Abstract
Erythropoietin (EPO) provides neuroprotection and neurorestoration after traumatic brain injury (TBI). The EPO doses used for treatment of TBI significantly increase hematocrit, which may affect the efficacy of EPO therapy for TBI. The aim of this study was to investigate whether normalization of hematocrit would affect EPO efficacy for treatment of TBI. Young adult male Wistar rats were randomly divided into 4 groups: 1) Sham group (n=6); 2) TBI + saline group (n=6); 3) TBI + EPO group (n=6); and 4) TBI + EPO + hemodilution group (n=7). TBI was induced by controlled cortical impact over the left parietal cortex. EPO (5,000 U/kg) or saline was administered intraperitoneally at days 1, 2, and 3 post injury. Neurological function was assessed using a modified neurological severity score (mNSS), footfault and the Morris water maze (MWM) tests. Animals were sacrificed 35 days after injury and brain sections stained for immunohistochemistry. Compared to the saline treatment, EPO treatment significantly reduced hippocampal cell loss, enhanced angiogenesis and neurogenesis in the injured cortex and hippocampus, and significantly improved sensorimotor functional outcome (lowered mNSS and foot faults) and spatial learning (MWM test). Normovolemic hemodilution effectively normalized the hematocrit and did not significantly affect the histological and functional outcome of EPO therapy for TBI. These data for the first time demonstrate that increased hematocrit does not affect therapeutic effects of EPO on histological and long-term functional outcomes in rats after TBI and also suggest that neuroprotection and neurorestoration of EPO treatment are independent of hematocrit.
Keywords: angiogenesis, erythropoietin, hemodilution, neurogenesis, traumatic brain injury
1. Introduction
Traumatic brain injury (TBI) is a common cause of mortality and morbidity worldwide, particularly among the young (Thurman and Guerrero, 1999) and may result in permanent functional deficits due to both primary and secondary injury mechanisms (Davis, 2000). The most prevalent and debilitating features in survivors of traumatic brain injury (TBI) are cognitive deficits and motor dysfunctions. To date, there is no effective treatment to promote functional recovery except for routine medical intervention and care (Narayan et al., 2002).
Erythropoietin (EPO) and the EPO receptor (EPOR), essential for erythropoiesis, are also expressed in the brain (Brines et al., 2000). While EPO and EPOR are only weakly expressed in normal adult brain, expression of EPO and EPOR is greatly increased in response to different types of brain injury (Grasso et al., 2004; Liao et al., 2008; Marti, 2004). Inhibition of EPO activity by the administration of soluble EPORs worsens the severity of neuronal injury (Sakanaka et al., 1998), suggesting that endogenous EPO is directly involved in an intrinsic neuronal repair pathway. EPO shows neuroprotection in animal models including stroke (Wang et al., 2004), spinal cord injury (Grasso et al., 2006), kainate-induced seizure activity (Brines et al., 2000), and autoimmune encephalomyelitis (Cerami, 2001; Zhang et al., 2005).
Recent work has shown that EPO provides substantial benefits in rats and mice after TBI (Brines et al., 2000; Cherian et al., 2007; Liao et al., 2008; Lu et al., 2005; Mahmood et al., 2007; Xiong et al., 2008). However, the EPO doses used for treatment significantly increased hematocrit (HCT) (Mahmood et al., 2007; Xiong et al., 2007). The concern is that increased HCT may pose potential adverse effects seen in the critically ill patients treated with EPO (Corwin et al., 2007). It is unclear whether normalization of HCT affects efficacy of EPO treatment for TBI in rats. Accordingly, using a controlled cortical impact TBI rat model, we investigated effects of normalization of HCT on EPO efficacy in terms of cortical and hippocampal injury, cell proliferation, neurogenesis, angiogenesis, long-term sensorimotor function and spatial learning recovery.
2. Results
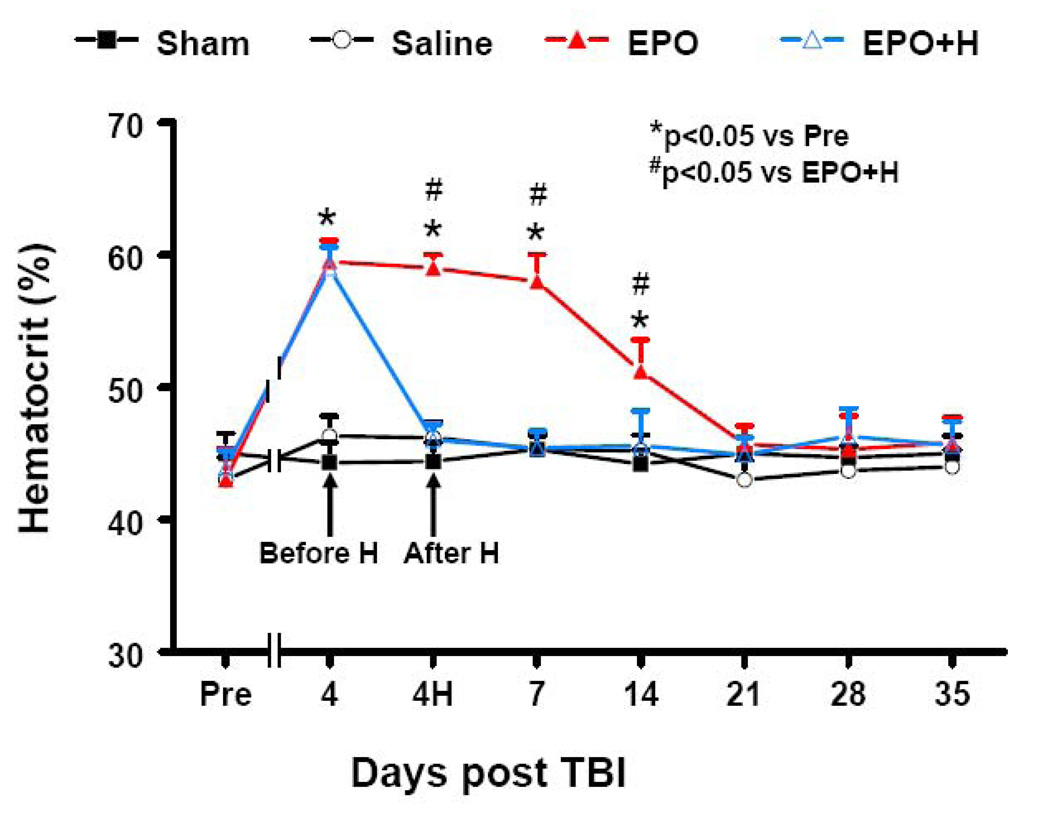
2.1. HCT
The baseline of HCT was similar for all animals before injury or sham-surgery (Fig. 1). Compared to preinjury levels, EPO treatment significantly increased HCT up to 2 weeks (P<0.05), which returned to normal thereafter. Normovolemic hemodilution at day 4 effectively reduced HCT from 59% to a normal level (45%).
Fig. 1.
Changes in hematocrit before and after EPO treatment. “Pre” represents preinjury level. Normovolemic hemodilution (H) was performed immediately after hematocrit measurement at day 4 post injury. H effectively reduced HCT to normal. Data represent mean ± SD. *P<0.05 vs. Pre (or Sham or Saline); # P<0.05 vs. EPO+H. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H).
2.2. Lesion volume
Rats were sacrificed at 35 days post TBI for histological measurements. EPO treatment and hemodilution did not affect the lesion volume after TBI (P>0.05). The lesion volume was 15.1±1.8%, 16.5±1.1%, and 15.8±1.5% for TBI rats treated with saline, EPO and EPO + hemodilution, respectively.
2.3. Spatial learning test
The modified Morris water maze (MWM) protocol in the present study was used to detect spatial learning deficits. To analyze day-by-day differences in the MWM, a repeated measures ANOVA was performed followed by Student-Newman-Keuls (SNK) tests for multiple comparisons. As shown in Fig. 2A, the time spent in the correct quadrant (Northeast, NE) by non-injured rats gradually increased 25% at day 31 to 50% at day 35 after sham surgery. The saline-treated rats with TBI were impaired relative to sham-operated rats at days 32–35 (P<0.05). However, compared to saline treatment, EPO-treated rats with TBI showed significant improvement at days 33–35 (P<0.05). Hemodilution did not affect the spatial learning performance compared to the EPO treatment alone (P>0.05).
Fig. 2.
