Abstract
Vaccinating with live, conditionally attenuated, pigmentation (Pgm)-deficient Yersinia pestis primes T cells that protect mice against pneumonic plague. However, Pgm-deficient strains are not considered safe for human use because they retain substantial virulence in animal models. Y. pestis strains engineered to express Escherichia coli LpxL are avirulent owing to constitutive production of lipopolysaccharide with increased Toll-like receptor 4-activating ability. We generated an LpxL-expressing Pgm-deficient strain (D27-pLpxL) and demonstrate here that this avirulent strain retains the capacity to prime protective T cells. Compared with unvaccinated controls, mice immunized intranasally with live D27-pLpxL exhibit a decreased bacterial burden and increased survival when challenged intranasally with virulent Y. pestis. T cells provide a substantial degree of this protection, as vaccine efficacy is maintained in B-cell-deficient μMT mice unless those animals are depleted of CD4 and CD8 T cells at the time of challenge. Upon challenge with Y. pestis, pulmonary T-cell numbers decline in naive mice, whereas immunized mice show increased numbers of CD44high CD43high effector T cells and T cells primed to produce tumor necrosis factor alpha and gamma interferon; neutralizing these cytokines at the time of challenge abrogates protection. Immunization does not prevent dissemination of Y. pestis from the lung but limits bacterial growth and pathology in visceral tissue, apparently by facilitating formation of granuloma-like structures. This study describes a new model for studying T-cell-mediated protection against pneumonic plague and demonstrates the capacity for live, highly attenuated, Y. pestis vaccine strains to prime protective memory T-cell responses safely.
Plague, also known as the Black Death, has killed hundreds of millions of people over the course of three major pandemics (33). Yersinia pestis, the etiologic agent of plague, is a gram-negative facultative intracellular bacterium naturally transmitted to mammals by the bite of an infected flea (31). There are three clinical forms of Y. pestis infection: bubonic, septicemic, and pneumonic plague (5). The bubonic form is characterized by a swelling of lymph nodes draining the fleabite. Left untreated, bubonic plague typically progresses to bacteremia and septicemia. The pneumonic form of plague, which can spread from person to person without an intermediary insect vector, occurs when Y. pestis colonizes the lung, either as a secondary consequence of bacteremia or via direct inhalation of infectious bacilli. Unless treated with antibiotics soon after symptom onset, all forms of plague can be fatal. Pneumonic plague is particularly fulminant and often is lethal even with antibiotic treatment (5, 20, 23).
Armed with knowledge of the cause of plague and its routes of transmissibility, public health efforts have substantially reduced the likelihood of a modern-day pandemic. However, sporadic plague outbreaks continue to afflict human populations (47), and Y. pestis is now entrenched in rodent populations on nearly every continent (7). Moreover, Y. pestis displays significant clonal diversity, and some strains already resist treatment with multiple antibiotics (13, 19). In addition to these natural threats, there is concern that Y. pestis may be exploited as a biological weapon (19). Accordingly, substantial resources are being devoted to the development of plague countermeasures.
The search for a safe and effective plague vaccine began shortly after Yersin identified the causative agent (48). Immunization with killed “whole-cell” Y. pestis bacilli protects humans against bubonic plague, but vaccines of this type are reactogenic, require frequent boosting, and are not thought to protect humans from pneumonic plague (5, 24, 43). Subunit vaccines comprised of the Y. pestis F1 and/or LcrV protein appear to be safe and well tolerated by humans (46). These vaccines provide substantial protection in animal models of pneumonic plague (38, 43). However, the F1/LcrV-based vaccines have failed, thus far, to fully protect nonhuman primates, and we lack adequate knowledge about immune correlates of protection to confidently predict whether or not they will protect humans (3, 38).
Administering monoclonal antibodies (MAbs) specific for F1 or LcrV can protect mice against pneumonic challenge with fully virulent Y. pestis (2, 15, 16). Given this documented efficacy of antibody-mediated defense, most F1/LcrV vaccine efforts have aimed to induce high-titer antibodies. However, bioweaponeers potentially could circumvent vaccines based solely on F1 and LcrV, since F1-deficient strains retain virulence and LcrV variants exist (38, 43). Moreover, a number of studies suggest that antibodies alone may not provide optimal protection against pneumonic plague (39). First, levels of antibodies in F1/LcrV-immunized mice and nonhuman primates often fail to correlate with protective efficacy (3). Second, F1/LcrV-immunized STAT4-deficient mice are poorly protected against plague challenge, despite possessing high antibody titers (8). STAT4-deficient mice lack the capacity to mount robust type 1 immune responses, and our recent studies indicate that the protection mediated by F1- and LcrV-specific antibody benefits from gamma interferon (IFN-γ) and tumor necrosis factor alpha (TNF-α), cytokine products of type 1 immunity (21). Chattopadhyay et al. recently demonstrated that protection conferred by immunizing mice with an LcrV-expressing viral vector benefits from the presence of CD4 T cells at the time of challenge (6). Together, these observations raise the possibility that high-titer antibody may not suffice to protect humans from pneumonic plague and suggest that vaccines harnessing both humoral and cellular defense mechanisms should provide superior defense (38, 39).
Live vaccines typically prime both antibody- and cell-mediated immune responses. Pigmentation (Pgm)-deficient strains of Y. pestis arise spontaneously during in vitro passage, usually owing to deletion of a 102-kb region of the chromosome that encodes proteins related to iron utilization (10). Immunization with Pgm-deficient strains, which are highly attenuated when administered subcutaneously (44), protects rodents against pneumonic plague (36). A Pgm-deficient vaccine strain, denoted EV76, was developed for human use nearly a century ago (14). It was administered to tens of millions of humans (14) and is still in use today in Russia (9, 50). However, live plague vaccines have never been licensed in the United States or the United Kingdom, in part because Pgm-deficient strains are only conditionally attenuated in mice, which tolerate high doses administered subcutaneously but succumb to disease at relatively low doses administered intravenously or intranasally (28, 29, 32, 44, 45). Moreover, primate species display various degrees of susceptibility (9, 25, 45).
In a prior study we demonstrated that immunizing mice with live conditionally attenuated Pgm-deficient Y. pestis strain D27 primes T-cell-mediated protection against pneumonic challenge (28). Here we extend that observation to D27-pLpxL, a Pgm-deficient Y. pestis strain rendered avirulent by engineered constitutive expression of inflammatory forms of lipopolysaccharide. The protection conferred by this strain does not require antibody production and is associated with robust priming of cytokine-producing T cells that enable leukocytes to form granuloma-like structures and resist the cytopathic effects that typically characterize visceral Y. pestis infections. These findings suggest that it should be possible to generate safe, highly attenuated, live Y. pestis vaccines that prime protective memory T-cell responses.
