Abstract
We analyzed HIV gp41 from 195 men in the United States who were HIV-1 infected between 1999 and 2002, before enfuvirtide (ENF) was approved for clinical use in the United States. gp41 genotyping results were obtained for 175 samples. None of the samples had major ENF resistance mutations. Six (3.4%) samples had minor ENF resistance mutations in the HR1 region (V38G, N43K, L44M, L45M). Twenty-eight (16%) samples had the N42S polymorphism, which is associated with ENF hypersusceptibility. Accessory mutations in the HR2 region were identified in some samples (E137K, S138A). Five of the six samples with HR1 resistance mutations were analyzed with a phenotypic assay; one sample had reduced ENF susceptibility (a sample with N42S + L44M + E137K). Prior to the availability of ENF, some men in the United States were infected with HIV that contained mutations associated with ENF resistance or hypersusceptibility. However, most of the mutations were not associated with phenotypic ENF resistance.
The HIV envelope glycoproteins gp120 and gp41 interact with cell surface proteins to mediate entry of HIV into target cells. The ectodomain of gp41 contains two highly conserved heptad repeat domains, HR1 and HR2. These domains interact to form a six-helix bundle that is critical for viral fusion.1,2 In 2003, the United States Food and Drug Administration (FDA) licensed the first HIV fusion inhibitor, enfuvirtide (ENF, Hoffmann-La Roche, Nutley, NJ).2 ENF is a 36-amino acid polypeptide that mimics the gp41 HR2 domain and prevents the formation of the six-helix bundle. This consequently blocks the entry of HIV into target cells.2 Resistance to ENF has been associated with mutations in the HR1 domain at codons 36–45.1,2 Mutations outside of this region and in the HR2 domain may also serve as secondary mutations.2
In this report, we analyzed HIV-1 gp41 HR1 and HR2 sequences from recently infected men from six major cities in the United States. A phenotypic assay was also used to measure the ENF susceptibility in a subset of the samples. Plasma or serum samples were obtained from the EXPLORE Study, a randomized clinical trial that examined the efficacy of a behavioral intervention for prevention of HIV acquisition in men who have sex with men (MSM).3 HIV-negative MSM (n = 4295) were enrolled in the study between 1999 and 2001 at sites in Boston, Chicago, Denver, New York, San Francisco, and Seattle. Men received either a behavioral intervention or standard risk reduction counseling, and were tested every 6 months for HIV infection. In the course of the study, 259 men acquired HIV infection. In a previous study, we genotyped HIV protease and reverse transcriptase, and determined the HIV subtype in the first HIV-positive sample from these men.4 One hundred and ninety-five of the HIV seroconverters had a genotypic resistance result.4 HIV from 31 (15.9%) of 195 men had evidence of resistance to either reverse transcriptase inhibitors or protease inhibitors, including seven who had evidence of multiclass resistance.4 All samples had subtype B HIV. The EXPLORE study was approved by the institutional review boards at each of the participating institutions and participants provided written informed consent.
In this study, gp41 genotyping was performed using research reagents and protocols (Celera). Methods for gp41 genotyping, which include HIV RNA extraction, reverse transcription, PCR amplification, DNA sequencing, and analysis of gp41 sequences, are described in a previous report.5 gp41 sequences from the EXPLORE samples were compared to the HXB2 reference sequence (GenBank accession number K03455) and were examined for the presence of mutations in the HR1 region that have been associated with ENF resistance or hypersusceptibility, and accessory mutations in HR2 that may increase the fitness of viruses with ENF mutations; the Stanford HIV Resistance Database was used as a reference (updated 6/10/08).6 The mutations analyzed included (1) mutations in HR1 that are associated with a > 10-fold reduction in most clinical isolates and site-directed mutants (major mutations: G36D/E, V38A/E, Q40H, and N43D), (2) other ENF resistance mutations in HR1 (G36S/V, I37V, V38G/M, N42T, N43K, L44M, and L45M), (3) N42S, a natural polymorphism in HR1 that has been associated with ENF hyper-susceptibility, and (4) HR2 accessory mutations (N126K, E137K, and S138A).6 gp41 sequences were deposited in Gen-Bank (accession numbers EU709526–EU709700).
