekly), participants in the computer-assisted treatment group met with their therapist for approximately 30 minutes for a brief check and to revise the sequence of modules if necessary. The weeks that participants in this treatment group met with their therapist, they were required to complete only two computerized CRA sessions. The voucher earnings by participants in the therapist-delivered CRA and computer-assisted CRA conditions were comparable across groups (t88 = 0.29; p = .77). Participants in the computer-assisted CRA condition earned a mean of $584.11 (SD=$492.85), and participants in the therapist-delivered CRA condition earned a mean of $555.51 (SD=$439.18).
During the first week of maintenance treatment, participants completed a computer-assisted CRA training program which taught them how to use the computer system. They also completed a “customization program” with their counselor to establish an individual treatment plan using the computer-based program to meet their treatment needs.
The computer-assisted CRA training that participants received involved fluency-based, Computer-Assisted Instruction (CAI) (© Copyright 1997, HealthSim, Inc.). Fluency-based technology is a procedural method of teaching information and skills that has been demonstrated to be effective in acquiring and retaining new information (Kuhn & Stahl, 2003). This approach requires patients to develop a predetermined level of accuracy and speed in responding. For each CRA topic, fluency-building CAI training included the following five steps. (1) Information relevant to a given CRA topic (e.g., social skills training; relationship counseling) was presented. (2) Multiple choice questions specific to the CRA topic were then randomly presented. (3) To promote fluency on a given topic, “read and response timing parameters” were manipulated. “Read time” is defined as the time elapsed between the appearance of a given question and the presentation of the response choices. “Response time” is defined as the time elapsed between the presentation and subsequent removal of response choices. Read and response times varied as a function of the participant’s comprehension of the material. That is, if a participant responded correctly to a question, both the read and response times decreased on the next presentation of that question and vice versa. A question was no longer presented once three consecutive correct responses were provided and the final response time was attained. (4) Fill-in-the-blank questions that addressed the most important facts from the multiple choice questions were then presented, with similar manipulation of read and response timing parameters. (5) Participants were given immediate computer-delivered feedback on their responses, i.e., the computer informed patients whether their responses were correct or incorrect. If incorrect, the computer provided the patient with the correct response and an explanation why the response was correct. In this process, the delivery of CRA topics were adjusted according to pre-determined levels of fluency, speed, and accuracy, making the patient an active participant in the educational process. To accommodate individuals with reading difficulties, participants could have the information, concurrent with its presentation, read aloud to them by computer via headphones.
Several modules within the computer-based system also included video-based simulation technologies (Issenberg, Gordon, Gordon, Safford, & Hart, 2001). The interactive videos presented actors modeling various behaviors in order for the program user to better learn the modeled behavior (e.g., progressive muscle relaxation). The videos also provided experiential learning environments that simulated real world experiences and thereby enabled the exploration of a wide variety of “what if” scenarios, while providing specific feedback in role-playing situations (e.g., effective drug-refusal skills; effective communication skills) (Gustafson, Bosworth, Chewning, & Hawkins, 1987; Orlandi, Dozier, & Marta, 1990).
Upon completion of the CAI portion and simulation portions of computer-assisted CRA training, the skills and information learned by the patients were personalized through other interactive exercises and worksheets (e.g., Practice Exercise for Managing Thoughts About Using, Time Management).
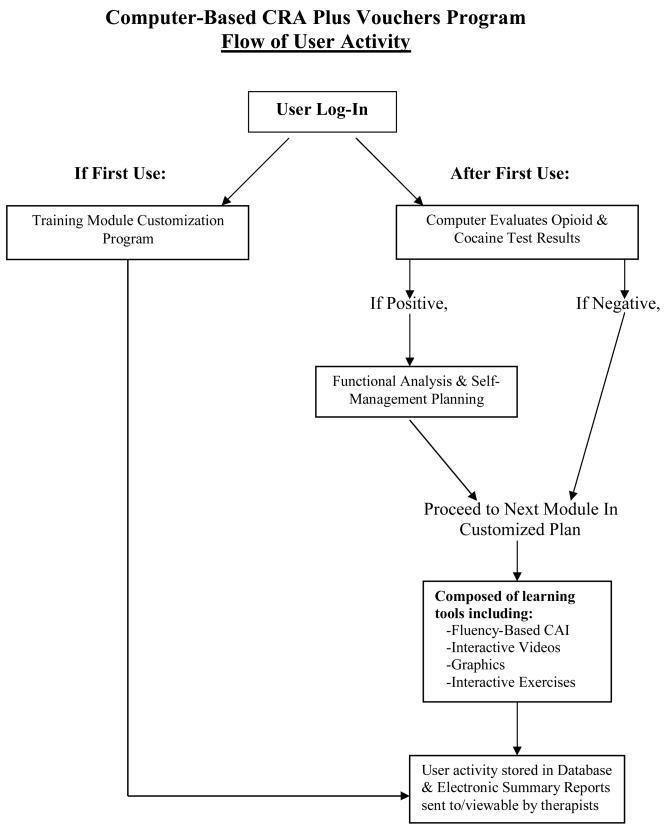
An electronic reporting system provided therapists the opportunity to view browser-based reports summarizing participants’ activity using the computer program as well as results and/or summary information of interactive exercises they completed on the computer (e.g., reports of recent drug use and circumstances surrounding the use). This feature allowed therapists to integrate participants’ use of the program into their biweekly counseling sessions. Figure 1 presents a flow chart of user activity with the computer-assisted CRA program.
Figure 1.
Flow of user activity with computer-based community reinforcement approach (CRA) plus vouchers program.