MATERIALS AND METHODS
Mice.
Wild-type, B-cell-deficient (μMT; B6.129S2-Igh-6tm1Cgn), and T-cell-deficient (TCRbd; B6.129P2-Tcrbtm1Mom Tcrdtm1Mom) mice on the C57BL/6 background were purchased from The Jackson Laboratory (Bar Harbor, ME) and bred in the specific-pathogen-free Trudeau Institute Animal Breeding Facility after embryo rederivation. Experimental mice were matched for age and sex. Mice were cared for according to Trudeau Institute Animal Care and Use Committee guidelines.
Bacteria.
All challenge studies used Y. pestis strain D27 (22), a Pgm-negative variant of Y. pestis KIM that was generously provided by Robert Brubaker (Michigan State University). Y. pestis bacilli from frozen glycerol stocks were grown overnight at 26°C with continuous shaking in Bacto heart infusion broth (Becton Dickinson and Company) supplemented with 2.5 mM CaCl2. After dilution to an optical density at 620 nm of 0.1, they were regrown for 3 h at 26°C, washed with saline, quantified by measuring the optical density at 620 nm, and applied in a volume of 30 μl saline to the nares of mice lightly anesthetized with isoflurane. The number of bacteria in the inoculating dose was confirmed by plating. The intranasal median lethal dose (MLD) of strain D27, as calculated by the method of Reed and Muench (34), is approximately 1 × 104 CFU when the strain is grown and administered as described above. The vaccine strain D27-pLpxL and control strain D27-pBR322 were prepared by transforming strain D27 with plasmid pLpxL or pBR322, respectively (26, 35). These strains were stored and grown as described for D27 in culture medium supplemented with 100 μg/ml ampicillin.
T-cell depletion and cytokine neutralization.
All MAbs were supplied by Bio X Cell (West Lebanon, NH), which reported endotoxin levels of less than 1.7 units per mg. T cells were depleted by treating mice with 1 mg rat immunoglobulin G2b (IgG2b) MAb specific for mouse CD4 (clone GK1.5) and/or CD8 (clone 2.43), diluted in phosphate-buffered saline and administered as two intraperitoneal doses of 500 μg each on the day before and the day after challenge. Control mice received an equal quantity of isotype-matched rat IgG2b MAb (clone LTF-2).
Cytokines were neutralized by treating mice with 1 mg rat IgG1 MAb specific for TNF-α (clone XT3.11) and 600 μg MAb specific for IFN-γ (clone XMG1.2) administered intraperitoneally. Control mice received an equal quantity of isotype-matched rat IgG1 MAb (clone HRPN).
Survival end points and bacterial burden.
In all survival studies, recumbent animals were considered moribund and euthanized. For measurements of bacterial burden, mice were euthanized by carbon dioxide narcosis at the indicated day after initiation of infection. Liver and lung tissues were harvested and plated for CFU determination as described previously (28, 30).
Flow cytometry.
Lungs were perfused with saline, minced, and digested with collagenase and DNase (28). Viable cells were quantified using trypan blue exclusion. Cells were stained immediately with CD4-fluorescein isothiocyanate (clone RM4-5), CD8-peridinin chlorophyll protein (clone 53-6.7), CD43-phycoerythrin (clone 1B11), and CD44-allophycocyanin (clone IM7) or were stained with CD4-fluorescein isothiocyanate, CD8-peridinin chlorophyll protein, TNF-α-phycoerythrin (clone MP6-XT22), and IFN-γ-allophycocyanin (clone XMG1.2) after culture on anti-CD3 (clone 145-2C11; 2 μg/ml)-coated plates for 5 h in medium containing brefeldin A (Sigma; 12.5 μg/ml). Data were collected on a Becton Dickinson FACSCalibur using forward- and side-scatter gating to exclude dead cells and debris. For each sample, at least 2,000 CD8-positive events were collected. Data were analyzed using FlowJo version 8.8 software (Tree Star, Inc.). For each condition, representative zebra plots with outliers shown as dots were created by concatenating the cytometry files of five individual mice.
Histology.
Tissues were fixed in 10% neutral buffered formalin, embedded in paraffin, sectioned, and stained with hematoxylin and eosin. Representative photomicrographs are presented at a magnification of ×200.
Statistics.
Survival data were analyzed by log rank tests. Flow cytometry and CFU data were analyzed by parametric tests (Student's t test or one-way analysis of variance, as indicated). When the bacterial burden fell below the detection limit of our assays, CFU were assigned values equal to the detection limit and, consequently, the data were analyzed by nonparametric tests (Mann-Whitney or Kruskal-Wallis, as indicated).
RESULTS
Y. pestis constitutively producing Escherichia coli LpxL is highly attenuated when administered by the intranasal route, despite disseminating to visceral tissue.
Transformation of Y. pestis with a plasmid encoding E. coli LpxL promotes constitutive production of hexa-acylated forms of LPS, thereby attenuating virulence by increasing Toll-like receptor 4 (TLR4)-activating ability (26). We transformed D27, a well-characterized Pgm-deficient variant of the Y. pestis KIM strain, with the same LpxL-producing plasmid described previously, thereby creating strain D27-pLpxL (35). To generate a control strain, we also transformed D27 with the parental plasmid, pBR322. As shown in Fig. 1A, strain D27-pBR322 retained virulence when administered intranasally to wild-type C57BL/6 mice. The MLD for D27-pBR322 was 6 × 103 CFU, which is nearly identical to that reported previously for D27 (28). In striking contrast, no mice succumbed to intranasal infection with strain D27-pLpxL, even at doses of as high as 1 × 107 CFU. We conclude that D27-pLpxL is more than 1,500-fold attenuated when administered to wild-type mice by the intranasal route.
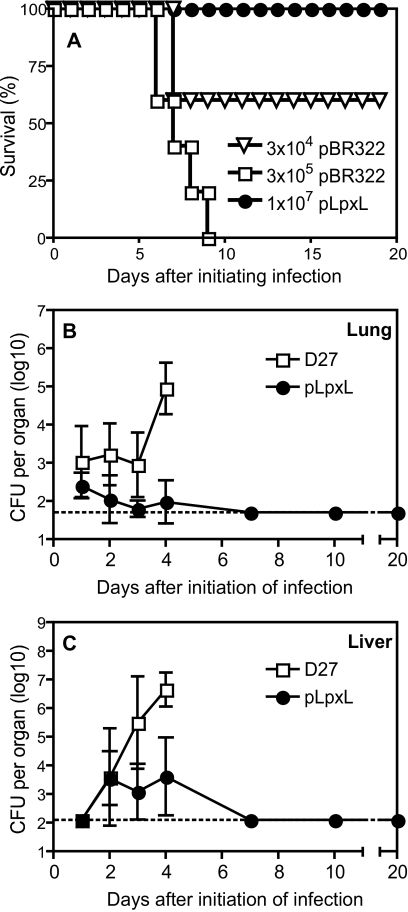
FIG. 1.
