Abstract
The aim of this study was to examine the potential correlation of sleep characteristics with glucose metabolism in nondiabetic men with obstructive sleep apnea syndrome (OSAS). Included were 31 male patients (mean age 46.7 ±11 years), recently diagnosed with OSAS by full polysomnography. There was a significant correlation of fasting glucose and glycosylated hemoglobin (HbA1c) levels with arousal index (P = 0.047 and P =0.014, respectively). Moreover, HbA1c levels were correlated with apnea hypopnea index (P =0.009), a widely accepted marker of the severity of OSAS, and with percentage of sleep time with saturation of hemoglobin with oxygen as measured by pulse oximetry (SpO2) < 90% (t < 90%) ( P =0.010). Finally, glucose and HbA1c levels showed a significant negative correlation with average SpO2 (P =0.013 and P = 0.012, respectively) and, additionally, glucose levels with minimum SpO 2 (P =0.027) during sleep. In conclusion, severity of OSAS among nondiabetic men is associated with increased HbA1c levels and increased fasting glucose. Thus, severity of OSAS may be an additional marker of cardiovascular risk, as well as of future diabetes, in these subjects. However, further work is needed to confirm the clinical significance of these observations.
Keywords: obstructive sleep apnea syndrome, glucose metabolism, glycated hemoglobin, sleep disordered breathing
Introduction
Obstructive sleep apnea syndrome (OSAS), a common disorder, affecting approximately 3%–7% of adult men and 2%–5% of adult women in the general population,1 is being increasingly recognized as an important cause of morbidity and mortality.2 This clinical condition is characterized by repeated episodes of complete or partial obstruction of the upper airway during sleep, associated with increased respiratory efforts, intermittent arterial oxygen desaturation, systemic and pulmonary arterial blood pressure alterations and sleep fragmentation. The cardinal symptoms of OSAS are nocturnal respiratory pauses, interrupted by loud snoring, and excessive daytime sleepiness.2
OSAS and type 2 diabetes mellitus (DM) are common comorbid conditions. Indeed, the prevalence of OSAS is estimated to be between 18% and 36% in subjects with type 2 DM.3,4 Vice versa, the prevalence of type 2 DM is approximately 30% in OSAS patients.5 Several lines of evidence suggest an independent association of OSAS with insulin resistance and DM.6–9
Ip and colleagues reported that markers of OSAS severity (Apnea Hypopnea Index [AHI] and minimum oxygen saturation) were associated with insulin resistance,6 while Punjabi and colleagues found that sleep-disordered breathing (SDB) was associated with insulin resistance in mildly obese but otherwise healthy males from the general population.7 Cross-sectional data from the Sleep Heart Health Study and the Wisconsin Sleep Cohort found similar results in population cohorts.8,9 However, the longitudinal data from the Wisconsin Cohort could not demonstrate a clear relationship between SDB and the subsequent development of DM.9 Other studies in snorers have confirmed the association of SDB and insulin resistance or diabetes in nonobese Korean and Indian males,10,11 and similar results were found in subjects with suspected OSAS.5,12,13 In all reports, the association was independent of obesity, even though obesity is known to increase the risk for impaired glucose tolerance. In normal subjects, hypoxia appears to be an important contributor to glucose intolerance.14 Recent state-of-the art reviews have emphasized the need for further clinical research in this direction.15,16
Little is known so far on the association between glycemic profile and severity of OSAS in patients that do not meet the criteria for the diagnosis of diabetes. Thus, the aim of the present study was to examine the potential correlation of sleep characteristics with glucose metabolism in nondiabetic men with OSAS.
Materials and methods
Study group
Thirty one consecutive male patients, with recently diagnosed OSAS (AHI > 15/hour) by polysomnography between January and June 2009, comprised the study group. Each participant was evaluated by full clinical examination and completed a detailed questionnaire about sleep habits. Exclusion criteria were: known diabetes mellitus or fasting glycemia (fasting glucose ≥ 126 mg/dl or glycosylated hemoglobin [HbA1c]> 6.5%),17 current smoking, cardiovascular or cerebrovascular disease, hypertension or other chronic disease, systemic medication use, as well as previous diagnosis/treatment for OSAS. The study was approved by the Institutional Ethics Committee and all subjects gave written informed consent.