Standard Methadone-Style Counseling
Standard counseling treatment, the treatment most methadone maintenance programs use (Ball & Ross, 1991), has been described fully and implemented successfully in a previously reported study (Bickel et al., 1997). In this study, throughout the 23-week maintenance treatment phase, standard counseling treatment was implemented in one 37-minute individual counseling session per week (based on the average duration of sessions in most methadone maintenance programs). In these sessions, compliance with program rules and rehabilitation were addressed. These sessions focused on helping participants with current problems (e.g., employment, recent arrests, illness, living arrangements), addressing participants’ treatment progress (attendance, urine test results) and helping them understand and comply with program rules. Counselors followed a manualized set of guidelines regarding the core content and philosophy associated with the delivery of standard therapy, based on the model described by Ball & Ross (1991).
Therapists and Treatment Fidelity
Three master’s-level therapists, who averaged six years experience with opioid-dependent patients, conducted therapy sessions for all participants. Treatment fidelity was assured using numerous strategies, as described here and elsewhere (Bickel et al., 1997). All therapists were trained rigorously in all therapy procedures. Each therapist was assigned an equivalent number of participants in each condition to avoid a therapist-by-condition confounding factor.
A manipulation check was conducted whereby treatment sessions between therapists and clients were audiotaped. An independent evaluator, blind to participants’ treatment conditions, reviewed randomly selected audiotapes to determine if a treatment session could be classified into its appropriate treatment condition based on a checklist that highlighted attributes of the respective therapies. Distinguishing characteristics included the duration of the session as well as adherence to the appropriate content and style of the manual for a given intervention (e.g., a focus on CRA content for those receiving therapist-delivered CRA; a focus on compliance with program rules and rehabilitation for those receiving standard treatment; and a review of progress on the computer and a restructuring of module order [as needed] for those receiving computerized CRA). The independent evaluator reviewed a total of 45 sessions, that is, one session of 25% of all patients (n=181), of which 135 were trial eligible and 46 ineligible. Importantly, across the 45 randomly selected sessions, there was approximately equal representation among the three therapists (15 sessions reviewed per therapist) and treatments (therapist-delivered CRA = 16 sessions, computer-assisted CRA = 13 sessions, standard counseling = 16 sessions). Overall, 82.2% (37/45) of treatment sessions were classified accurately into their respective treatment categories by the independent evaluator. The number of misclassifications were generally comparable across study conditions (3/13 were misclassified in the computer-assisted CRA condition, 1/16 was misclassified in the therapist-delivered CRA condition, and 4/16 were misclassified in the standard condition).
Medication Administration
Patients participated in three dosing phases with the sublingual, partial opioid agonist buprenorphine: induction (6–10 days), maintenance (23 weeks), and withdrawal (9 weeks). Buprenorphine induction lasted approximately 6 – 10 days (Amass, Bickel, Higgins, & Badger, 1994; Amass, Bickel, Higgins, & Hughes, 1994; Bickel et al., 1997). On days 1 and 2, participants were given a 6 mg and 12 mg dose of the buprenorphine mono formulation (Subutex), respectively. On day 3, based on agonist and withdrawal ratings (Himmelsbach, 1939) taken on day 2, participants were given their maintenance dose of either 6, 12, or 18 mg of buprenorphine/naloxone (Suboxone), which they received daily for the remainder of their induction phase (unless agonist or withdrawal ratings after day 3 indicated a further dose adjustment was warranted) and during the 23-week maintenance treatment period using a thrice weekly dosing schedule, in which patients received a double maintenance dose on Mondays and Wednesdays and a triple maintenance dose on Fridays). Medication was gradually tapered during the 9-week withdrawal period. All medication was administered under double-blind conditions.
Outcome Measures
Opioid and cocaine abstinence
Continuous opioid and cocaine abstinence was defined a priori as the primary outcome measure, and statistical power calculations for this study were determined based on this primary outcome measure. One week of continuous opioid and cocaine abstinence was defined as three consecutive (i.e., Monday, Wednesday, Friday) opioid- and cocaine-negative urine samples. Missed urine samples were considered positive. The longest period of continuous abstinence achieved was recorded for each patient. Secondary analyses were performed comparing treatment conditions on the percent of scheduled urinalyses results classified as negative or missing.
Treatment retention
Treatment retention was defined as the percentage of participants in each treatment that were retained in treatment through the maintenance treatment phase. Participants were considered discontinued from maintenance treatment if they (1) completed the 23-week maintenance treatment period, or (2) missed 3 consecutive medication doses.
Addiction Severity Index (ASI)
The ASI (McLellan et al., 1985) is a structured clinical interview designed to provide a reliable, valid measure of multiple problems common among substance abusers. The ASI computes a severity score for substance abuse problems as well as a score for employment, medical, social, legal, and psychological functioning.
The Helping Alliance Questionnaire-Patient Version (HAQ-P)
The HAQ-P (Luborsky et al., 1996) is a 19-item inventory that measures the alliance (degree of helping relationship) between patients and their therapists and enables the calculation of a total alliance score. This measure has adequate internal consistency, test-retest reliability, and convergent validity with the California Psychotherapy Alliance Scale.
Contact time between patients and therapists
Worksheets were completed by therapists thrice weekly to document how much time participants in each study condition spent with their counselor in therapy sessions during the treatment maintenance phase of the trial.
Statistical analyses
Comparisons between treatment groups on baseline characteristics were performed using either analysis of variance or Kruskal-Wallis tests for continuous measures and chi-square tests for categorical variables. Analyses of primary outcome measures associated with continuous abstinence and treatment retention were based on all subjects randomized. Analysis of variance was used to compare groups with respect to the primary outcome measure of mean duration of documented continuous opioid and cocaine abstinence. Analysis of variance was also used to examine percent of scheduled urinalyses attended and results classified as negative. Pairwise comparisons among treatment groups were performed using Fisher’s Least Significant Difference (LSD) procedure. Effect sizes associated with abstinence outcome measures were computed based on the estimated correlation coefficient. Time to event analysis, utilizing a logrank test, was used to compare retention time among treatment groups. In addition, a chi square test was used to compare groups on the percentage of subjects retained through the 23-week treatment maintenance phase.
