Abstract
The purpose of this study was to examine the interaction of childhood height and childhood BMI in the prediction of young adult BMI. The 2,802 subjects in this study were from the Child and Adolescent Trial for Cardiovascular Health (CATCH). The subjects' heights and weights were measured in 3rd grade (mean age 8.7 years) and again in 12th grade (mean age 18.3 years). The associations and interactions between height (cm) and BMI (kg/m2) were assessed using mixed linear regression models with adult BMI as the dependent variable. We found a significant interaction between childhood height and childhood BMI in the prediction of adult BMI (P < 0.0001). Stratification by Centers for Disease Control and Prevention (CDC) reference quintiles revealed that a positive association between childhood height and adult BMI existed only for those subjects in the top quintile of childhood BMI, within whom predicted adult BMI ranged from 27.5 (95% confidence interval = 26.4-28.6) for those in the shortest height quintile to 30.2 (95% confidence interval = 29.7-30.6) for those in the highest height quintile. Among children with high BMI levels, those who were taller, as compared to those who were shorter, had significantly higher young adult BMI levels. This pattern seems primarily due to the positive association of childhood height and childhood BMI. Clinicians should recognize the risk of excess body weight in young adulthood for all children who have a high BMI, and pay special attention to those who are tall, because their childhood height will not protect them from subsequent weight gain and elevated BMI.
INTRODUCTION
Obesity is now considered a worldwide health epidemic (1). In the United States, the prevention and treatment of obesity is the subject of a recent Surgeon General's report and a major goal for Healthy People 2010 (2,3). Pediatric obesity is a major risk factor for adult obesity (4-10). Accordingly, to control the adult obesity epidemic, it is important to study the growth characteristics of children who are at risk for adult obesity.
Although obesity generally refers to excessive adipose tissue relative to lean mass, the exact definition of excessive has not been standardized. As a clinical measure of obesity to be used in many settings, BMI, defined as weight (in kilograms) divided by height (in meters) squared, has been advocated for use in both children and adults (2,11-16). Studies have consistently found an association between childhood BMI and adult BMI (9,10,17-19). Elevated adult BMI is associated with a variety of adverse health effects (20). Thus, childhood BMI has been advocated as an easily assessed and meaningful marker from which clinicians and researchers should judge a child's risk for excessive adult BMI (10).
The formula for BMI was derived, in part, to adjust body weight for height, with the goal of minimizing the effect of stature on body weight. However, in children, increased height has been found to be positively associated with BMI and adiposity (18,21-23). Given the association of childhood BMI with adult BMI, it follows that childhood height has been associated with both BMI and adiposity in adulthood (18,21,24,25). In adults, there does not appear to be an association between concurrent height and BMI, even in longitudinal cohorts where an association between height and BMI existed in childhood (21,26). Thus, although heavy prepubescent children are generally taller than average children, they tend to become average height as adults. Previous research has called for further investigation into the associations between height and BMI in childhood and adulthood using other cohorts (18,24,26).
The purpose of this study was to evaluate the longitudinal associations of childhood BMI and childhood height to young adult BMI in a geographically diverse US cohort. Our primary goal was to examine the interaction of childhood height and childhood BMI in the prediction of young adult BMI in a large prospective analysis. Our hypothesis was that among children with high BMI levels, taller children, as compared with shorter children, would have higher BMI levels in early adulthood.
METHODS AND PROCEDURES
Study population
The subjects from this study come from the Child and Adolescent Trial for Cardiovascular Health (CATCH). CATCH was a multicenter, cluster-randomized field trial aimed at evaluating the effectiveness of an elementary school-based intervention to improve cardiovascular risk factors via diet, physical activity, and smoking prevention. Ninety-six schools near four field centers (the University of California at San Diego, La Jolla; University of Minnesota, Minneapolis; University of Texas at Austin; and Tulane University School of Public Health and Tropical Medicine, New Orleans, LA) were randomized to either intervention (14 schools per site, 56 total) or control (10 per site, 40 total). The details of the original study are described in detail elsewhere (27).