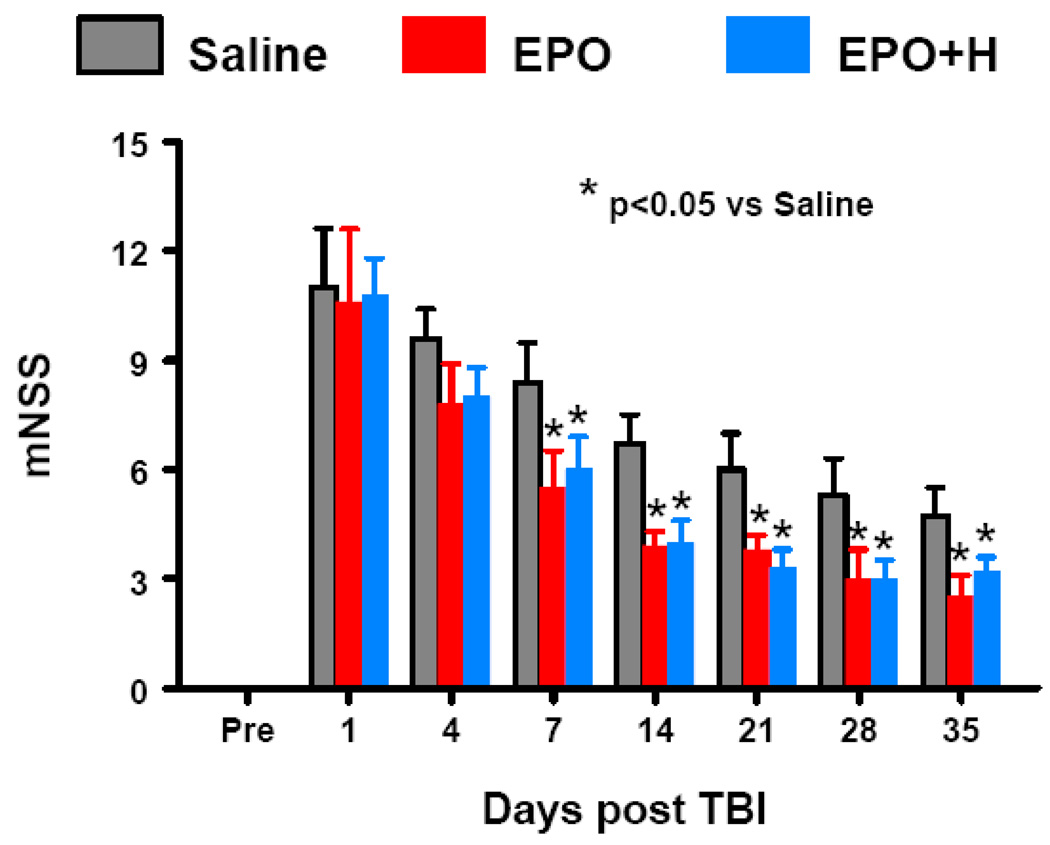
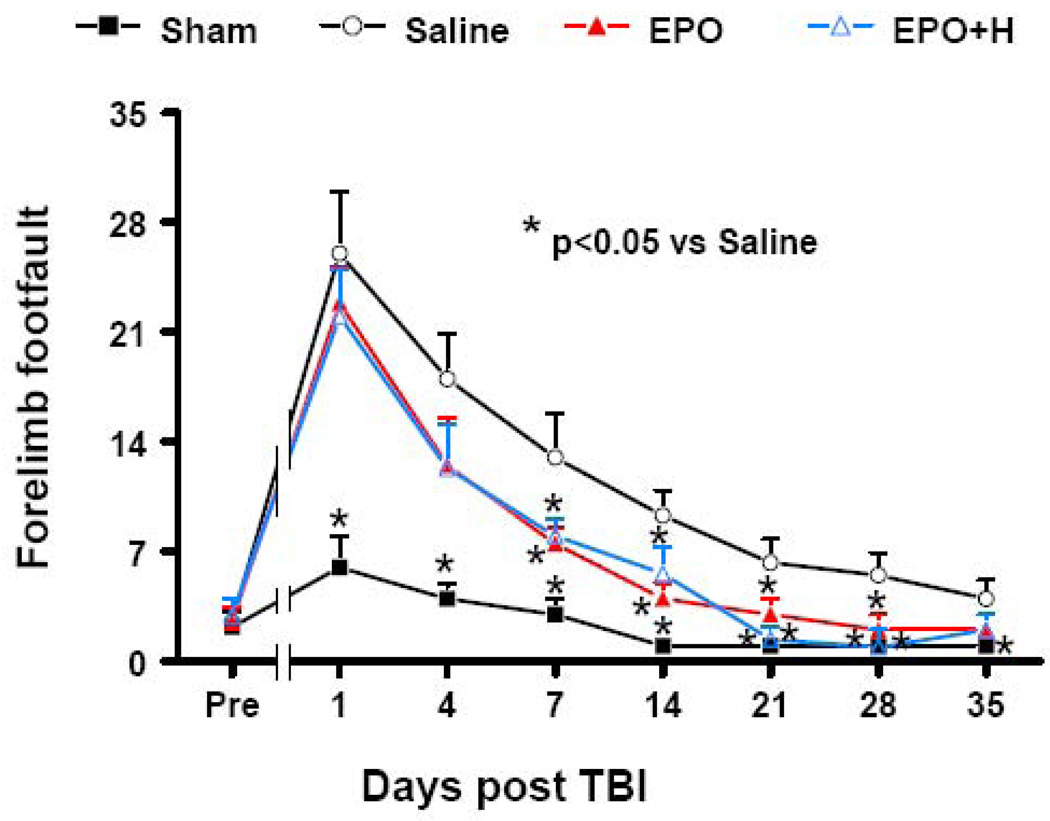
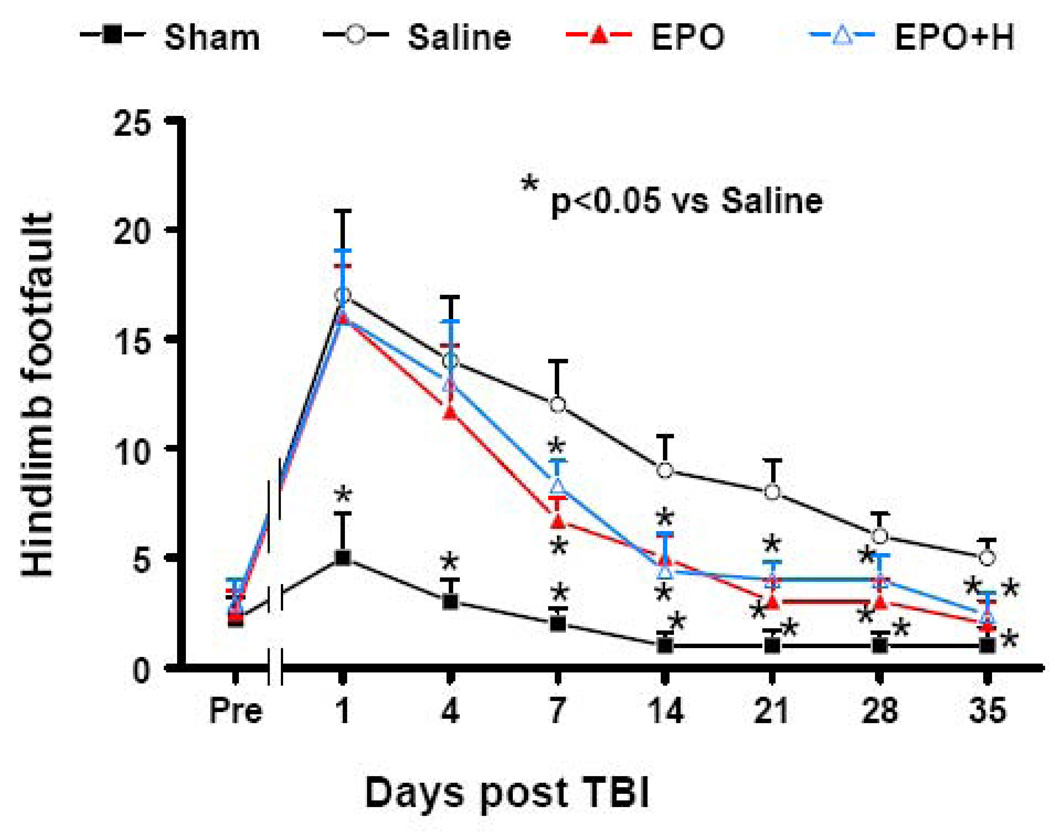
Graphs. A: Effect of EPO on spatial learning function 31–35 days after TBI. Delayed treatment with EPO (both EPO and EPO+H groups) improves spatial learning performance measured by a recent version of the water maze test at days 33–35 compared with the saline group (P<0.05). Hemodilution did not affect the spatial learning performance compared to EPO alone group. Data represent mean ± SD. * P<0.05 vs. Saline group. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). B: Effect of EPO on sensorimotor function (forelimb footfault) before and after TBI. “Pre” represents pre-injury level. Delayed EPO treatment significantly reduces forelimb foot faults at days 7–28 compared with the saline group (P<0.05). Hemodilution did not affect forelimb footfaults compared to EPO alone group. Data represent mean ± SD. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). C: Effect of EPO on sensorimotor function (hindlimb footfault) before and after TBI. “Pre” represents pre-injury level. Delayed EPO treatment significantly reduces hindlimb foot faults at days 7–21 compared with the saline group (P<0.05). Hemodilution did not affect hindlimb footfaults compared to EPO alone group. Data represent mean ± SD. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). D: The bar graph shows the functional improvement detected on the modified neurological severity scores (mNSS). EPO treatment significantly lowers mNSS scores at days 7–35 compared to saline group (P<0.05). Hemodilution did not affect mNSS scores ompared to EPO alone group. Data represent mean ± SD. N = 6 (Saline); 6 (EPO); 7 (EPO+H).