Repeated measures analyses of variance were used for treatment comparisons on Helping Alliance scores and ASI composite scores when retention was still high in all study conditions. The repeated measures analysis of variance corresponding to Helping Alliance was based on the first 12 weeks of treatment, so as not to have subject dropout adversely influence group comparisons. One hundred and twenty four subjects (92%) were included in these analyses of which ninety-eight were available at 12-weeks (Computer n=34, Therapist n=30 and Standard n=34). Analyses were performed using SAS, PROC MIXED which produces least square means, which adjust for subjects’ missing data at specific time points. ASI composite scores collected at intake and week 13, when retention was still quite high in all study conditions (96/135 = 71% retention) were analyzed in a similar fashion.
Statistical analyses were performed using SAS statistical software (SAS Institute, Cary, NC). The sample sizes of 45 subjects per treatment arm was determined using data from our prior studies in order for the current study to have sufficient power (1-B= .90) to detect a 5 week difference in mean continuous abstinence between any two of the treatment conditions.
Results
As shown in Table 1, with the exception of age, the characteristics of participants assigned to the three treatment groups did not differ. Participants’ age was not predictive of treatment outcome when considered as a covariate.
Table 1.
Participant Demographics by Treatment Condition
| Standard n=45 | Therapist n=45 | Computer n=45 | p-value | |
|---|---|---|---|---|
| Demographics | ||||
| White (%) | 98 | 98 | 93 | .44 |
| Male (%) | 58 | 56 | 53 | .91 |
| Never married (%) | 58 | 76 | 60 | .16 |
| High school education (%) | 71 | 67 | 69 | .90 |
| Employed (%) | 47 | 44 | 49 | .91 |
| Age (in years)a | 30.1 ± 9.2 | 26.1 ± 6.9 | 29.7 ± 8.9 | .05 |
| Monthly income (in dollars)b | 523 (50,1236) | 698 (220,1500 ) | 675 (300,1100) | .56 |
| Opioid use | ||||
| Prior treatment (%) | 64 | 68 | 70 | .82 |
| Years of regular usea | 5.6 ± 6.2 | 5.2 ± 4.4 | 6.4 ± 6.3 | .62 |
| Age of first usea | 22.4 ± 7.9 | 18.9 ± 5.3 | 21.8 ± 8.2 | .08 |
| Days/Week use opioidsa | 6.7 ± 1.1 | 6.7 ± 0.8 | 6.9 ± 0.3 | .50 |
| Preferred route | ||||
| Intravenous (%) | 62 | 80 | 68 | .17 |
| Intranasal (%) | 38 | 20 | 32 | |
| Other drug dependence | ||||
| Alcohol (%) | 18 | 9 | 16 | .44 |
| Cocaine (%) | 24 | 16 | 27 | .38 |
| Sedative (%) | 13 | 7 | 9 | .56 |
| Cannabis (%) | 16 | 18 | 14 | .87 |
| ASI composite scalesa | ||||
| Medical | .20 ± .32 | .19 ± .31 | .17 ± .29 | .92 |
| Employment | .59 ± .30 | .66 ± .31 | .62 ± .33 | .54 |
| Alcohol | .05 ± .11 | .06 ± .11 | .06 ± .10 | .93 |
| Drug | .39 ± .09 | .38 ± .08 | .39 ± .08 | .78 |
| Psychiatric | .32 ± .22 | .36 ± .26 | .31 ± .22 | .58 |
| Legal | .34 ± .25 | .35 ± .28 | .25 ± .24 | .11 |
| Family-social | .31 ± .24 | .21 ± .21 | .23 ± .24 | .11 |
| Beck Depression Inventorya | 20.5 ± 9.1 | 21.6 ± 9.7 | 19.5 ± 9.8 | .60 |
| Michigan Alcoholism Screening Testa | 10.4 ± 13.3 | 11.5 ± 9.2 | 8.7 ± 9.0 | .46 |
| Buprenorphine dose | 15.9 | 16 | 16.4 | 0.71 |
Note: Tabled values are percents unless otherwise indicated, statistical significance based on Chi Square Test
Mean ± SD, statistical significance based on F Test
Median (interquartile range), statistical significance based on Kruskal-Wallis Chi Square Test
Primary Analyses of Opioid and Cocaine Abstinence
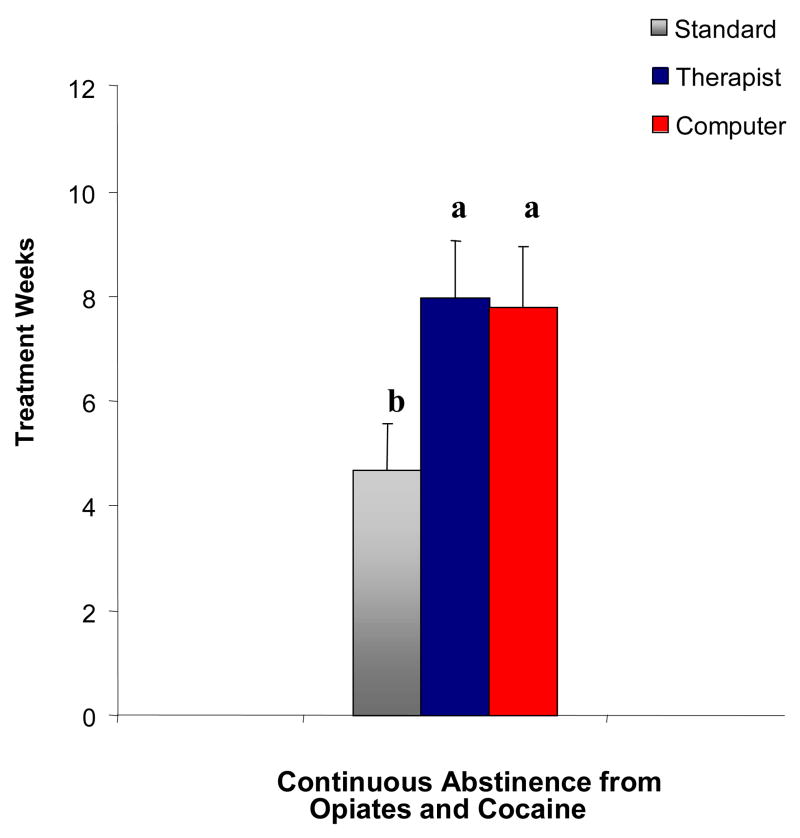
Participants in the standard, therapist-delivered, and computer-assisted treatment conditions achieved an average of 4.69 (SEM = 0.88), 7.98 (SEM = 1.09), and 7.78 (SEM = 1.17) weeks of continuous opioid and cocaine abstinence, respectively, while in maintenance treatment (see Figure 2). This measure significantly differed across treatment groups (F(2, 132) = 3.06; p = 0.05), such that the therapist-delivered and computer-assisted treatment conditions did not significantly differ from one another, but both produced significantly greater weeks of continuous opioid and cocaine abstinence relative to the standard treatment group (Fisher’s LSD, p<.05). The estimated effect size (r) for the therapist-delivered treatment condition was r = 0.19 (SE = .09; 95% CI = .02, .35; p = .03) and for the computer-assisted treatment condition was r= .18 (SE = .09; 95% CI = .01, .34; p = .04), when expressed relative to the standard condition.