Polysomnography
Each subject underwent standard full night polysomnography (PSG). Sleep records were manually scored, according to standardized criteria.18 AHI was defined as the total number of apneas and hypopneas per hour of electroencephalographic sleep. Arousal Index (AI) was the total number of arousals per hour of recorded sleep. OSAS was defined as an AHI of ≥ 15/hour.
Blood assays
Fasting venous blood samples were collected the day after PSG, between 8 and 9 AM, after an overnight fast. Biochemical analyses were performed in an ILAB 600 analyzer (Biochem, Tokyo, Japan) with enzymatic method for glucose (mg/dL) while HbA1c was measured by high-performance liquid chromatography (Adams A1c HA-8160; Arkray, Kyoto, Japan).
Statistical analysis
Analysis was performed with SPSS for Windows, version 15.0 (SPSS, Chicago, IL, USA). Normality was examined by the Kolmogorov-Smirnoff test. Descriptive results for continuous variables are expressed as mean ±SD. Regression analysis was applied to explore relationships between glucose or HbA1c values and apnea-related characteristics, independently of body mass index (BMI). Statistical significance was defined at a level of 5% (P < 0.05).
Results
Mean age was 46.7 ±11 years (ranging between 28–71 years) and mean BMI was 34.8 ±6.6 kg/m 2 (ranging between 28 and 54.9 Kg/m2). Neck circumference was 44.5 ±2.8 cm while waist circumference was 119.9 ±18.6 cm. Sleep and metabolic characteristics of patients are presented in Table 1.
Table 1.
Sleep and metabolic characteristics of OSAS patients
| Parameter | Mean ±SD | Range |
|---|---|---|
| AHI (events/hour) | 55.1 ±26.4 | 15.2–108 |
| Average SpO2 (%) | 90 ±5.7 | 72–95 |
| Minimum SpO2 (%) | 71.7 ±12.1 | 41–88 |
| t < 90 (%) | 31.39 ±31.42 | 0–99 |
| AI (events/hour) | 45.1 ±23.3 | 5–100 |
| Sleep efficiency (%TST) | 77.4 ±14.4 | 34.4–93.9 |
| Sleep latency (minutes) | 23.7 ±15.1 | 5.5–66.5 |
| Stage 1 (%TST) | 36.7 ±16.4 | 9.4–77.1 |
| Stage 2 (%TST) | 45.7 ±10.4 | 25.8–69.1 |
| SWS (%TST) | 8 ±9.3 | 0–38.2 |
| REM (%TST) | 12.4 ±5.8 | 0–24.4 |
| Fasting glucose (mg/dl) | 95.1 ±12.5 | 67–125 |
| HbA1c(%) | 5.2 ±0.6 | 4.2–6.3 |
Abbreviations: AHI, Apnea Hypopnea Index; AI, Arousal Index; HbA1c, glycosylated hemoglobin; OSAS, obstructive sleep apnea syndrome; REM, rapid eye motion; SD, standard deviation; SpO2, saturation of hemoglobin with oxygen as measured by pulse oximetry; SWS, slow-wave sleep; TST, total sleep time.
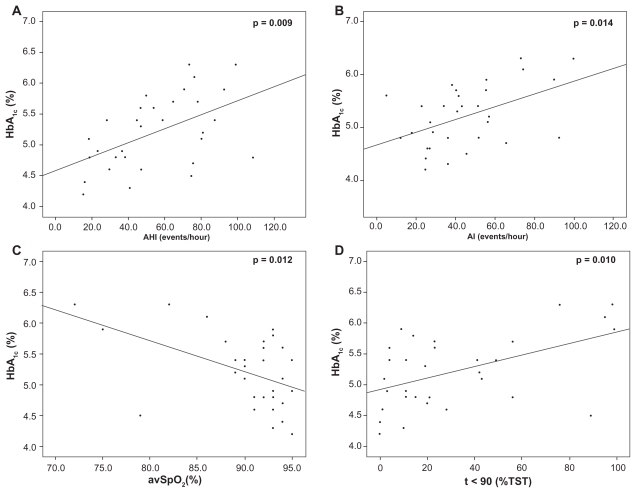
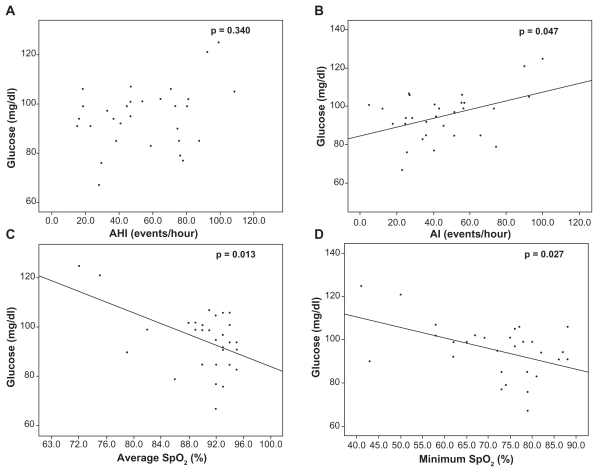
A significant correlation between HbA1c levels and apnea-related parameters (AHI, average saturation of hemoglobin with oxygen as measured by pulse oximetry [SpO2], percentage of sleep time with SpO2 < 90%, ie, t < 90, and AI) was revealed (Figure 1). Moreover, fasting glucose levels were significantly correlated with AI and average and minimum SpO2 (Figure 2). As shown in Table 2, correlations were independent of BMI.