2.4. Footfault test
The incidence of forelimb footfaults during baseline (preoperatively) was about 5% (Fig. 2B). TBI significantly increased the occurrence of right forelimb footfaults contralateral to the TBI at 1 to 35 days postinjury compared with the pre-injury baseline. TBI significantly increased the incidence of contralateral forelimb footfaults at 1 to 35 days post-injury. Treatment with EPO significantly reduced the number of contralateral forelimb footfaults at 7 to 28 days after TBI compared to treatment with saline (P<0.05). Hemodilution did not affect the forelimb footfaults compared to the EPO treatment alone (P>0.05).
Similar results were found for the contralateral hindlimb (Fig. 2C). As compared to preinjury baseline, TBI significantly increased the incidence of contralateral hindlimb footfaults at 1 to 35 days post-injury. Treatment with EPO significantly reduced the number of contralateral hindlimb footfaults 7 to 35 days postinjury compared to treatment with saline (P<0.05). Hemodilution did not significantly alter the hindlimb footfaults compared to the EPO therapy alone (P>0.05).
2.5. Neurological severity score (mNSS)
Fig. 2D shows that mNSS score was significantly reduced in both EPO and EPO + hemodilution groups at days 7–35 post TBI compared to saline controls (P<0.05). However, hemodilution did not significantly affect mNSS score compared to the EPO therapy alone (P>0.05).
2.6. Cell loss in the CA3 and DG
When examined at 35 days post TBI (Fig. 3), the neuron counts in the ipsilateral CA3 and DG had significantly decreased (Fig. 3b and 3f, P<0.05) compared to sham controls (Fig. 3a and 3e). Compared to saline controls, EPO treatment with or without hemodilution significantly increased the neuron counts in the CA3 and DG (P<0.05). Hemodilution slightly reduced the cell number in the DG but this reduction did not reach a significance compared to the EPO therapy alone (P>0.05).
Fig. 3.
Effect of EPO on cell loss in the ipsilateral DG and CA3 region at 35 days after TBI. H&E staining: a–h. Delayed treatment with EPO (c, g) and EPO+H (d, h) significantly reduced cell loss as compared with the saline group (b, f) (P<0.05). The cell number in the DG and CA3 region is shown in (i). Hemodilution did not affect cell loss compared to EPO alone group. * P<0.05 vs. corresponding sham. # P<0.05 vs. the saline group. Data represent mean ± SD. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). Scale bar = 50 µm (a).
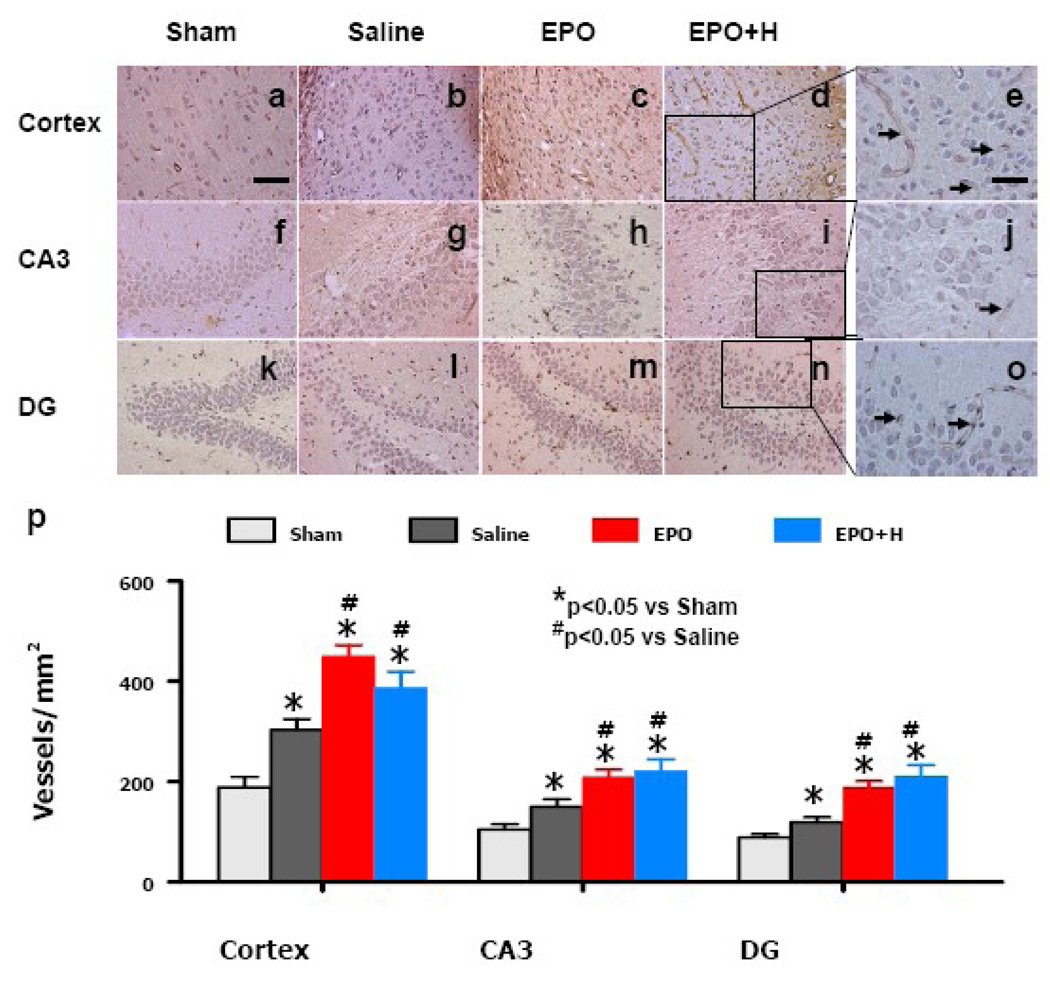
2.7. Angiogenesis
von Willebrand factor (vWF)-staining has been used to identify vascular structure in the brain after TBI (Xiong et al., 2007). TBI alone significantly increased the density of vWF-positive vessels in the injured cortex, ipsilateral CA3 and DG compared to sham controls (Fig. 4, P<0.05). EPO treatment significantly increased the vascular density in these regions compared to saline treatment (Fig. 4, P<0.05). There is no significant difference in the vascular density between the EPO alone and EPO + hemodilution groups.
Fig. 4.
Effect of EPO on vWF-staining vascular structure in the ipsilateral cortex, DG and CA3 region 35 days after TBI. TBI alone (b, g, i) significantly increased the vascular density in these regions compared to sham controls (P<0.05). EPO treatment (EPO and EPO+H) further enhanced angiogenesis after TBI compared to saline groups (P<0.05). Hemodilution did not affect vascular density compared to EPO alone group. The density of vWF-stained vasculature is shown in (p). Data represent mean ± SD. * P<0.05 vs. Sham. #P<0.05 vs. the saline group. Data represent mean ± SD. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). Scale bar = 50 µm (a); 25 µm (e).
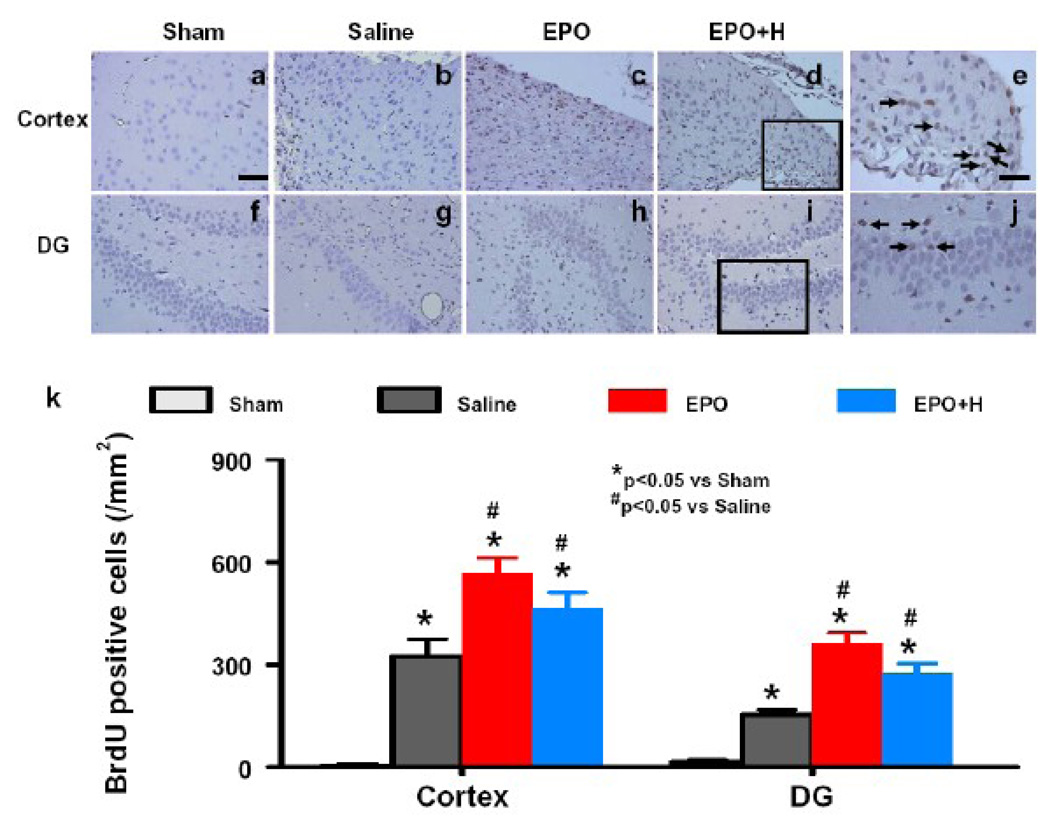
2.8. Cell proliferation
5-Bromo-2’-deoxyuridine (BrdU, an analog of thymidine), is widely used to detect proliferating cells in living tissues (Lu et al., 2005). BrdU can be incorporated into the newly synthesized DNA of replicating cells during the S phase of the cell cycle, substituting for thymidine during DNA replication. The number of BrdU-positive cells found in the ipsilateral cortex and DG was significantly increased at 35 days after TBI, compared with sham controls (Fig. 5, P<0.05). However, EPO treatment with or without hemodilution further increased the number of BrdU-positive cells in these regions after TBI compared to saline controls (P<0.05). There is no significant difference in the cell proliferation between the EPO alone and EPO + hemodilution groups.