All of the 195 HIV seroconverters in the EXPLORE cohort who were analyzed previously for genotypic resistance to reverse transcriptase and protease inhibitors had an HIV RNA sample from the time of HIV diagnosis available for analysis of the gp41 region. DNA encoding the gp41 region was successfully amplified from 176 (90.3%) of the 195 samples. Failure to amplify the remaining samples may reflect the fact that stored HIV RNA extracts were used for analysis, rather than plasma samples. In a previous study using the same gp41 genotyping system, all of the 11 subtype B samples tested were successfully amplified.5 Sequencing of gp41 was successful for 175 (99.4%) of the 176 amplified samples. Bidirectional sequences were obtained for all but eight of those samples; sequencing failed with the forward primer for four samples, and with the reverse primer for four samples.
Minor ENF resistance mutations were identified in six samples; none of the samples had major ENF resistance mutations (Fig. 1 and Table 1). V38G was detected in samples from two men, one of whom also had resistance to nucleoside reverse transcriptase inhibitors (NRTIs; zidovudine and stavudine, with possible resistance to didanosine and tenofovir), nonnucleoside reverse transcriptase inhibitors (NNRTIs; nevirapine, delavirdine, and efavirenz), and protease inhibitors (PIs; indinavir, saquinavir, ritonavir, and nelfinavir, with possible resistance to amprenavir, fosamprenavir, lopinavir, and atazanavir). L44M was detected in three men who had no evidence of resistance to other antiretroviral drugs. One man had two ENF resistance mutations: L43K and L45M; that man also had resistance to all three NNRTIs (nevirapine, delavirdine, and efavirenz). The N42S polymorphism was detected in 28 (16%) of the 175 samples, including two samples that also had L44M, one of which also had E137K (see below).
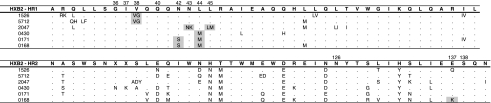
FIG. 1.
HR1 (top) and HR2 (bottom) sequences from the six men who had ENF resistance mutations detected were aligned and compared to the HXB2 reference sequence (shown above each alignment in bold). Dots are used to indicate that the amino acid in the test sequence matched the amino acid in the HXB2 sequence. Mutations associated with ENF resistance or hypersusceptibility are shaded. Amino acid mixtures are indicated (e.g., QM). Some ENF resistance mutations were detected as mixtures with the wild-type (HXB2) codons (V38A in samples #1526 and #5712; N43K and L45M in sample #2047); mutations in the other samples were present as the major sequence (no mixture detected).
Table 1.
HIV gp41 Amino Acid Polymorphisms in the HR1 Regiona
| AA# | HXB2 | ENF Res (HS)b | Amino acid polymorphisms in test samplesc |
|---|---|---|---|
| 30 | A | 1T | |
| 31 | R | 2K | |
| 32 | Q | 47L, 2S, 2N, 1M, 1E, 1V, 1H | |
| 33 | L | 1F | |
| 34 | L | 1M | |
| 35 | S | 1T, 1F | |
| 36 | G | G36D/E/S/V | |
| 37 | I | I37V | |
| 38 | V | V38A/E/G/M | 2G |
| 39 | Q | 1Rd | |
| 40 | Q | Q40H | |
| 41 | Q | ||
| 42 | N | N42T/(S) | (28S) |
| 43 | N | N43D/K/S | 1Ke |
| 44 | L | L44M | 3M |
| 45 | L | L45M | 1Me |
| 46 | R | 18K, 4M, 1Q | |
| 47 | A | 1X=A/F/S/V | |
| 48 | I | 1V, 1L | |
| 49 | E | 3Q, 3D | |
| 50 | A | ||
| 51 | Q | 1H | |
| 52 | Q | 1H | |
| 53 | H | 5R | |
| 54 | L | 40M, 2I, 2V | |
| 55 | L | 1V, 1W | |
| 56 | Q | 1R, 1X=Q/K/R | |
| 57 | L | 1I | |
| 58 | T | 1I | |
| 59 | V | 1I | |
| 60 | W | ||
| 61 | G | ||
| 62 | I | ||
| 63 | K | ||
| 64 | Q | ||
| 65 | L | ||
| 66 | Q | 4R | |
| 67 | A | ||
| 68 | R | ||
| 69 | I | 157V, 3L | |
| 70 | L |
This table shows the single letter code for the amino acid at each position (AA#) in the HXB2 reference strain (HXB2).
