Abstract
Introduction and background
Based on a policy initiative and the foundation of the Competence Centre for Integrated Care by the Austrian Social Security Institutions in 2006, the aim of the project was to identify and prioritise potential diseases and target groups for which integrated care models should be developed and implemented within the Austrian health system. The project was conducted as a cooperation between the Competence Centre for Integrated Care of the Viennese Health Insurance Fund and the Institute of Social Medicine of the Medical University Vienna to ensure the involvement of both, theory and practice.
Project report
The focus of the project was to develop an evidence-based process for the identification and prioritisation of diseases and target groups for integrated care measures. As there was no evidence of similar projects elsewhere, the team set out to design the prioritisation process and formulate the selection criteria based on the work in a focus group, literature reviews and a scientific council of national and international experts. The method and criteria were evaluated by an expert workshop.
Discussion
The active involvement of all stakeholders from the beginning was crucial for the success. The time constraint proved also beneficial since it allowed the project team to demand focus and cooperation from all experts and stakeholders included.
Conclusion
Our experience demonstrates that, with a clear concept and model, an evidence-based prioritisation including all stakeholders can be achieved. Ultimately however, the prioritisation is a political discussion and decision. Our model can only help base these decisions on sound and reasonable assumptions.
Keywords: integrated care priorities, national priority setting, project management, process design, decision making
Introduction
This article is based on a policy initiative creating a national Competence Centre for Integrated Care (CCIV) as a service centre for the Austrian Health Insurance Funds and Social Security Institutions in 2006. In order to establish a national strategy for integrated care, the question within the health insurance funds arose which priorities and diseases should be considered as relevant and urgent in the Austrian context. In a collaboration of the Competence Centre for Integrated Care with the Institute of Social Medicine at the Centre for Public Health of the Medical University Vienna a project was designed to identify and evaluate integrated care priorities on a national level. The invitation for the Institute of Social Medicine to act as the scientific partner was to ensure a research-guided and quality-assured procedure and outcome. Together, the two project partners designed the process and defined the framework.
The authors represent the project management and coordination team. The project was realised between July and December 2007.
Background and problem statement
In its business plan the Competence Centre for Integrated Care (CCIV) had the set target to identify and prioritise diseases, which show a potential to be managed by an integrated care model within the context of the Austrian health care system.
So far there has not been any comparable effort to systematically identify and evaluate integrated care priorities on a national level, which made it necessary to develop an adequate methodology for the project. So, from the start one of the targets was to create a model, which would be transferable to other settings and countries, and at the same time regard the specific context of the Austrian health system.
The Austrian context
Austria features an array of institutions and funds concerning themselves with the health system, but the country has not yet developed national health targets, which could have been used as a global guidance. Nevertheless, most federal states have already developed their own health targets. The last major health care reform was introduced in 2004, creating a federal institute for health (Gesundheit Österreich GmbH, Health Austria Limited) and creating a national health plan among other things. Unfortunately, many structural and financial issues have not yet been resolved and are still on the agenda for an upcoming reform.
The Austrian health care system follows the Bismarckian principles of universal coverage and insurance-based delivery of services. Around 98% of Austrians are covered by one of the 19 public health insurers (organised by profession and region) and about 1/3 of the population have additional private insurance [1, 2]. Obstacles include the dysfunctional barriers arising from different insurance agencies covering basic health services, rehabilitation, accidents and retirement. The primary sources of health care funding are the compulsory health insurance (45%) and federal government subsidies (25%). While this system secures catholic health services provision, the Austrian system has also been declared as excessively fragmented, with a tendency to over-supply and dis-supply of services. Still, it is one of the best performing systems in the world concerning health outcomes and access to services [1, 3].
In this setting, the aim of the Competence Centre for Integrated Care is to concentrate national and international knowledge and experience on the topic of integrated care by creating a comprehensive database and building a team of experts who will develop integrated care models for Austria, assist in project management and design and distribute information. Its services are provided to all social security institutions and health insurance funds in Austria. However, as the Competence Centre is in its first right a service centre for the health insurance institutions, it sees integrated care as a means to better manage and coordinate the insured, identify high risk target groups (e.g. migrant women, multi-morbid persons, etc.) and design care models accordingly, within the scope of the legally binding tasks for Austrian health insurance funds. Even though neither the intra-mural sector nor the social services are in its direct field of influence, the models to be designed by the Competence Centre will define the relevant interfaces and describe necessary services regardless of sector or provider. In order to ensure the development of adequate integrated care models focusing on the needs of the intended target group, co-operations with other relevant service providers and players will be sought accordingly. The definitions guiding the understanding of integrated care in Austria are those of Gröne/Barbero (2004) [4], Kodner/Spreeuwenberg (2002) [5] and Weatherly et al. (2007) [6].
