Abstract
Highly active antiretroviral therapy (HAART) has significantly improved the prognosis for many individuals with HIV infection. Consequently, HIV infection has become a chronic and manageable disease. The focus on long-term management of patients with HIV infection has broadened to include comorbid conditions, most notably cardiovascular disease. Patients with HIV infection share many cardiovascular risk factors with the general population, and HIV infection itself may increase cardiovascular risk. Changes in lipid profiles associated with increased cardiovascular risk that have been observed with some HAART regimens have been a cause for concern among clinicians who treat HIV-infected patients. However, the lipid effects of HAART seem to depend on the type and duration of regimens employed. They can be managed effectively according to current guidelines that recommend lifestyle changes (eg, improved diet, increased exercise, smoking cessation) and pharmacologic therapy described in established treatment paradigms for patients on antiretroviral therapy and similar to measures currently used by the general population. A review of the clinical data indicates that the virologic and immunologic benefits of HAART clearly outweigh any metabolic effects observed in some patients over time and that preexisting, established cardiovascular risk factors contribute significantly to the potential development of cardiovascular events.
These benefits of antiretroviral therapy have been demonstrated in studies comparing the superior efficacy of continuous vs. intermittent HAART.
Keywords: antiretroviral, cardiovascular, cholesterol, HAART, lopinavir, protease inhibitor, triglycerides
INTRODUCTION
Changing Paradigm of Care for Chronic HIV Disease
The past decade has witnessed a revolution in the treatment of and long-term prognosis for patients with HIV infection. The advent of highly active antiretroviral therapy (HAART) has made HIV infection a chronic manageable disease for many patients.1–3 In 1986, the median survival for a person with HIV infection was 10 years; currently, more than 85% of patients with HIV infection survive more than 10 years.3,4 After the implementation of HAART as standard of care in 1996, mortality due to AIDS decreased substantially—both the total number of deaths and the rate of death after diagnosis—as a result of the effectiveness of current therapy in providing sustained suppression of viral replication and preservation of immune system function.3,5,6 Consequently, in the HAART era, traditional risk factors (eg, trauma, smoking), high-risk behaviors (eg, injection drug use, high-risk sexual activity), and chronic debilitating illnesses such as decompensated hepatic failure, cirrhosis, hepatitis C virus (HCV) infection, pulmonary disease, diabetes, hypertension, and malignancies have become more important proportionally as major causes of morbidity and mortality for many patients.5,7
The benefits of HAART in reducing fatal and nonfatal events have recently been underscored by results from the Strategies for Management of AntiRetroviral Therapy (SMART) study, which showed that intermittent antiretroviral therapy (ART) based on CD4+ cell count-guided drug conservation was associated with significantly greater disease progression and mortality risk (hepatic, renal, cardiovascular events) than continuous ART.8 In addition, patients who delayed HAART until CD4+ T-cell counts fell below 250 cells per cubic millimeter had a 7 times higher risk of a serious non-AIDS illness, and their risk of a fatal or nonfatal opportunistic disease or a serious non-AIDS illness (a composite end point) was 5 times higher after an average of 18 months of follow-up.9 In contrast, patients with continuous therapy spent more than twice as much follow-up time with a CD4+ count >500 cells per cubic millimeter than patients who deferred therapy.9
As a result of advances in treatment of HIV infection over the last 10 years, the goals of therapy have shifted from simply keeping patients alive to maintaining good quality of life and effectively treating comorbidities. Management of HIV-infected patients must now include the prevention and treatment of concomitant diseases such as chronic kidney disease, diabetes, or HCV coinfection.10–12
Cardiovascular Disease and HIV/AIDS in Perspective
Cardiovascular disease is the number 1 cause of mortality in the general population.13 It is also an important cause of death among patients with HIV infection. However, other causes of death (ie, hepatic disease, cancer) have also become common among patients with HIV infection.14,15 In 2005, one third of deaths among patients infected with HIV were due to malignancies.15
Cardiovascular Risk Factors
Individuals who develop cardiovascular disease usually have multiple risk factors for this condition (Table 1). Well-established risk factors for cardiovascular disease include lack of exercise, obesity, smoking, diabetes, hypertension, advanced age, dyslipidemia [high levels of total cholesterol and low-density lipoprotein cholesterol (LDL-C) and low levels of high-density lipoprotein cholesterol (HDL-C)], and insulin resistance/impaired glucose intolerance.16,17 There is synergy among cardiovascular risk factors such that the co-occurrence of 2 or more risk factors (eg, hypertension and dyslipidemia) may have greater than additive effects on overall cardiovascular risk.18 Of interest, analysis of data from 2 large patient cohorts showed that patients with HIV infection have a significantly greater prevalence of smoking, along with higher total:HDL-C and LDL-C:HDL-C ratios and serum triglyceride levels than uninfected subjects, thus placing these HIV-infected patients at even greater risk for cardiovascular disease.19
TABLE 1.
Risk Factors for Cardiovascular Disease16
| Factors used to determine LDL-C goals |
| Cigarette smoking |
| Hypertension |
| Low HDL-C |
| Diabetes |
| Family history of premature coronary heart disease |
| Age |
| Additional established risk factors |
| Obesity |
| Physical inactivity |
| Atherogenic diet |
| Emerging risk factors |
| Lipoprotein (a) |
| Homocysteine |
| Prothrombotic and proinflammatory factors |
| Impaired fasting glucose |
| Subclinical atherosclerosis |
Impact of HIV Infection on Cardiovascular Risk
The presence of HIV infection itself may increase cardiovascular risk. Uncontrolled HIV replication has been demonstrated to be a significant independent risk factor for similar lipid changes found to be associated with increased risk for cardiovascular disease in the general population, including hypercholesterolemia, elevated levels of very low-density cholesterol, and triglycerides, and lowered HDL-C levels.20,21 In HIV-infected patients, these lipid changes have been found to be statistically associated with lower CD4+ T-cell counts and higher viral RNA levels.20 In addition, a higher viral load is correlated with endothelial dysfunction, which is also related to an increased risk of cardiovascular events.22 Endothelial dysfunction manifesting as increased carotid intima—media thickness (CIMT) is strongly correlated with traditional risk factors for atherosclerosis and cardiovascular disease, including increased plasma levels of thrombophilic factor VIII activity and very low-density cholesterol and decreased clearance of apolipoprotein particles that is correlated with reduced plasma adiponectin levels.21,23 In patients with HIV infection, CIMT is also associated with increased CD4+ and CD8+ T-cell activation and nadir CD4+ cell count ≤200 cells per cubic millimeter.24–27 These patients may also present before and during ART with an increased atherogenic profile consistent with greater circulating amounts of small, dense lipoprotein particles, greater LDL triglyceride content, and smaller mean LDL particle size.28
Other surrogate markers may prove to be useful in evaluating the risk for cardiovascular disease in HIV-infected patients. Inflammatory markers such as C-reactive protein (CRP), an acute phase protein, is elevated in HIV-infected patients and associated with more rapid disease progression to AIDS.25,29 Higher intrahepatic levels of the proinflammatory cytokines, tumor necrosis factor-α (TNF-α) and interferon gamma, are found in treatment-naive patients with HIV/HCV coinfection,30 and elevated serum levels of TNF-α receptor in patients with HIV-associated lipodystrophy are correlated with severe insulin resistance.31 However, the correlation of these proinflammatory markers with increased cardiovascular risk and long-term outcomes in HIV-infected patients remains to be validated in larger studies.
Several studies reported at the 2008 Conference on Retroviruses and Opportunistic Infections shed additional light on the association between certain inflammatory and endothelial markers and cardiovascular risk. Kristoffersen et al32 demonstrated significantly higher serum concentrations of the inflammatory and endothelial activation markers, high-sensitive CRP (hs-CRP), tissue plasminogen activator inhibitor-1, and soluble intercellular adhesion molecule-1 (sICAM-1), in HIV-infected patients (n = 115) vs. HIV-uninfected, age-matched, and gender-matched controls (n = 300). In this study, 3 months of combination ART elicited significant decreases in levels of E-selectin (15.1 ± 0.8ng/mL; P < 0.01), sICAM-1 (248 ± 12 ng/mL; P < 0.05), soluble vascular cell adhesion molecule-1 (sVCAM-1) (766 ± 33 ng/mL; P < 0.001), and hs-CRP (14,708 ± 2358 ng/mL; P < 0.001), but not tissue plasminogen activator inhibitor-1. These markers remained at reduced levels through 12 months of ART.32
Ross et al33 reported results from a small, prospective study to assess the correlation between inflammatory and endothelial activation biomarkers and CIMT in HIV-infected patients. Compared with HIV-uninfected controls (n = 32), HIV-infected patients (n = 62) had significantly more CIMT and increased expression of the inflammatory markers, hs-CRP, soluble TNF receptor II, and interleukin 6 (IL-6), and the endothelial activation marker, sICAM-1. In both HIV-infected and HIV-uninfected patients, inflammatory markers correlated with the endothelial activation marker, sVCAM-1.33
The realization that HIV infection, particularly uncontrolled viremia, and the presence of risk factors shared with the general population are important causes of cardiovascular disease among patients with HIV infection has significant implications for therapeutic intervention in patients with both conditions. Most importantly, it suggests that stopping or interrupting HAART may be of relatively little benefit in decreasing cardiovascular risk.