The study originally assessed 5,106 3rd graders during the fall of 1991. In the spring of 2001, 2,909 of the original subjects were reevaluated in 12th grade. Dropouts from the original cohort were those moving out of the area or choosing not to participate in the follow-up survey (n = 1,968), and those who did not return consent forms (n = 229). In addition, 107 had missing data in either the 3rd or 12th grade. The final sample analyzed for this study consisted of 2,802 subjects (55% of the original cohort) followed longitudinally. Compared with those included in this longitudinal analysis, those lost to follow-up were boys (55%vs. 49%), older (mean age 8.8 years vs. 8.7 years), and Hispanic (18% vs. 10%). Those lost to follow-up were of similar weight z-scores, but they were shorter (height z-score = 0.07vs. 0.14) and had higher BMI z-scores (0.41vs. 0.34). Among the cohort used in this analysis, the intervention and control groups did not differ with respect to weight, height, or BMI at baseline or follow-up and they were therefore merged and analyzed together as a single cohort. In addition, group assignment was controlled for statistically as a fixed effect in all analyses. The subjects in 12th grade were generally over 18 years of age (mean 18.3 years, s.d. 0.5). For the sake of these analyses, 3rd graders will be referred to as “children” and 12th graders will be “young adults.”
Anthropometry
All measurements were taken by certified CATCH examiners who received training in standard protocols annually from the central coordinating center (28). In both the 3rd and 12th grades the subjects were measured after removing their shoes, sweaters, and outerwear. Standing height was measured twice without shoes to the nearest 0.1cm using a portable stadiometer (Perspective Enterprises, Kalamazoo, MI), and the mean of the two values was used for analysis. Weight was measured twice to the nearest 0.1kg using balance beam scales (Detecto Medic balance scale; Detecto Scales, Brooklyn, NY), and the mean of the two measurements was used for the analysis. BMI was calculated as weight (in kilograms) divided by height (in meters) squared. Age, gender, and race/ethnicity were recorded for all participants.
Statistical analyses
Sample characteristics for categorical variables (gender, ethnicity, over-weight, obesity) were described by distribution in percentage. Exact percentiles for weight, height, and BMI for age and gender were calculated for the Centers for Disease Control and Prevention (CDC) 2000 reference values derived from the US population of the 1960s, 1970s, and 1980s (29,30). For children, overweight was defined the 85th percentile or more and less than the 95th percentile for CDC reference, and obese was defined as more than equal to 95th percentile for CDC reference (31). For adults (those in the 12th grade) overweight was defined as a BMI ≥25 and <30, and obese was defined as a BMI ≥30. Continuous variables (age, weight, height, and BMI) were described by means and standard deviation and by medians and 25th percentile and 75th percentile of the cohort.
The relationships of childhood BMI (kg/m2) and adult BMI (kg/m2), and childhood height (cm) and adult BMI (kg/m2) were graphically displayed using smoothed adjusted means, using a smoothing spline and adjusting for age, gender, site, intervention arm, and ethnicity in a generalized additive model (32). Linear and nonlinear associations of anthropometric variables were assessed using linear mixed models, including age, gender, ethnicity, site, and intervention arm as fixed effects (adjusting for confounding) and school as a random intercept term. School was modeled as a random term to consider the clustering effect arising from the sampling design. Linear associations between the anthropometric variables were tested by including the variable as a continuous term, and departure from linearity by including a quadratic term. Spearman correlations were computed and P values <0.05 were considered to be statistically significant.
Hypothesis-driven interactions with childhood height to predict adult BMI were tested by including an interaction term; e.g., childhood BMI × childhood height. Childhood BMI and height were stratified according to CDC reference quintiles to analyze their interaction in predicting young adult BMI. We performed a global test for interaction by including childhood BMI and height as categorical variables in the model. We then analyzed whether childhood height and adult BMI were linearly associated according to childhood BMI strata, and if these linear trends differed according to BMI strata. Similarly, we analyzed the association of childhood BMI and adult BMI according to childhood height strata. In addition, test for trend in predicting adult BMI was analyzed for childhood height quintiles across the childhood BMI quintile strata and for childhood BMI quintiles across the childhood height strata. The analyses were performed using a linear mixed model to account for the school cluster and all the models were adjusted by gender, age, site, ethnicity, and intervention arm. Analysis was performed in SAS (version 9; SAS Institute, Cary, NC) and graphical displays performed in Splus (version 6; MathSoft, Seattle, WA).