Figure 2.
Mean weeks continuous abstinence from opiates and cocaine by treatment condition. Means sharing a common letter are not significantly different from one another.
Secondary Analyses of Opioid and Cocaine Abstinence
Secondary analyses were performed to investigate the role of missing data in urinalyses results. The percent of scheduled urinalyses sessions (n=69) that were attended by study participants were nearly equal across the three conditions (71% for standard, 70% therapist and 70% computer, F2, 132 = 0.04, p= .97). When analyses were restricted to the period in which subjects were retained in treatment (i.e. prior to drop-out), there was also no evidence of differences in the percentage of scheduled urinalysis sessions attended across treatments (87% for standard treatment, 88% for therapist-delivered CRA, and 87% for computer-assisted CRA (F 2,132 = 0.04, p= .96). When urinalysis results were restricted to those samples that were documented to be either positive or negative (i.e. excluding missing urines), 70%, 73% and 57% were negative for opioids and cocaine for Computer-assisted CRA, Therapist-delivered CRA, and Standard groups respectively (F2,131=2.47 p= .08). Effect sizes corresponding to this outcome measure were r = .17 (SE = .11; 95% CI = − .03, .36, p= .10) for the computer-delivered CRA condition, and r = .21 (SE = .10; 95% CI: = .01, .40, p= .05) for the therapist-delivered CRA condition, when expressed relative to the standard condition.
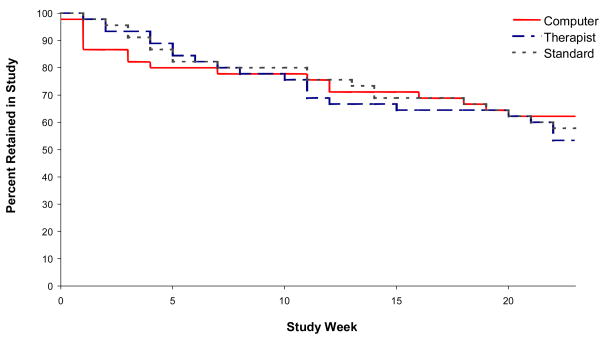
Treatment Retention
An average of 58%, 53%, and 62% of participants in the standard, therapist-delivered, and computer-assisted treatment conditions, respectively, were retained in treatment for the entire 23 weeks of the maintenance phase of treatment. The percentage of participants retained in treatment for the duration of maintenance treatment did not significantly differ across treatment conditions (χ2(2) = 0.73; p = .69). Survival estimates for each group, presented in Figure 3, were also not statistically significant across groups (logrank test χ2(2) = 0.38; p = .82).
Figure 3.
Retention by treatment condition during 23-week treatment maintenance phase.
Addiction Severity Index (ASI)
Composite scores on the Addiction Severity Index (ASI) at the time of treatment intake were highest on the scales measuring functioning in Employment (mean = 0.55; SEM = 0.04), Drug (mean = 0.38; SEM = 0.01), Legal (mean = 0.33; SEM = 0.03), and Psychiatric (mean = 0.30; SEM = 0.03); moderate on the scales for Family (mean = 0.20; SEM = 0.03) and Medical (mean = 0.18; SEM= 0.03), and lowest on the scale for Alcohol problems (mean = 0.06; SEM = 0.01). ASI composite scores were shown to significantly reduce from their intake levels during maintenance treatment (all p-values <.05), with the exception of the alcohol composite score, which was low at the time of treatment intake and remained low during the maintenance phase of treatment. There was no evidence of differential reductions in ASI composite scores across dosing groups (all p-values >.05).
The Helping Alliance Questionnaire-Patient Version
Scores on the Patient version of the Helping Alliance Questionnaire were high throughout maintenance treatment and did not significantly differ across the three treatment conditions (F (2,121) = 0.15; p = 0.86). Average scores across the first 12-weeks of maintenance were 4.74 (SEM = 0.05), 4.84 (SEM = 0.04), and 4.86 (SEM = 0.05) for standard, therapist-delivered CRA, and computer-assisted CRA treatments, respectively.