Results from a cardiovascular substudy of the SMART trial indicated that patients in the CD4-guided intermittent treatment group were at increased risk for evidence of myocardial damage, including repolarization abnormalities and increased heart rate, compared with patients who received treatment aimed at early and continuous viral suppression.34 In a follow-up to the SMART study, Kuller et al35 demonstrated that CD4-guided structured treatment interruption elicited significant increases in IL-6 (a proinflammatory and anti-inflammatory cytokine) and the coagulation marker D-dimer, as compared with matched patients receiving continuous ART (viral suppression group). Elevated levels (upper fourth quartile) of baseline D-dimer and IL-6 (ie, non-ART associated) were significantly associated with increased mortality risk, whereas D-dimer and amyloid-P were modestly associated with increased cardiovascular risk.35 Similar to this study, Calmy et al36 measured various inflammatory and endothelial activation markers in 145 HIV-infected patients with stable, undetectable HIV RNA levels and CD4 counts >350 cells per cubic millimeter that were randomized to continuous ART or CD4-guided structured treatment interruption. At 24 weeks after randomization, patients receiving continuous ART had significantly lower levels of sVCAM, adiponectin, macrophage chemotactic protein 1, and IL-10. Retreatment of patients in the treatment interruption arm was followed by a 30% decrease for adiponectin (P < 0.001), a 76% decrease for IL-10 (P = 0.03), and a 55% increase for sVCAM (P = 0.002). Therefore, results from these 2 latter studies showed that acute viral replication occurring after treatment interruption is related to a potentially deleterious changes in key markers of cardiovascular risk.
These outcomes underscore the important point that untreated HIV infection may increase the risk of not only AIDS-related complications but also cardiovascular disease. In addition, the results from the SMART study led to the early cessation of this trial and prompted the recommendation that ART in patients with HIV infection be neither stopped nor interrupted because of concerns regarding potentially increased cardiovascular risk.37 This recommendation is supported by findings from a cohort of more than 8000 HIV-infected patients followed since 1993 in the HIV Outpatient Study, which showed no significant association between treatment adherence (<95% or ≥95%) to HAART and increased cardiovascular risk.38 In this study, univariate and multivariate analysis showed that age greater than 40 years, nadir HDL-C level, hyperlipidemia, hypertension, and diabetes were the factors most significantly associated with increased risk of cardiovascular disease (odds ratio >2.4).38 In contrast, pre-HAART CD4+ cell count, peak viral load, percentage of time on HAART since initiation of the first regimen, specific ART classes, ART switches, body mass index greater than 30 kg/m2, and peak total cholesterol, LDL-C, and triglyceride levels were not associated with an increased risk of cardiovascular disease.38 The use of lipid-lowering agents significantly reduced the risk of cardiovascular disease.
Study results briefly summarized in the above section indicate that the increased risk of cardiovascular disease among patients with HIV infection may be due, in large part, to traditional risk factors that are shared by the general population. In addition, HIV infection itself may result in metabolic and inflammatory events that increase cardiovascular risk. Finally, available data also support the conclusion that stopping or switching therapy in patients with HIV infection is not likely to decrease cardiovascular risk.
Influence of ART on Cardiovascular Risk
Recent results from the SMART study indicate that interruption of HAART is associated with increased cardiovascular risk in patients with HIV infection.8 However, older studies concerned with the relationship between HAART and cardiovascular risk have provided conflicting results. Some older studies have suggested that protease inhibitor (PI)— containing HAART regimens in particular may significantly increase cardiovascular risk in patients with HIV infection,39 whereas others have not.40 The varied results from these older studies may be due, at least in part, to limitations in study design, short durations of HAART exposure, and a low incidence of cardiovascular events for analysis.
A retrospective/prospective observational study in a clinic-based population of HIV-infected patients in Los Angeles county between 1990 and 2000 examined the relationship between PI use and cardiovascular disease, defined as ischemic heart disease/coronary artery disease and cerebrovascular disease/stroke. Within a database of 5667 HIV-infected individuals contributing 15,550 person-years of follow-up, 80 incident cases of cardiovascular disease (1.4%) were identified. Cox proportional hazards model analysis showed that for these 80 patients, the use of PIs [hazard ratio (HR) = 6.22, P < 0.001] and time-dependent non-PI use (HR = 3.18, P < 0.001) were associated with incident cardiovascular disease.41
One of the largest studies to date on cardiovascular risks in HIV infection and treatment is the ongoing Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study of 23,437 patients with HIV infection in whom 345 myocardial infarctions (MIs) (1.5%) were recorded for more than 94,469 person-years.42 Results of this study using Poisson regression analysis models identified certain risk factors for MIs that included older age, current or former smoking, previous cardiovascular disease, and male gender. Elevated total cholesterol and triglyceride levels and diabetes were also associated with an increased incidence of MI. After adjusting for exposure to the other drug class and established cardiovascular risk factors (eg, hypertension and diabetes), the relative risk of MI associated with the use of PIs was 1.16 per year of exposure (95% confidence interval, 1.10 to 1.23), whereas treatment with a nonnucleoside reverse transcriptase inhibitor (NNRTI) did not increase the risk of MI appreciably (relative risk = 1.05/year of exposure; 95% confidence interval, 0.98 to 1.13.42
Although PI use was associated with increased cardiovascular risk in the D:A:D study, it is important to compare this risk with those resulting from other factors. For example, PI-associated risk was considerably lower than the annual increase in risk associated with advanced age (1.39, P < 0.001), male gender (1.91, P = 0.002), or current smoking (2.83, P < 0.001).42 In addition, the MI incidence rates for PIs and NNRTIs in this study overlapped through 4 years of follow-up. There was a sudden drop in MI incidence associated with NNRTI use by year 5, but the reason for this trend is not clear.43 It should also be noted that the absolute risk of MI among patients receiving PIs in the D:A:D study was 0.6% per year and lower than that for all patients in the SMART study (0.8% per year).8,43
Other clinical results suggest that the association between use of PIs and increased cardiovascular risk is complex. A retrospective analysis of cardiovascular and cerebrovascular disease among 36,766 patients who received care for HIV infection at Veterans Affairs facilities between January 1993 and June 2001 demonstrated that newer therapies for HIV were associated with significant mortality benefits. These benefits were not diminished by any increase in the rate of cardiovascular or cerebrovascular events or related mortality.40 Results from 1744 patients contributing data to HIV Outpatient Study from 1993 to 2005 indicated a trend toward decreased cardiovascular risk among patients who remained on HAART for more than 13 years of follow-up. There was also a temporal decline in the incidence of MI events overall, from the highest number observed in 2000 (3.4/1000 patient-years) to only 1.1 per 1000 patient-years in 2005, that paralleled a dramatic increase in the use of lipid-lowering agents.38 Cox proportional hazards analysis among patients with hyperlipidemia in this study showed nearly statistically significant increases in cardiovascular risk associated with age greater than 40 years (HR = 2.38), smoking (HR = 2.22), and diabetes (HR = 2.45), whereas the use of lipid-lowering agents significantly decreased cardiovascular risk (HR = 0.34).38
All these results suggest that cardiovascular disease in patients with HIV infection, including those being treated with PIs, can be characterized as relatively modest and manageable, as opposed to the emerging epidemic suggested by earlier data.43 Other studies support the view that HAART actually decreases surrogate markers for cardiovascular events. Results from 134 subjects enrolled in AIDS Clinical Trials Group (ACTG 5078) indicated that treatment with a PI-containing HAART regimen was not associated with a significant increase in CIMT, compared with PI-naive patients.44 There is also evidence that HAART can significantly improve endothelial function. A prospective, randomized, multicenter trial assessed the effects of 3 class-sparing ART regimens on endothelial function in patients with HIV infection. The 3 regimens were nucleoside reverse transcriptase inhibitor (NRTI) [efavirenz (EFV)] plus NNRTI, NRTI plus PI [lopinavir/ritonavir (LPV/r)], and NNRTI plus PI. Before the start of ART, flow-mediated vasodilation (FMD) was impaired. At 4 weeks after initiation of ART, FMD increased by 2.8% (P = 0.003), with no significant differences among treatment arms (P = 0.609). After 24 weeks, FMD was increased by 3.0% (P < 0.001), with significant improvements for each treatment (P < 0.02) and no significant differences among treatment arms (P = 0.828).45 Thus, ART rapidly improves endothelial function in treatment-naive HIV-positive individuals independent of the specific regimen, with significant benefit observed by 4 weeks and maintained for at least 24 weeks. The improved vascular reactivity observed with ART may result in a rapid reduction in cardiovascular risk among patients with HIV infection.