The process development
In order to be able to fulfil these tasks and get a better understanding of what is possible and required within the Austrian setting, the project “Prioritisation of Indication-based Integrated Care in Austria” was initiated. The first phase was to
research and analyse international experience and evidence.
identify and prioritise diseases for which indication-based IC could be applicable in Austria.
create a list of indicators for the design of integrated care models.
generate a White Paper with recommendations which diseases should be targeted preferentially.
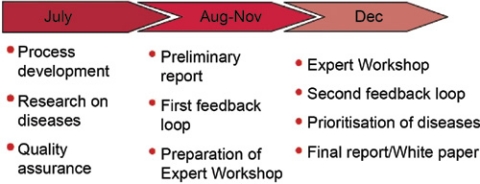
Due to the deadlines laid down in the business plan of the Competence Centre for Integrated Care, the timeline was quite strict (see Figure 1). While it did pose additional challenges for the project team, it turned out to be a beneficial restriction in the end.
Figure 1.
The timeline from July to December 2007.
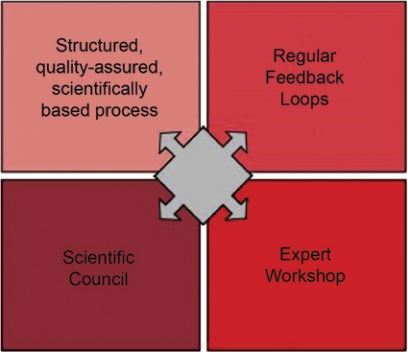
The four core elements (see Figure 2) were defined by the team as quintessential for the project. The base line of the project was a structured, quality-assured process, which included regular feedback loops by way of expert questionnaires and incorporation of the comments made by the scientific council. Ultimately, the expert workshop was expected to provide a final validation and evaluation of the methodology and the necessary input for the priority setting. This process was developed following the good practices of project management and elements of different change management methods, such as the Search Conference, Future Search and the Participative Design Workshop [7, 8].
Figure 2.
The core elements of the project.
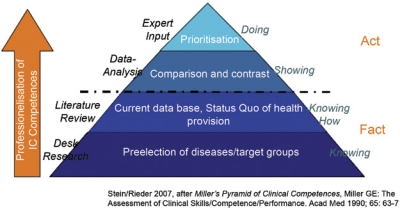
The process design: The Pyramid of Integrated Care Competences
Based on Miller’s (1990) ‘Pyramid of Clinical Competences’ [9] a ‘Pyramid of Integrated Care Competences’ (see Figure 3) was developed to guide the process. Along with the core elements, which were identified as key components of the project, the pyramid was used as the framework for further research. Each level represents a specific stage in the process, enhancing the knowledge and comprehension of the current situation, influences and demands, which ought to be considered during the analysis. It is a continuous and flexible model incorporating the basic principles of project management [8, 10].
Figure 3.
The Pyramid of Integrated Care.
The pyramid of integrated care illustrates the step-by-step approach to building knowledge and competences on relevant aspects of the health and social system. This process enables one to base decisions of integrated care activities on as much evidence as available. Furthermore, it facilitates the pre-, peri- and post-evaluation process by defining clear indicators and criteria.