RESULTS
Summary statistics describing the study sample are presented in Table 1. The population was ethnically diverse with 22% self identifying as either “non-Hispanic black” or “Hispanic.” Compared to the CDC 2000 reference levels, the cohort was heavier and taller. The median levels for weight, height, and BMI were higher than the mean levels due to the uneven distribution of the sample whereby a higher proportion of children had values in the upper percentiles of weight, height, and BMI in comparison to the middle and lower percentiles. Approximately 25.4% of the children had a BMI that placed them above the childhood categorical level for overweight (i.e., ≥85th percentile of the CDC reference). In young adulthood (mean age 18.3 years), the mean BMI was at 24.5 kg/m2, and 35.6% of the subjects had a BMI that was above the categorical cutoff of 25 for adult overweight.
Table 1.
Descriptive statistics
| Descriptive statistics (n = 2,802) | ||
|---|---|---|
| Children | Young adults | |
| Age in years (mean (s.d.)) | 8.7 (0.45) | 18.3 (0.5) |
| Date of measurement | Fall 1991 | Spring 2001 |
| Gender (female %) | 51.2 | |
| Ethnicity (n (%)) | ||
| Non-Hispanic white | 2,070 (74%) | |
| Non-Hispanic black | 335 (12%) | |
| Hispanic | 290 (10%) | |
| Other | 107 (4%) | |
| Weight (kg) (mean (s.d.)) | 30.9 (6.9) | 74.1 (17.5) |
| Weight percentile* | ||
| Mean (s.d.) | 59.6 (28.1) | 64.1 (28.5) |
| Median (25th, 75th %) | 62.3 (37.6, 84.9) | 70.7 (42.5, 89.4) |
| Height (cm) (mean (s.d.)) | 132.5 (6.1) | 170.5 (9.4) |
| Height percentile* | ||
| Mean (s.d.) | 53.8 (27.5) | 53.7 (28.6) |
| Median (25th, 75th %) | 55.8 (31.3, 77.1) | 54.5 (29.2, 79.0) |
| BMI (mean (s.d.)) | 17.5 (2.9) | 24.5 (5.3) |
| BMI percentile* | ||
| Mean (s.d.) | 59.9 (28.1) | 61.9 (29.4) |
| Median (25th, 75th %) | 63.3 (37.9, 85.3) | 67.2 (38.7, 88.5) |
Cohort percentiles are based on Centers for Disease Control and Prevention 2000 reference standards (29).
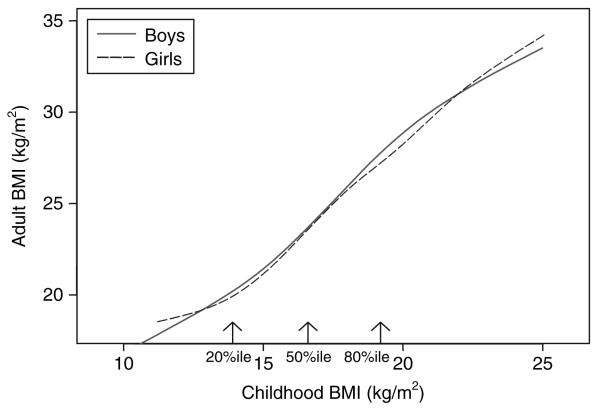
The longitudinal association of childhood BMI (adjusted for age, gender, site, and intervention) and young adult BMI is presented as smoothed adjusted means in Figure 1. The association of childhood BMI and young adult BMI was approximately linear with an overall slope of 1.29 kg/m2 (s.e. 0.02, P < 0.0001). Thus, every childhood BMI unit increase was associated with about 1.3 units of increase in adult BMI. The Spearman correlation between adjusted BMI in childhood and BMI in early adulthood was 0.73. The association departed from linearity (P = 0.0012 for the quadratic term). There was no interaction between gender and childhood BMI in predicting adult BMI (P = 0.58).
Figure 1.
Association of childhood BMI (kg/m2) and adult BMI (kg/m2) by gender, represented by smooth means adjusted for age, ethnicity, site, and intervention. 20th, 50th, and 80th percentiles listed are based on Centers for Disease Control and Prevention age matched height reference units and approximate averages of the genders.