In summary, historical data have provided a somewhat confusing picture with respect to the relationship between HAART and cardiovascular risk. However, a growing body of evidence suggests that HIV-positive patients, regardless of HAART regimen, generally have traditional risk factors for cardiovascular disease that may complicate determination of risk associated with specific antiretroviral agents. For example, cardiovascular risk associated with PI use is modest in studies that have reported such a relationship and may be confounded by various factors including duration of follow-up, low numbers of cardiovascular events during the study period, and different durations of use for agents from different classes. Recent data suggest that ART may improve factors (eg, endothelial dysfunction) associated with increased cardiovascular risk and that this benefit extends to all classes of antiretroviral agents.
Metabolic Effects of HAART
The link between HAART and an increased risk of cardiovascular events demonstrated in some epidemiologic studies has generally been attributed to adverse effects of therapy on lipid and glucose metabolism.46–48 However, these relationships are highly variable, and emerging data demonstrate that even when treatment alters lipid/glucose metabolism, the effects of these changes on cardiovascular risk may be relatively modest. Analysis of serum samples collected between 1984 and 2002 from HIV seroconverters indicated that HIV seroconversion resulted in reductions in total cholesterol, LDL-C, and HDL-C levels and that initiation of HAART increased both total cholesterol and LDL-C levels. However, these increases were generally a return to pre-HAART values.49 Although certain ART agents including NNRTIs may increase HDL-C levels, this effect may not translate into improved profiles of triglycerides and total cholesterol or decreased cardiovascular risk50,51 and no studies to date have demonstrated a decrease in cardiovascular incidence or risk after such improvements.
Much of the concern about the effects of HAART on lipid metabolism has focused on the adverse consequences of PI therapy. However, accruing evidence of the long-term effects of specific antiretroviral agents generally supports the view that the metabolic effects are relatively modest and can occur with most PI-containing HAART regimens (Table 2). To date, there are no data that support increased cardiovascular risk with the use of entry or integrase inhibitors.
TABLE 2.
Results from Selected Studies that Evaluated the Effects of Combination Therapies on Lipid Profiles
| Reference | Treatment | No. Patients | Duration of Treatment |
Change From Baseline (mg/dL) |
|||
|---|---|---|---|---|---|---|---|
| Total Cholesterol | LDL-C | HDL-C | Triglycerides | ||||
| Dupon et al52 | LPV/r | 127 | 18 mo | ART naive: +13.0 | NC | NC | +1.0 |
| PI naive: +9.0 | NC | NC | +77.0 | ||||
| TX-exp: +21.0 | NC | NC | +69.0 | ||||
| Montes et al53 | LPV/r | 107 | 12 mo | +40.7 | — | +11.0 | +73.3 |
| Lafeuillade et al54 | LPV/r | 159 | 45 mo | +16.9 | — | — | +76.1 |
| Eron et al55 | LPV/r | 878 | 48 wks | +52.5 | +22.5 | +14.0 | +77.5 |
| FPV + RTV | +71.0 | +28.0 | +13.0 | +67.0 | |||
| Haubrich et al56 | LPV/r + EFV | 753 | 96 wks | +57.0 | — | +16.0 | +62.0 |
| LPV/r + 2 NRTIs | +32.0 | — | +8.0 | +46.0 | |||
| EFV + 2 NRTIs | +33.0 | — | +9.0 | +19.0 | |||
| Kerr et al57 | EFV + IDV + RTV | 250 | 110 wks | +108.0 | — | +16.0 | — |
| d4T + ddI + SQV | — | — | — | — | |||
| ZDV + 3TC + IDV + RTV | +48.0 | — | −3.0 | — | |||
| ZDV + 3TC + SQV | — | — | — | — | |||
| ZDV + 3TC + IDV | +13.0 | — | −2.0 | — | |||
| Fischl et al58 | EFV + NRTI | 236 | 24 wks | — | — | — | +23.0 |
| LPV/r + EFV | — | — | — | +257.0 | |||
| Tebas et al59 | EFV + NRTI | 62 | 48 wks | −7.0 | — | — | +11.0 |
| LPV/r + EFV | +19.0 | — | — | +85.0 | |||
| Smith et al60 | ATV + RTV | 106 | 48 wks | +27.0 | +4.0 | +9.0 | +7.0 |
| FPV + RTV | +11.0 | +4.0 | +5.0 | +34.0 | |||
| Hicks et al61 | FPV + RTV (100 mg) | 58 | 48 wks | +209.0 | +126.0 | +46.0 | +172.0 |
| FPV + RTV (200 mg) | 57 | +197.0 | +108.0 | +50.0 | +149.0 | ||
| Change from baseline (%) | |||||||
| Shafran et al62 | RTV | 20 | 14 d | +10.0 | +16.0 | −5.0 | +26.0 |
| LPV/r | +19.0 | +24.0 | +1.0 | +49.0 | |||
| Malan et al63 | ATV | 199 | 48 wks | +11.0 | +16.0 | +9.0 | −15.0 |
| ATV + RTV | +24.0 | +22.0 | +9.0 | +14.0 | |||
| Absolute value at follow-up (mg/dL) | |||||||
| Trein et al64 | LPV/r | 111 | — | 214.0 | 120.0 | 42.0 | 211.0 |
| ATV + RTV | — | 203.0 | 112.0 | 39.0 | 201.0 | ||
ddI, didanosine; IDV, indinavir; NC, no change; SQV, saquinavir; TX-exp, treatment experienced.
Study 5125s was a 144-week study; the data at 48 weeks of therapy are reported.59
Metabolic Effects of PIs
Bristol-Myers Squibb (BMS) 089 is a 96-week, randomized, open-label, prospective study in 200 ART-naive subjects comparing the efficacy and safety of atazanavir (ATV) 300 mg + ritonavir (RTV) 100 mg with that of ATV 400 mg, both in combination with lamivudine (3TC) and extended-release stavudine (d4T), all administered once daily. Results at 48 weeks indicated that ATV + RTV significantly increased baseline levels of LDL-C and triglycerides above those noted with unboosted ATV (median increases of 24% vs. 16% LDL-C and 11% vs. − 12% triglycerides, respectively).63 The effects of RTV boosting were evaluated in the REDUCE trial, in which 115 patients were randomized to treatment with either fosamprenavir (FPV) 1400 mg + RTV 100 mg or FPV 1400 mg + RTV 200 mg once daily. Results from the 48-week analysis found that lipid changes were similar between the 2 treatment groups, with somewhat greater increases in total cholesterol and triglycerides noted with the 100 mg RTV dose.61
Results from the COL102060 study also suggested that RTV boosting substantially influences the effects of ATV on serum lipids.65 This 48-week, open-label, prospective study in 112 treatment-naive patients assessed the effects of ATV 300 mg + RTV 100 mg plus abacavir (ABC)/3TC, all administered once daily. At 48 weeks, there were reductions in the proportion of patients at or below the near optimal level recommended in the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) guidelines compared with baseline for triglycerides (44% vs. 68%), total cholesterol (52% vs. 84%), and LDL-C (37% vs. 46%). Results from the small, 48-week, open-label Atazanavir or Lexiva with Ritonavir and Truvada study indicated that RTV-boosted FPV (FPV 1400 mg + RTV 100 mg once daily) had effects on serum lipids similar to those of ATV 300 mg + RTV 100 mg once daily.60 The median increases in serum lipids observed with these regimens were low to moderate and, with the exception of the small median increase in HDL-C seen with ATV + RTV, did not exceed the thresholds recommended in the NCEP ATP III guidelines for interventional therapy using lipid-lowering agents.16,60
In the KLEAN study, an open-label, noninferiority trial, 878 ART-naive, HIV-positive patients were randomized to RTV-boosted FPV (FPV 700 mg + RTV 100 mg twice daily) or LPV/r (400/100 mg) twice daily. No between-group differences in lipid levels were seen after 48 weeks of treatment.55 Similarly, 48-week results from the GEMINI study comparing twice-daily saquinavir + RTV with LPV/r, each in combination with once-daily emtricitabine/tenofovir (TDF), showed that both agents elicited comparable, low to modest increases in serum cholesterol, HDL-C and LDL-C. However, use of LPV/r was associated with a statistically greater increase in triglycerides (55 mg/dL) than saquinavir + RTV (14 mg/dL).66
In the M05-730 randomized study comparing the safety and efficacy of twice-daily to once-daily administration of LPV/r tablets in ART-naive patients, similar modest increases in serum triglycerides, HDL-C, and LDL-C were observed in both treatment arms at 48 weeks, although there were greater numerical elevations in all lipids except HDL-C in the bid treatment group.67 It is important to note that the mean baseline lipid parameters were within the low normal to normal range except for HDL-C which was 39 mg/dL, therefore the clinical significance of these modest elevations are unknown. The only statistical difference between arms was noted in total cholesterol. The total cholesterol mean baseline of 155 mg/dL increased by 29 mg/dL in the once-daily arm compared with 35 mg/dL in the twice-daily arm. Four percent of subjects developed total cholesterol greater than 300 mg/dL in the daily arm compared with 3% in the twice-daily arm. Although 6% of subjects in the twice-daily arm did develop triglycerides greater than 750 mg/dL, only 3% did in the once-daily arm. This difference between arms was not statistically significant, thereby probably reflecting the small number of subjects who did develop these lipid elevations. Nevertheless, these trends have prompted some clinicians to prefer prescribing once-daily dosing for patients with preexisting lipid abnormalities, but data are lacking to warrant recommendations regarding optimal dosing schedules at this time.