D27-pLpxL is avirulent when administered by the intranasal route. (A) Wild-type C57BL/6 mice were infected intranasally with the indicated dose of D27-pBR322 or D27-pLpxL (n = 5 mice/group). (B and C) Wild-type C57BL/6 mice were infected intranasally with 2 × 105 CFU D27 or 2 × 106 CFU of D27-pLpxL, and the bacterial burden in lung (B) or liver (C) was measured on the indicated days postinfection. Data are compiled from two independent experiments and are the means ± standard deviations for 5 mice per group for days 1, 2, 3, 7, 10, and 20 and 10 mice per group for day 4.
In subsequent studies we compared the pulmonary and hepatic bacterial burdens in mice infected with D27 or D27-pLpxL. As shown in Fig. 1B, and as reported previously (28), intranasal infection with 20 MLDs of strain D27 (2 × 105 CFU) led to a relatively constant level of pulmonary infection for several days followed by an abrupt increase in burden on day 4 postinfection. Strain D27 disseminated to the liver by day 2 postinfection, and the hepatic burden then increased more than 10-fold per day through day 4 (Fig. 1C).
Infection with D27-pLpxL also caused a persistent acute infection. Specifically, intranasal administration of 2 × 106 CFU strain D27-pLpxL led to a measurable pulmonary burden in most animals for the first 4 days of infection, although the burden was lower than that observed in mice infected with D27 and fell below the detection level of our assay in all animals by day 7 postinfection (Fig. 1B). Notably, despite the lower pulmonary burden and attenuated virulence, D27-pLpxL still disseminated to the liver and persisted in that organ through day 4 postinfection (Fig. 1C). We obtained nearly identical CFU numbers when plating infected tissue on agar containing or lacking ampicillin (not shown), indicating that the pLpxL plasmid was stably maintained in vivo, at least through day 4 postinfection.
Immunization with strain D27-pLpxL confers T-cell-dependent protection against pneumonic plague.
Montminy et al. previously reported that subcutaneously infecting wild-type mice with a Pgm-positive Y. pestis strain expressing LpxL primed immune responses that confer resistance to virulent Y. pestis challenge (26). Given that wild-type mice survived intranasal infection with high doses of D27-pLpxL, a Pgm-negative strain expressing LpxL (Fig. 1), we investigated whether this exposure immunized against virulent Y. pestis challenge. Mice were intranasally infected with 2 × 106 CFU of strain D27-pLpxL, rested for 30 days, and then challenged intranasally with 20 MLDs of strain D27. In parallel, we challenged age- and sex-matched control mice that had not been exposed to D27-pLpxL. In this model of pneumonic plague, all mice previously infected with D27-pLpxL survived challenge with virulent Y. pestis, whereas none of the control mice survived (not shown).
We next investigated whether T cells or B cells participate in the protection conferred by immunization with live D27-pLpxL. Wild-type mice, μMT mice, and TCRbd-deficient mice were infected intranasally with 2 × 106 CFU of strain D27-pLpxL, rested for 60 days, and then challenged intranasally with 20 MLDs of strain D27. This challenge dose is lethal for naive wild-type, μMT, and TCRbd-deficient mice (not shown). All D27-pLpxL-immunized wild-type mice and B-cell-deficient μMT mice survived the virulent Y. pestis challenge, whereas significantly fewer (40%) of the immunized T-cell-deficient TCRbd mice survived (Fig. 2A) (P < 0.05). Measurements of bacterial burdens in lung and liver tissues on day 3 after challenge with strain D27 helped to explain the reduced survival of the T-cell-deficient mice (Fig. 2B). In immunized wild-type mice, we observed low numbers of bacterial CFU in the lungs and no evidence of dissemination to hepatic tissue. The lung and liver tissues of the immunized B-cell-deficient μMT mice harbored somewhat more bacteria than those of the wild-type mice, but these increases did not achieve statistical significance. In contrast, the lung and liver tissues of the immunized T-cell-deficient mice harbored significantly increased bacterial CFU (P < 0.05). Notably, bacteria had disseminated to the livers of all the T-cell-deficient mice. Altogether, these findings suggest that both B and T cells contribute to host defense in this model of vaccine-mediated protection against pneumonic plague but that T cells play a more critical role in restraining Y. pestis growth and dissemination after immunization with strain D27-pLpxL.
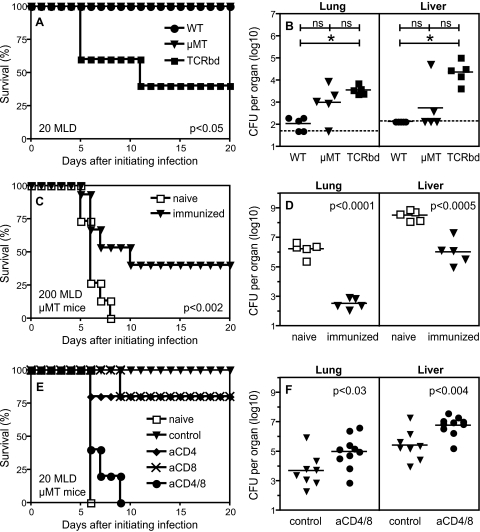
FIG. 2.
T cells play critical roles during protection mediated by immunization with D27-pLpxL. (A and B) Wild-type mice (WT), B-cell-deficient mice (μMT), and T-cell-deficient mice (TCRbd) were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 20 MLDs of strain D27. In comparison with wild-type mice or μMT mice, TCRbd mice displayed significantly reduced survival (n = 5 mice/group; P < 0.05 by log rank test). At day 3 after challenge, bacterial CFU were increased significantly in the lung and liver tissues of TCRbd mice (n = 5 mice/group; ns, not significant; *, P < 0.05 by Kruskal-Wallis with Dunn's multiple comparison test). (C and D) B-cell-deficient μMT mice were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 200 MLDs of strain D27. In comparison with naive controls, mice immunized with D27-pLpxL displayed significantly greater survival (n = 15 mice/group; P < 0.002 by log rank test). At day 5 after challenge, bacterial CFU were decreased significantly in the lung (P < 0.0001) and liver (P < 0.0005) tissues of immunized mice (n = 5 mice/group; Student's t test). (E and F) B-cell-deficient μMT mice were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 20 MLDs of strain D27. At the time of challenge, mice received MAb specific for CD4 (aCD4), CD8 (aCD8), or both CD4 and CD8 (aCD4/8) or an isotype-matched MAb (control). In parallel, sex- and age-matched naive mice were challenged with 20 MLDs of strain D27. Mice treated with MAb specific for both CD4 and CD8 displayed significantly reduced survival in comparison with mice treated with control MAb (n = 5 mice/group; P = 0.0015 by log rank test). Similar results were observed in a second experiment. At day 5 after challenge, bacterial CFU were increased significantly in lungs (P < 0.03) and livers (P < 0.004) of immunized mice treated with MAb specific for both CD4 and CD8 (n = 8 to 10 mice/group; Student's t test).