Fig. 5.
Effect of EPO on BrdU-positive cells in the ipsilateral cortex and DG 35 days after TBI. The cells with BrdU (brown stained) that clearly localized to the nucleus (hematoxylin stained) were counted as BrdU-positive cells (arrows in e and j). TBI alone (b, g) significantly increased the number of BrdU-positive cells in the ipsilateral cortex and DG compared to sham controls (P<0.05). EPO treatment (EPO and EPO+H) significantly increased the number of BrdU-positive cells in these regions (c, d, h, i) compared to saline groups (P<0.05). The number of BrdU-positive cells is shown in (k). Data represent mean ± SD. *P< 0.05 vs. Sham. #P< 0.05 vs. the saline group. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). Scale bar = 50 µm (a); 25 µm (e).
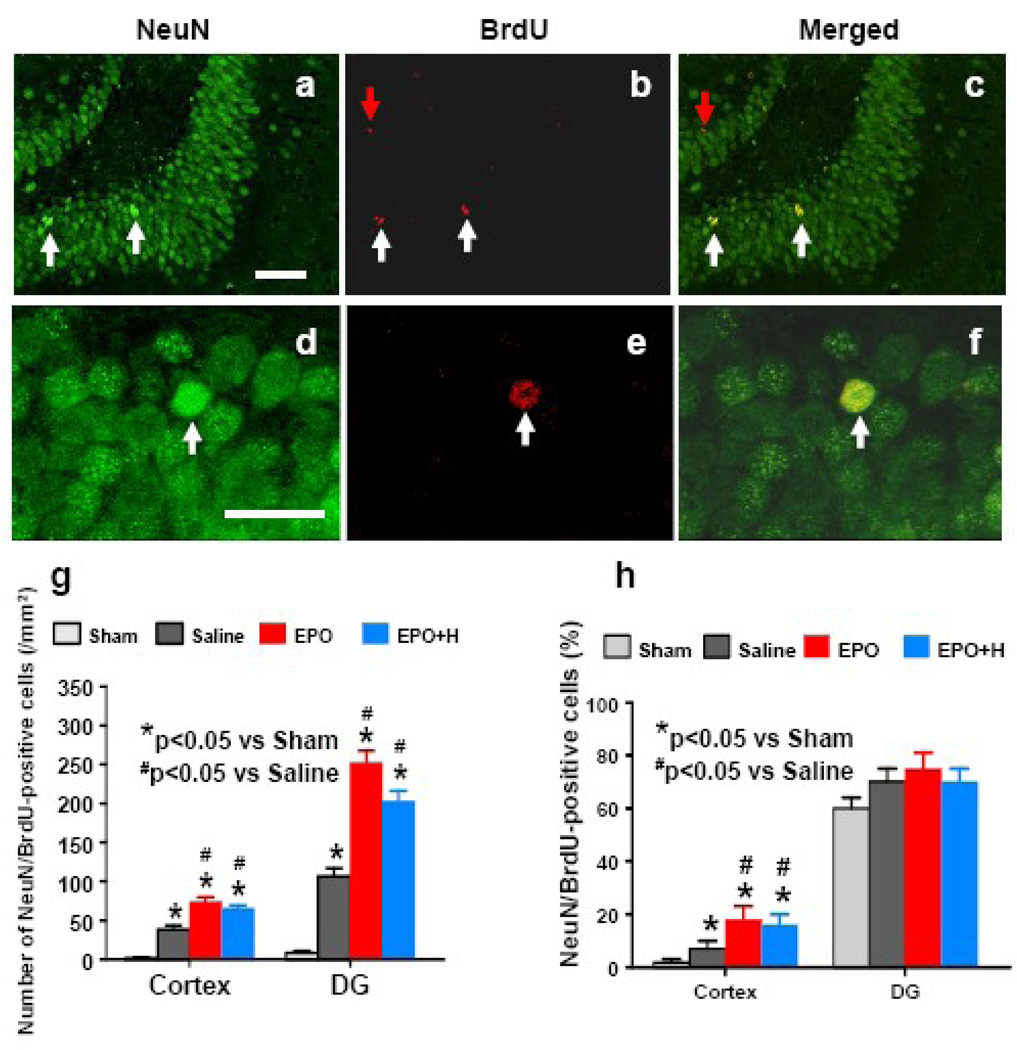
2.9. Neurogenesis
Newly generated neurons were identified by double labeling for BrdU (proliferating marker) and NeuN (neuronal nuclei, mature neuronal marker). TBI significantly increased the number of NeuN/BrdU-colabeled cells (newborn neurons) in the injured cortex and DG after compared to sham controls (Fig. 6g, P<0.05). EPO treatment significantly increased the number of newborn neurons in the injured cortex and DG (Fig. 6g, P<0.05) compared to saline controls. Hemodilution slightly reduced the number of newborn neurons in the injured cortex and DG without a significant difference (P>0.05). EPO treatment significantly increased the percentage of NeuN/BrdU-colabeled cells in the injured cortex (Fig. 6h, P<0.05) compared to saline controls. However, there is no significant difference in the percentage of newborn neurons in the DG among sham, saline-, EPO−, and EPO + hemodilution-treated groups (Fig. 6h).
Fig. 6.
Double fluorescent staining for NeuN (green) and BrdU (red) to identify newborn neurons (yellow after merge) in the injured brain at 35 days after TBI. Newborn BrdU-positive cells in the DG (red, band e) differentiate into neurons expressing NeuN (yellow, c and f). The total number and percentage of NeuN/BrdU-colabeled cells in the ipsilateral cortex and DG are shown in (g) and (h), respectively. Data represent mean ± SD. *P<0.05 vs. corresponding sham. #P<0.05 vs. the saline group. N = 6 (Sham); 6 (Saline); 6 (EPO); 7 (EPO+H). Scale bars = 50 µm (a); 25 µm (d).
3. Discussion
Delayed EPO treatment provides substantial benefits in terms of reducing hippocampal cell loss, increasing ipsilateral cortical and hippocampal angiogenesis and neurogenesis, and improving spatial learning and sensorimotor functional recovery after TBI in rats. EPO therapy significantly increases HCT; normovolemic hemodilution effectively reduces HCT to normal. To the best of our knowledge, the present study for the first time demonstrates that normalization of HCT does not affect therapeutic effects of EPO on treatment for TBI in rats and also suggests that therapeutic effects of EPO is independent of increased hematocrit.
Our previous studies have shown that early (6 h) EPO therapy does not affect angiogenesis in mice after TBI (Xiong et al., 2008) but delayed (24 h) EPO treatment significantly enhances angiogenesis after stroke in rats (Wang et al., 2004). Our present study demonstrates that delayed EPO treatment increases angiogenesis in the ipsilateral hippocampus and cortex in rats after TBI. In adult mammal brains, neurogenesis in the subgranular zone of the DG and subventricular zone (SVZ) takes place within an angiogenic microenvironment, where neurogenesis and angiogenesis are highly coupled and they work together to promote brain remodeling and subsequent improvement of neurological functional after brain injury (Zhang and Chopp, 2009). Our present study supports the coupling of angiogenesis and neurogenesis, which is shown by the increased number of NeuN/BrdU-positive cells in the injured cortex and hippocampus where angiogenesis is also enhanced after TBI. Delayed EPO treatment further increased angiogenesis and neurogenesis. EPO significantly increased the total number and percentage of newborn neurons found in the injured cortex, suggesting that neuroblasts may migrate from the SVZ into the injured cortex, where some of the SVZ-derived neuroblasts differentiate into mature neurons (Goings et al., 2004; Sundholm-Peters et al., 2005; Zhang et al., 2004; Zhang et al., 2008; Zhang et al., 2009). Although EPO therapy significantly increased the total number of newborn neurons in the DG, it did not affect the percentage (approximately 80%) of newborn neurons, suggesting that most of the BrdU-positive cells in the DG differentiate into granule neurons. This finding is in agreement with the report that the majority of BrdU-positive cells in the DG become granule neurons after TBI and these newborn neurons exhibit extensive anatomical integration into the CA3 region at the time cognitive recovery is observed (Sun et al., 2007). Our present data suggest that EPO-induced cell survival and neurogenesis may participate in functional recovery such as spatial learning (MWM test) and sensorimotor function (lowered mNSS and footfault).
