A 62 year old woman was admitted with a week's history of jaundice. Examination showed deep icterus and hepatomegaly. She had no history of liver disease, blood transfusion, alcohol or drug misuse, or travel abroad. She had been hypertensive for 15 years and took atenolol 50 mg daily. Treatment had been changed to irbesartan (Aprovel, Bristol-Myers Squibb, Hounslow) 300 mg daily one month before admission.
Liver function tests showed concentrations of albumin 240 g/l (normal range 360-520 g/l), bilirubin 403 μmol/l (0-17 μmol/l), alkaline phosphatase 3193 IU/l (20-125 IU/l), γ-glutamyltransferase 1924 IU/l (10-50 IU/l), and aspartate aminotransferase 177 IU/l (0-40 IU/l). Serology for hepatitis A, B, and C, cytomegalovirus, Epstein-Barr virus, and autoimmune screen gave negative results. Tests for haemochromatosis and α1 antitrypsin deficiency gave normal results. An ultrasonogram and computerised tomogram were normal.
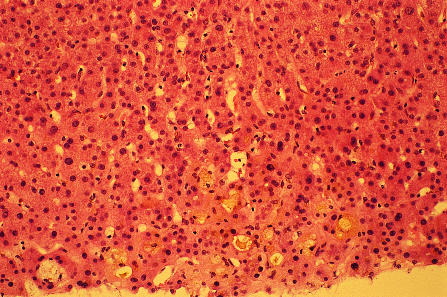
Irbesartan was stopped one week after admission and substituted with amlodipine and atenolol. The patient remained jaundiced, with a bilirubin concentration of 324 μmol/l after two months. A liver biopsy sample obtained on two different occasions showed notable portal tract expansion with minimal inflammation, ectatic bile ductules, and cholestatic rosettes (figure). These features were more pronounced in the second biopsy sample. Endoscopic retrograde cholangiopancreatography gave normal results. Her condition gradually improved and the bilirubin concentration returned to normal in about 16 weeks. She continues to be anicteric at more than one year's follow up.
The temporal profile of her cholestatic jaundice in relation to the irbesartan and the lack of an alternative cause for liver dysfunction suggests a drug reaction. The diagnosis also fulfils the international consensus criteria for drug induced hepatotoxicity.1
A review of hepatotoxicity with angiotensin converting enzyme inhibitors showed that a cholestatic pattern was present in the liver of eight out of 13 patients.2 There have been reports of severe acute hepatic injury as well as 80 reports of minor liver injury in association with losartan.3–5 The manufacturers of irbesartan were, however, previously unaware of any association between this drug and severe hepatic dysfunction.
Figure.
Parenchymal cholestasis with “cholestatic rosettes” and ballooning degeneration of hepatocytes in liver biopsy sample (haematoxylin and eosin × 20)
Acknowledgments
We thank Dr A P Dhillon at the Royal Free Medical School, London, for reviewing the histopathology slides.
Footnotes
Competing interests: None declared.
References
- 1.Benichou C. Criteria of drug-induced liver disorders. Report of an international consensus meeting. J Hepatol. 1990;11:272–276. doi: 10.1016/0168-8278(90)90124-a. [DOI] [PubMed] [Google Scholar]
- 2.Hagley MT, Hulisz DT, Burns CM. Hepatotoxicity associated with angiotensin converting enzyme inhibitors. Ann Pharmacother. 1993;27:228–231. doi: 10.1177/106002809302700220. [DOI] [PubMed] [Google Scholar]
- 3.Bosch X. Losartan-induced hepatotoxicity. JAMA. 1997;278:1572. [PubMed] [Google Scholar]
- 4.Andrade RJ. Hepatic injury associated with losartan. Ann Pharmacother. 1998;32:1371. doi: 10.1345/aph.18087a. [DOI] [PubMed] [Google Scholar]
- 5.Nygaard B, Strandgaard S. Marked hepatotoxicity associated with losartan treatment. Blood Press. 1996;5:190–191. doi: 10.3109/08037059609062128. [DOI] [PubMed] [Google Scholar]