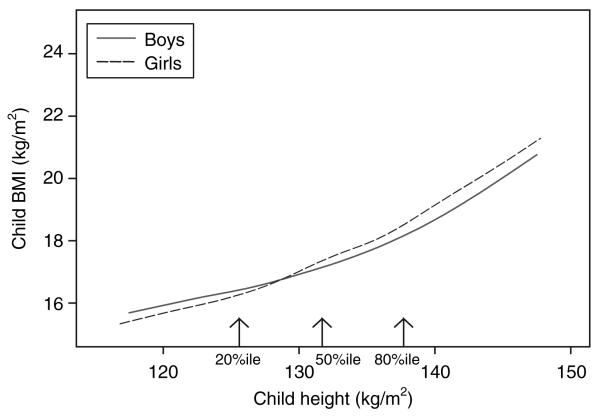
As seen in Figure 2, cross-sectional analysis found that childhood height (adjusted for age, ethnicity, site, and intervention) was associated with childhood BMI. The average linear slope was 0.18kg/m2/cm (s.e. 0.01, P < 0.0001). Thus, an increase of 5.6cm in childhood height was associated with an increase of 1 childhood BMI unit. The relationship is curvilinear with a steeper slope at taller heights. A test for nonlinearity was significant with a quadratic term, P < 0.0001. The Spearman correlation between adjusted height and BMI in childhood was 0.33. There was a statistically significant interaction of gender and child height to predict child BMI, whereby there was a stronger association within girls as compared with boys (P = 0.04).
Figure 2.
Association of childhood height (cm) and childhood BMI (kg/m2) by gender, represented by smooth means adjusted for age, ethnicity, site, and intervention. 20th, 50th, and 80th percentiles listed are based on Centers for Disease Control and Prevention age matched height reference units and approximate averages of the genders.
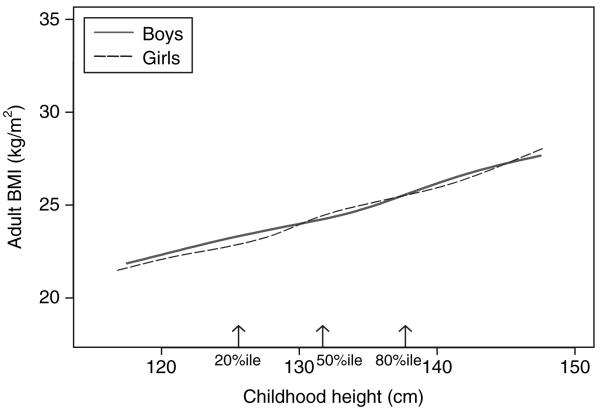
As seen in Figure 3, longitudinal analysis revealed a statistically significant linear association between childhood height (adjusted for age, ethnicity, site, and intervention) and adult BMI. The linear slope was 0.2kg/m2/cm, s.e. 0.01, P < 0.0001. Hence, an increase of 4cm of childhood height was associated with an increase of 1 adult BMI unit. There was no statistical departure from linearity (P = 0.13 for the quadratic term). The Spearman correlation was 0.25. However, after adjustment of childhood height for childhood BMI, there was not a statistically significant association of childhood height and adult BMI (slope = 0.02, s.e. = 0.01, P = 0.12) There was no interaction between gender and childhood height in predicting adult BMI (P value for interaction = 0.10). In adulthood, there was no association between height and BMI (Spearman correlation = 0.03).
Figure 3.
Association of childhood height (cm) and adult BMI (kg/m2) by gender, represented by smooth means adjusted for age, ethnicity, site, and intervention. 20th, 50th, and 80th percentiles listed are based on Centers for Disease Control and Prevention age matched height reference units and approximate averages of the genders.
Our primary goal was to explore the interaction between childhood height and childhood BMI in predicting young adult BMI. Observed adjusted means of adult BMI stratified by CDC reference quintiles of childhood height and childhood BMI is presented in Table 2. Overall, we found a statistically significant interaction between childhood height and childhood BMI in predicting adult BMI (P < 0.0001). As seen by the columns in Table 2, within each of the four lower quintiles of childhood BMI, there was no association between childhood height and adult BMI. However, within the top quintile of childhood BMI, there was a significant positive linear association between childhood height quintiles and adult BMI levels (P < 0.0001). Among children in the top quintile of childhood BMI, the tallest children had an adult BMI level of approximately two units more than those children in the middle quintile of childhood height and nearly three BMI units more than those in the lowest quintile of childhood height. After adjusting for childhood BMI, the association between childhood height and adult BMI among the children in the highest BMI quintile became nonsignificant (P = 0.25). In addition, there was no difference between genders (P value for interaction = 0.25).