Mutations and amino acid polymorphisms that are associated with enfuvirtide (ENF) resistance are shown (ENF Res, rows 36–38, 40, and 42–45); mutations associated with >10× reduction in ENF susceptibility are underlined.7 The N42S mutation is associated with ENF hypersusceptibility (HS, indicated with parentheses).
Amino acids identified in the test samples that differ from the HXB2 sequence are shown using the single letter code. The number of test samples with each amino acid difference is shown (e.g., at position 30 in the HR1 region, one sample has the A30T substitution). Many of the amino acid substitutions were present as a mixture with the amino acid present in the HXB2 sequence (not shown). X indicates the presence of a degenerate nucleotide codon that encodes two or more amino acids in addition to the amino acid presence in the HXB2 sequence; in this case, the amino acids encoded at that position are shown (e.g., in one sample, the amino acids A = alanine, F = phenylalanine, S = serine, and V = valine are encoded at position 47). ENF resistance mutations were also detected in some samples (bold).
Q39R is included in the International AIDS Society-USA list of ENF resistance mutations (13).
The mutations N43K and L45M were detected in the same study subject.
Polymorphisms in the HR2 region (e.g., N126K, E137K, and S138A) may increase the fitness of HIV-1 viruses that have ENF resistance mutations in HR1.6 We detected E137K in 27 (15.4%) of the samples and detected S138A in 15 (8.6%) of the samples; four samples had both of these polymorphisms. Five samples with E137K and one sample with S138A also had N42S; one sample with E137K also had N42S and L44M. Other HR2 polymorphisms were identified in the EXPLORE samples (Table 2).
Table 2.
HIV gp41 Amino Acid Polymorphisms in the HR2 Regiona
| AA# | HXB2 | ENF Resb | Amino acid polymorphisms in test samplesc |
|---|---|---|---|
| 100 | N | 1K | |
| 101 | A | 78T, 12N, 6D, 5V, 4S, 1K, 1I, 1G, 1X=A/D/I/N/T/Y | |
| 102 | S | 4T, 1N | |
| 103 | W | ||
| 103–4 | — | 1SK | |
| 104 | S | ||
| 104–5 | — | 3N, 3K, 1SKG, 1H | |
| 105 | N | 2S, 1X=N/K/R/S | |
| 106 | K | 24R, 1N | |
| 106–7 | — | 1TN, 1SLKD | |
| 107 | S | 10N, 22T, 1A, 1D, 1X=S/A/D/Y | |
| 108 | L | 18Y, 10V, 9Q, 9M, 5H, 5F, 2I, 1E, 1W | |
| 109 | E | 84D, 34N, 14S, 7K, 4H, 2G, 2T, 1R, 1A, 1X=N/S; 1X=D/I/N/V | |
| 110 | Q | 42E, 35D, 24K, 19Y, 8T, 5N, 5M, 3S, 4A, 2F, 2R, 1H, 1I, 1V, 1X=D/E/Y | |
| 111 | I | 1V | |
| 112 | W | ||
| 112–3 | — | 1E | |
| 113 | N | 62D, 19G, 16E, 6Q, 5K, 4H, 2N, 1S | |
| 114 | H | 170N, 2H, 2K, 1S | |
| 115 | T | 168M, 4L, 1K, 1X=H/I/K | |
| 116 | T | ||
| 117 | W | ||
| 118 | M | 4R, 2I, 1L | |
| 119 | E | 85Q, 7D, 2K, 1A | |
| 120 | W | ||
| 121 | D | 158E | |
| 122 | R | 72K | |
| 123 | E | ||
| 124 | I | 1V | |
| 125 | N | 126D, 12S, 10E, 1A, 1H | |
| 126 | N | N126K | 1D |
| 127 | Y | 1H | |
| 128 | T | ||
| 129 | S | 58G, 31D, 19N, 11E, 3R, 2Q, 2H, 1I, 1T, 1K, 1A, 4X=E/G; D/E/G; S/D/G/N; D/E/K/N | |
| 130 | L | 25I, 12T, 9V, 7E, 3S, 2F, 2Y, 1K, 1Q, 1X=I/P/T | |
| 131 | I | 1V | |
| 132 | H | 174Y | |
| 133 | S | 79T, 44N, 7K, 4D, 4R, 1Q, 1F, 1L, 1X=N/T | |
| 134 | L | ||
| 135 | I | 56L | |
| 136 | E | 4T, 3G, 1Q, 1A, 1I, 1L, 1V | |
| 137 | E | E137K | 27K, 15Q, 9N, 9D, 4G, 3A, 3T, 2I |
| 138 | S | S138A | 15A |
| 139 | Q | ||
| 140 | N | 4T, 11I, 3Y, 2H, 1S, 1D, 1F, 1R |
The table shows the single letter code for the amino acid at each position (AA#) in the HXB2 reference strain (HXB2).