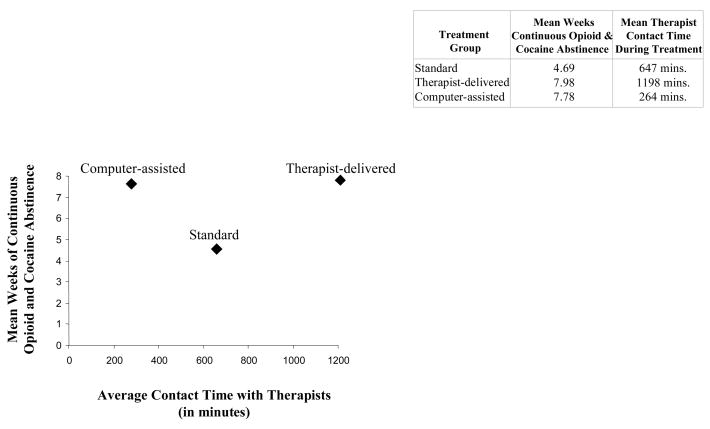
Patient-Therapist Contact Time
Participants in the therapist-delivered treatment condition spent an average of 1198 minutes (SEM = 91.6; 95% CI = 1012–1382) in therapy sessions with their counselor during the trial, while those in computer-assisted treatment condition spent an average of 264 minutes (SEM = 21.5; 95% CI = 221–308) and those in the standard treatment group spent an average of 647 minutes (SEM = 55.2; 95% CI = 536–758) in therapy sessions during the trial. As shown in Figure 4, participants in the computer-assisted treatment condition achieved a similar number of weeks of continuous opioid and cocaine abstinence as those in the therapist-delivered treatment condition, but with markedly reduced contact time with their counselor during the trial.
Figure 4.
Mean weeks of continuous opioid and cocaine abstinence plotted by mean contact time with therapist during treatment by treatment condition.
Discussion
This study, to our knowledge, was the first to evaluate an interactive, computer-delivered intervention theoretically grounded in the evidence-based community reinforcement approach (CRA) of behavioral therapy for individuals with opioid dependence. Results demonstrated that the exclusively therapist-delivered CRA plus vouchers intervention and the computer-assisted CRA plus vouchers intervention produced comparable levels of continuous opioid and cocaine abstinence among participants and markedly higher levels of abstinence than produced by the standard intervention. There are five points we would like to make about the study.
First, the results suggest that when computerized treatment for opioid dependence is integrated into other treatment components, treatment outcomes may be comparable to those achieved from exclusively therapist-delivered therapy. This finding is consistent with the literature on computerized therapy as developed in other contexts. Importantly, even though the two active CRA interventions produced comparable periods of sustained opioid and cocaine abstinence, the abstinence rates among those in the computer-assisted CRA condition were achieved even though only approximately one sixth of the intervention was delivered through a therapist and five sixths of the intervention was delivered by the interactive computer program. These results suggest that a computer-based program may enable more widespread dissemination of the evidence-based CRA plus vouchers intervention in a manner that is cost-effective and ensures fidelity.
Second, this less intensive and expensive computer-based intervention was more efficacious than standard treatment. In addition, the therapist-delivered treatment and the computer-assisted treatment did not produce any less therapeutic alliance between therapists and participants relative to the traditional counseling condition. This suggests, in turn, that treatment programs might be able to integrate computer-based counseling into existing care without jeopardizing clinically important alliances with therapeutic staff. Although this system was evaluated in a clinic setting in the present trial, it may be useful in providing evidence-based psychosocial treatment in a wide range of settings. For example, this system may be useful when accessed in the privacy of one’s home via secure Internet access or from the offices of health providers (such as physicians offering office-based buprenorphine treatment). Indeed, both the CRA and contingency management components of the intervention may be delivered online in light of recent research demonstrating that contingency management can be effectively conducted over the Internet (Dallery & Glenn, 2005). Finally, this program may be useful as a supplement to group therapy or as an alternative to group therapy for patients, which may be particularly important for patients with social anxiety or social phobias.
Third, one potential criticism of this study is that these treatments are all largely ineffective and therefore treatment differences are not meaningful. This concern may be addressed by comparing the results of this study with those of prior studies. The magnitude of treatment effects reported here replicates or exceeds those observed in prior reports of similar procedures with similar populations. For example, in this study the standard, therapist-delivered and computer-assisted treatment conditions achieved an average of 4.69, 7.98 and 7.78 weeks of continuous opioid and cocaine abstinence, respectively. Effect sizes observed for urine samples documented to be opioid and cocaine negative were of the same magnitude as those observed for our primary outcome measure of continuous opioid and cocaine abstinence. These secondary group comparisons did not achieve statistical significance; however, power calculations, which were performed prior to the study, were based on continuous abstinence. Other studies conducted with patients receiving buprenorphine or methadone report standard treatment resulted in approximately 2 to 4 weeks of continuous abstinence and the community reinforcement approach with contingency management procedures resulted in 4 to 5 weeks of continuous abstinence (e.g., Gross et al., 2006; Schottenfeld et al., 2005). Similarly, a recent meta-analysis of contingency management studies targeting cocaine and opioids reported a mean weighted effect size of .21 (95% CI = .05 to .36) compared to control conditions, while the effect size in the present study for the counselor and computer based treatments were 0.19 and 0.18, respectively, when compared to the standard treatment (Lussier, Heil, Mongeon, & Badger, 2006). Thus, treatment effectiveness as reported here is consistent with prior results.
Fourth, this study did not measure the independent contribution of computerized therapy given that it was provided in the context of treatment components with documented efficacy (e.g., buprenorphine and contingency management). Indeed, the uniformly high retention as well as attendance rates across all three treatments is likely, at least in part, a result of the buprenorphine (the common treatment element). We decided the first step in this new area of research was to examine whether comparable outcomes would be obtained when computerized CRA was substituted for therapist provided CRA and whether a combined treatment package was more efficacious than standard treatment. If the results had shown that the computerized treatment package was less effective than the therapist treatment package, then there would be little value in examining the independent effects of computerized treatment alone. Given the comparable efficacy of computerized and therapist delivered CRA packages established in the present study, we believe that the next step would be to isolate the effects of the computerized CRA as was done recently with therapist delivered CRA (in which both CRA and vouchers were shown to contribute to the overall efficacy of the treatment package (Higgins et al., 2003).