Metabolic Effects of NNRTIs
The use of NNRTIs may also be associated with lipid elevations in HIV-infected patients. Recent data from the 3-arm A5095 metabolic study have demonstrated that the addition of EFV to previous dual- or triple-nucleoside— containing ART regimens marked increased levels of all measured serum lipids above baseline values.68 These investigators also observed a significant increase in lipids in patients switched to an EFV-containing intensification regimen that was not observed in patients switched to a TDF-containing regimen. These results point to the potential for lipid elevations with certain combination regimens that incorporate NNRTIs in the absence of PIs and suggest that lipid effects may be more common with certain drug combinations.
Other data supporting a general effect of HAART on lipid levels come from recent results of Study A5142, a randomized trial comparing the safety and efficacy of LPV/r + EFV or each agent in combination with 2 NRTIs in treatment-naive patients.56 Results of this cross-class comparative study showed that LPV/r was not associated with significantly greater increases in the percentages of patients with triglyceride levels greater than 750 mg/dL or LDL-C levels greater than 190 mg/dL than EFV. Data from the 96-week analysis showed both agents elicited similar and modest increases in serum lipids, with a significantly greater increase in triglycerides with LPV/r than with EFV (46 vs. 19 mg/dL) and a statistically significant effect of d4T in eliciting increases in all serum lipids except non—HDL-C.56
In the earlier 2NN study of EFV vs. nevirapine (NVP) alone or together in a backbone regimen of d4T and 3TC in treatment-naive patients, the use of NVP was associated with a significantly lower increase in serum triglycerides and increased HDL-C levels than EFV.69 In this study, levels of all serum lipids except HDL-C continued to increase gradually over the course of the 48-week treatment period in patients receiving either NNRTI or both.
Metabolic Effects of NRTIs
Currently, there are no clinical data that strongly support an increased cardiovascular risk with the use of NRTIs; mitochondrial toxicity and insulin resistance are the main adverse effects of some agents in this class.70,71 However, data demonstrating the differential effects of certain NRTIs in combination ART on the development of potentially atherogenic lipid profiles are provided by results from the study on lipid and metabolic effects of a PI-sparing regimen vs. nelfinavir-containing regimens on a backbone of either zidovudine (ZDV) or d4T.72 In this study with ethnically and racially diverse HIV-infected patients, treatment with ABC/3TC/ZDV (Trizivir) produced statistically lower levels of LDL-C levels by 96 weeks in both men and women compared with both d4T + 3TC + nelfinavir (NFV) and ZDV/3TC (Combivir) + NFV regimens and lower than d4T + 3TC + NFV in African Americans and Hispanics. The change from baseline total cholesterol and the percentage of patients with total cholesterol >200 mg/mL were significantly higher with the d4T-containing regimen than with Trizivir. The effect of d4T on higher triglyceride levels was particularly evident in women and Hispanics, whereas its effect on elevated LDL-C was most notable in African American patients and women. In addition, the greater elevation of lactate with inclusion of d4T in the ART regimen was consistent with this agent’s known mitochondrial toxicity. No significant changes in HDL-C were observed with any of these ART regimens.72
In a subanalysis of 517 patients enrolled in the D:A:D study who experienced a MI during ART, recent use of both didanosine and ABC remained significantly associated with increased rates of MI [relative rate 1.49, 1.14–1.95 (P = 0.004) for didanosine; relative rate 1.89, 1.47–2.45 (P = 0.0001) for ABC] compared with those who had never received or who had only past exposure to the drugs, after adjustment for the predicted 10-year risk of coronary heart disease.73 It should be noted that the D:A:D study is an observational database and initial interpretation could lead one to believe that the apparent association between these ART agents and increased MI rates likely reflect providers’ preferences to prescribe ABC to those subjects who have the highest cardiovascular risk. However, this does not explain why this association decreases when patients stop taking ABC for more than 6 months. The D:A:D database did not have adequate sample size to evaluate cardiovascular effects on those taking TDF, another preferred NRTI for those with high cardiovascular risk factors. Regardless of whether future studies demonstrate a similar risk with TDF, the underlying pathogenesis remains elusive and warrants further investigation.
Effects of ART on Global Cardiovascular Risk Estimates: Framingham Scores
An instructive approach to determining effects of HAART on cardiovascular risk in patients with HIV infection is to evaluate the change in global risk associated with such therapy. This has been done in a study that employed the Framingham equation to determine the 10-year risk of coronary heart disease at baseline and after 48 weeks of treatment with LPV/r + TDF + emtricitabine.74 At baseline, the mean 10-year coronary heart disease risk was 4.6%; at week 48, it was 5.0%. Study results indicated that 75% of patients had a 10-year risk lower than 7% at baseline and week 48, a level well below moderate to high risk (10%) or high risk (≥20%) according to this risk calculation system.74
Treatment to Reduce Cardiovascular Risk in Patients With HIV Infection
The Infectious Diseases Society of America (IDSA) and Adult ACTG have provided guidance for the treatment of dyslipidemia and reducing cardiovascular risk in patients with HIV infection. These guidelines borrow heavily from NCEP ATP III.16,47 In general, patients with dyslipidemia and HIV infection should be treated in a manner similar to the general population.75 Statin therapy is recommended for patients with hypercholesterolemia, but statins are likely to interact with PIs, particularly RTV, and must be used with caution. For example, pravastatin levels have been shown to increase 81% when this statin is given with darunavir plus RTV,76 whereas pravastatin levels are decreased with use of all other PIs. Hence, pravastatin is usually considered the “safest” statin to use in combination with PIs. Simvastatin and lovastatin should be avoided in patients being treated with PIs given the large increase in area under the curve (AUC).47,77,78 In contrast, simvastatin and atorvastatin levels decrease when given concomitantly with EFV.79 Recent results have also shown that rosuvastatin levels are increased in HIV-seronegative subjects who are being treated with LPV/r.80 Interestingly, in this study, the LDL-C responses to rosuvastatin while subjects were receiving LPV/r were diminished even though the rosuvastatin levels were higher. In a separate pharmacokinetic study by van der Lee et al81 in HIV-infected patients, the addition of rosuvastatin to LPV/r-based ART did not affect LPV/r concentrations, but rosuvastatin levels increased 1.6-fold compared with data obtained from healthy volunteers. The mean reductions in total cholesterol and LDL-C from baseline to week 4 on rosuvastatin 10 mg once a day were 27.6% and 31.8%, respectively. Newer agents from other classes, such as ezetimibe, have been shown to be safe and effective when used to lower cholesterol in patients with HIV infection.82–84
The IDSA/ACTG guidelines also recommend administration of gemfibrozil or fenofibrate for patients with hypertriglyceridemia.47,85 Dual therapy with a statin and a fibrate may be the best approach for achieving NCEP ATP III lipid targets in patients with HIV infection, as shown in a recent study of pravastatin plus fenofibrate in HIV-infected subjects.86,87 Study ACTG A5087 was a randomized trial of HIV-infected persons with combined hyperlipidemia who received either fenofibrate or pravastatin monotherapy for 12 weeks followed by dual-agent therapy for up to 48 weeks for those subjects who did not meet NCEP goals for LDL-C, HDL-C, and triglyceride levels. In addition to lipids, subjects were also analyzed for plasma levels of the proinflammatory marker, hs-CRP, along with atherogenic lipoprotein particle (a) and apolipoproteins A1/B, P-selectin (cell adhesion molecule), plasminogen activator inhibitor-1, and adiponectin. The majority of subjects (60/74 chosen subjects) switched to dual therapy at week 12 (n = 32, pravastatin added to fenofibrate monotherapy and n = 28, fenofibrate added to pravastatin). Results showed that from baseline to week 12, adiponectin, apoB levels, and Apo B/A1 ratios all significantly decreased in the pravastatin and fenofibrate arms, whereas lipoprotein particle (a) and Apo A1 increased significantly in the fenofibrate arm only (P = 0.01 for both measures). Combination therapy elicited improvements in lipid profiles without changes in the inflammatory and endothelial cell markers hs-CRP, plasminogen activator inhibitor-1, and P-selectin. From weeks 12–48, Apo B levels and Apo B/A1 ratios declined significantly in those subjects adding pravastin to fenofibrate (P < 0.01 and P = 0.01, respectively), whereas adiponectin levels significantly decreased in both combination treatment groups. These investigators suggested that HIV infection or other comorbid infections may inhibit the anti-inflammatory effects associated with lipid-lowering agents in non—HIV-infected persons.