Pre-selection of diseases
As illustrated by the base level of the pyramid, it is principally necessary to formulate the goals of the integrated care strategy and pre-select adequate diseases and/or target groups. For the purpose of basing this pre-selection process on comprehensible and justifiable criteria, the project team defined and analysed relevant parameters, which impact and determine integrated care and the prioritisation of diseases in a European health system and identified the following key institutions and factors:
EU (Focal Points of the 7th Framework Programme)
WHO (Health 21)
International Journal for Integrated Care
Most common integrated care contracts in Germany
Austrian Association of Family Doctors
Topics of the Austrian Integrated Care Conferences
National hospital release statistics
Medicinal costs of the Austrian social security
Self help groups
These nine institutions build the international and national, political, societal and social security-related framework which influences the relative importance of diseases within the Austrian health system. The inclusion of the foci of international organisations, scientific journals, national statistics and experiences constitutes a broad scientific, societal and economic base on which the pre-selection of diseases could be predicated upon. For example, alcohol abuse and depression were identified by the Austrian Association of Family Doctors as the most important, under-estimated and disregarded conditions for which no adequate services or enough attention existed, leaving many primary care doctors with limited possibilities. On the other hand, cataract was identified as the one condition with the highest relative medical costs per insured for social security since it was still mostly done in hospitals with an overnight stay. So, disregarding other aspects lists of the top ten priorities of each institution and database were compiled, compared and synthesised into a first selection of relevant conditions to be systematically analysed (see Table 1).
Table 1.
The 14 pre-selected diseases
| Alcohol abuse | Hemiated disc |
| Arthroses | Hypertension |
| Breast cancer | Intestinal cancer |
| Cataract | Lung cancer |
| Dementia | Obesity |
| Depression | Osteoporosis |
| Heart failure | Prostate cancer |
As an additional discriminator, those diseases were not taken into consideration for which Disease Management Programmes or similar initiatives already existed or were in planning in Austria. This holds true for Diabetes I and II, stroke and post-Myocardial infarction, allergies and Asthma/COPD. A further constraint was the fact that the selection process was based on the scope of health insurance activities.
Having taken the foci of the institutions and Austrian developments into account, a list of 14 diseases was compiled (see Table 1).
Taking the restrictions mentioned above into consideration, this list of diseases did not yield big surprises. It has to be highlighted that the focus was to ensure a verifiable and transparent selection process, even at this early stage rather than following perceived and observed trends.
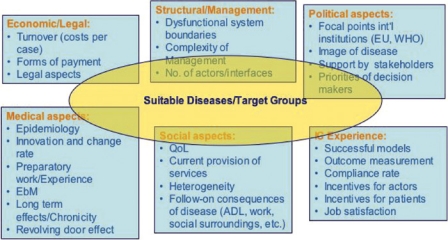
For the detailed analysis of these 14 diseases a catalogue of criteria was developed and summarised in six dimensions. These were used to further structure the research and identify common goals and indicators along which the literature review was conducted.
Identifying the criteria
Integrated Care is influenced by various societal, political, medical and economic interests all of which should be considered when designing new concepts and models of service delivery. Our research did not provide us with evidence of other countries using systematically identified criteria on which to base resource allocation decisions concerning integrated care. Nor did we find validated frameworks on how to determine relevant integrated care initiatives. And even if selection criteria were published, they often proved very project- or country-specific. In the meantime, the very informative and comprehensive literature review by MacAdam (2008) [11] on frameworks for integrated care has provided a basis from which to start.
The Austrian project team hence set out to develop a framework of criteria, which could be used on a more general level. The six dimensions in which criteria were to be defined are the following:
-
Political criteria:
The political environment forms the framework for the health system and hence integrated care. Thus, it is of utmost importance to consider health targets, targeted programmes, national interests and the image of a disease or groups concerned for the analysis.
-
Economic/legal criteria:
It is not the primary aim of integrated care to achieve cost reduction but to enable a cost-efficient and cost-effective resource allocation. Here, aspects such as the costs per case or medicinal costs are included as well as legal requirements. Often disregarded but of utmost importance is the consideration of ethical issues, as for example the topic of an advance directive or the restriction of services.
-
Structural/management criteria:
This dimension analyses the existing structures, identifies interfaces and highlights dysfunctional barriers in the system (e.g. concerning financing structures). It is a tool to describe the complexity of the service delivery and management as well as the most important actors and stakeholders.
-
Medical criteria:
In this cluster, medical and epidemiological indicators are summarised to analyse the burden of disease, the descriptors for the patient groups and which trends in treatment and service delivery can be expected for the future. This would also include an estimation of long-term effects and re-hospitalisation rates.
-
Social criteria:
An imminent aspect of (chronic) disease, frailty or disability is the effect on quality of life. Whether it is the diminished activity level of the patient and the caregiver(s) or the possible stigmatisation caused by the diagnosis—these issues have to be addressed within new service delivery concepts and therefore have to be surveyed. Additional relevant criteria include effects such as inability to work, isolation or need for assistance, as well as social background, gender and age.