It is conceivable that some current treatment programs may wish to adopt a treatment package of computerized CRA and vouchers. Indeed, the cost savings from computerized CRA (relative to person-delivered CRA) may be used to support the cost of voucher-based incentives. By automating this treatment package, treatment programs may be provided with a means to readily provide this science-based treatment package with fidelity. However, our overall planned line of research, including future dismantling studies, will allow us to generate empirical data to inform approaches that may markedly improve the substance abuse treatment system (not just to fit into the current treatment system).
While it would have been interesting to have also directly assessed acquisition of skills during training on the computerized CRA modules in this study as well participants’ perceptions of the acceptability and utility of the intervention, the main focus of this study was to assess the efficacy of this computerized therapeutic tool on clinically meaningful outcome measures such as treatment retention and opioid abstinence. Thus, outcome measures were selected consistent with the primary focus of this clinical trial. Our prior work with computerized interventions has shown, however, that computer-based interventions, which use the informational technologies that we also employed in the present study, are highly acceptable and can promote significant gains in both knowledge and skills acquisition (e.g., Marsch & Bickel, 2004; Marsch, Bickel, & Grabinski, 2007; Marsch, Bickel, Grabinski, & Badger, 2007). Future evaluations could assess the specific knowledge and skills impacted by the computerized CRA package. Moreover, the primary focus of the present study was to assess the efficacy of the computerized CRA intervention during maintenance treatment for opioid dependence. Given the chronic, relapsing nature of opioid dependence and the need for ongoing maintenance treatment for many opioid-dependent individuals (e.g., Ball & Ross, 1991), outcomes during treatment are of clinical significance. Nonetheless, future evaluations should include follow-up data to examine post-treatment outcomes.
Fifth and finally, the computerization of some aspects of addiction treatment may also have other broader implications. Adoption of evidence-based research innovations permits addiction treatment programs to improve patient services and evolve while failing to adopt innovation may render treatment a static and less than optimally effective enterprise (Bickel & Marsch, 2007). Indeed, as McLellan and colleagues convincingly argue in a recent review of the numerous systemic problems that exist within the national addiction treatment infrastructure (McLellan et al., 2003), “without modernization and investment, the addiction treatment system will fail to meet the public’s needs”. Although informational technology continues to expand and bring about profound changes in our society in general, it has been infrequently employed in the addiction field. If computer and other informational technologies were routinely employed in the field, they might lead to not only cost-effective interventions but ultimately to more rapid diffusion and adoption of research findings. That is, if computer-delivered therapies that require minimal therapist involvement and are efficacious, then dissemination of new empirically supported treatments may be provided by simply sending computer programs to treatment providers. By reassigning some portions of addiction treatment for delivery by computer-based technology, evidence-based treatment may be routinely provided, the need to train counselors to deliver new therapies may be decreased, counselors may be permitted to focus on those aspects of treatment that they are uniquely suited to address and focus more on problematic clients with recurring drug use and/or crises, and treatment cost may be reduced. In order for such changes to occur, research must be conducted on how to computerize treatments and assess their efficacy. Thus, the present study not only provided a demonstration of the efficacy of computer-assisted therapy for opioid dependence, but also represents an initial step in bringing information technologies to bear on issues of substance abuse treatment.
Acknowledgments
This study was sponsored by grant #R01 DA 12997 from the National Institute on Drug Abuse, Bethesda, MD. We thank Mr. Michael Grabinski for his assistance with computer program design, Dr. Alan Budney for his comments on an earlier draft of this paper, and the medical and research staff at the University of Vermont Substance Abuse Treatment Center for their assistance with the conduct of this clinical trial. We also thank the Investigational Drug Pharmacy at Fletcher Allen Health Care for medication preparation. Portions of this research were presented at the “e-Therapy, Telehealth, Telepsychiatry and Beyond Conference” sponsored by the Substance Abuse and Mental Health Services Administration in December 2004, Rockville, MD; the annual meeting of the American Psychological Association in August 2003, Toronto, CA; the annual meeting of the College on Problems of Drug Dependence in June 2002, Quebec City, CA; and at an invited presentation at the White House Office of National Drug Control Policy in March 2003, Washington, D.C. In addition to having university roles, the first two authors are affiliated with HealthSim, Inc., the health-promotion software development organization that developed the fluency-based, Computer-Assisted Instruction (CAI) technology employed in the computer-based program evaluated in the present study. This educational technology is unique to HealthSim, Inc. and was included in the present project because it is an integral part of the computer-based program that was evaluated in the study. The authors have worked extensively with the University of Vermont’s Conflict of Interest Committee, Office of Sponsored Programs, as well as with the College of Medicine’s Associate Dean of Research and Academic Affairs to monitor the relationship between these two organizations, oversee all aspects of collaborative projects between the organizations, and ensure that no conflict exists between the authors’ roles in each organization. The analysis plan and results were reviewed by an independent statistician blind to treatment assignments.