Mutations and amino acid polymorphisms that have been associated with enfuvirtide (ENF) resistance are shown (ENF Res).
Amino acids identified in the test samples that differ from the HXB2 sequence are shown using the single letter code. The number of test samples with each amino acid difference is shown (e.g., at position 126 in the HR2 region, one sample has the N126D substitution). Many of the amino acid substitutions were present as a mixture with the amino acid present in the HXB2 sequence (not shown). X indicates the presence of a degenerate nucleotide codon that encodes two or more amino acids in addition to the amino acid presence in the HXB2 sequence; in this case, the amino acids encoded at that position are shown (e.g., in one sample, the amino acids N = asparagine, K = lysine, R = arginine, and S = serine are encoded at position 105). Rows 126, 137, and 138 indicate the positions of accessory mutations that may increase the fitness of viruses with ENF resistance mutations. ENF resistance mutations were detected in some samples (bold).
The PhenoSense HIV Entry assay (Monogram Biosciences, South San Francisco)7 was used to measure the ENF susceptibility of HIV-1 from the samples with HR1 ENF resistance mutations (Fig. 1), and samples with the N42S polymorphism. In the PhenoSense HIV Entry Assay, HIV RNA is extracted from the test sample and first strand cDNA is prepared by reverse transcription. A 2.5-kb amplification product including the entire gp160 coding region is generated and cloned into an env expression vector. The resulting plasmid pool is cotransfected into human embryonic kidney 293 cells with an HIV genomic vector that contains a luciferase expression cassette inserted within a deleted region of the env gene to produce pseudotyped viruses with HIV envelope proteins. Viral stocks are used to inoculate U87 target cell cultures in 96-well plates containing serial dilutions of ENF. Viral replication is monitored by measuring luciferase expression in infected target cells 3 days after inoculation. The drug concentration required to inhibit virus replication by 50% (IC50) is determined for each test sample. The fold change in drug susceptibility is determined by comparing the IC50 value of the test virus to the IC50 of the assay control (JRCSF). The susceptibility cut-off is set at the 99th percentile of the distribution of the enfuvirtide-naive viruses (cut-off: fold change IC50 > 6.48).
ENF susceptibility results were obtained for five of six samples with ENF resistance mutations in HR1 and for 21/26 additional samples with N42S. Only one of 26 samples had HIV with evidence of reduced ENF susceptibility (fold change IC50 above the assay cut-off). The HIV from that sample (#0168) had the HR1 ENF resistance mutations N42S + L44M, as well as the HR2 accessory mutation E137K, and had a fold change IC50 of 24. HIV from another sample that had N42S + L44M without E137K (#0171) had a fold change IC50 of 1.3 (susceptible; Fig. 1).
Other studies have examined ENF resistance mutations in ENF-naive individuals, including those with subtype B and non-B HIV infection.8–12 It is difficult to compare results of those studies to the results in this report, because the mutations considered in assessing ENF resistance varied from study to study. Using the Stanford HIV Resistance Database as a reference, we identified minor HR1 mutations associated with reduced susceptibility to ENF in 6 (3.4%) of 175 samples from men in the EXPLORE cohort (V38G, N43K, L44M, and L45M). We also detected the N42S hypersusceptibility mutation in 28 (16%) of the 175 samples; this is similar to the rate of detection of N42S in other cohorts of ENF-naive individuals with subtype B HIV infection.8,9 The HR2 accessory mutations, E137K and S138A, were detected in 27 (15.4%) and 15 (8.6%) of the 175 EXPLORE samples, respectively; four samples had both E137K and S138A.