EPO has been successfully used in clinical practice for more than two decades mainly to treat anemia in patients with chronic kidney disease (Wish, 2009) and chemotherapy (Milano and Schneider, 2007). Although insufficient information exists to accurately predict the association between EPO treatment and adverse side effects, results of clinical trials suggest that higher doses of EPO are more likely to be associated with adverse side effects. Several clinical trials with EPO in cancer patients were terminated following increased symptomatic or fatal thrombosis (Leyland-Jones, 2003; Rosenzweig et al., 2004). However, cancer patients who receive chemotherapy administered via catheters have a markedly increased risk for thrombosis (Henke et al., 2003).
More recently, long-term high-dose EPO treatment in patients with multiple sclerosis was found to be safe and well tolerated without adverse effects even when the hemoglobin increased by 20% (Ehrenreich et al., 2007). No safety concerns were identified among stroke patients treated with EPO (33,000 U, administered once daily for 3 days after stroke), who showed an improvement in neurological outcome (Ehrenreich et al., 2002). EPO administered subcutaneously three times a week (150 U/kg) or once a week (40,000 U/subject) for 4 weeks in healthy humans with HCT increased by 23% was well tolerated and no serious adverse events occurred (Cheung et al., 2001). In the present study, EPO treatment increases HCT by 30% at Days 4–7, by 13% at day 14 and HCT returns to normal at day 21 post TBI. Our present data show that the increased HCT does not change the efficacy of EPO for treatment of TBI in rats. This is in agreement with our previous studies that long-term EPO therapy improves functional outcomes without obvious side effects seen in rats after stroke (7-day treatment) (Wang et al., 2004) and TBI (14-day treatment) (Lu et al., 2005). A recent study demonstrates that a raised HCT after EPO treatment is not associated with an increased risk for thrombosis because endothelial nitric oxide production serves as a compensatory mechanism (Lindenblatt et al., 2007). A transgenic mouse line (tg6) that reaches an HCT concentration of 0.85 due to constitutive overexpression of human EPO did not show thrombembolic complications in all investigated organs at any age (Shibata et al., 2003). Although the evidence above indicates EPO therapy is well tolerated in animals and humans, Corwin et al reported that treatment with EPO is associated with an increase in the incidence of thrombotic events in the critically ill patients (Corwin et al., 2007). However, EPO may reduce mortality in patients with trauma and did not increase in the incidence of thrombotic events when prophylactic heparin was used (Corwin et al., 2007). The limitation of the present study is that it only focused on whether increased HCT induced by EPO would affect the therapeutic benefits for treatment of TBI in rats and other potential side effects were not studied in this study.
Management of TBI patients, after the primary insult, focuses on avoiding secondary brain injury from factors such as hypoxia, hypotension, and anemia (Jeremitsky et al., 2003). Anemia is associated with adverse outcomes in patients with TBI; however, blood transfusion to correct the anemia does not appear to improve outcomes (Carlson et al., 2006; Salim et al., 2008). The reason remains unclear. Our present study that increased HCT does not affect functional outcomes after EPO therapy in TBI rats, also suggests that blood transfusion alone may not effectively improve outcomes. Nearly all phase II/III clinical trials in neuroprotection have failed to show any consistent improvement in outcome for TBI patients (Narayan et al., 2002). The disappointing clinical phase-III trials may be due to heterogeneity of the population of TBI patients and variability in treatment approaches. Another important aspect is that TBI evokes many different pathophysiologic cascades leading to secondary injury. Brain mitochondrial dysfunction is one of the pathophysiological events after TBI in animals (Gilmer et al., 2009; Robertson et al., 2009; Xiong et al., 1997) and patients (Verweij et al., 2000). Mitochondria play a critical role in important cellular functions including energy production, apoptosis, and calcium regulation (Robertson et al., 2009; Sullivan et al., 2002). If normal mitochondrial function is impaired, a simple increase of oxygen supply and glucose by blood transfusion will not translate effectively into therapeutic efficacy. Our recent study shows that EPO treatment is capable of improving mitochondrial function in TBI rats, which may promote cellular energy generation and cell survival (Xiong et al., 2009). In addition to improving mitochondrial function, EPO treatment provides therapeutic benefits through angiogenesis, neurogenesis, synaptogenesis, anti-apoptosis, anti-oxidation, anti-inflammation and axonal regeneration after brain injury (Brines et al., 2000; Cherian et al., 2007; Grasso et al., 2007; Li et al., 2007; Liao et al., 2008; Lu et al., 2005; Mahmood et al., 2007; Wang et al., 2004; Xiong et al., 2008; Zhang et al., 2005), all of which appear independent of increased HCT. EPO treatment reduces lesion volume and improves functional recovery when administered within 6 h after experimental TBI (Brines et al., 2000; Cherian et al., 2007) or stroke (Wang et al., 2004). Changes in lesion volume after a cortical controlled impact injury are often used to imply recovery of function. However, delayed EPO therapy without reduction of lesion is capable of improving functional recovery through restorative effects including angiogenesis, neurogenesis, and synaptogenesis (Lu et al., 2005; Wang et al., 2004; Zhang and Chopp 2009). Therefore, EPO provides both neuroprotection (early therapy) and neurorestoration (delayed therapy).
In conclusion, in addition to the routine management of TBI patients, exploration of other potential therapies with neuroprotection and neurorestoration are warranted. In light of the positive outcome in using EPO to treat stroke in a recent small clinical trial (Ehrenreich et al., 2002) and our findings that EPO improves long-term histological outcome, sensorimotor function and spatial learning recovery, EPO is a promising neuroprotective and neurorestorative agent for TBI which warrants further investigation.
4. Experimental procedures
4.1. TBI Model
All experimental procedures were approved by the Institutional Animal Care and Use Committee (IACUC) of Henry Ford Health System.
A controlled cortical impact (CCI) model of TBI in the rat was utilized for the present study (Dixon et al., 1991; Mahmood et al., 2004). Young adult male Wistar rats (300–400 g) were anesthetized intraperitoneally with 350 mg/kg/body weight chloral hydrate. Rectal temperature was kept at 37 °C with a feedback-regulated water-heating pad. A controlled cortical impact device was used to induce the injury. Rats were placed in a stereotactic frame. Two 10-mm diameter craniotomies were performed adjacent to the central suture, midway between lambda and bregma. The second craniotomy allowed for movement of cortical tissue laterally. The dura was kept intact over the cortex. Injury was delivered by impacting the left cortex (ipsilateral cortex) with a pneumatic piston containing a 6-mm diameter tip at a rate of 4 m/s and 2.5 mm of compression. Velocity was measured with a linear velocity displacement transducer.
4.2. Experimental Groups and Treatment
Young adult male Wistar rats were randomly divided into 4 groups: 1) Sham group (n=6); 2) TBI + Saline group (n=6); 3) TBI + EPO group (n=6); and 4) TBI + EPO + hemodilution group (n=7). TBI was induced by controlled cortical impact over the left parietal cortex. Sham rats underwent surgery without injury. EPO at a dose of 5000 U/kg body weight (Epoetin alpha, AMGEN, Thousand Oaks, CA) was administered intraperitoneally (i.p.) at days 1, 2 and 3 after TBI. Animals in the saline-treated group received an equal volume of saline at days 1, 2 and 3 after surgery. For labeling proliferating cells, BrdU (100 mg/kg; Sigma, St. Louis, MO) was injected i.p. into rats daily for 10 days, starting 1 day after TBI. All rats were sacrificed at 35 days after TBI or surgery.
4.3. HCT
To determine the effects of EPO on HCT, a blood sample (50 µl) was collected via tail vein before injury, at day 4 and weekly after TBI or sham up to 5 weeks. HCT was measured in micro-HCT capillary tubes (Fisher Scientific, Pittsburgh, PA) using standard procedures (Readacrit Centrifuge, Clay Adams, Parsippany, NJ) (Xiong et al., 2007).
4.4. Normovolemic hemodilution
Under anesthetization with chloral hydrate, TBI or sham rats (day 4 post injury or sham-surgery) underwent cannulation of the left femoral artery with polyethylene catheter. To reach normal HCT target, the volume (V) of blood to be removed was calculated as follows (Ge et al., 2007): V = EBV × (Hi-Hf)/Hav, where EBV is the estimated blood volume (70 ml/kg), Hi is the initial HCT (59% in the present study), Hf is the final HCT (45% in the present study) after hemodilution. Hav is the mean HCT (mean of Hi and Hf). Withdrawal of a certain amount (V) of arterial blood was followed by immediate replacement with the same volume of normal saline (warmed to 37 °C). Normal saline is chosen, as it is commonly used clinically in the resuscitation of patients with multiple trauma (Li et al., 2006). During the experiment, a heating pad was used to maintain the temperature of rats at about 37 °C. Animals in the sham or saline or EPO alone groups underwent left femoral cannulation without hemodilution.
4.5. MWM test
All functional tests were performed by investigators blinded to the treatment status.