Recent data have also demonstrated the lipid-lowering benefits with fish oils administered alone or with fenofibrate during ART. In a study of 100 patients enrolled in the A5186 prospective, phase 2 clinical trial, Gerber et al88 reported that twice-daily administration of fish oil supplement or once-daily fenofibrate reduced triglyceride levels by medians of 283 mg/dL (46%) and 367 mg/dL (58%), respectively. Patients not responding to either medication alone and treated subsequently with both agents demonstrated a 65.5% reduction from baseline in triglyceride levels. This combination therapy only achieved triglyceride levels of ≤200 mg/dL in 22.7% of study subjects; however, the median triglyceride level at baseline was 667 mg/dL. In a separate randomized study by De Truchis et al,89 thrice-daily administration of fish oil supplement for 8 weeks to HIV-infected patients on stable ART resulted in a median 25.5% decrease in serum triglycerides (n = 58) compared with only a 1% decrease in patients receiving a paraffin oil control (n = 62). In an open-label phase of the study, this effect was maintained through 16-week continued treatment with fish oil supplement, whereas patients switched from placebo to fish oil supplement demonstrated a 21.2% decrease in serum triglycerides.
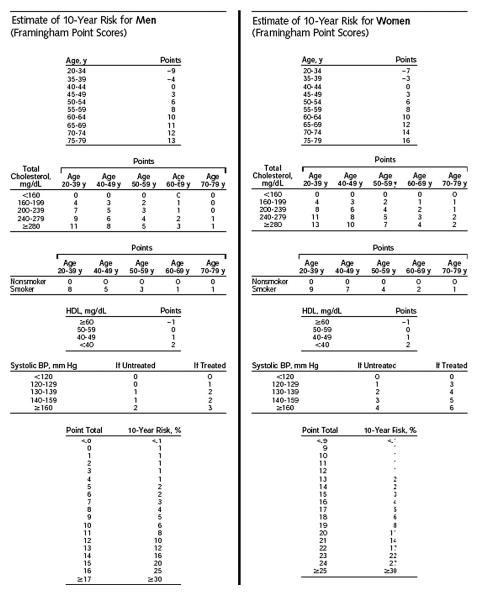
The IDSA/ACTG guidelines emphasize that altering a treatment regimen to improve the lipid profile may not deliver the anticipated result because of the multifactorial nature of dyslipidemia in patients receiving treatment for HIV infection.47 Results from clinical studies suggest that a change in HAART may have only limited effects on overall cardiovascular risk. A study of 88 patients with HIV infection assessed the metabolic effects of switching from a stable LPV/r-containing regimen to ATV + RTV. This switch decreased levels of total cholesterol and triglycerides, and the total cholesterol:HDL-C ratio, but produced only slight reductions in Framingham-calculated 10-year coronary heart disease risk.90 One important reason for this limited effect is that other factors, such as smoking status and blood pressure, contribute significantly to the overall risk calculated with this equation (Fig. 1).
FIGURE 1.
Framingham equation for calculation of 10-year risk of coronary heart disease.16
Patients on stable ART who have elevated lipids and atherogenic lipid profiles may nevertheless require therapeutic intervention in the form of either switching ART or administration of lipid-lowering agents concomitant with current HIV therapy. A recent randomized prospective study in HIV-infected patients with mixed hyperlipidemia on their first HAART regimen compared the lipid-lowering effects of switching from PI-based ART to either NVP-based or EFV-based ART or to treatment with either pravastatin or bezofibrate added to the current unchanged ART regimen for up to 12 months.91 These treatment strategies resulted in reductions in mean triglyceride levels of 25.2%, 9.4%, 41.2%, and 46.6%, respectively, with statistically significant differences noted between the NNRTI arms and the lipid-lowering agents (P < 0.01). In addition, treatment with pravastatin or bezofibrate resulted in significantly greater decreases in mean plasma total and LDL-C than those observed in the NVP-treated and EFV-treated patients.91
A recent comparative analysis of the metabolic effects of either lipid-lowering treatments (LLT) with switching from PI-based to NNRTI-based ART in patients enrolled in the D:A:D study showed significant reductions in total cholesterol with both LLT and ART switching compared with controls who received neither intervention.92 Between-group analysis showed that intervention with LLT resulted in greater mean reductions in total and LDL-C (nonsignificant difference), whereas switching to NNRTI-based ART resulted in a greater mean reduction in serum triglycerides (nonsignificant) and a significantly greater mean increase in HDL-C.92
The results of these studies support the benefits of interventions for dyslipidemia in patients with HIV infection. As an alternative strategy to switching ART regimens, the addition of certain LLT agents to ongoing ART may also provide the benefits associated with these agents, including improved cardiovascular outcomes resulting from decreased proinflammatory events and a reduction in atherogenic LDL-C levels.93,94
CONCLUSIONS
Patients infected with HIV share traditional cardiovascular disease risk factors with the general population. In addition, HIV infection itself significantly increases the risk of cardiovascular disease. Control of viremia with potent and durable regimens can help reduce overall risk. Thus, effective suppression of viral replication and management of traditional risk factors (eg, lipids, blood pressure, smoking) with conventional methods provide the best approach to lowering total cardiovascular risk in patients with HIV infection. Although there is evidence that HAART may have negative effects on the serum lipid profile, these are modest, and the incremental cardiovascular risk associated with HAART is small and may be managed with treatments (eg, statins, fibrates, ezetimibe) commonly used in the general population. Switching antiretroviral agents may not resolve lipid abnormalities and should be cautiously considered, weighing the small but potential risk of virologic failure. A determination of the absolute risk of coronary heart disease in individual patients with the use of Framingham score calculations or other global risk calculators can provide valuable guidance for patient management and treatment planning.
ACKNOWLEDGMENTS
Jeffery Brubaker, PhD of Science and Medicine, assisted in the development of this article. Dr. J.A.A. has received honoraria for serving on the advisory boards or for participating in CME events for Abbott, Boerhinger-Ingelheim, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Merck, Pfizer, Roche, and Tibotec. She is currently serving as an investigator on studies supported by Gilead, GlaxoSmith-Kline, Merck, Pfizer, and Tibotec.
Supported in part by the National Institute of Allergy and Infectious Diseases AIDS Clinical Trials Unit, Grant no. AI-AI068636 and New York University AIDS Clinical Trials Unit Grant no. AI-069532. Abbott Laboratories provided financial support of editorial services for this article, however, the nominal author, J.A.A., MD, did not receive any financial compensation.
Footnotes
Posters and oral presentations from the following scientific conferences were cited in this manuscript: 15th Conference on Retroviruses and Opportunistic Infections (CROI), February 3–6, 2008, Boston, MA; 14th CROI, February 25–28, 2007, Los Angeles, CA; 13th CROI, February 5–8, 2006, Denver, CO; 11th CROI, February 8–11, 2004, San Francisco, CA; 11th European AIDS Conference, October 25–26, 2007, Madrid, Spain; 4th International AIDS Society Conference, July 22–25, 2007, Sydney, Australia; 43rd American Society of Clinical Oncology Annual Meeting Educational Book, June 1–5, 2007, Chicago, IL; 8th International Workshop on Pharmacology of HIV Therapy, April 16–18, 2007, Budapest, Hungary; 8th International Congress on Drug Therapy in HIV Infection, November 12–16, 2006, Glasgow, United Kingdom; and 16th International AIDS Conference, August 13–18, 2006, Toronto, Canada.