Phenotypic analysis in this study demonstrated that the presence of ENF resistance mutations was not sufficient to reduce susceptibility to ENF in some samples. In two samples (#5712 and #2047), we may not have detected reduced ENF susceptibility in the PhenoSense HIV Entry assay because the ENF resistance mutations were present as low-level mixtures with wild-type codons. However, in the other two samples (#0430 and #0171) the mutations were detected without mixtures (Fig. 1), and there was no reduction in ENF susceptibility.
The same samples tested in this study (gp41 genotyping and ENF susceptibility) were previously tested using the ViroSeq™ HIV-1 Genotyping System, to identify mutations associated with resistance to HIV protease and reverse transcriptase inhibitors.4 Two of the six samples that had minor ENF resistance mutations also had genotypic evidence of resistance to other antiretroviral drugs: one sample with V38G also had genotypic evidence of resistance to three other classes of antiretroviral drugs (NRTIs, NNRTIs, and PIs), and one sample with N43K and L45M also had genotypic evidence of NNRTI resistance. However, neither of those samples had reduced ENF susceptibility in the phenotypic assay.
In a previous study, we used the same gp41 genotyping reagents and protocols to analyze the gp41 region in 119 diverse HIV strains, including 11 subtype B and 108 non-B strains; all subjects were unaware of their HIV infection at the time of sample collection, and were presumed to be antiretroviral drug naive.5 Using the same list of ENF resistance mutations as in this report, we did not detect any HR1 ENF resistance mutations in those samples. In contrast, six men in the EXPLORE cohort (3.4%) had ENF resistance mutations in HR1 (0/119 vs. 6/175, p = 0.085). Among the 108 non-B samples analyzed previously, 82 (75.9%) had N42S (vs. 16% in EXPLORE), one (0.6%) had N126K (vs. none in EXPLORE), seven (6.5%) had E137K (vs. 15.4% in EXPLORE), and four (3.7%) had S138A (vs. 8.6% in EXPLORE).5 When comparing these two studies, it is not clear whether the observed differences in the frequencies of ENF mutations reflect differences in HIV subtype (B vs. non-B), the country of origin of the samples (United States vs. non-United States), the years of sample collection (1999–2002 vs. 1993–2001), the stage of disease of the infected individuals (recent infection vs. unknown time of infection), the cohort type (MSM vs. blood donors), or other factors.
Because the men in EXPLORE were infected with HIV prior to FDA clearance of ENF, the observed mutations in HR1 and HR2 are likely to represent naturally occurring polymorphisms. However, we cannot rule out the possibility that some of the men in the EXPLORE cohort were infected by individuals who received ENF in a clinical trial or through a compassionate access program. The men in the EXPLORE study were not followed after seroconversion, so it was not possible to determine whether the HIV variants with ENF resistance mutations persisted over time in these men. In summary, we found that ENF resistance mutations were present in HIV from recently infected MSM in the United States prior to the availability of ENF. However, in most cases, the samples retained phenotypic susceptibility to the drug.
Acknowledgments
The authors thank the EXPLORE study participants and the EXPLORE study team for providing the samples used in this study, thank the Monogram Biosciences Clinical Reference Laboratory for performing the phenotypic ENF resistance assays, and thank Chris Petropoulos for his critical review. This work was supported by (1) the HIV Prevention Trials Network (HPTN) sponsored by the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Child Health and Human Development (NICHD), National Institute on Drug Abuse, National Institute of Mental Health, and Office of AIDS Research, of the National Institutes of Health (NIH), Dept. of Health and Human Services (U01-AI-46745, U01-AI-48054, and U01-AI068613); (2) the HIV Network for Prevention Trials (HIVNET, N01-AI-35173, N01-AI-45200, and NOI-AI-35173-417, NIAID); and (3) the international Maternal Pediatric Adolescent AIDS Clinical Trials Network (U01-AI-068632, NIAID, NIHCD).