Table 2.
Predicted adjusted meansa of adulthood BMI (kg/m2) according to childhood height and BMI cdc reference quintiles and 95% confidence intervals
| CDC quintiles of child BMI |
|||||||
|---|---|---|---|---|---|---|---|
| 0–20 | 20–40 | 40–60 | 60–80 | 80–100 | |||
| n = 312 | n = 443 | n = 548 | n = 629 | n = 870 | P trend | ||
| CDC quintiles of child height |
0–20 | 19.6 (18.7, 20.4) | 21.2 (20.4, 21.9) | 22.3 (21.4, 23.1) | 24.7 (23.8, 25.7) | 27.5 (26.4, 28.6) | P < 0.0001 |
| n = 402 | n = 81 | n = 102 | n = 92 | n = 75 | n = 52 | ||
| 20–40 | 19.8 (18.9, 20.6) | 21.5 (20.7, 22.2) | 22.7 (22, 23.4) | 24.2 (23.5, 24.9) | 28.4 (27.7, 29.1) | P < 0.0001 | |
| n = 566 | n = 84 | n = 108 | n = 134 | n = 120 | n = 120 | ||
| 40–60 | 20.3 (19.3, 21.3) | 21.4 (20.6, 22.2) | 22.6 (21.9, 23.4) | 24.3 (23.6, 24.9) | 28.2 (27.6, 28.8) | P < 0.0001 | |
| n = 565 | n = 57 | n = 97 | n = 107 | n = 148 | n = 156 | ||
| 60–80 | 19.6 (18.6, 20.6) | 20.9 (20, 21.7) | 22.5 (21.8, 23.1) | 24.8 (24.2, 25.5) | 28.7 (28.1, 29.2) | P < 0.0001 | |
| n = 662 | n = 58 | n = 80 | n = 137 | n = 160 | n = 227 | ||
| 80–100 | 20.4 (19, 21.8) | 21.5 (20.4, 22.5) | 22.2 (21.3, 23.1) | 24.3 (23.6, 25) | 30.2 (29.7, 30.6) | P < 0.0001 | |
| n = 607 | n = 32 | n = 56 | n = 78 | n = 126 | n = 315 | ||
| P trend | P = 0.40 | P = 0.98 | P = 0.83 | P = 0.80 | P < 0.0001 | ||
CDC, Centers for Disease Control and Prevention.
Adjusted by age, gender, ethnicity, site, and intervention.
As seen within the rows of Table 2, within each quintile of childhood height there was a statistically significant linear trend between quintiles of childhood BMI and observed adult BMI (P < 0.0001 for each childhood height quintile). There was a statistically significant difference in the linear trend whereby the highest quintiles of height had steeper slopes. For example, per BMI quintile, the slope for the tallest quintile was 1.02 BMI units higher than the slope of 1.89 BMI units for the shortest quintile of height (P < 0.0001).
DISCUSSION
Our study of 2,802 subjects with measured heights and weights in the 3rd grade (mean age 8.7 years) and then again in the 12th grade (mean age 18.3 years) found a significant interaction between childhood height and childhood BMI for the prediction of young adult BMI. For those children with a BMI that was in the top CDC reference quintile, childhood height had a significant positive association with young adult BMI. Comparing two 3rd grade children of similar age, gender, and ethnicity who have a BMI above the 80thpercentile, one whose height is the top 80th to 100th percentile would have a predicted BMI in 12th grade that was approximately two units higher than a child who stood between the 40th to 60th percentile, and nearly three BMI units higher than a child with a height in the lowest quintile. Assuming the child grows to be an average height female (e.g., 5 feet, 4 inches tall), or an average height male (e.g., 5 feet, 10 inches tall), two BMI units signifies ∼12 or 14 pounds of weight, respectively. This amount of weight gain has been associated with increased obesity-related cardiovascular risk factors (33,34).