REFERENCES
- 1.Palella FJ, Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 2.Koutkia P, Grinspoon S. HIV-associated lipodystrophy: pathogenesis, prognosis, treatment, and controversies. Annu Rev Med. 2004;55:303–317. doi: 10.1146/annurev.med.55.091902.104412. [DOI] [PubMed] [Google Scholar]
- 3.Mocroft A, Ledergerber B, Katlama C, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003;362:22–29. doi: 10.1016/s0140-6736(03)13802-0. [DOI] [PubMed] [Google Scholar]
- 4.Sepkowitz KA. AIDS—the first 20 years. N Engl J Med. 2001;344:1764–1772. doi: 10.1056/NEJM200106073442306. [DOI] [PubMed] [Google Scholar]
- 5.Manfredi R, Sabbatani S, Agostini D. Trend of mortality observed in a cohort of drug addicts of the metropolitan area of Bologna, North-Eastern Italy, during a 25-year-period. Coll Antropol. 2006;30:479–488. [PubMed] [Google Scholar]
- 6.U.S. Public Health Service Task Force [Accesssed July 8, 2008];Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV-1 transmission in the United States. Available at: http://AIDSinfo.nih.gov. [PubMed]
- 7.Wong MD, Shapiro MF, Boscardin WJ, et al. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 8.El-Sadr WM, Lundgren JD, Neaton JD, et al. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–2296. doi: 10.1056/NEJMoa062360. [DOI] [PubMed] [Google Scholar]
- 9.Emery S, the SMART Study Group and INSIGHT Major clinical outcomes in patients not treated with antiretroviral therapy (ART) at baseline in SMART: a rationale for a trial to examine early treatment of HIV disease. Presented at: 4th IAS Conference on HIV Pathogenesis, Treatment, and Prevention; Sydney, Australia. 2007. Abstract. [Google Scholar]
- 10.Choi AI, Rodriguez RA, Bacchetti P, et al. The impact of HIV on chronic kidney disease outcomes. Kidney Int. 2007;72:1380–1387. doi: 10.1038/sj.ki.5002541. [DOI] [PubMed] [Google Scholar]
- 11.Fernando SK, Finkelstein FO, Moore BA, et al. Prevalence of chronic kidney disease in an urban HIV infected population. Am J Med Sci. 2008;335:89–94. doi: 10.1097/MAJ.0b013e31812e6b34. [DOI] [PubMed] [Google Scholar]
- 12.Ledergerber B, Furrer H, Rickenbach M, et al. Factors associated with the incidence of type 2 diabetes mellitus in HIV-infected participants in the Swiss HIV Cohort Study. Clin Infect Dis. 2007;45:111–119. doi: 10.1086/518619. [DOI] [PubMed] [Google Scholar]
- 13.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 14.Mocroft A, Soriano V, Rockstroh J, et al. Is there evidence for an increase in the death rate from liver-related disease in patients with HIV? AIDS. 2005;19:2117–2125. doi: 10.1097/01.aids.0000194799.43799.ea. [DOI] [PubMed] [Google Scholar]
- 15.Costagliola D. Cancer risk and mortality for patients with HIV in the combination antiretroviral therapy era: evolving epidemiology. Presented at: 43rd American Society of Clinical Oncology Annual Meeting Educational Book; Chicago, IL. 2007. Abstract. [Google Scholar]
- 16.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 17.Reusch JE. Current concepts in insulin resistance, type 2 diabetes mellitus, and the metabolic syndrome. Am J Cardiol. 2002;90:19G–26G. doi: 10.1016/s0002-9149(02)02555-9. [DOI] [PubMed] [Google Scholar]
- 18.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 19.Savès M, Chene G, Ducimetière P, et al. Risk factors for coronary heart disease in patients treated for human immunodeficiency virus infection compared with the general population. Clin Infect Dis. 2003;37:292–298. doi: 10.1086/375844. [DOI] [PubMed] [Google Scholar]
- 20.El-Sadr WM, Mullin CM, Carr A, et al. Effects of HIV disease on lipid, glucose and insulin levels: results from a large antiretroviral-naive cohort. HIV Med. 2005;6:114–121. doi: 10.1111/j.1468-1293.2005.00273.x. [DOI] [PubMed] [Google Scholar]
- 21.Das S, Shahmanesh M, Stolinski M, et al. In treatment-naive and antiretroviral-treated subjects with HIV, reduced plasma adiponectin is associated with a reduced fractional clearance rate of VLDL, IDL and LDL apolipoprotein B-100. Diabetologia. 2006;49:538–542. doi: 10.1007/s00125-005-0085-3. [DOI] [PubMed] [Google Scholar]
- 22.Blum A, Hadas V, Burke M, et al. Viral load of the human immunodeficiency virus could be an independent risk factor for endothelial dysfunction. Clin Cardiol. 2005;28:149–153. doi: 10.1002/clc.4960280311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Saint Martin L, Pasquier E, Vandhuick O, et al. Correlations between carotid IMT, factor VIII activity level and metabolic disturbances: a cardio-vascular risk factor in the HIV positive persons. Curr HIV Res. 2007;5:361–364. doi: 10.2174/157016207780636498. [DOI] [PubMed] [Google Scholar]
- 24.Hsue PY, Lo JC, Franklin A, et al. Progression of atherosclerosis as assessed by carotid intima-media thickness in patients with HIV infection. Circulation. 2004;109:1603–1608. doi: 10.1161/01.CIR.0000124480.32233.8A. [DOI] [PubMed] [Google Scholar]
- 25.Hsue PY, Hunt PW, Sinclair E, et al. Increased carotid intima-media thickness in HIV patients is associated with increased cytomegalovirus-specific T-cell responses. AIDS. 2006;20:2275–2283. doi: 10.1097/QAD.0b013e3280108704. [DOI] [PubMed] [Google Scholar]
- 26.Tien PC, Benson C, Zolopa AR, et al. The study of fat redistribution and metabolic change in HIV infection (FRAM): methods, design, and sample characteristics. Am J Epidemiol. 2006;163:860–869. doi: 10.1093/aje/kwj111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maggi P, Lillo A, Perilli F, et al. Colour-Doppler ultrasonography of carotid vessels in patients treated with antiretroviral therapy: a comparative study. AIDS. 2004;18:1023–1028. doi: 10.1097/00002030-200404300-00010. [DOI] [PubMed] [Google Scholar]
- 28.Badiou S, De Boever C Merle, Dupuy AM, et al. Decrease in LDL size in HIV-positive adults before and after lopinavir/ritonavir-containing regimen: an index of atherogenicity? Atherosclerosis. 2003;168:107–113. doi: 10.1016/s0021-9150(03)00058-3. [DOI] [PubMed] [Google Scholar]
- 29.Lau B, Sharrett AR, Kingsley LA, et al. C-reactive protein is a marker for human immunodeficiency virus disease progression. Arch Intern Med. 2006;166:64–70. doi: 10.1001/archinte.166.1.64. [DOI] [PubMed] [Google Scholar]
- 30.Sitia G, De Bona A, Bagaglio S, et al. Naive HIV/HCV-coinfected patients have higher intrahepatic pro-inflammatory cytokines than coinfected patients treated with antiretroviral therapy. Antivir Ther. 2006;11:385–389. [PubMed] [Google Scholar]
- 31.Mynarcik DC, McNurlan MA, Steigbigel RT, et al. Association of severe insulin resistance with both loss of limb fat and elevated serum tumor necrosis factor receptor levels in HIV lipodystrophy. J Acquir Immune Defic Syndr. 2000;25:312–321. doi: 10.1097/00042560-200012010-00004. [DOI] [PubMed] [Google Scholar]
- 32.Kristoffersen US, Kofoed K, Kronborg G, et al. Changes in circulating markers of endothelial function in HIV patients starting combination antiretroviral therapy. Presented at: 15th Conference on Retroviruses and Opportunistic Infections (CROI); Boston, MA. 2008. Abstract. [Google Scholar]
- 33.Ross AC, Rizk N, O’Riordan MA, et al. Inflammatory markers correlate with carotid intima-media thickness and endothelial activation in HIV-infected patients. Presented at: 15th Conference on Retroviruses and Opportunistic Infections (CROI); Boston, MA. 2008. Abstract. [Google Scholar]
- 34.Prineas R, Roediger M, Carr A, et al. Effect of alternate treatment protocols on the incidence of electrocardiographic abnormalities among HIV infected adults in the SMART trial. Presented at: 4th International AIDS Society (IAS) Conference on HIV Pathogenesis, Treatment and Prevention; Sydney, Australia. 2007. Abstract. [Google Scholar]
- 35.Kuller L, the SMART Study Group Elevated levels of interleukin-6 and D-dimer are associated with an increased risk of death in patients with HIV. Presented at: 15th Conference on Retroviruses and Opportunistic Infections; Boston, MA. 2008. Abstract. [Google Scholar]
- 36.Calmy A, Nguyen A, Montecucco F, et al. HIV activates markers of cardiovascular risk in a randomized treatment interruption trial: STACCATO. Presented at: 15th Conference on Retroviruses and Opportunistic Infections (CROI); Boston, MA. 2008. Abstract. [Google Scholar]