To detect spatial learning impairments, a recent version of the MWM test was used (Choi et al., 2006). The procedure was modified from previous versions (Morris, 1984) and has been found to be useful for chronic spatial memory assessment in rats and mice with brain injury (Choi et al., 2006; Lu et al., 2005). All animals were tested during the last five days (i.e., from 31–35 days after TBI or surgery) before sacrifice. Data collection was automated by the HVS Image 2020 Plus Tracking System (US HVS Image, San Diego, CA.). For data collection, a blue pool (1.8 m in diameter) was subdivided into four equal quadrants formed by imaging lines. The pool was located in a large test room, where there were many clues external to the maze (e.g., pictures, lamps); these were visible from the pool and presumably used by the rats for spatial orientation. The position of the cues remained unchanged throughout the task. At the start of a trial, the rat was placed randomly at one of four fixed starting points, facing toward the wall (designated North, South, East and West) and allowed to swim for 90 seconds or until they found the platform within 90 seconds. If the animal found the platform, it was allowed to remain on it for 10 seconds. If the animal failed to find the platform within 90 seconds, it was placed on the platform for 10 seconds. Throughout the test period the platform was located in the NE quadrant 2 cm below water in a randomly changing position, including locations against the wall, toward the middle of the pool or off-center but always within the target quadrant. If the animal was unable to find the platform within 90 sec, the trial was terminated and a maximum score of 90 seconds was assigned. If the animal reached the platform within 90 seconds, the percentage of time traveled within the NE (correct) quadrant was calculated relative to the total amount of time spent swimming before reaching the platform and employed for statistical analysis. The advantage of this version of the water maze is that each trial takes on the key characteristics of a probe trial because the platform is not in a fixed location within the target quadrant (Schallert, 2006).
4.6. Footfault test
To evaluate sensorimotor function, the footfault test was carried out before TBI and at 1, 4, 7, 14, 21, 28 and 35 days after TBI or surgery. The rats were allowed to walk on a grid (Xiong et al., 2007). With each weight-bearing step, a paw might fall or slip between the wires and, if this occurred, it was recorded as a footfault. A total of 50 steps were recorded for each right forelimb and hindlimb.
4.7. Modified neurological test
Neurological functional measurement was performed using the mNSS score test (Chen et al., 2001). The test was carried out on all rats preinjury and on days 1, 4, 7, 14, 21, 28, and 35 after TBI. The mNSS is a composite of the motor (muscle status, abnormal movement), sensory (visual, tactile and proprioceptive) and reflex tests and has been employed in previous studies (Lu et al., 2007a). In this TBI model, injury in the left hemispheric cortex of rats causes sensory and motor functional deficiency with elevated scores on motor, sensory, and Beam Balance Tests in the early phase after injury (day 1 after injury). Absent reflexes and abnormal movements can be measured on rats with severe injury. Slow recovery in asymmetry deficiency as reflected by Beam Balance Test results has been reported in unilateral brain injuries (Lu et al., 2007a). The mNSS score test is suitable for evaluating long-term neurological function after unilateral brain injury.
4.8. Tissue preparation and measurement of lesion volume
At day 35 after TBI, rats were anesthetized i.p. with chloral hydrate, and perfused transcardially first with saline solution, followed by 4% paraformaldehyde in 0.1 M phosphate buffered saline (PBS), pH 7.4. Their brains were removed and post-fixed in 4% paraformaldehyde for 2 days at room temperature. The brain tissue was cut into 7 equally spaced (1 mm) coronal blocks, and processed for paraffin sectioning. A series of adjacent 6-µm thick sections were cut from each block in the coronal plane and stained with hematoxylin and eosin (H&E). For lesion volume measurement, the 7 brain sections were traced by a microcomputer imaging device (MCID) (Imaging Research, St. Catharine’s, Ontario, Canada), as previously described (Chen et al., 2005). The indirect lesion area was calculated (i.e., the intact area of the ipsilateral hemisphere is subtracted from the area of the contralateral hemisphere) (Swanson et al., 1990), and the lesion volume presented as a volume percentage of the lesion compared with the contralateral hemisphere. H&E sections from Block E and F containing hippocampus were used to acquire images of the DG at 20 X magnification. To evaluate the cell loss after TBI, we counted the cell number per mm in the DG.
4.9. Immunohistochemistry
To examine the effect of EPO on cell proliferation and angiogenesis, coronal sections were histochemically stained with mouse anti-BrdU and rabbit anti-human vWF (Lu et al., 2005), respectively. For BrdU detection, paraffin-embedded coronal sections (6 µm) were deparaffinized and rehydrated. Antigen retrieval was performed by boiling sections in 10 mM citrate buffer (pH 6.0) for 10 min (Chen et al., 2001). After washing with PBS, sections were incubated with 0.3 % H2O2 in PBS for 10 min, blocked with 1 % BSA containing 0.3 % Triton-X 100 for 1 h at room temperature, and incubated with mouse anti-BrdU (1:200; Dako, Carpinteria, CA) at 4 °C overnight. After washing, sections were incubated with biotinylated anti-mouse antibody (1:200; Vector Laboratories, Inc., Burlingame, CA) at room temperature for 30 min. After washing, sections were incubated with an avidin-biotin-peroxidase system (ABC kit, Vector Laboratories, Inc., Burlingame, CA). Diaminobenzidine (Sigma, St. Louis, MO) was then used as a sensitive chromogen for light microscopy. Sections were counterstained with hematoxylin.
To identify vascular structure, brain sections were deparaffinized and then incubated with 0.4% Pepsin solution at 37 °C for 1 h. After washing, the sections were blocked with 1% BSA at room temperature for 1 h, and then incubated with rabbit anti-human vWF (1:200; DakoCytomation, Carpinteria, CA) at 4°C overnight. After washing, sections were incubated with biotinylated anti-rabbit antibody (1:200; Vector Laboratories, Inc., Burlingame, CA) at room temperature for 30 min. The subsequent procedures were the same as for BrdU staining.
BrdU-positive cells and vWF-stained vascular structures in the hippocampus and the cortex of both contralateral and ipsilateral hemispheres were examined at a magnification of 20 and counted.
4.10. Immunofluorescent staining
Newly generated neurons were identified by double labeling for BrdU and NeuN. After dehydration, tissue sections were boiled in 10 mM citric acid buffer (pH 6) for 10 min. After washing with PBS, sections were incubated in 2.4 N HCl at 37 °C for 20 min. Sections were incubated with 1% BSA containing 0.3% Triton-X-100 in PBS. Sections were then incubated with mouse anti-NeuN antibody (1:200; Chemicon, Temecula, CA) at 4 °C overnight. FITC-conjugated anti-mouse antibody (1:400; Jackson ImmunoResearch, West Grove, PA) was added to sections at room temperature for 2 h. Sections were then incubated with mouse anti-BrdU antibody (1:200; Dako, Glostrup, Denmark) at 4°C overnight. Sections were then incubated with Cy3-conjugated anti-mouse antibody (1:400; Jackson ImmunoResearch, West Grove, PA) at room temperature for 2 h. Each of the steps was followed by three 5-min rinses in PBS. Tissue sections were mounted with Vectashield mounting medium (Vector laboratories, Burlingame, CA). Images were collected with fluorescent microscopy. NeuN/BrdU-colabeled cells in the DG and the cortex were counted at a magnification of 40.
4.11. Cell counting and quantization
Cell counts were performed by observers blinded to the individual treatment status of the animals. Five sections with 50-µm intervals from the dorsal DG were analyzed with a microscope (Nikon i80) at 400x magnification via the MCID system (Lu et al., 2005). All counting was performed on a computer monitor to improve visualization and in one focal plane to avoid oversampling (Zhang et al., 2002). To evaluate whether intraperitoneally administered EPO reduces neuronal damage after TBI, the number of cells was counted in the DG and CA3 region using the MCID system. Counts were averaged and normalized by measuring the linear distance (in mm) of the DG and CA3 region for each section. Although it is just an estimate of the cell number, this method permits a meaningful comparison of differences between groups. For cell proliferation, the total number of BrdU-positive cells was counted in the lesion boundary zone (LBZ) and the DG region of the hippocampus, using the MCID system. The cells with BrdU (brown stained) that clearly localized to the nucleus (hematoxylin stained) were counted as BrdU-positive cells. The number of BrdU-positive cells was expressed in cells/mm2 in the LBZ and the DG. For analysis of neurogenesis, additional sections used in the above studies were used to evaluate neurogenesis in the DG and the cortex by calculating the density of BrdU-labeled cells and BrdU/NeuN-colabeled cells (Lu et al., 2007b). The number of BrdU-positive cells (red stained) and NeuN/BrdU-colabeled cells (yellow after merge) were counted in the DG and the LBZ. The percentage of NeuN/BrdU-colabeled cells over the total number of BrdU-positive cells in the corresponding regions (DG or LBZ) was estimated and used as a parameter to evaluate neurogenesis (Xiong et al., 2008).
4.12. Statistical analysis
All data are presented as means with standard deviations (SD). Data on mNSS were first evaluated for normality. The rank data were used for the analysis since data were not normal. Analysis of variance (ANCOVA), PROC MIXED with CONTRAST statement in SAS, was employed to test the group difference on mNSS. The analysis began testing the overall group effect, followed by pair-wise group comparisons if the overall group effect was detected at the 0.05 level; otherwise the pair-wise group comparisons would be considered as exploratory analysis. Data on HCT and sensorimotor function were analyzed by ANOVA for repeated measurements. For lesion volume, cell counting, and vWF-stained vascular density, a one-way ANOVA followed by post hoc SNK tests were used to compare the difference between the EPO-treated, EPO-hemodilution-treated, saline-treated and sham groups. Statistical significance was set at P<0.05.