To investigate the degree of T-cell-mediated protection conferred by immunization with strain D27-pLpxL, we immunized B-cell-deficient μMT mice, rested them for 60 days, and challenged them with 200 MLDs of strain D27, a 10-fold-higher dose than used in any of our prior studies. All naive control mice succumbed to this high-dose challenge, whereas significantly more (6 of 15, 40%; P < 0.002) of the immunized mice survived (Fig. 2C). Measurements of bacterial CFU at day 5 after challenge revealed that immunization with D27-pLpxL did not prevent bacterial dissemination in B-cell-deficient mice (Fig. 2D) but significantly reduced bacterial burdens in both lung (P < 0.0001) and liver (P < 0.0005) tissues.
To further define the roles for T cells in this model of vaccine-mediated protection against pneumonic plague, we immunized μMT mice with strain D27-pLpxL, waited 60 days, administered MAb specific for mouse CD4 and/or CD8, and then challenged intranasally with 20 MLDs of strain D27. Control animals included naive mice and immunized mice treated with an isotype-matched MAb of irrelevant specificity. As shown in Fig. 2E and F, administration of MAb specific for either CD4 or CD8 led to a slight decrease in protection, whereas simultaneous administration of MAb specific for both CD4 and CD8 fully abrogated protection. These findings suggest that protection conferred by immunizing μMT mice with strain D27-pLpxL is mediated by both CD4 and CD8 T cells. Measurements of bacterial burden at day 5 after challenge revealed that depletion of CD4 and CD8 cells significantly increased the numbers of CFU in pulmonary and hepatic tissues (Fig. 2F) (P < 0.03 and P < 0.004, respectively, for lung and liver).
T cells facilitate the formation of granuloma-like structures in mice immunized with strain D27-pLpxL.
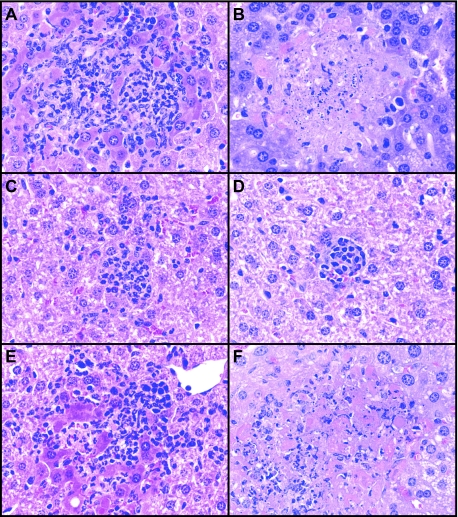
Prior studies of hepatic histopathology in naive mice infected with Pgm-deficient Y. pestis described microabscesses containing predominantly polymorphonuclear neutrophils that fail to clear the bacteria and, rather, progress to large areas of necrosis (27, 41). Likewise, we observed that naive μMT mice challenged with D27 developed areas of hepatic inflammation characterized initially by clusters of leukocytes on day 3 after infection that appear to disintegrate as the infection progresses, culminating in widespread necrosis by day 5 (Fig. 3A and B). In mice immunized with D27-pLpxL, clusters of leukocytes were also evident on day 3 after challenge with D27, although they were smaller in size and number (Fig. 3C). In striking contrast to the case in unimmunized mice, these clusters became more clearly circumscribed and granuloma-like as the infection progressed in the immunized mice (Fig. 3D). Depleting CD4 and CD8 cells from the immunized mice at the time of D27 challenge tended to suppress the formation of these granuloma-like structures (Fig. 3F), resulting in necrosis similar to that observed in the unimmunized mice (Fig. 3B).
FIG. 3.
Immunization with D27-pLpxL alters hepatic pathology in mice challenged with pneumonic plague. B-cell-deficient μMT mice were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 20 MLDs of strain D27. On day 3 (A, C, and E) and day 5 (B, D, and F) after challenge, hepatic tissue was collected, fixed with formalin, embedded in paraffin, sectioned, and stained with hematoxylin and eosin. Tissue was collected and analyzed, in parallel, from unimmunized mice (A and B) and immunized mice (C and D) and from immunized mice treated with MAb specific for both CD4 and CD8 (aCD4/8) (E and F) at the time of challenge.
Immunization with strain D27-pLpxL overcomes an infection-associated depletion of pulmonary T cells in mice challenged with pneumonic plague.
Given that T cells contribute to protection mediated by immunization with strain D27-pLpxL (Fig. 2 and 3), we investigated whether enhanced T-cell responses could be detected in the immunized mice. On day 5 after intranasal challenge with 20 MLDs of strain D27, we collected lung tissue from control and immunized μMT mice. We also collected tissue from age- and sex-matched naive μMT mice. After isolating leukocytes, we measured frequencies of pulmonary CD4+ cells and CD8+ cells using flow cytometry.
As shown in Fig. 4 (top panel), the CD4/CD8 cell ratio was nearly 1.0 in the lungs of naive μMT mice. After challenge infection of unimmunized mice with 20 MLDs of strain D27, the frequency of CD4+ cells in the lungs decreased notably, resulting in a CD4/CD8 ratio of 0.4. Immunization with strain D27-pLpxL prevented the infection-stimulated decrease in the CD4/CD8 ratio and, moreover, increased the frequencies of both CD4+ and CD8+ cells.
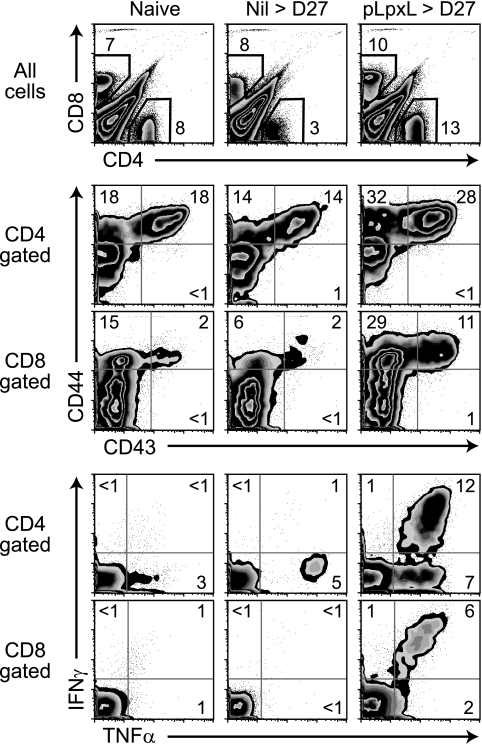
FIG. 4.