- 37.Phillips A, Carr A, Neuhaus J, et al. Interruption of ART and risk of cardiovascular disease in persons with HIV-1 infection: exploratory analyses from the SMART Trial. Antivir Ther. 2008;13:177–187. doi: 10.1177/135965350801300215. [DOI] [PubMed] [Google Scholar]
- 38.Lichtenstein K, Armon C, Buchacz K, et al. Analysis of cardiovascular risk factors in the HIV outpatient study cohort. Presented at: 13th Conference on Retroviruses and Opportunistic Infections (CROI); Denver, CO. 2006. Abstract. [Google Scholar]
- 39.Mary-Krause M, Cotte L, Simon A, et al. Increased risk of myocardial infarction with duration of protease inhibitor therapy in HIV-infected men. AIDS. 2003;17:2479–2486. doi: 10.1097/00002030-200311210-00010. [DOI] [PubMed] [Google Scholar]
- 40.Bozzette SA, Ake CF, Tam HK, et al. Cardiovascular and cerebrovascular events in patients treated for human immunodeficiency virus infection. N Engl J Med. 2003;348:702–710. doi: 10.1056/NEJMoa022048. [DOI] [PubMed] [Google Scholar]
- 41.Vaughn G, Detels R. Protease inhibitors and cardiovascular disease: analysis of the Los Angeles County adult spectrum of disease cohort. AIDS Care. 2007;19:492–499. doi: 10.1080/09540120701203329. [DOI] [PubMed] [Google Scholar]
- 42.D:A:D Study Group. Friis-Moller N, Reiss P, et al. Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med. 2007;356:1723–1735. doi: 10.1056/NEJMoa062744. [DOI] [PubMed] [Google Scholar]
- 43.Stein JH. Cardiovascular risks of antiretroviral therapy. N Engl J Med. 2007;356:1773–1775. doi: 10.1056/NEJMe078037. [DOI] [PubMed] [Google Scholar]
- 44.Currier J, Kendall M, Henry K, et al. Progression of carotid intima-media thickening in HIV-infected and uninfected adults: ACTG 5078. AIDS. 2007;21:1137–1145. doi: 10.1097/QAD.0b013e32811ebf79. [DOI] [PubMed] [Google Scholar]
- 45.Torriani F, Komarow L, Cotter B, et al. Control of HIV viral replication is associated with rapid improvement in endothelial function sustained over 24 weeks: A5152s, a substudy of A5142. Presented at: 4th International AIDS Society (IAS) Conference on HIV Pathogenesis, Treatment and Prevention; Sydney, Australia. 2007. Abstract. [Google Scholar]
- 46.Hadigan C, Meigs JB, Corcoran C, et al. Metabolic abnormalities and cardiovascular disease risk factors in adults with human immunodeficiency virus infection and lipodystrophy. Clin Infect Dis. 2001;32:130–139. doi: 10.1086/317541. [DOI] [PubMed] [Google Scholar]
- 47.Dubé MP, Stein JH, Aberg JA, et al. Guidelines for the evaluation and management of dyslipidemia in human immunodeficiency virus (HIV)-infected adults receiving antiretroviral therapy: recommendations of the HIV Medical Association of the Infectious Disease Society of America and the Adult AIDS Clinical Trials Group. Clin Infect Dis. 2003;37:613–627. doi: 10.1086/378131. [DOI] [PubMed] [Google Scholar]
- 48.Brown TT, Cole SR, Li X, et al. Prevalence and incidence of pre-diabetes and diabetes in the multicenter AIDS cohort study. Presented at: 11th Conference on Retroviruses and Opportunistic Infections (CROI); San Francisco, CA. 2004. Abstract. [Google Scholar]
- 49.Riddler SA, Smit E, Cole SR, et al. Impact of HIV infection and HAART on serum lipids in men. JAMA. 2003;289:2978–2982. doi: 10.1001/jama.289.22.2978. [DOI] [PubMed] [Google Scholar]
- 50.Bergersen BM. Cardiovascular risk in patients with HIV Infection: impact of antiretroviral therapy. Drugs. 2006;66:1971–1987. doi: 10.2165/00003495-200666150-00006. [DOI] [PubMed] [Google Scholar]
- 51.Fisac C, Fumero E, Crespo M, et al. Metabolic benefits 24 months after replacing a protease inhibitor with abacavir, efavirenz or nevirapine. AIDS. 2005;19:917–925. doi: 10.1097/01.aids.0000171405.46113.bf. [DOI] [PubMed] [Google Scholar]
- 52.Dupon M, Livrozet J-M, Morand-Joubert L, et al. Lipid-profile of lopinavir/ritonavir (LPV/r) in an 18-month French observational prospective cohort (Kaleobs cohort). Presented at: 8th International Congress on Drug Therapy in HIV Infection; Glasgow, United Kingdom. 2006. [Google Scholar]
- 53.Montes ML, Pulido F, Barros C, et al. Lipid disorders in antiretroviralnaive patients treated with lopinavir/ritonavir-based HAART: frequency, characterization and risk factors. J Antimicrob Chemother. 2005;55:800–804. doi: 10.1093/jac/dki063. [DOI] [PubMed] [Google Scholar]
- 54.Lafeuillade A, Hittinger G, Philip G, et al. Metabolic evaluation of HIV-infected patients receiving a regimen containing lopinavir/ritonavir (Kaletra) HIV Clin Trials. 2004;5:392–398. doi: 10.1310/Q0TG-0V50-9JML-638U. [DOI] [PubMed] [Google Scholar]
- 55.Eron J, Jr, Yeni P, Gathe J, Jr, et al. The KLEAN study of fosamprenavirritonavir versus lopinavir-ritonavir, each in combination with abacavirlamivudine, for initial treatment of HIV infection over 48 weeks: a randomised non-inferiority trial. Lancet. 2006;368:476–482. doi: 10.1016/S0140-6736(06)69155-1. [DOI] [PubMed] [Google Scholar]
- 56.Haubrich R, Riddler S, DiRienzo G, et al. Metabolic outcomes of ACTG 5142: a prospective, randomized phase III trial of NRTI-, PI-, and NNRTI-sparing regimens for initial treatment of HIV-1. Presented at: 14th Conference on Retroviruses and Opportunistic Infections (CROI); Los Angeles, CA. 2007. Abstract. [Google Scholar]
- 57.Kerr SJ, Duncombe C, Avihingsanon A, et al. Dyslipidemia in an Asian population after treatment for two years with protease inhibitor-containing regimens. J Int Assoc Physicians AIDS Care (Chic Ill) 2007;6:36–46. doi: 10.1177/1545109706295946. [DOI] [PubMed] [Google Scholar]
- 58.Fischl MA, Collier AC, Mukherjee AL, et al. Randomized open-label trial of two simplified, class-sparing regimens following a first suppressive three or four-drug regimen. AIDS. 2007;21:325–333. doi: 10.1097/QAD.0b013e328011ddfa. [DOI] [PubMed] [Google Scholar]
- 59.Tebas P, Zhang J, Yarasheski K, et al. Switching to a protease inhibitor-containing, nucleoside-sparing regimen (lopinavir/ritonavir plus efavirenz) increases limb fat but raises serum lipid levels: results of a prospective randomized trial (AIDS clinical trial group 5125s) J Acquir Immune Defic Syndr. 2007;45:193–200. doi: 10.1097/QAI.0b013e318042e204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smith KY, Weinberg WG, Dejesus E, et al. Fosamprenavir or atazanavir once daily boosted with ritonavir 100 mg, plus tenofovir/emtricitabine, for the initial treatment of HIV infection: 48-week results of ALERT. AIDS Res Ther. 2008;5:5. doi: 10.1186/1742-6405-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hicks C, DeJesus E, Wohl D, et al. Once-daily fosamprenavir (FPV) boosted with either 100 mg or 200 mg of ritonavir (r) along with abacavir (ABC)/lamivudine (3TC): 48 week safety and efficacy: results from COL100758. Presented at: 11th European AIDS Conference; Madrid, Spain. October 25–26, 2007; Abstract. [Google Scholar]
- 62.Shafran SD, Mashinter LD, Roberts SE. The effect of low-dose ritonavir monotherapy on fasting serum lipid concentrations. HIV Med. 2005;6:421–425. doi: 10.1111/j.1468-1293.2005.00328.x. [DOI] [PubMed] [Google Scholar]
- 63.Malan DR, Krantz E, David N, et al. Efficacy and safety of atazanavir, with and without ritonavir as part of once-daily highly active antiretroviral therapy regimens in antiretroviral naive patients, 089 Study Group. J Acquir Immune Defic Syndr. 2008;47:161–167. doi: 10.1097/QAI.0b013e31815ace6a. [DOI] [PubMed] [Google Scholar]
- 64.Trein A, Schnaitmann E, Richter WO. Lipids and lipoproteins in HIV-subjects treated with lopinavir/ritonavir (L) or atazanavir/ritonavir (A) based antiretroviral therapy. Presented at: 8th International Congress on Drug Therapy in HIV Infection; Glasgow, United Kingdom. 2006. Abstract. [Google Scholar]
- 65.Elion R, DeJesus E, Sension M, et al. Once-daily abacavir/lamivudine and ritonavir-boosted atazanavir for the treatment of HIV-1 infection in antiretroviral-naïve patients: a 48-week pilot study. HIV Clin Trials. 2008;9:152–163. doi: 10.1310/hct0903-152. [DOI] [PubMed] [Google Scholar]