Acknowledgments
This work was supported by NIH grants RO1 NS 62002, PO1 NS42345.
Sources of financial support: NIH grants RO1 NS62002 (Ye Xiong) and PO1 NS42345 (Asim Mahmood, Michael Chopp).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Brines ML, Ghezzi P, Keenan S, Agnello D, de Lanerolle NC, Cerami C, Itri LM, Cerami A. Erythropoietin crosses the blood-brain barrier to protect against experimental brain injury. Proc Natl Acad Sci U S A. 2000;97:10526–10531. doi: 10.1073/pnas.97.19.10526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson AP, Schermer CR, Lu SW. Retrospective evaluation of anemia and transfusion in traumatic brain injury. J Trauma. 2006;61:567–571. doi: 10.1097/01.ta.0000231768.44727.a2. [DOI] [PubMed] [Google Scholar]
- Cerami A. Beyond erythropoiesis: novel applications for recombinant human erythropoietin. Semin Hematol. 2001;38:33–39. doi: 10.1016/s0037-1963(01)90128-3. [DOI] [PubMed] [Google Scholar]
- Chen J, Sanberg PR, Li Y, Wang L, Lu M, Willing AE, Sanchez-Ramos J, Chopp M. Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke. 2001;32:2682–2688. doi: 10.1161/hs1101.098367. [DOI] [PubMed] [Google Scholar]
- Chen J, Zhang C, Jiang H, Li Y, Zhang L, Robin A, Katakowski M, Lu M, Chopp M. Atorvastatin induction of VEGF and BDNF promotes brain plasticity after stroke in mice. J Cereb Blood Flow Metab. 2005;25:281–290. doi: 10.1038/sj.jcbfm.9600034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherian L, Goodman JC, Robertson C. Neuroprotection with erythropoietin administration following controlled cortical impact injury in rats. J Pharmacol Exp Ther. 2007;322:789–794. doi: 10.1124/jpet.107.119628. [DOI] [PubMed] [Google Scholar]
- Cheung W, Minton N, Gunawardena K. Pharmacokinetics and pharmacodynamics of epoetin alfa once weekly and three times weekly. Eur J Clin Pharmacol. 2001;57:411–418. doi: 10.1007/s002280100324. [DOI] [PubMed] [Google Scholar]
- Choi SH, Woodlee MT, Hong JJ, Schallert T. A simple modification of the water maze test to enhance daily detection of spatial memory in rats and mice. J Neurosci Methods. 2006;156:182–193. doi: 10.1016/j.jneumeth.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Corwin HL, Gettinger A, Fabian TC, May A, Pearl RG, Heard S, An R, Bowers PJ, Burton P, Klausner MA, Corwin MJ. Efficacy and safety of epoetin alfa in critically ill patients. N Engl J Med. 2007;357:965–976. doi: 10.1056/NEJMoa071533. [DOI] [PubMed] [Google Scholar]
- Davis AE. Mechanisms of traumatic brain injury: biomechanical, structural and cellular considerations. Crit Care Nurs Q. 2000;23:1–13. doi: 10.1097/00002727-200011000-00002. [DOI] [PubMed] [Google Scholar]
- Dixon CE, Clifton GL, Lighthall JW, Yaghmai AA, Hayes RL. A controlled cortical impact model of traumatic brain injury in the rat. J Neurosci Methods. 1991;39:253–262. doi: 10.1016/0165-0270(91)90104-8. [DOI] [PubMed] [Google Scholar]
- Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, Rustenbeck HH, Breiter N, Jacob S, Knerlich F, Bohn M, Poser W, Ruther E, Kochen M, Gefeller O, Gleiter C, Wessel TC, De Ryck M, Itri L, Prange H, Cerami A, Brines M, Siren AL. Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med. 2002;8:495–505. [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich H, Fischer B, Norra C, Schellenberger F, Stender N, Stiefel M, Siren AL, Paulus W, Nave KA, Gold R, Bartels C. Exploring recombinant human erythropoietin in chronic progressive multiple sclerosis. Brain. 2007;130:2577–2588. doi: 10.1093/brain/awm203. [DOI] [PubMed] [Google Scholar]
- Ge YL, Lv R, Zhou W, Ma XX, Zhong TD, Duan ML. Brain damage following severe acute normovolemic hemodilution in combination with controlled hypotension in rats. Acta Anaesthesiol Scand. 2007;51:1331–1337. doi: 10.1111/j.1399-6576.2007.01448.x. [DOI] [PubMed] [Google Scholar]
- Gilmer LK, Roberts KN, Sullivan PG, Miller K, Scheff S. Early mitochondrial dysfunction following cortical contusion injury. J Neurotrauma. 2009 Apr 22; doi: 10.1089/neu.2008.0857. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goings GE, Sahni V, Szele FG. Migration patterns of subventricular zone cells in adult mice change after cerebral cortex injury. Brain Res. 2004;996:213–226. doi: 10.1016/j.brainres.2003.10.034. [DOI] [PubMed] [Google Scholar]
- Grasso G, Sfacteria A, Cerami A, Brines M. Erythropoietin as a tissue-protective cytokine in brain injury: what do we know and where do we go? Neuroscientist. 2004;10:93–98. doi: 10.1177/1073858403259187. [DOI] [PubMed] [Google Scholar]
- Grasso G, Sfacteria A, Erbayraktar S, Passalacqua M, Meli F, Gokmen N, Yilmaz O, La Torre D, Buemi M, Iacopino DG, Coleman T, Cerami A, Brines M, Tomasello F. Amelioration of spinal cord compressive injury by pharmacological preconditioning with erythropoietin and a nonerythropoietic erythropoietin derivative. J Neurosurg Spine. 2006;4:310–318. doi: 10.3171/spi.2006.4.4.310. [DOI] [PubMed] [Google Scholar]
- Grasso G, Sfacteria A, Meli F, Fodale V, Buemi M, Iacopino DG. Neuroprotection by erythropoietin administration after experimental traumatic brain injury. Brain Res. 2007;1182:99–105. doi: 10.1016/j.brainres.2007.08.078. [DOI] [PubMed] [Google Scholar]
- Henke M, Laszig R, Rube C, Schafer U, Haase KD, Schilcher B, Mose S, Beer KT, Burger U, Dougherty C, Frommhold H. Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: randomised, double-blind, placebo-controlled trial. Lancet. 2003;362:1255–1260. doi: 10.1016/S0140-6736(03)14567-9. [DOI] [PubMed] [Google Scholar]
- Jeremitsky E, Omert L, Dunham CM, Protetch J, Rodriguez A. Harbingers of poor outcome the day after severe brain injury: hypothermia, hypoxia, and hypoperfusion. J Trauma. 2003;54:312–319. doi: 10.1097/01.TA.0000037876.37236.D6. [DOI] [PubMed] [Google Scholar]
- Leyland-Jones B. Breast cancer trial with erythropoietin terminated unexpectedly. Lancet Oncol. 2003;4:459–460. doi: 10.1016/s1470-2045(03)01163-x. [DOI] [PubMed] [Google Scholar]
- Li M, Ratcliffe SJ, Knoll F, Wu J, Ances B, Mardini W, Floyd TF. Aging: impact upon local cerebral oxygenation and blood flow with acute isovolemic hemodilution. J Neurosurg Anesthesiol. 2006;18:125–131. doi: 10.1097/00008506-200604000-00006. [DOI] [PubMed] [Google Scholar]
- Li Y, Lu Z, Keogh CL, Yu SP, Wei L. Erythropoietin-induced neurovascular protection, angiogenesis, and cerebral blood flow restoration after focal ischemia in mice. J Cereb Blood Flow Metab. 2007;27:1043–1054. doi: 10.1038/sj.jcbfm.9600417. [DOI] [PubMed] [Google Scholar]
- Liao ZB, Zhi XG, Shi QH, He ZH. Recombinant human erythropoietin administration protects cortical neurons from traumatic brain injury in rats. Eur J Neurol. 2008;15:140–149. doi: 10.1111/j.1468-1331.2007.02013.x. [DOI] [PubMed] [Google Scholar]
- Lindenblatt N, Menger MD, Klar E, Vollmar B. Darbepoetin-alpha does not promote microvascular thrombus formation in mice: role of eNOS-dependent protection through platelet and endothelial cell deactivation. Arterioscler Thromb Vasc Biol. 2007;27:1191–1198. doi: 10.1161/ATVBAHA.107.141580. [DOI] [PubMed] [Google Scholar]
- Lu D, Mahmood A, Qu C, Goussev A, Schallert T, Chopp M. Erythropoietin enhances neurogenesis and restores spatial memory in rats after traumatic brain injury. J Neurotrauma. 2005;22:1011–1017. doi: 10.1089/neu.2005.22.1011. [DOI] [PubMed] [Google Scholar]
- Lu D, Mahmood A, Qu C, Hong X, Kaplan D, Chopp M. Collagen scaffolds populated with human marrow stromal cells reduce lesion volume and improve functional outcome after traumatic brain injury. Neurosurgery. 2007a;61:596–602. doi: 10.1227/01.NEU.0000290908.38438.B2. discussion 602–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu D, Qu C, Goussev A, Jiang H, Lu C, Schallert T, Mahmood A, Chen J, Li Y, Chopp M. Statins increase neurogenesis in the dentate gyrus, reduce delayed neuronal death in the hippocampal CA3 region, and improve spatial learning in rat after traumatic brain injury. J Neurotrauma. 2007b;24:1132–1146. doi: 10.1089/neu.2007.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood A, Lu D, Chopp M. Marrow stromal cell transplantation after traumatic brain injury promotes cellular proliferation within the brain. Neurosurgery. 2004;55:1185–1193. doi: 10.1227/01.neu.0000141042.14476.3c. [DOI] [PubMed] [Google Scholar]