As summarized by Wolff in 1954, studies from the 1930s began documenting that obese children were taller than their peers (35,36). More recently, a cross-sectional analysis of children and adolescents in the Bogalusa Heart Study found a significant association between height and BMI in children aged under 10 years, such that the shorter children (height for age <20th percentile) had only a 1-2% prevalence of obesity (BMI ≥ 95th percentile), whereas those who were taller (height for age >80th percentile) had a prevalence of obesity between 11 and 26% (21). Although numerous previous studies have documented an association of cross-sectional childhood height and BMI (18,21-23), we are aware of few investigations into whether the interaction between childhood height and childhood BMI alters the prediction of adult BMI. Freedman et al. analyzed data from 1,055 subjects from the Bogalusa Heart Study in childhood (aged 2–8 years) and then again an average of 18 years later (24). They found that childhood height provided additional information on adult adiposity even if childhood levels of BMI were known. At similar BMI levels, a taller child in their cohort had a higher adult BMI level. However, there discussion section also states that additional analyses found that among children aged ≥9 years, height was not independently related to adult adiposity. The subjects in our study were nearly 9 years of age, and thus our finding that child height adjusted for child BMI was not statistically independently associated with adult BMI is likely consistent with their findings.
Our results confirmed several associations seen in past research. Specifically, we found a significant positive association between childhood BMI and young adult BMI. Childhood BMI was found to account for 53% of the variation in young adult BMI. We also found significant positive associations between childhood height and childhood BMI, and between childhood height and adult BMI. However, after adjustment for childhood BMI, there was no longer an association between childhood height and adult BMI. Thus, childhood height was not an independent predictor of adult BMI. In young adults, we found no association between height and BMI.
In a longitudinal analysis of 626 subjects from the Bogalusa Heart Study, Freedman et al. found that the effect of childhood height on adult BMI was “strongest among children who were relatively heavy” (25). Our analysis was consistent with this finding as the association between child height and adult BMI occurred only in children with a BMI in the upper quintile. These results support a model whereby proximal obesogenic factors may be causing an increase in both childhood BMI and childhood skeletal growth and maturation. It is important to note that the association of childhood height and adult BMI among those in the top quintile of childhood BMI exists for far >20% of the current population. In our study, 31% of the subjects had a childhood BMI that was in the upper quintile of the BMI-for-age CDC reference, and the proportion in the current US population is even higher. National Health and Nutrition Examination Survey data for the years 1999–2004 suggest that ∼37% of children in the United States, aged 6-11 years, have BMI levels in only the top 15 percentiles (37). Thus, the association between height in 3rd grade and adult BMI for those children with elevated childhood BMI may pertain to nearly half of the current US population of similar aged children. Furthermore, these are the same children that are at most risk for adult overweight and obesity. In our study, of the 870 children who had a BMI over the 80th percentile, 345 (40%) went on to become over-weight as young adults (BMI ≥ 25 and <30), and another 305 (35%) went on to become obese (BMI ≥ 30) as young adults. Thus, the association between childhood height and adult BMI occurs in a large proportion of children in today's society, and in those children who need the closest monitoring due to their high risk of becoming overweight and obese.
There are several factors about the CATCH dataset that strengthen our findings. We are unaware of any published study in the United States with a larger number of subjects with measured heights and weights in both childhood and in late adolescence/early adulthood. The subjects were from four geographically and culturally distinct areas of the United States, and ethnically diverse. The childhood measurements were done in the years 1992-1993 and the early adult measurements were completed in the years 2000-2001. Thus, the children grew up in a US environment well after the start of the rise in obesity rates seen in the 1970s and 1980s.
There were also limitations to our study. Only 55% of the original cohort was available for the longitudinal analyses. Analysis of the longitudinal cohort suggests that they were generally similar to the original cohort. The earliest CATCH measurements were carried out in the 3rd grade, with the children being ∼8–9 years of age, and the follow-up measurements were collected when the subjects were in 12th grade at an average of 18.3 years of age. Our findings would have likely been stronger if we had measurements from earlier in childhood and later in adulthood. We assumed that the stature of the 12th graders was their adult height, although skeletal maturation was not assessed. A large longitudinal study in Sweden found that 99.2% of their subjects had reached final height by 18 years of age (26).