Flow cytometry reveals altered frequencies of CD4 and CD8 T cells in the lungs of mice immunized with D27-pLpxL. B-cell-deficient μMT mice were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 20 MLDs of strain D27. On day 5 after challenge, leukocytes were isolated from lung tissue and analyzed by flow cytometry. In parallel, leukocytes from unimmunized mice challenged with 20 MLDs of strain D27 were analyzed. Each plot depicts a concatenation of data from five mice per condition. The numbers depict the percentage of cells present in the indicated gate or quadrant. Similar results were observed in three independent experiments.
Infection and immunization also led to significant changes in the absolute numbers of pulmonary T cells. As shown in Fig. 5A, challenge with 20 MLDs of strain D27 significantly reduced the number of pulmonary CD4+ cells (P < 0.001). Immunization with D27-pLpxL prevented this reduction and, instead, significantly increased the number of CD4+ cells (P < 0.001). Overall, this led to a sevenfold increase in CD4+ cell numbers in immunized mice compared with unimmunized mice challenged with 20 MLDs of strain D27. Challenge with D27 also significantly reduced the absolute number of pulmonary CD8+ cells in unimmunized mice (Fig. 5A) (P < 0.01). As with CD4+ cells, immunization prevented this reduction and significantly increased the number of pulmonary CD8+ cells in the infected mice (P < 0.001).
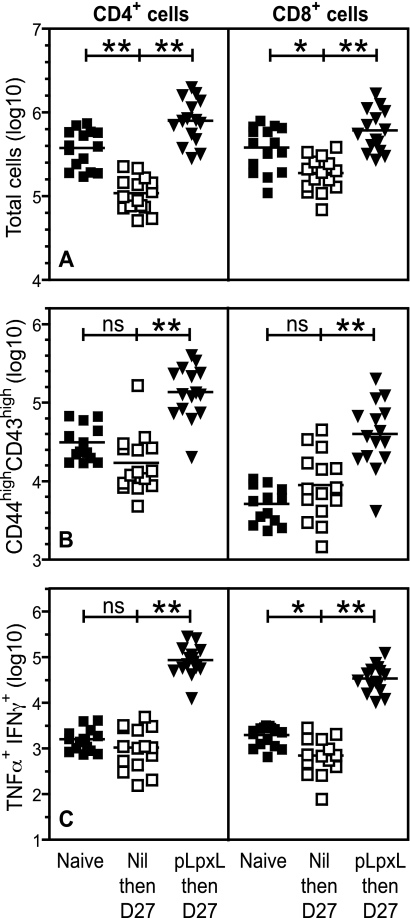
FIG. 5.
Increased numbers of CD4 and CD8 T cells in the lungs of mice immunized with D27-pLpxL. B-cell-deficient μMT mice were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 20 MLDs of strain D27 (triangles). On day 5 after challenge, leukocytes were isolated from lung tissue, counted, and analyzed by flow cytometry. In parallel, leukocytes from sex- and age-matched untreated naive mice (solid squares) and from unimmunized mice challenged with 20 MLDs of strain D27 (open squares) were analyzed. Data are pooled from three independent experiments, and statistical significance was measured by one-way analysis of variance with Bonferroni's multiple-comparison test (ns, not significant; *, P < 0.01; **, P < 0.001).
Immunization with strain D27-pLpxL increases the number of CD44high CD43high T cells in the lungs of mice challenged with pneumonic plague.
In mouse models of respiratory virus infection, antigen-specific T cells in the lung express high levels of CD44 and CD43 (17, 18). As shown in the middle panels of Fig. 4, we observed increased frequencies of CD44high CD43high cells in the lungs of mice immunized with strain D27-pLpxL compared with unimmunized mice. These frequency changes reflected significant increases in the absolute numbers of CD44high CD43high cells when comparing unimmunized and immunized mice challenged with 20 MLDs of strain D27 (Fig. 5B) (P < 0.001). Specifically, immunization increased the frequency of CD4+ CD44high CD43high cells eightfold and increased the frequency of CD8+ CD44high CD43high cells fourfold.
Immunization with strain D27-pLpxL increases the number of TNF-α- and IFN-γ-producing T cells in the lungs of mice challenged with pneumonic plague.
We also measured the frequencies of cytokine-producing T cells in the lungs of mice immunized with D27-pLpxL. Specifically, we used an intracellular staining procedure to quantify cells that had the capacity to produce TNF-α and IFN-γ upon ex vivo activation with plate-bound MAb specific for CD3, a component of the T-cell receptor. As shown in the lower panels of Fig. 4, very few pulmonary CD4 or CD8 cells in naive μMT mice produced either TNF-α or IFN-γ. Five days after challenge with 20 MLDs of strain D27, we observed a small increase in the frequency of TNF-α-producing CD4+ cells in unimmunized mice; however, there was no measurable increase in the frequency of TNF-α-producing CD8+ cells or in the frequency of CD4+ or CD8+ cells producing IFN-γ. In striking contrast, the frequencies of CD4+ cells and CD8+ cells simultaneously producing both TNF-α and IFN-γ increased dramatically in the mice immunized with strain D27-pLpxL prior to challenge. The absolute number of TNF-α- and IFN-γ-producing CD4+ cells increased more than 80-fold in the immunized mice, while the number of TNF-α- and IFN-γ-producing CD8+ cells increased nearly 50-fold (Fig. 5C).
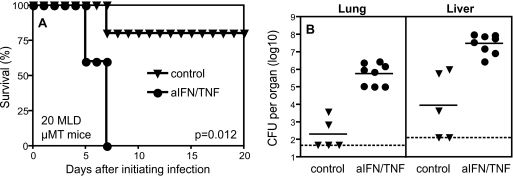
TNF-α and IFN-γ contribute to protection mediated by immunization with strain D27-pLpxL.
Given that immunization with strain D27-pLpxL was associated with an accumulation of pulmonary T cells with the capacity to produce TNF-α and IFN-γ (Fig. 4 and 5), we investigated functional roles for TNF-α and IFN-γ. We immunized μMT mice with strain D27-pLpxL, rested them for 60 days, treated them with neutralizing MAbs specific for mouse TNF-α and IFN-γ, and then challenged them with 20 MLDs of strain D27. Control animals included unimmunized mice and immunized mice treated with an isotype-matched MAb of irrelevant specificity. As shown in Fig. 6, neutralizing cytokines at the time of challenge fully abrogated protection in this model of pneumonic plague, as measured by survival (P < 0.015) and by bacterial burdens in lung and liver (both P < 0.002).
FIG. 6.