Figure 1.
Correlations of HbA1c levels with AHI (A), AI (B), average SpO2 (C) and percentage of sleep time with SpO2< 90% (D).
Abbreviations: AHI, Apnea Hypopnea Index; AI, Arousal Index; HbA1c, glycosylated hemoglobin; SpO2, saturation of hemoglobin with oxygen as measured by pulse oximetry.
Figure 2.
Correlations of fasting glucose levels with AHI (A), AI (B), average SpO2 (C), and minimum SpO2 (D).
Abbreviations: AHI, Apnea Hypopnea Index; AI, Arousal Index; SpO2, saturation of hemoglobin with oxygen as measured by pulse oximetry.
Table 2.
Results of regression analysis
| Glucose levels |
|||
|---|---|---|---|
| B ± SD | Beta | P | |
| BMI | 0.640 ±0.336 | 0.339 | 0.223 |
| AHI | 0.092 ±0.095 | 0.195 | 0.340 |
| AI | 0.196 ±0.094 | 0.365 | 0.047 |
| t < 90 | 12.405 ±7.176 | 0.312 | 0.095 |
| Average SpO2 | −0.973 ±0.366 | −0.442 | 0.013 |
| Minimum SpO2 | −0.419 ±0.179 | −0.410 | 0.027 |
| HbA1clevels | |||
| BMI | 0.000 ±0.016 | 0.006 | 0.976 |
| AHI | 0.011 ±0.004 | 0.511 | 0.009 |
| AI | 0.011 ±0.004 | 0.448 | 0.014 |
| t < 90 | 0.877 ±0.319 | 0.470 | 0.010 |
| Average SpO2 | −0.470 ±0.017 | −0.456 | 0.012 |
| Minimum SpO2 | −0.015 ±0.09 | −0.305 | 0.112 |
Abbreviations: AHI, Apnea Hypopnea Index; AI, Arousal Index; BMI, body mass index; SD, standard deviation; SpO2, saturation of hemoglobin with oxygen as measured by pulse oximetry.
Discussion
The present study examined the potential correlation of sleep characteristics with glucose metabolism in nondiabetic men with OSAS. Our results suggest that in nondiabetic male OSAS patients without comorbidities, the severity of OSAS (evaluated by the number of respiratory cessation events, the indices of hypoxemia during sleep and the arousal index) is associated with increased fasting glucose and HbA1c levels.
The novel association of HbA1c with severity of OSAS appears interesting, and may have important implications in clinical practice. Essentially, not only is HbA1c the major target for the prevention of complications in type 2 DM,19 but it also represents a significant risk marker for cardiovascular disease in the general population.20–22 It is, therefore, tempting to consider whether the severity of OSAS may be viewed as a risk marker for cardiovascular disease. This assumption enhances the increasing awareness that OSAS itself is a risk factor for cardiovascular morbidity.23 Equally importantly, HbA1c is being increasingly appreciated as a risk marker for the development of DM in the general population.24,25 Hence, the severity of OSAS may be associated with increased risk for the development of DM. The utility of HbA1c in the prediction of diabetes in subjects with OSAS is plausible, given the association between these two conditions. However, the number of our patients is small, and further research is required to confirm our findings.