-
Integrated care experience:
Finally, the experiences already made in the field, nationally and internationally, should be taken into account. Also, the question of compliance of actors and the incentives for them to participate in an integrated care model are included in this aspect.
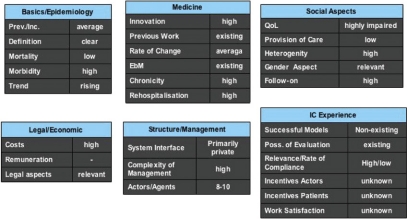
Figure 4 depicts the criteria in more detail. It should be noted that the sequence does not entail any valuation or weighting.
Figure 4.
Integrated care criteria and dimensions.
These criteria formed the basis for a detailed literature review of the 14 diseases, which were then compiled in a White paper [12]. The literature review and data collection was conducted using PubMed, UpToDate, the internal database of the Austrian health insurers, OECD and WHO databases and the publications of Statistics Austria [1–3, 13]. Furthermore, where a lack of data and evidence base was discovered, grey literature and expert interviews were used to complete the picture.
Expert workshop and prioritisation process
As the final and decisive step in the project, the scientific board and additional experts were invited to a workshop in order to discuss the process, evaluate the outcomes and conduct a prioritisation of the diseases. As a base for their discussions, they were provided with a summary of the research results and the process development. In addition to providing the project team with a feedback on the methodology used and the concepts developed, the national and international experts were asked to prioritise the 14 diseases according to their expertise and from the perspective of a national social security agency.
The experts represented all stakeholders including
the Ministry of Health
General Practitioners and specialised doctors
the Patients Advocate
health economists and other academic areas
Public Health experts
the Viennese Health Insurance Fund
international experts from Germany, the Netherlands and Switzerland to provide an outside perspective
The discussion took place in December 2007 during the expert workshop in Vienna which was prepared and facilitated by the project team.
Reviewing the process
The experts unanimously considered the process a milestone for integrated care projects, since such a systematic and structured identification of priorities has so far not been attempted elsewhere. The criteria were evaluated as comprehensive and valid. However, the lack of national health targets [14] was seen as a political obstacle for the further progress of the project. Also, the paramount role of the quality aspect was underlined several times and identified as a primal goal of integrated care.
The cornerstones of the workshop
In order to explain the framework in which the project had been operating and which would hence influence the further discussions, it was emphasised that the results of the workshop and the prioritisation process would be summarised in a catalogue of recommendations for Austrian decision makers in social security and politics. At the time of the workshop, there was no fixed timeframe but the results of the prioritisation process were considered to be medium- to long-term.
Then the experts were presented with the six dimensions of criteria (see Figure 4) and the results of the data analysis [9]. An example of how the information was prepared is depicted in Figure 5.
Figure 5.
Results of the data analysis illustrated by the example of Dementia.
The detailed paper had been sent to the experts prior to the workshop to enable them to prepare for the discussions.
Valuing the criteria
It quickly became apparent to the experts that a prioritisation could only be undertaken by a valuation of the goals and criteria in order to make the discussion and process more manageable. This necessitated the identification of those parameters and criteria, which were considered most important. Here, for the first time, the specific actor’s perspective was taken into account in order to adapt the general criteria catalogue to its goals. Moreover, a first weighting was performed during the discussion, which culminated in the identification of four top priority goals, derived from the criteria catalogue:
-
Incidence/effect:
This aim pictures the public health component of the disease, representing how many people are affected, the future prognosis for the prevalence and what effects arise for public health.
-
Should be/As is-ratio:
Another important indicator for the usefulness and necessity of an integrated care approach is seen in the delta of the status quo service delivery and the ideal situation.
-
Long-term perspective:
This aim is divided into two components: first, it encompasses the effects of the disease, especially chronicity and co-morbidities. Secondly, it illustrates expected medical and social developments, which could make the disease a priority issue in the future. Hence, this aim is closely linked to the first one.
-
Complexity/feasibility:
The fourth aspect describes the complexity of management of the disease/target group. This entails interface organisation, the number of actors and stakeholders involved and the willingness to change. It also provides decision makers with an estimation of the feasibility of the model according to current information and knowledge base.