IFN-γ and TNF-α contribute to protection mediated by immunization with D27-pLpxL. B-cell-deficient μMT mice were infected intranasally with strain D27-pLpxL, rested for 60 days, and then challenged with 20 MLDs of strain D27. At the time of challenge, mice received MAb specific for IFN-γ and TNF-α (aIFN/TNF) or an isotype-matched MAb (control). (A) Survival was decreased significantly in mice treated with MAb specific for IFN-γ and TNF-α compared with mice treated with isotype-matched control MAb (n = 5 mice/group; P = 0.012 by log rank test). (B) Bacterial CFU were measured at day 5 after challenge with strain D27. Treatment with MAb specific for IFN-γ and TNF-α significantly increased bacterial burdens in lung and liver (both P < 0.002 by Mann-Whitney test).
DISCUSSION
Y. pestis is a facultative intracellular bacterium. It is generally acknowledged that the most effective vaccines against intracellular bacteria are live attenuated mutants (12, 42). Live attenuated plague vaccines have been used effectively in humans, and the live Pgm-negative EV76 plague vaccine is licensed for use in several former states of the Soviet Union (9, 14, 50). However, passage of EV76 has resulted in a number of genetically distinct substrains (49). Moreover, EV76 evokes significant inflammatory responses in humans and retains virulence in mice and some primates, where it persists, disseminates, and can even cause mortality (45). The licensure of live vaccines in the United States presents substantial hurdles, including the identification of well-characterized, stable mutants sufficiently attenuated for human use yet still capable of priming protective immune responses (12). The U.S. Army investigated the vaccine potential of a well-characterized Pgm-negative mutant but found that it retained significant virulence in primates (45). Removing other genes, such as pla, pcm, yopH, lpxM, or lpp, also can attenuate Y. pestis strains while maintaining their capacity to prime protective responses (4, 9, 11, 37, 45), but previously it has not been demonstrated that these more highly attenuated Y. pestis strains retain the capacity to prime protective cellular responses. Here we have presented the first evidence that a highly attenuated Y. pestis strain can retain the capacity to prime protective cell-mediated immunity.
Despite its attenuation and immunogenicity, strain D27-pLpxL is not likely to meet the standards for vaccine licensure, at least not in its current form. Minimally, one would like to prevent reversion to virulence by ensuring stable maintenance of the LpxL-expressing plasmid, as might be accomplished using balanced-lethal platforms (40). It also may be necessary to further attenuate D27-pLpxL, since, despite its avirulence in mice, our data clearly show that this strain persists in vivo for several days and even disseminates to visceral tissue. Presently, we are investigating whether dendritic cells participate in the persistence and dissemination of Y. pestis in vivo, since we know that D27-pLpxL potently activates dendritic cells and promotes their migration in vitro in a TLR4-dependent manner (35). Notably, Airhart et al. recently described TLR4-activating lipid A mimetics that act as potent adjuvants for the F1/LcrV-based subunit plague vaccine (1). Future studies will need to determine whether increased TLR4 activation alone accounts for the robust immunity primed by D27-LpxL or whether transient persistence and/or dissemination also is a necessary criterion for the induction of protective cellular immunity by live attenuated Y. pestis vaccine strains. It also will be interesting to investigate the impact of the immunization route (e.g., intranasal, subcutaneous, or intramuscular) on vaccine efficacy.
Independent of its potential use as a vaccine, D27-pLpxL already is a valuable research tool for dissecting mechanisms underlying the nature of protective cellular immunity against plague and for defining correlates of protective cellular immunity. This report provides the first detailed characterization of T-cell responses during pulmonary Y. pestis infection. Our analysis revealed that pulmonary Y. pestis infection is accompanied by a significant depletion of both CD4 and CD8 T cells from the lungs of mice. Immunization with D27-pLpxL prevents this depletion and, moreover, primes for robust accumulation of activated (CD44high CD43high) T cells possessing the capacity to rapidly produce the cytokines IFN-γ and TNF-α. These quantitative analyses of pulmonary T cells provide new correlates of protection for pneumonic plague that should be applicable to other vaccination and therapeutic approaches under development. Specifically, this report describes robust flow cytometric assays that can measure the extent to which plague countermeasures facilitate the accumulation of pulmonary T cells with effector phenotypes. A future challenge is to identify parameters that can be measured prior to challenge that accurately predict vaccine efficacy. We anticipate that the identification of specific antigens recognized by protective Y. pestis-specific T cells will enable the development of sensitive enzyme-linked immunospot or major histocompatibility complex multimer assays that, in turn, may serve as surrogate assays for vaccine efficacy.
We do not propose that T cells alone are likely to suffice in protecting humans from pneumonic plague or that measures of T cells alone will suffice as surrogate assays for protective efficacy in humans. While we demonstrated that T cells can protect significantly against 200 MLDs of intranasally administered Y. pestis strain D27 (Fig. 2C and D), we continue to believe that vaccines that prime both T cells and antibodies will provide optimal protection. The Pgm-deficient D27 strain used for the challenge studies presented here is virulent when administered intranasally, but, in contrast to wild-type Pgm-positive Y. pestis, this strain is highly attenuated when administered subcutaneously. In extensions of our prior work, we observed that cellular immunity primed by immunization with strain D27 in tandem with serotherapy (28) significantly delays the time to morbidity in μMT mice infected with Pgm-positive Y. pestis strain CO92 (unpublished data). However, the immunized animals nevertheless succumbed to infection, suggesting that cellular immunity may not suffice to protect antibody-deficient mice against fully virulent Y. pestis. Accordingly, we anticipate that cellular immunity and humoral immunity collaborate to provide the optimal defense against pneumonic plague. Studies now under way aim to decisively establish that Y. pestis-specific T cells can augment defense provided by suboptimal antibody titers.
Another interesting correlate of protection observed in this study was the formation of granuloma-like structures in the livers of mice challenged with virulent Y. pestis. Nakajima et al. previously described the formation of similar structures in mice treated with protective LcrV-specific antibodies prior to intravenous infection with Y. pestis (27). Likewise, we observed phenotypically similar structures in the livers of mice infected intranasally with Y. pestis and then treated with protective MAb specific for LcrV (unpublished). We find it striking that the histological hallmarks of protection mediated solely by cellular immunity (Fig. 3) are so reminiscent of those described previously for antibody-mediated protection. Interestingly, similar structures also are characteristic of hepatic immune responses in mice clearing avirulent Y. pestis mutants (27, 41), including mice infected with LpxL-expressing Y. pestis (26). Altogether, these data suggest that a common mechanism may account for much of the clearance of Y. pestis from visceral tissue. A better understanding of this mechanism could lead to novel therapeutic approaches.