Similarly, a significant correlation was observed between fasting glucose levels and severity of nocturnal hypoxemia (evaluated by the average SpO2 and the minimum SpO2 during sleep). In view of the fact that the level of hyperglycemia is an established risk factor for both diabetes20,25 and cardiovascular morbidity and mortality,20,26–28 this association enhances the significance of the severity of OSAS as a risk factor for diabetes and vascular disease. While it is known that OSAS and impaired glucose homeostasis are interrelated,6–11 our dataset emphasizes the role of OSAS severity in putting otherwise healthy male patients at increased cardiovascular risk.
Both fasting glucose and HbA1c exhibited a significant correlation with AI. This finding indicates that the effect of OSAS on glycemic profile was, partly at least, mediated by sympathetic nervous system activation.1,5 The latter is a recognized mechanism underlying the pathogenesis of insulin resistance and impaired glucose metabolism in OSAS patients.2,5–8 Our data provide additional evidence for the potential role of sympathetic overactivity in the modification of hyperglycemia in otherwise healthy individuals with OSAS.
Finally, BMI did not correlate with HbA1c levels or glucose levels. Hence, OSAS severity was directly associated with impaired glucose metabolism independently of obesity. This result agrees with studies showing that SDB is associated with glucose intolerance and insulin resistance independently of BMI.8,9,12,13 The role of SDB is enhanced by evidence showing that experimental hypoxia directly causes glucose intolerance.14 However, other workers advocate an important role for central obesity in impaired glucose metabolism, and so recent state-of-the art reviews highlight the need for further clarification.15,16 In the type of subjects herein examined, OSAS severity appears to outweigh obesity, as demonstrated by its direct association with impaired glucose metabolism.
Notably, this study excluded women, in order to avoid potential discrepancies between the two genders. Indeed, there is evidence of a different effect of sleep apnea on metabolic profile and on inflammatory response in women, partly at least due to different hormonal regulation.1,29 For this reason, the correlations found need to be investigated in women as well.
The limitations of the present report include the small number of patients and the cross-sectional design. Based on our findings, it is plausible to propose that risk factors for diabetes and vascular disease in otherwise healthy OSAS patients may be identified in association with OSAS severity. Nonetheless, there is no prospective data to confirm that this risk translates into worse outcome in actual clinical practice. Such follow-up was beyond the scope of this study, and further prospective research is needed to provide a definite answer.
In conclusion, among nondiabetic men with OSAS, the severity of this condition is associated with increased HbA1c levels and increased fasting glucose. Thus, the severity of OSAS may be an additional marker of cardiovascular risk as well as of future diabetes in these subjects. Nevertheless, the clinical significance of our observations remains to be confirmed by prospective studies.
Footnotes
Disclosures
The authors report no conflicts of interest in this work.
References
- 1.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;15(2):136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNicholas WT, Bonsigore MR. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29(1):156–178. doi: 10.1183/09031936.00027406. [DOI] [PubMed] [Google Scholar]
- 3.West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax. 2006;61(11):945–950. doi: 10.1136/thx.2005.057745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Einhorn D, Stewart DA, Erman MK, Gordon N, Philis-Tsimikas A, Casal E. Prevalence of sleep apnea in a population of adults with type 2 diabetes mellitus. Endocr Pract. 2007;13(4):355–362. doi: 10.4158/EP.13.4.355. [DOI] [PubMed] [Google Scholar]
- 5.Meslier N, Gagnadoux F, Giraud P, et al. Impaired glucose-insulin metabolism in males with obstructive sleep apnoea syndrome. Eur Respir J. 2003;22(1):156–160. doi: 10.1183/09031936.03.00089902. [DOI] [PubMed] [Google Scholar]
- 6.Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165(5):670–676. doi: 10.1164/ajrccm.165.5.2103001. [DOI] [PubMed] [Google Scholar]
- 7.Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med. 2002;165(5):677–682. doi: 10.1164/ajrccm.165.5.2104087. [DOI] [PubMed] [Google Scholar]