All the other criteria and aims are not less valuable or important, but according to the expert workshop can be considered as sub-goals of these primary goals or may be used as sources for additional information whenever needed in the decision making process. As further indicator, the top priority goal of the social security agency is the optimal service provision to its clients. This is expected to be achieved through integrated care, especially when dealing with chronic diseases.
Additional recommendations by the expert workshop
Experiences made in other countries have demonstrated that clear and realistic health targets are a prerequisite for a successful implementation of integrated care. Furthermore, the experts recommended to start with diseases, which are complex in steering and management but which nevertheless feature a sound database and clear specifications. The degree of complexity must be definable in order to be able to achieve positive outcomes, which in their turn will provide evidence and arguments for additional support.
Results of the prioritisation process
Following the four criteria, which were identified during the earlier discussion, an evaluation and weighting of the 14 diseases was conducted, again through a discussion process, which aimed at a unanimous consensus of all experts. After a short discussion, an agreement was reached as to take a pragmatic approach and use three straightforward levels of weighting:
↑=high/strong
↔=average
↓=low/weak
Based on the results of the discussion, Table 2 depicts the prioritisation according to the experts.
Table 2.
Results of the prioritisation process
| Incidence/effect | Should be/as is ratio | Long-term perspective | Complexity/feasibility | |
| Alcohol abuse | ↑ | ↓ | ↑ | ↓ |
| Arthroses | ↑ | ↓ | ↑ | ↓ |
| Breast cancer | ↔ | ↔ | ↑ | ↑ |
| Cataract | ↑ | ↓ | ↓ | ↔ |
| Dementia | ↑ | ↑ | ↑ | ↑ |
| Depression | ↔ | ↑ | ↑ | ↔ |
| Heart failure | ↑ | ↔ | ↑ | ↑ |
| Herniated disc | ↓ | ↔ | ↑ | ↓ |
| Hypertension | ↑ | ↑ | ↑ | ↓ |
| Intestinal cancer | ↔ | ↔ | ↑ | ↑ |
| Lung cancer | ↓ | ↔ | ↑ | ↔ |
| Obesity | ↑ | ↔ | ↑ | ↓ |
| Osteoporosis | ↑ | ↑ | ↑ | ↑ |
| Prostate cancer | ↔ | ↔ | ↑ | ↔ |
The ultimate step was to summarise these weightings into levels of prioritisation (see Table 3). These three levels represent the recommendation of the expert workshop and the scientific council for the decision makers as to where to start with integrated care measures in Austria. The highest level of prioritisation is represented by Level 1:
Table 3.
Levels of prioritisation
| Level 1 | Dementia, Osteoporosis; Heart failure, Hypertension* |
| Level 2 | Breast/Colon cancer |
| Level 3 | Depression |
*Mid-term action, to be integrated into the Disease Management Programme Post-Myocardial Infarction (DMP Post-MI, also in development as of 2008).
Regarding cancer care, it is explicitly mentioned that Austria needs to shift more resources and focus to the issue of palliative/end of life care and develop a national concept for all cancer patients. The remaining seven diseases which are not listed in the prioritisation can be considered as Level 4 and were not identified as high priority in the Austrian context. Since the business plan of the Competence Centre for Integrated Care suggests to develop one integrated care model per year, they will be of guidance for future developments.
Discussion
Even though the time constraint was an issue, the project fulfilled its targets and was therefore evaluated as a success: by the end of the project a White paper compiling status quo on 14 conditions had been written [12], together with an evidence-based and reproducible process. Throughout the process it was ensured that all stakeholders were involved. The White paper was the basis for the decision makers and the bodies within the Social Security to define the strategy concerning integrated care for the Austrian Social Security setting. They followed the recommendations of the experts and selected dementia as the first disease target group for which to develop an integrated care model.
The process also demonstrated the importance of allocating sufficient time to discussions and to seek a consensus right from the beginning—making it more difficult for representatives of a stakeholder or interest group to block decisions and actions later on in the process. In hindsight, the limited project time of only six months proved beneficial, since it not only created pressure but could also be used as an argument to ask for discipline and focus during the process. So what was considered a weakness in the beginning of the project was used to create positive effects. It also guaranteed commitment and determination by all parties involved to reach a common understanding and result. The biggest obstacles encountered during the project were inaccessibility or lack of data, little evidence on specific integrated care models and the incertitude due to the exploratory nature of the project. Here, one could argue that more time would have permitted the project team to carry out controlling, testing and feedback loops to ensure reliability of outcomes. In what ways that would have altered the results remains a question for future research.