We believe that our findings raise some important questions for future research. It would be of interest to know whether childhood height interacts with body fat measurements per se to predict adult obesity and obesity-related cardiovascular risk factors. Use of body fat measurements would also serve to avoid the statistical conundrum that is inherent when evaluating both height and BMI, the latter including height-squared in the equation. Can the assessment of future obesity risk in a child that is both tall and overweight be improved by body fat measurements, or by evaluation of skeletal maturity?
Our results have potential implications for clinical practice. At present, when a clinician or a parent assesses a child whose BMI is high, but whose stature is also high, there may be the hope that the child will “thin out” and become a tall and normal weight adult. Thus, increased stature may be interpreted to be protective toward the risk of subsequent obesity. However, our findings suggest the opposite. For children in the upper BMI percentiles, those with increased height had higher predicted levels of young adult BMI.
Obesity is associated with excessive morbidity and mortality in the United States and in much of the world (20,38-40). This longitudinal prospective study of 2,802 subjects with measured heights and weights in 3rd grade, and again in 12th grade, found that children with a BMI above the 80th percentile went on to have mean BMI levels in young adulthood that were in the overweight to obese range. Given the strong association between childhood obesity and adult obesity (4-10), it is important to understand factors of childhood growth that predict excessive body weight in adulthood. Our study found a positive association between childhood height and young adult BMI in children with a childhood BMI at or above the 80th percentile of CDC standards. Among children with higher BMI levels, those who were taller, as compared to those who were shorter, had significantly higher young adult BMI levels. This pattern seems primarily due to the positive association of childhood height and childhood BMI. There is a need for further research into the proximal factors causing early increases in both childhood height and childhood BMI. Clinicians should recognize the risk of excess body weight in young adulthood for all children who have a high BMI, and pay special attention to those who are tall, because their childhood height will not protect them from subsequent weight gain and elevated BMI.
ACKNOWLEDGMENTS
This work was supported by funds from the National Cancer Institute Centers for Transdisciplinary Research on Energetics and Cancer (U54CA116849) and the University of Minnesota Obesity Prevention Center. The opinions or assertions contained herein are the private ones of the authors and are not considered as reflecting the views of the National Institutes of Health.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.York DA, Rössner S, Caterson I, et al. Prevention Conference VII: obesity, a worldwide epidemic related to heart disease and stroke: Group I: worldwide demographics of obesity. Circulation. 2004;110:e463–e470. doi: 10.1161/01.CIR.0000140125.26161.49. [DOI] [PubMed] [Google Scholar]
- 2.Surgeon General's Call to Action: A call to action to prevent and decrease overweight and obesity. 2007 < http://www.surgeongeneral.gov/topics/obesity/>. Accessed 30 August 2007.
- 3.Healthy People 2010. 2007 < http://healthypeople.gov/document/pdf/Volume2/19Nutrition.pdf>. Accessed 30 August 2007.
- 4.Parsons TJ, Power C, Logan S, Summerbell CD. Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord. 1999;23(Suppl 8):S1–S107. [PubMed] [Google Scholar]
- 5.Freedman DS, Khan LK, Serdula MK, et al. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115:22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 6.Guo SS, Huang C, Maynard LM, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obes Relat Metab Disord. 2000;24:1628–1635. doi: 10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 7.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 8.Clarke WR, Lauer RM. Does childhood obesity track into adulthood? Crit Rev Food Sci Nutr. 1993;33:423–430. doi: 10.1080/10408399309527641. [DOI] [PubMed] [Google Scholar]
- 9.Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res. 2005;13:163–169. doi: 10.1038/oby.2005.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–e144. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 11.Bellizzi MC, Dietz WH. Workshop on childhood obesity: summary of the discussion. Am J Clin Nutr. 1999;70:S173–S175. doi: 10.1093/ajcn/70.1.173s. [DOI] [PubMed] [Google Scholar]