References
- Abbott PJ, Weller SB, Delaney HD, Moore BA. Community reinforcement approach in the treatment of opiate addicts. American Journal of Drug and Alcohol Abuse. 1998;24:17–30. doi: 10.3109/00952999809001696. [DOI] [PubMed] [Google Scholar]
- Amass L, Bickel WK, Higgins ST, Badger GJ. Alternate day dosing during buprenorphine treatment of opioid dependence. Life Science. 1994;54(17):1215–1228. doi: 10.1016/0024-3205(94)00848-5. [DOI] [PubMed] [Google Scholar]
- Amass L, Bickel WK, Higgins ST, Hughes JR. A preliminary investigation of outcome following gradual or rapid buprenorphine detoxification. Journal of Addictive Diseases. 1994;13:33–45. doi: 10.1300/j069v13n03_04. [DOI] [PubMed] [Google Scholar]
- Ball JC, Ross A. The effectiveness of methadone maintenance treatment: Patients, programs, services, and outcomes. New York: Springer-Verlag; 1991. [Google Scholar]
- Bickel WK, Amass L. Buprenorphine treatment of opioid dependence: A review. Experimental and Clinical Psychopharmacology. 1995;3(4):477–489. [Google Scholar]
- Bickel WK, Amass L, Higgins ST, Badger GJ, Esch RA. Effects of adding behavioral treatment to opioid detoxification with buprenorphine. Journal of Consulting and Clinical Psychology. 1997;65(5):803–810. doi: 10.1037//0022-006x.65.5.803. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. A future for drug abuse prevention and treatment in the 21st century: Applications of computer-based information technologies. In: Henningfield J, Bickel WK, editors. Addiction Treatment: Science and Policy in the Twenty-First Century. Baltimore, MD: Johns Hopkins Press; 2007. pp. 35–43. [Google Scholar]
- Bickel WK, McLellan AT. Can management by outcome invigorate substance abuse treatment? The American Journal on Addictions. 1996;5:281–291. [Google Scholar]
- Budney AJ, Higgins ST. Therapy manuals for drug addiction, a community reinforcement plus vouchers approach: Treating cocaine addiction. Rockville, MD: National Institute on Drug Abuse; 1998. [Google Scholar]
- Buglione SA, Devito AJ, Mulloy JM. Traditional group therapy and computer- administered treatment for test anxiety. Anxiety, Stress & Coping. 1990;3(1):33 – 39. [Google Scholar]
- Burling TA, Seidner AL, Gaither DE. A computer-directed program for smoking cessation treatment. Journal of Substance Abuse. 1994;6:427–431. doi: 10.1016/s0899-3289(94)90362-x. [DOI] [PubMed] [Google Scholar]
- Carise D, Ozge GA, McLellan T, Dugosh K, Kendig C. Getting patients the services they need using a computer-assisted system for patient assessment and referral-CASPAR. Drug and Alcohol Dependence. 2005;80:177–189. doi: 10.1016/j.drugalcdep.2005.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr AC, Ghosh A, Marks IM. Computer-supervised exposure treatment for phobias. Canadian Journal of Psychiatry. 1988;33(2):112–117. doi: 10.1177/070674378803300208. [DOI] [PubMed] [Google Scholar]
- Curry SJ, McBride C, Grothaus LC, Louie D, Wagner EH. A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. Journal of Consulting and Clinical Psychology. 1995;63:1005–1014. doi: 10.1037//0022-006x.63.6.1005. [DOI] [PubMed] [Google Scholar]
- Dallery J, Glenn IM. Effects of an internet-based voucher reinforcement program for smoking abstinence: A feasibility study. Journal of Applied Behavior Analysis. 2005;38:349–357. doi: 10.1901/jaba.2005.150-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dede C, Fontana L. Transforming health education via new media. In: Harris L, editor. Health and the new media: Technologies transforming personal and public health. Mahwah, NJ: Lawrence Erlbaum Associates; 1995. pp. 163–184. [Google Scholar]
- Dijkstra A, DeVries H, Roijackers J. Long-term effectiveness of computer-generated tailored feedback in smoking cessation. Health Education Research: Theory & Practice. 1998;13:207–214. doi: 10.1093/her/13.2.207. [DOI] [PubMed] [Google Scholar]
- Gross A, Marsch LA, Badger GJ, Bickel WK. A comparison between low magnitude voucher and buprenorphine medication contingencies in promoting abstinence from opioids and cocaine. Experimental and Clinical Psychopharmacology. 2006;14(2):148–156. doi: 10.1037/1064-1297.14.2.148. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, Bosworth K, Chewning B, Hawkins RP. Computer-based health promotion: Combining technological advances with problem-solving techniques to effect successful health behavior changes. Annual Review of Public Health. 1987;8:387–415. doi: 10.1146/annurev.pu.08.050187.002131. [DOI] [PubMed] [Google Scholar]
- Hester RK, Delaney HD. Behavioral self-control program for Windows: Results of a controlled clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:686–693. doi: 10.1037//0022-006x.65.4.686. [DOI] [PubMed] [Google Scholar]
- Hester RK, Squires DD, Delaney HD. The drinker’s check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. Journal of Substance Abuse Treatment. 2005;28(2):159–169. doi: 10.1016/j.jsat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK. Achieving cocaine abstinence with a behavioral approach. American Journal of Psychiatry. 1993;150:763–769. doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg FE, Donham R, Badger GJ. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry. 1994;51(7):568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Delaney DD, et al. A behavioral approach to achieving initial cocaine abstinence. American Journal of Psychiatry. 1991;148(9):1218–1224. doi: 10.1176/ajp.148.9.1218. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Sigmon SC, Wong CJ, et al. Community reinforcement therapy for cocaine-dependent outpatients. Archives of General Psychiatry. 2003;60(10):1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- Himmelsbach CK. Studies of certain addiction characteristics of (a) dihydromorphone. Journal of Pharmacology and Experimental Therapeutics. 1939;67:239–249. [Google Scholar]
- Issenberg SB, Gordon MS, Gordon DL, Safford RE, Hart IR. Simulation and new learning technologies. Medical Teacher. 2001;23(1):16–23. doi: 10.1080/01421590020007324. [DOI] [PubMed] [Google Scholar]