- 8.Punjabi NM, Shahar E, Redline S, Gottlieb DJ, Givelber R, Resnick HE. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am J Epidemiol. 2004;160(6):521–530. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 9.Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005;172(12):1590–1595. doi: 10.1164/rccm.200504-637OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shin C, Kim J, Lee S, et al. Association of habitual snoring with glucose and insulin metabolism in nonobese Korean adult men. Am J Respir Crit Care Med. 2005;171(3):287–291. doi: 10.1164/rccm.200407-906OC. [DOI] [PubMed] [Google Scholar]
- 11.Udwadia ZF, Doshi AV, Lonkar SG, Singh CI. Prevalence of sleep-disordered breathing and sleep apnea in middle-aged urban Indian men. Am J Respir Crit Care Med. 2004;169(2):168–173. doi: 10.1164/rccm.200302-265OC. [DOI] [PubMed] [Google Scholar]
- 12.Tassone F, Lanfranco F, Gianotti L, et al. Obstructive sleep apnoea syndrome impairs insulin sensitivity independently of anthropometric variables. Clin Endocrinol (Oxf) 2003;59(3):374–379. doi: 10.1046/j.1365-2265.2003.01859.x. [DOI] [PubMed] [Google Scholar]
- 13.Makino S, Handa H, Suzukawa K, et al. Obstructive sleep apnoea syndrome, plasma adiponectin levels, and insulin resistance. Clin Endocrinol (Oxf) 2006;64(1):12–19. doi: 10.1111/j.1365-2265.2005.02407.x. [DOI] [PubMed] [Google Scholar]
- 14.Oltmanns KM, Gehring H, Rudolf S, et al. Hypoxia causes glucose intolerance in humans. Am J Respir Crit Care Med. 2004;169(11):1231–1237. doi: 10.1164/rccm.200308-1200OC. [DOI] [PubMed] [Google Scholar]
- 15.Tasali E, Mokhlesi B, Van Cauter E. Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest. 2008;133(2):496–506. doi: 10.1378/chest.07-0828. [DOI] [PubMed] [Google Scholar]
- 16.Shaw JE, Punjabi NM, Wilding JP, et al. Sleep-disordered breathing and type 2 diabetes: a report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res Clin Pract. 2008;81(1):2–12. doi: 10.1016/j.diabres.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 17.International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–1334. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Academy of Sleep Medicine (AASM) International Classification of Sleep Disorders. Westchester, IL: AASM; 2005. [Google Scholar]
- 19.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Vegt F, Dekker JM, Ruhe HG, et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia. 1999;42(8):926–931. doi: 10.1007/s001250051249. [DOI] [PubMed] [Google Scholar]
- 21.Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N. Asso- with cardiovascular disease and mortality in ciation of hemoglobin A1c adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med. 2004;141(6):413–420. doi: 10.7326/0003-4819-141-6-200409210-00006. [DOI] [PubMed] [Google Scholar]
- 22.Khaw KT, Wareham N. Glycated hemoglobin as a marker of cardiovascular risk. Curr Opin Lipidol. 2006;17(6):637–643. doi: 10.1097/MOL.0b013e3280106b95. [DOI] [PubMed] [Google Scholar]
- 23.Thurnheer R. Obstructive sleep apnea and cardiovascular disease – time to act! Swiss Med Wkly. 2007;137(15–16):217–222. doi: 10.4414/smw.2007.11671. [DOI] [PubMed] [Google Scholar]
- 24.Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ. Utility of hemoglobin A1c in predicting diabetes risk. J Gen Intern Med. 2004;19(12):1175–1180. doi: 10.1111/j.1525-1497.2004.40178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inoue K, Matsumoto M, Kobayashi Y. The combination of fasting plasma glucose and glycosylated hemoglobin predicts type 2 diabetes in Japanese workers. Diabetes Res Clin Pract. 2007;77(3):451–458. doi: 10.1016/j.diabres.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 26.Beks PH, Mackaay AJ, de Vries H, de Neeling JN, Bouter LM, Heine RJ. Carotid artery stenosis is related to blood glucose level in an elderly Caucasian population: the Hoorn Study. Diabetologia. 1997;40(3):290–298. doi: 10.1007/s001250050676. [DOI] [PubMed] [Google Scholar]
- 27.Beks PJ, Mackaay AJ, de Neeling JN, de Vries H, Bouter LM, Heine RJ. Peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: the Hoorn study. Diabetologia. 1995;38(1):86–96. doi: 10.1007/BF02369357. [DOI] [PubMed] [Google Scholar]
- 28.Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: the Chennai Urban Population Study. Diabetes Care. 2000;23(9):1295–1300. doi: 10.2337/diacare.23.9.1295. [DOI] [PubMed] [Google Scholar]
- 29.Miller MA, Kandala NB, Kivimaki J, et al. Gender differences in the cross-sectional relationships between sleep duration and markers of inflammation: Whitehall II Study. Sleep. 2009;32(7):857–864. [PMC free article] [PubMed] [Google Scholar]