- 12.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dietz WH, Robinson TN. Use of the body mass index (BMI) as a measure of overweight in children and adolescents. J Pediatr. 1998;132:191–193. doi: 10.1016/s0022-3476(98)70426-3. [DOI] [PubMed] [Google Scholar]
- 14.Barlow SE, Dietz WH. Management of child and adolescent obesity: summary and recommendations based on reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110:236–238. [PubMed] [Google Scholar]
- 15.Poskitt EM. Defining childhood obesity: the relative body mass index (BMI). European Childhood Obesity group. Acta Paediatr. 1995;84:961–963. doi: 10.1111/j.1651-2227.1995.tb13806.x. [DOI] [PubMed] [Google Scholar]
- 16.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5(Suppl 1):4–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 17.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329:1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 18.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 19.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76:653–658. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 20.Overweight, obesity, and health risk. National Task Force on the Prevention and Treatment of Obesity. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 21.Freedman DS, Khan LK, Serdula MK, et al. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28:10–16. doi: 10.1038/sj.ijo.0802544. [DOI] [PubMed] [Google Scholar]
- 22.Williams SM. Weight and height growth rate and the timing of adiposity rebound. Obes Res. 2005;13:1123–1130. doi: 10.1038/oby.2005.131. [DOI] [PubMed] [Google Scholar]
- 23.Freedman DS, Thornton JC, Mei Z, et al. Height and adiposity among children. Obes Res. 2004;12:846–853. doi: 10.1038/oby.2004.102. [DOI] [PubMed] [Google Scholar]
- 24.Freedman DS, Khan LK, Mei Z, et al. Relation of childhood height to obesity among adults: the Bogalusa Heart Study. Pediatrics. 2002;109:E23. doi: 10.1542/peds.109.2.e23. [DOI] [PubMed] [Google Scholar]
- 25.Freedman DS, Kettel KL, Serdula MK, Srinivasan SR, Berenson GS. BMI rebound, childhood height and obesity among adults: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2001;25:543–549. doi: 10.1038/sj.ijo.0801581. [DOI] [PubMed] [Google Scholar]
- 26.He Q, Karlberg J. BMI in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001;49:244–251. doi: 10.1203/00006450-200102000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Perry CL, Stone EJ, Parcel GS, et al. School-based cardiovascular health promotion: the child and adolescent trial for cardiovascular health (CATCH) J Sch Health. 1990;60:406–413. doi: 10.1111/j.1746-1561.1990.tb05960.x. [DOI] [PubMed] [Google Scholar]
- 28.Webber LS, Osganian V, Luepker RV, et al. Cardiovascular risk factors among third grade children in four regions of the United States. The CATCH Study. Child and Adolescent Trial for Cardiovascular Health. Am J Epidemiol. 1995;141:428–439. doi: 10.1093/oxfordjournals.aje.a117445. [DOI] [PubMed] [Google Scholar]
- 29.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000:1–27. [PubMed] [Google Scholar]
- 30.A SAS program for the CDC 2000 growth charts. 2007 < http://www.cdc.gov/nccdphp/dnpa/growthcharts/sas.htm>. Accessed 30 August 2007.
- 31.Barlow SE. Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 32.Hastie T, Tibshirani R. Generalized Additive Models. Chapman and Hall; London: 1990. [DOI] [PubMed] [Google Scholar]
- 33.Gelber RP, Gaziano JM, Manson JE, Buring JE, Sesso HD. A prospective study of body mass index and the risk of developing hypertension in men. Am J Hypertens. 2007;20:370–377. doi: 10.1016/j.amjhyper.2006.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wannamethee SG, Shaper AG, Walker M. Overweight and obesity and weight change in middle aged men: impact on cardiovascular disease and diabetes. J Epidemiol Community Health. 2005;59:134–139. doi: 10.1136/jech.2003.015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolff OH. Obesity in childhood; a study of the birth weight, the height, and the onset of puberty. Q J Med. 1955;24:109–123. [PubMed] [Google Scholar]
- 36.Bruch H. Obesity in childhood: physical growth and development of obese children. Am J Dis Child. 1939;58:457–484. [Google Scholar]
- 37.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 38.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 39.Asia Pacific Cohort Studies Collaboration The burden of overweight and obesity in the Asia-Pacific region. Obes Rev. 2007;8:191–196. doi: 10.1111/j.1467-789X.2006.00292.x. [DOI] [PubMed] [Google Scholar]
- 40.Andreyeva T, Michaud PC, van SA. Obesity and health in Europeans aged 50 years and older. Public Health. 2007;121:497–509. doi: 10.1016/j.puhe.2006.11.016. [DOI] [PubMed] [Google Scholar]