- Mahmood A, Lu D, Qu C, Goussev A, Zhang ZG, Lu C, Chopp M. Treatment of traumatic brain injury in rats with erythropoietin and carbamylated erythropoietin. J Neurosurg. 2007;107:392–397. doi: 10.3171/JNS-07/08/0392. [DOI] [PubMed] [Google Scholar]
- Marti HH. Erythropoietin and the hypoxic brain. J Exp Biol. 2004;207:3233–3242. doi: 10.1242/jeb.01049. [DOI] [PubMed] [Google Scholar]
- Milano M, Schneider M. EPO in cancer anemia: benefits and potential risks. Crit Rev Oncol Hematol. 2007;62:119–125. doi: 10.1016/j.critrevonc.2006.11.011. [DOI] [PubMed] [Google Scholar]
- Morris R. Developments of a water-maze procedure for studying spatial learning in the rat. J Neurosci Methods. 1984;11:47–60. doi: 10.1016/0165-0270(84)90007-4. [DOI] [PubMed] [Google Scholar]
- Narayan RK, Michel ME, Ansell B, Baethmann A, Biegon A, Bracken MB, Bullock MR, Choi SC, Clifton GL, Contant CF, Coplin WM, Dietrich WD, Ghajar J, Grady SM, Grossman RG, Hall ED, Heetderks W, Hovda DA, Jallo J, Katz RL, Knoller N, Kochanek PM, Maas AI, Majde J, Marion DW, Marmarou A, Marshall LF, McIntosh TK, Miller E, Mohberg N, Muizelaar JP, Pitts LH, Quinn P, Riesenfeld G, Robertson CS, Strauss KI, Teasdale G, Temkin N, Tuma R, Wade C, Walker MD, Weinrich M, Whyte J, Wilberger J, Young AB, Yurkewicz L. Clinical trials in head injury. J Neurotrauma. 2002;19:503–557. doi: 10.1089/089771502753754037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson CL, Scafidi S, McKenna MC, Fiskum G. Mitochondrial mechanisms of cell death and neuroprotection in pediatric ischemic and traumatic brain injury. Exp Neurol. 2009;218:371–380. doi: 10.1016/j.expneurol.2009.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig MQ, Bender CM, Lucke JP, Yasko JM, Brufsky AM. The decision to prematurely terminate a trial of R-HuEPO due to thrombotic events. J Pain Symptom Manage. 2004;27:185–190. doi: 10.1016/j.jpainsymman.2003.06.010. [DOI] [PubMed] [Google Scholar]
- Sakanaka M, Wen TC, Matsuda S, Masuda S, Morishita E, Nagao M, Sasaki R. In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci U S A. 1998;95:4635–4640. doi: 10.1073/pnas.95.8.4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salim A, Hadjizacharia P, DuBose J, Brown C, Inaba K, Chan L, Margulies DR. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008;207:398–406. doi: 10.1016/j.jamcollsurg.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Schallert T. Behavioral tests for preclinical intervention assessment. NeuroRx. 2006;3:497–504. doi: 10.1016/j.nurx.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibata J, Hasegawa J, Siemens HJ, Wolber E, Dibbelt L, Li D, Katschinski DM, Fandrey J, Jelkmann W, Gassmann M, Wenger RH, Wagner KF. Hemostasis and coagulation at a hematocrit level of 0.85: functional consequences of erythrocytosis. Blood. 2003;101:4416–4422. doi: 10.1182/blood-2002-09-2814. [DOI] [PubMed] [Google Scholar]
- Sullivan PG, Keller JN, Bussen WL, Scheff SW. Cytochrome c release and caspase activation after traumatic brain injury. Brain Res. 2002;949:88–96. doi: 10.1016/s0006-8993(02)02968-2. [DOI] [PubMed] [Google Scholar]
- Sun D, McGinn MJ, Zhou Z, Harvey HB, Bullock MR, Colello RJ. Anatomical integration of newly generated dentate granule neurons following traumatic brain injury in adult rats and its association to cognitive recovery. Exp Neurol. 2007;204:264–272. doi: 10.1016/j.expneurol.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Sundholm-Peters NL, Yang HK, Goings GE, Walker AS, Szele FG. Subventricular zone neuroblasts emigrate toward cortical lesions. J Neuropathol Exp Neurol. 2005;64:1089–1100. doi: 10.1097/01.jnen.0000190066.13312.8f. [DOI] [PubMed] [Google Scholar]
- Swanson RA, Morton MT, Tsao-Wu G, Savalos RA, Davidson C, Sharp FR. A semiautomated method for measuring brain infarct volume. J Cereb Blood Flow Metab. 1990;10:290–293. doi: 10.1038/jcbfm.1990.47. [DOI] [PubMed] [Google Scholar]
- Thurman D, Guerrero J. Trends in hospitalization associated with traumatic brain injury. Jama. 1999;282:954–957. doi: 10.1001/jama.282.10.954. [DOI] [PubMed] [Google Scholar]
- Verweij BH, Muizelaar JP, Vinas FC, Peterson PL, Xiong Y, Lee CP. Impaired cerebral mitochondrial function after traumatic brain injury in humans. J Neurosurg. 2000;93:815–820. doi: 10.3171/jns.2000.93.5.0815. [DOI] [PubMed] [Google Scholar]
- Wang L, Zhang Z, Wang Y, Zhang R, Chopp M. Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke. 2004;35:1732–1737. doi: 10.1161/01.STR.0000132196.49028.a4. [DOI] [PubMed] [Google Scholar]
- Wish JB. Past, present, and future of chronic kidney disease anemia management in the United States. Adv Chronic Kidney Dis. 2009;16:101–108. doi: 10.1053/j.ackd.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Xiong Y, Gu Q, Peterson PL, Muizelaar JP, Lee CP. Mitochondrial dysfunction and calcium perturbation induced by traumatic brain injury. J Neurotrauma. 1997;14:23–34. doi: 10.1089/neu.1997.14.23. [DOI] [PubMed] [Google Scholar]
- Xiong Y, Mahmood A, Lu D, Qu C, Goussev A, Schallert T, Chopp M. Role of gender in outcome after traumatic brain injury and therapeutic effect of erythropoietin in mice. Brain Res. 2007;1185:301–312. doi: 10.1016/j.brainres.2007.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y, Lu D, Qu C, Goussev A, Schallert T, Mahmood A, Chopp M. Effects of erythropoietin on reducing brain damage and improving functional outcome after traumatic brain injury in mice. J Neurosurg. 2008;109:510–521. doi: 10.3171/JNS/2008/109/9/0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y, Chopp M, Lee CP. Erythropoietin improves brain mitochondrial function in rats after traumatic brain injury. Neurol Res. 2009;31:496–502. doi: 10.1179/174313208X353703. [DOI] [PubMed] [Google Scholar]
- Zhang J, Li Y, Cui Y, Chen J, Lu M, Elias SB, Chopp M. Erythropoietin treatment improves neurological functional recovery in EAE mice. Brain Res. 2005;1034:34–39. doi: 10.1016/j.brainres.2004.11.036. [DOI] [PubMed] [Google Scholar]
- Zhang R, Wang Y, Zhang L, Zhang Z, Tsang W, Lu M, Zhang L, Chopp M. Sildenafil (Viagra) induces neurogenesis and promotes functional recovery after stroke in rats. Stroke. 2002;33:2675–2680. doi: 10.1161/01.str.0000034399.95249.59. [DOI] [PubMed] [Google Scholar]
- Zhang R, Zhang Z, Wang L, Wang Y, Gousev A, Zhang L, Ho KL, Morshead C, Chopp M. Activated neural stem cells contribute to stroke-induced neurogenesis and neuroblast migration toward the infarct boundary in adult rats. J Cereb Blood Flow Metab. 2004;24:441–448. doi: 10.1097/00004647-200404000-00009. [DOI] [PubMed] [Google Scholar]
- Zhang RL, Zhang ZG, Chopp M. Ischemic stroke and neurogenesis in the subventricular zone. Neuropharmacology. 2008;55:345–352. doi: 10.1016/j.neuropharm.2008.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang RL, Chopp M, Gregg SR, Toh Y, Roberts C, Letourneau Y, Buller B, Jia L, S PND, Zhang ZG. Patterns and dynamics of subventricular zone neuroblast migration in the ischemic striatum of the adult mouse. J Cereb Blood Flow Metab. 2009;29:1240–1250. doi: 10.1038/jcbfm.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang ZG, Chopp M. Neurorestorative therapies for stroke: underlying mechanisms and translation to the clinic. Lancet Neurol. 2009;8:491–500. doi: 10.1016/S1474-4422(09)70061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]