- 66.Walmsley S, Ruxrungtham K, Slim J, et al. Saquinavir/r (SQV/r) BID versus lopinavir/r (LPV/r) BID, plus emtricitabine/tenofovir (FTC/TDF) QD as initial therapy in HIV-1-infected patients: the Gemini Study. Presented at: 11th European AIDS Conference (EACS); Madrid, Spain. 2007. Abstract. [Google Scholar]
- 67.Gathe J, Jr, da Silva BA, Loutfy M, et al. Study M05-730 primary efficacy results at week 48: phase 3, randomized, open-label study of lopinavir/ritonavir (LPV/r) tablets once daily (QD) versus twice daily (BID), co-administered with tenofovir DF (TDF) + emtricitabine (FTC) in antiretroviral-naïve (ARV) HIV-1 infected subjects. Presented at: 15th Conference on Retroviruses and Opportunistic Infections (CROI); Boston, Ma. 2008. Abstract. [Google Scholar]
- 68.Shikuma CM, Yang Y, Glesby MJ, et al. Metabolic effects of protease inhibitor-sparing antiretroviral regimens given as initial treatment of HIV-1 infection (AIDS Clinical Trials Group Study A5095) J Acquir Immune Defic Syndr. 2007;44:540–550. doi: 10.1097/QAI.0b013e318031d5a0. [DOI] [PubMed] [Google Scholar]
- 69.van Leth F, Phanuphak P, Stroes E, et al. Nevirapine and efavirenz elicit different changes in lipid profiles in antiretroviral-therapy-naive patients infected with HIV-1. PLoS Med. 2004;1:e19. doi: 10.1371/journal.pmed.0010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hammond E, Nolan D, James I, et al. Reduction of mitochondrial DNA content and respiratory chain activity occurs in adipocytes within 6-12 months of commencing nucleoside reverse transcriptase inhibitor therapy. AIDS. 2004;18:815–817. doi: 10.1097/00002030-200403260-00015. [DOI] [PubMed] [Google Scholar]
- 71.Carr A, Miller J, Law M, et al. A syndrome of lipoatrophy, lactic acidaemia and liver dysfunction associated with HIV nucleoside analogue therapy: contribution to protease inhibitor-related lipodystrophy syndrome. AIDS. 2000;14:F25–F32. doi: 10.1097/00002030-200002180-00001. [DOI] [PubMed] [Google Scholar]
- 72.Kumar PN, Rodriguez-French A, Thompson MA, et al. A prospective, 96-week study of the impact of Trizivir, Combivir/nelfinavir, and lamivudine/stavudine/nelfinavir on lipids, metabolic parameters and efficacy in antiretroviral-naive patients: effect of sex and ethnicity. HIV Med. 2006;7:85–98. doi: 10.1111/j.1468-1293.2006.00346.x. [DOI] [PubMed] [Google Scholar]
- 73.Sabin CA, Worm SW, Weber R, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet. 2008;371:1417–1426. doi: 10.1016/S0140-6736(08)60423-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gathe J, Podzamczer D, Johnson M, et al. Once-daily vs. twice-daily lopinavir/ritonavir in antiretroviral-naïve patients: 48-week results. Presented at: 11th Conference on Retroviruses and Opportunistic Infections (CROI); San Francisco, CA. 2004. Abstract. [Google Scholar]
- 75.Tungsiripat M, Aberg JA. Dyslipidemia in HIV patients. Cleve Clin J Med. 2005;72:1113–1120. doi: 10.3949/ccjm.72.12.1113. [DOI] [PubMed] [Google Scholar]
- 76.Sekar V, Spinosa-Guzman S, Marien K. Pharmacokinetic drug-drug interaction between the new HIV protease inhibitor darunavir (TMC114) and the lipid-lowering agent pravastatin. Presented at: 8th International Workshop on Pharmacology of HIV Therapy; Budapest, Hungary. April 16-18, 2007; Abstract. [Google Scholar]
- 77.Fichtenbaum CJ, Gerber JG. Interactions between antiretroviral drugs and drugs used for the therapy of the metabolic complications encountered during HIV infection. Clin Pharmacokinet. 2002;41:1195–1211. doi: 10.2165/00003088-200241140-00004. [DOI] [PubMed] [Google Scholar]
- 78.Moyle GJ, Lloyd M, Reynolds B, et al. Dietary advice with or without pravastatin for the management of hypercholesterolaemia associated with protease inhibitor therapy. AIDS. 2001;15:1503–1508. doi: 10.1097/00002030-200108170-00007. [DOI] [PubMed] [Google Scholar]
- 79.Gerber JG, Rosenkranz SL, Fichtenbaum CJ, et al. Effect of efavirenz on the pharmacokinetics of simvastatin, atorvastatin, and pravastatin: results of AIDS Clinical Trials Group 5108 Study. J Acquir Immune Defic Syndr. 2005;39:307–312. doi: 10.1097/01.qai.0000167156.44980.33. [DOI] [PubMed] [Google Scholar]
- 80.Kiser JJ, Gerber JG, Predhomme JA, Wolfe P, et al. Drug/drug interaction between lopinavir/ritonavir and rosuvastatin in healthy volunteers. J Acquir Immune Defic Syndr. 2008;47:570–578. doi: 10.1097/QAI.0b013e318160a542. [DOI] [PubMed] [Google Scholar]
- 81.van der Lee M, Sankatsing R, Schippers E, et al. Pharmacokinetics and pharmacodynamics of combined use of lopinavir/ritonavir and rosuvastatin in HIV-infected patients. Antivir Ther. 2007;12:1127–1132. [PubMed] [Google Scholar]
- 82.Negredo E, Molto J, Puig J, et al. Ezetimibe, a promising lipid-lowering agent for the treatment of dyslipidaemia in HIV-infected patients with poor response to statins. AIDS. 2006;20:2159–2164. doi: 10.1097/01.aids.0000247573.95880.db. [DOI] [PubMed] [Google Scholar]
- 83.Wohl D, Hsue P, Richard S, et al. Ezetimibe’s effects on the LDL cholesterol levels of HIV-infected patients receiving HAART. Presented at: 14th Conference on Retroviruses and Opportunistic Infections (CROI); Los Angeles, CA. 2007. Abstract. [Google Scholar]
- 84.Bennett MT, Johns KW, Bondy GP. Ezetimibe is effective when added to maximally tolerated lipid lowering therapy in patients with HIV. Lipids Health Dis. 2007;6:15. doi: 10.1186/1476-511X-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Miller J, Brown D, Amin J, et al. A randomized, double-blind study of gemfibrozil for the treatment of protease inhibitor-associated hypertriglyceridaemia. AIDS. 2002;16:2195–2200. doi: 10.1097/00002030-200211080-00012. [DOI] [PubMed] [Google Scholar]
- 86.Aberg JA, Zackin RA, Brobst SW, et al. A randomized trial of the efficacy and safety of fenofibrate versus pravastatin in HIV-infected subjects with lipid abnormalities: AIDS Clinical Trials Group Study 5087. AIDS Res Hum Retroviruses. 2005;21:757–767. doi: 10.1089/aid.2005.21.757. [DOI] [PubMed] [Google Scholar]
- 87.Fichtenbaum CJ, Yeh T-M, Evans SR, et al. Changes in markers of atherogenic dyslipidemia, inflammation, and platelet activation with treatment with pravastatin, fenofibrate, or the combination: results from ACTG A5087. Presented at: 15th Conference on Retroviruses and Opportunistic Infections (CROI); Boston, MA. 2008. Abstract. [Google Scholar]
- 88.Gerber JG, Kitch DW, Fichtenbaum CJ, et al. Fish oil and fenofibrate for the treatment of hypertriglyceridemia in HIV-infected subjects on antiretroviral therapy: results of ACTG A5186. J Acquir Immune Defic Syndr. 2008;47:459–466. doi: 10.1097/QAI.0b013e31815bace2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.De Truchis P, Kirstetter M, Perier A, et al. Reduction in triglyceride level with N-3 polyunsaturated fatty acids in HIV-infected patients taking potent antiretroviral therapy: a randomized prospective study. J Acquir Immune Defic Syndr. 2007;44:278–285. doi: 10.1097/QAI.0b013e31802c2f3d. [DOI] [PubMed] [Google Scholar]
- 90.Guillemi S, Toulson A, Joy R, et al. Changes in lipid profile upon switching from lopinavir/ritonavir (LPV/r) to atazanavir + ritonavir (ATZ + RTV) based HAART. Presented at: XVI International AIDS Conference; Toronto, Canada. 2006. Abstract. [Google Scholar]
- 91.Calza L, Manfredi R, Colangeli V, et al. Substitution of nevirapine or efavirenz for protease inhibitor versus lipid-lowering therapy for the management of dyslipidaemia. AIDS. 2005;19:1051–1058. doi: 10.1097/01.aids.0000174451.78497.8f. [DOI] [PubMed] [Google Scholar]
- 92.Van Der Valk M, Friis-øller N, Sabin C, et al. Effect of interventions to improve dyslipidaemia. Presented at: 8th International Congress on Drug Therapy in HIV Infection; Glasgow, United Kingdom. 2006. Abstract. [Google Scholar]
- 93.Rosenson RS. Low high-density lipoprotein cholesterol and cardiovascular disease: risk reduction with statin therapy. Am Heart J. 2006;151:556–563. doi: 10.1016/j.ahj.2005.03.049. [DOI] [PubMed] [Google Scholar]
- 94.Kostis JB. The importance of managing hypertension and dyslipidemia to decrease cardiovascular disease. Cardiovasc Drugs Ther. 2007;21:297–309. doi: 10.1007/s10557-007-6032-4. [DOI] [PubMed] [Google Scholar]