- Kuhn MR, Stahl SA. Fluency: A review of developmental and remedial practices. Journal of Educational Psychology. 2003;95:3–21. [Google Scholar]
- Luborsky L, Barber JP, Siqueland L, Johnson S, Najavits LM, Frank A, et al. The revised helping alliance questionnaire (HAz-II) Journal of Psychotherapy Practice and Research. 1996;5:260–271. [PMC free article] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK. Efficacy of computer-based HIV/AIDS education for injection drug users. American Journal of Health Behavior. 2004;28(4):316–327. doi: 10.5993/ajhb.28.4.3. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK, Grabinski MJ. Application of interactive, computer technology to adolescent substance abuse prevention and treatment. In: Cohall AT, Rickert V, Ryan O, editors. Harnessing technology for adolescent health promotions. American Academy of Pediatrics; 2007. pp. 342–356. [PubMed] [Google Scholar]
- Marsch LA, Bickel WK, Grabinski MJ, Badger GJ. Applying computer technology to substance abuse prevention science: Results of a preliminary examination. Journal of Child and Adolescent Substance Abuse. 2007;16:69–97. [Google Scholar]
- McLellan AT, Carise D, Kleber HD. Can the national addiction treatment infrastructure support the public’s demand for quality care? Journal of Substance Abuse Treatment. 2003;25(2):117–121. [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, et al. New data from the Addiction Severity Index. Reliability and validity in three centers. Journal of Nervous and Mental Disorders. 1985;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- Murphy L, Mitchell DL. When writing helps to heal: e-mail as therapy. British Journal of Guidance & Counseling. 1998;26:21–32. [Google Scholar]
- Newman MG, Consoli S, Taylor CB. Computers in assessment and cognitive behavioral treatment of clinical disorders: Anxiety as a case in point. Behavior Therapy. 1997;28:211–235. [Google Scholar]
- Newman MG, Kenardy J, Herman S, Taylor CB. The use of hand-held computers as an adjunct to cognitive-behavior therapy. Computers in Human Behavior. 1996;12:135–143. [Google Scholar]
- Newman MG, Kenardy J, Herman S, Taylor CB. Comparison of palmtop-computer-assisted brief cognitive-behavioral treatment to cognitive-behavior treatment for panic disorder. Journal of Consulting and Clinical Psychology. 1997;65:178–183. doi: 10.1037//0022-006x.65.1.178. [DOI] [PubMed] [Google Scholar]
- North MM, North SM, Coble JR. Virtual reality therapy for fear of flying (letter) American Journal of Psychiatry. 1997;154:130. doi: 10.1176/ajp.154.1.130b. [DOI] [PubMed] [Google Scholar]
- Orlandi MA, Dozier CE, Marta MA. Computer-assisted strategies for substance abuse prevention: Opportunities and barriers. Journal of Consulting and Clinical Psychology. 1990;58:425–431. doi: 10.1037//0022-006x.58.4.425. [DOI] [PubMed] [Google Scholar]
- Osgood-Hynes DJ, Greist JH, Marks IM, Baer L, Heneman SW, Wenzel KW, et al. Self-administered psychotherapy for depression using a telephone-accessed computer system plus booklets: An open U.S.-U.K. study. Journal of Clinical Psychiatry. 1998;59:358–365. doi: 10.4088/jcp.v59n0704. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Guardagnoli E, Rossi JS. Patterns of change: Dynamic typology applied to smoking cessation. Multivariate Behavioral Research. 1991;26:83–107. doi: 10.1207/s15327906mbr2601_5. [DOI] [PubMed] [Google Scholar]
- Rafaeli S. Interactivity: From new media to communication. In: Hawkins RP, Wiemann JM, Pingree S, editors. Advancing communication science: Merging mass and interpersonal processes. Newbury Park, CA: Sage; 1988. pp. 110–134. [Google Scholar]
- Schneider SJ, Schwartz MD, Fast J. Computerized, telephone-based health promotion: I. Smoking cessation program. Computers in Human Behavior. 1995;11:135–148. [Google Scholar]
- Schneider SJ, Tooley J. Self-help computer conferencing. Computers and Biomedical Research. 1986;19:274–281. doi: 10.1016/0010-4809(86)90022-4. [DOI] [PubMed] [Google Scholar]
- Schottenfeld RS, Chawarski MC, Pakes JR, Pantalon MV, Carroll KM, Kosten TR. Methadone versus buprenorphine with contingency management or performance feedback for cocaine and opioid dependence. American Journal of Psychiatry. 2005;162:340–349. doi: 10.1176/appi.ajp.162.2.340. [DOI] [PubMed] [Google Scholar]
- Selmi PM, Klein MH, Greist JH, Sorrell SP, Erdman HP. Computer-administered cognitive-behavioral therapy for depression. American Journal of Psychiatry. 1990;147:51–56. doi: 10.1176/ajp.147.1.51. [DOI] [PubMed] [Google Scholar]
- Selmi PM, Klein MH, Greist JH, Sorrell SP, Erdman HP. Computer- administered therapy for depression. MD Computing. 1991;8(2):98–102. [PubMed] [Google Scholar]
- Steuer J. Defining virtual reality: Dimensions determining telepresence. Journal of Communication. 1992;42:73–93. [Google Scholar]
- Strecher VJ, Kreuter M, Den Boer DJ, Kobrin S, Hospers HJ, Skinner CS. The effects of computer-tailored smoking cessation messages in family practice settings. The Journal of Family Practice. 1994;39:262–270. [PubMed] [Google Scholar]
- Street RL, Rimal RN. Health promotion and interactive technology: A conceptual foundation. In: Street R, Gold WR, Manning T, editors. Health promotion and interactive technology: Theoretical applications and future directions. Mahwah, NJ: Lawrence Erlbaum Associates; 1997. pp. 1–18. [Google Scholar]
- Taylor CB, Luce KH. Computer- and internet-based psychotherapy interventions. Current directions in psychological science. 2003;12(1):18–22. [Google Scholar]
- Thorkildsen R, Bickel WK, Williams JG. A micro-computer video-disc CAI system fo rthe mentally retarded. Journal of Special Education Technology. 1979;1:45–51. [Google Scholar]
- Velicer WF, Prochaska JO, Bellis JM, DiClemente CC, Rossi JS, Fava JL, et al. An expert system intervention for smoking cessation. Addictive Behaviors. 1993;18:269–290. doi: 10.1016/0306-4603(93)90029-9. [DOI] [PubMed] [Google Scholar]
- Wantland DJ, Portillo CJ, Holzemer W, Slaughter R, McGhee EM. The effectiveness of web-based vs. non-web-based intervention: A meta-analysis of behavioral change outcomes. Journal of Medical Internet Research. 2004;6(4):e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]