In prior studies we demonstrated that immunizing mice with live Pgm-deficient strain D27 can prime memory T cells that protect against pneumonic challenge. However, our prior immunization protocols either resulted in the death of half the vaccinees (32) or required therapeutic administration of anti-Yersinia serum to prevent vaccine-induced mortality (28). Here we have described a robust model for safely priming protective T cells in an antibody-independent system. The protection conferred by immunization with strain D27-pLpxL does not require antibody production and is associated with robust priming of cytokine-producing T cells that suppress the cytopathic effects that typically characterize visceral Y. pestis infections. These findings support the feasibility of developing safe, highly attenuated, live Y. pestis vaccines that protect humans against pneumonic plague, at least in part, by priming memory T-cell responses.
Acknowledgments
This research was supported by funding from the Trudeau Institute and PHS grants R01-AI061577 (to S. T. Smiley), U54-AI057158 (to W. I. Lipkin), and R01-AI057588 and R01-AI075318 (to E. Lien).
We thank Debbie Duso for technical assistance and the employees of the Trudeau Institute animal facilities for dedicated care and breeding of the mice used in these studies. We also thank Robert Brubaker for generously providing access to the D27 Y. pestis strain.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 20 July 2009.
REFERENCES
- 1.Airhart, C. L., H. N. Rohde, C. J. Hovde, G. A. Bohach, C. F. Deobald, S. S. Lee, and S. A. Minnich. 2008. Lipid A mimetics are potent adjuvants for an intranasal pneumonic plague vaccine. Vaccine 26:5554-5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson, G. W., Jr., P. L. Worsham, C. R. Bolt, G. P. Andrews, S. L. Welkos, A. M. Friedlander, and J. P. Burans. 1997. Protection of mice from fatal bubonic and pneumonic plague by passive immunization with monoclonal antibodies against the F1 protein of Yersinia pestis. Am. J. Trop. Med. Hyg. 56:471-473. [DOI] [PubMed] [Google Scholar]
- 3.Bashaw, J., S. Norris, S. Weeks, S. Trevino, J. J. Adamovicz, and S. Welkos. 2007. Development of in vitro correlate assays of immunity to infection with Yersinia pestis. Clin. Vaccine Immunol. 14:605-616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bubeck, S. S., and P. H. Dube. 2007. Yersinia pestis CO92 delta yopH is a potent live, attenuated plague vaccine. Clin. Vaccine Immunol. 14:1235-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butler, T. 1983. Plague and other yersinia infections. Plenum Press, New York, NY.
- 6.Chattopadhyay, A., S. Park, G. Delmas, R. Suresh, S. Senina, D. S. Perlin, and J. K. Rose. 2008. Single-dose, virus-vectored vaccine protection against Yersinia pestis challenge: CD4+ cells are required at the time of challenge for optimal protection. Vaccine 26:6329-6337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dennis, D. T., K. L. Gage, N. Gratz, J. D. Poland, and E. Tikhomirov. 1999. Plague manual: epidemiology, distribution, surveillance and control. WHO/CDS/CSR/EDC/99.2. World Health Organization, Geneva, Switzerland.
- 8.Elvin, S. J., and E. D. Williamson. 2004. Stat 4 but not Stat 6 mediated immune mechanisms are essential in protection against plague. Microb. Pathog. 37:177-184. [DOI] [PubMed] [Google Scholar]
- 9.Feodorova, V. A., L. N. Pan'kina, E. P. Savostina, L. V. Sayapina, V. L. Motin, S. V. Dentovskaya, R. Z. Shaikhutdinova, S. A. Ivanov, B. Lindner, A. N. Kondakova, O. V. Bystrova, N. A. Kocharova, S. N. Senchenkova, O. Holst, G. B. Pier, Y. A. Knirel, and A. P. Anisimov. 2007. A Yersinia pestis lpxM-mutant live vaccine induces enhanced immunity against bubonic plague in mice and guinea pigs. Vaccine 25:7620-7628. [DOI] [PubMed] [Google Scholar]
- 10.Fetherston, J. D., P. Schuetze, and R. D. Perry. 1992. Loss of the pigmentation phenotype in Yersinia pestis is due to the spontaneous deletion of 102 kb of chromosomal DNA which is flanked by a repetitive element. Mol. Microbiol. 6:2693-2704. [DOI] [PubMed] [Google Scholar]
- 11.Flashner, Y., E. Mamroud, A. Tidhar, R. Ber, M. Aftalion, D. Gur, S. Lazar, A. Zvi, T. Bino, N. Ariel, B. Velan, A. Shafferman, and S. Cohen. 2004. Generation of Yersinia pestis attenuated strains by signature-tagged mutagenesis in search of novel vaccine candidates. Infect. Immun. 72:908-915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frey, J. 2007. Biological safety concepts of genetically modified live bacterial vaccines. Vaccine 25:5598-5605. [DOI] [PubMed] [Google Scholar]
- 13.Galimand, M., A. Guiyoule, G. Gerbaud, B. Rasoamanana, S. Chanteau, E. Carniel, and P. Courvalin. 1997. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N. Engl. J. Med. 337:677-680. [DOI] [PubMed] [Google Scholar]
- 14.Girard, G. 1963. Immunity in plague. Results of 30 years of work on the “Pasteurella pestis Ev” (Girard and Robic) strain. Biol. Med. (Paris) 52:631-731. [PubMed] [Google Scholar]
- 15.Green, M., D. Rogers, P. Russell, A. J. Stagg, D. L. Bell, S. M. Eley, R. W. Titball, and E. D. Williamson. 1999. The SCID/beige mouse as a model to investigate protection against Yersinia pestis. FEMS Immunol. Med. Microbiol. 23:107-113. [DOI] [PubMed] [Google Scholar]
- 16.Hill, J., J. E. Eyles, S. J. Elvin, G. D. Healey, R. A. Lukaszewski, and R. W. Titball. 2006. Administration of antibody to the lung protects mice against pneumonic plague. Infect. Immun. 74:3068-3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hogan, R. J., E. J. Usherwood, W. Zhong, A. A. Roberts, R. W. Dutton, A. G. Harmsen, and D. L. Woodland. 2001. Activated antigen-specific CD8+ T cells persist in the lungs following recovery from respiratory virus infections. J. Immunol. 166:1813-1822. [DOI] [PubMed] [Google Scholar]
- 18.Hogan, R. J., W. Zhong, E. J. Usherwood, T. Cookenham, A. D. Roberts, and D. L. Woodland. 2001. Protection from respiratory virus infections can be mediated by antigen-specific CD4(+) T cells that persist in the lungs. J. Exp. Med. 193:981-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inglesby, T. V., D. T. Dennis, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, J. F. Koerner, M. Layton, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, M. Schoch-Spana, K. Tonat, et al. 2000. Plague as a biological weapon: medical and public health management. JAMA 283:2281-2290. [DOI] [PubMed] [Google Scholar]
- 20.Kool, J. L. 2005. Risk of person-to-person transmission of pneumonic plague. Clin. Infect. Dis. 40:1166-1172. [DOI] [PubMed] [Google Scholar]
- 21.Kummer, L. W., F. M. Szaba, M. A. Parent, J. J. Adamovicz, J. Hill, L. L. Johnson, and S. T. Smiley. 2008. Antibodies and cytokines independently protect against pneumonic plague. Vaccine 26:6901-6907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lahteenmaki, K., R. Virkola, A. Saren, L. Emody, and T. K. Korhonen. 1998. Expression of plasminogen activator Pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect. Immun. 66:5755-5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lien-Teh, W. 1926. A treatise on pneumonic plague. Leaugue of Nations Health Organisation, Geneva, Switzerland.