Disclosure Statement
N. Marlowe and R. Bruce are employees of Celera. W. Huang is an employee of Monogram Biosciences. S. Eshleman is a member of the Clinical Advisory Board of Monogram Biosciences.
References
- 1.Greenberg ML. Cammack N. Resistance to enfuvirtide, the first HIV fusion inhibitor. J Antimicrob Chemother. 2004;54:333–340. doi: 10.1093/jac/dkh330. [DOI] [PubMed] [Google Scholar]
- 2.Briz V. Poveda E. Soriano V. HIV entry inhibitors: Mechanisms of action and resistance pathways. J Antimicrob Chemother. 2006;57:619–627. doi: 10.1093/jac/dkl027. [DOI] [PubMed] [Google Scholar]
- 3.Koblin B. Chesney M. Coates T. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: The EXPLORE randomised controlled study. Lancet. 2004;364:41–50. doi: 10.1016/S0140-6736(04)16588-4. [DOI] [PubMed] [Google Scholar]
- 4.Eshleman SH. Husnik M. Hudelson S, et al. Analysis of antiretroviral drug resistance, HIV-1 tropism, and HIV-1 subtype among men who have sex with men recently infected with HIV-1 in the United States: The EXPLORE Study. AIDS. 2007;21:1165–1174. doi: 10.1097/QAD.0b013e32810fd72e. [DOI] [PubMed] [Google Scholar]
- 5.Eshleman SH. Hudelson SE. Bruce R, et al. Analysis of HIV type 1 gp41 sequences in diverse HIV-1 strains. AIDS Res Human Retroviruses. 2007;23:1603–1608. doi: 10.1089/aid.2007.0130. [DOI] [PubMed] [Google Scholar]
- 6.Stanford University HIV Drug Resistance Database. Fusion Inhibitor Resistance Notes. hivdb.stanford.edu/cgi-bin/FIResiNote.cgi. [Oct 6;08 ]. hivdb.stanford.edu/cgi-bin/FIResiNote.cgi.
- 7.Limoli K. Huang W. Toma J, et al. Validation, performance characteristics of the PhenoSense HIV fusion inhibitor susceptibility assay. 45th Annual Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); Washington, DC. Dec 16–19;2005 ; Abstract #H1076. [Google Scholar]
- 8.Loutfy MR. Raboud JM. Montaner JS, et al. Assay of HIV gp41 amino acid sequence to identify baseline variation and mutation development in patients with virologic failure on enfuvirtide. Antiviral Res. 2007;75:58–63. doi: 10.1016/j.antiviral.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Carmona R. Perez-Alvarez L. Munoz M, et al. Natural resistance-associated mutations to enfuvirtide (T20) and polymorphisms in the gp41 region of different HIV-1 genetic forms from T20 naive patients. J Clin Virol. 2005;32:248–253. doi: 10.1016/j.jcv.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Peuchant O. Capdepont S. Ragnaud JM, et al. Primary resistance to enfuvirtide (T20) in recently HIV-1 infected, antiretroviral-naive patients from the ANRS Aquitaine Cohort. Antiviral Ther. 2007;12:559–562. doi: 10.1177/135965350701200413. [DOI] [PubMed] [Google Scholar]
- 11.Roman F. Gonzalez D. Lambert C, et al. Uncommon mutations at residue positions critical for enfuvirtide (T-20) resistance in enfuvirtide-naive patients infected with subtype B and non-B HIV-1 strains. J Acquir Immune Defic Syndr. 2003;33:134–139. doi: 10.1097/00126334-200306010-00003. [DOI] [PubMed] [Google Scholar]
- 12.Holguin A. Faudon JL. Labernardiere JL. Soriano V. Susceptibility of HIV-1 non-B subtypes and recombinant variants to enfuvirtide. J Clin Virol. 2007;38:176–180. doi: 10.1016/j.jcv.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Johnson VA. Brun-Vezinet F. Clotet B, et al. Update of the drug resistance mutations in HIV-1: Spring 2008. Top HIV Med. 2008;16:62–68. doi: 10.1007/s11750-007-0034-z. [DOI] [PubMed] [Google Scholar]