- 24.Meyer, K. F. 1970. Effectiveness of live or killed plague vaccines in man. Bull. W. H. O. 42:653-666. [PMC free article] [PubMed] [Google Scholar]
- 25.Meyer, K. F., G. Smith, L. Foster, M. Brookman, and M. Sung. 1974. Live, attenuated Yersinia pestis vaccine: virulent in nonhuman primates, harmless to guinea pigs. J. Infect. Dis. 129(Suppl.):S85-S112. [DOI] [PubMed] [Google Scholar]
- 26.Montminy, S. W., N. Khan, S. McGrath, M. J. Walkowicz, F. Sharp, J. E. Conlon, K. Fukase, S. Kusumoto, C. Sweet, K. Miyake, S. Akira, R. J. Cotter, J. D. Goguen, and E. Lien. 2006. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat. Immunol. 7:1066-1073. [DOI] [PubMed] [Google Scholar]
- 27.Nakajima, R., V. L. Motin, and R. R. Brubaker. 1995. Suppression of cytokines in mice by protein A-V antigen fusion peptide and restoration of synthesis by active immunization. Infect. Immun. 63:3021-3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parent, M. A., K. N. Berggren, L. W. Kummer, L. B. Wilhelm, F. M. Szaba, I. K. Mullarky, and S. T. Smiley. 2005. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect. Immun. 73:7304-7310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parent, M. A., K. N. Berggren, I. K. Mullarky, F. M. Szaba, L. W. Kummer, J. J. Adamovicz, and S. T. Smiley. 2005. Yersinia pestis V protein epitopes recognized by CD4 T cells. Infect. Immun. 73:2197-2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parent, M. A., L. B. Wilhelm, L. W. Kummer, F. M. Szaba, I. K. Mullarky, and S. T. Smiley. 2006. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect. Immun. 74:3381-3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Philipovskiy, A. V., and S. T. Smiley. 2007. Vaccination with live Yersinia pestis primes CD4 and CD8 T cells that synergistically protect against lethal pulmonary Y. pestis infection. Infect. Immun. 75:878-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pollitzer, R. 1954. Plague. Monogr. Ser. W. H. O. 22:1-698. [Google Scholar]
- 34.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 35.Robinson, R. T., S. A. Khader, R. M. Locksley, E. Lien, S. T. Smiley, and A. M. Cooper. 2008. Yersinia pestis evades TLR4-dependent induction of IL12(p40)2 by dendritic cells and subsequent cell migration. J. Immunol. 181:5560-5567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Russell, P., S. M. Eley, S. E. Hibbs, R. J. Manchee, A. J. Stagg, and R. W. Titball. 1995. A comparison of Plague vaccine, USP and EV76 vaccine induced protection against Yersinia pestis in a murine model. Vaccine 13:1551-1556. [DOI] [PubMed] [Google Scholar]
- 37.Sha, J., S. L. Agar, W. B. Baze, J. P. Olano, A. A. Fadl, T. E. Erova, S. Wang, S. M. Foltz, G. Suarez, V. L. Motin, S. Chauhan, G. R. Klimpel, J. W. Peterson, and A. K. Chopra. 2008. Braun lipoprotein (Lpp) contributes to virulence of yersiniae: potential role of Lpp in inducing bubonic and pneumonic plague. Infect. Immun. 76:1390-1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smiley, S. T. 2008. Current challenges in the development of vaccines for pneumonic plague. Expert Rev. Vaccines 7:209-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smiley, S. T. 2008. Immune defense against pneumonic plague. Immunol. Rev. 225:256-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spreng, S., and J. F. Viret. 2005. Plasmid maintenance systems suitable for GMO-based bacterial vaccines. Vaccine 23:2060-2065. [DOI] [PubMed] [Google Scholar]
- 41.Straley, S. C., and M. L. Cibull. 1989. Differential clearance and host-pathogen interactions of YopE− and YopK− YopL− Yersinia pestis in BALB/c mice. Infect. Immun. 57:1200-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Titball, R. W. 2008. Vaccines against intracellular bacterial pathogens. Drug Discov. Today 13:596-600. [DOI] [PubMed] [Google Scholar]
- 43.Titball, R. W., and E. D. Williamson. 2004. Yersinia pestis (plague) vaccines. Expert Opin. Biol. Ther. 4:965-973. [DOI] [PubMed] [Google Scholar]
- 44.Une, T., and R. R. Brubaker. 1984. In vivo comparison of avirulent Vwa− and Pgm− or Pstr phenotypes of yersiniae. Infect. Immun. 43:895-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Welkos, S., M. L. Pitt, M. Martinez, A. Friedlander, P. Vogel, and R. Tammariello. 2002. Determination of the virulence of the pigmentation-deficient and pigmentation-/plasminogen activator-deficient strains of Yersinia pestis in non-human primate and mouse models of pneumonic plague. Vaccine 20:2206-2214. [DOI] [PubMed] [Google Scholar]
- 46.Williamson, E. D., H. C. Flick-Smith, C. Lebutt, C. A. Rowland, S. M. Jones, E. L. Waters, R. J. Gwyther, J. Miller, P. J. Packer, and M. Irving. 2005. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect. Immun. 73:3598-3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization. 2005. Plague, Democratic Republic of The Congo. Wkly. Epidemiol. Rec. 80:65. [PubMed] [Google Scholar]
- 48.Yersin, A. 1894. La peste bubonique a Hong Kong. Ann. Inst. Pasteur (Paris) 8:662-667. [Google Scholar]
- 49.Zhou, D., Y. Han, E. Dai, Y. Song, D. Pei, J. Zhai, Z. Du, J. Wang, Z. Guo, and R. Yang. 2004. Defining the genome content of live plague vaccines by use of whole-genome DNA microarray. Vaccine 22:3367-3374. [DOI] [PubMed] [Google Scholar]
- 50.Zilinskas, R. A. 2006. The anti-plague system and the Soviet biological warfare program. Crit. Rev. Microbiol. 32:47-64. [DOI] [PubMed] [Google Scholar]