Taken all this into account, our experience demonstrates that, with a clear concept and model, an evidence-based prioritisation including all stakeholders can be achieved.
A model for the future
Integrated Care is a model to face the challenges of today’s and tomorrow’s health care systems and can also be utilised to restructure health care provision on a national level. Still, many countries and actors within health systems consider integrated care to be the philosopher’s stone and thus, the solution to all resource allocation/limitation problems. With this mindset, it is only too easy to neglect the paramount principles of good project management, which include assigning enough time and consideration to the definition of aims and restrictions, as well as identifying the relevant stakeholders [8, 10].
We believe that we have designed a model, which can be used as a basis for other countries and institutions wanting to define and implement an integrated care strategy efficiently and effectively. Even though it has been used as a top-down approach in the Austrian context, it may be adapted to define the strategies and goals of a bottom-up approach as well since the main aim was to design a strategy and formulate measurable goals for future integrated care initiatives. With further elaboration, it may also assist in meeting one of the biggest challenges of integrated care: providing a framework with which to plan and evaluate integrated care. In any case, it should be seen as a basis for further discussion and research.
Notwithstanding the powers of scientific analysis, evaluation and recommendation it has however to be underlined, that ultimately, the prioritisation and target selection is a political discussion and decision. Our model can only help base these decisions on sound and reasonable assumptions.
The next phase of the project is the development and implementation of an integrated care model for dementia within the Austrian Social Security setting. Along with the model a national guideline for dementia will be developed by the Federal Institute for Quality in the Health System. It is underway and is scheduled to be completed by March 2010.
Contributor Information
Karin Eger, Head of the Competence Centre Integrated Care, Viennese Health Insurance Fund, Wienerbergstrasse 15–19, 1100 Vienna, Austria.
Sonja Gleichweit, Competence Centre Integrated Care, Viennese Health Insurance Fund, Wienerbergstrasse 15–19, 1100 Vienna, Austria.
Anita Rieder, Professor of Social Medicine, Institute of Social Medicine, Centre for Public Health, Medical University Vienna, Rooseveltplatz 3, 1090 Vienna, Austria.
K. Viktoria Stein, Institute of Social Medicine, Centre for Public Health, Medical University Vienna, Rooseveltplatz 3, 1090 Vienna, Austria.
Reviewers
Bengt Ahgren, MPolSc, PhD, Senior Lecturer, Nordic School of Public Health, Göteborg, Sweden
Peter Berchtold, PD Dr, Director of the College for Management in Healthcare (College-M), Bern, Switzerland
Nick Bosanquet, Professor of Health Policy, Department of Bioengineering, Imperial College, London, UK
References
- 1.Organisation for Economic Cooperation and Development. OECD health data 2008: Statistics and indicators for 30 countries. How does Austria compare. Paris: OECD; 2008. [cited Oct 30]. Available from: http://www.oecd.org/topicdocumentlist/0,3448,en_33873108_33873245_1_1_1_1_37407,00.html. [Google Scholar]
- 2.Statistik Austria. Gesundheitsausgaben in Österreich. [Health Expenditure in Austria]. Vienna: Statistiek Austria; 2008. [cited Oct 30]. Available from: http://www.statistik.at/web_de/statistiken/gesundheit/gesundheitsausgaben/index.html. [in German] [Google Scholar]
- 3.Hofmarcher MM, Rack H-M. Austria. Health system review. Available from the European Observatory on Health Systems and Policies website: http://www.euro.who.int/countryinformation/CtryInfoRes?COUNTRY=AUT. [Health Systems in Transition 2006 Vol 8, No. 3]. [also available in German]
- 4.Gröne O, Garcia-Barbero M. Integrated care: a position paper of the WHO European Office for Integrated Health Care Services. International Journal of Integrated Care [serial online] 2001 Jun 1;1 Available from: http://www.ijic.org/ [PMC free article] [PubMed] [Google Scholar]
- 5.Kodner D, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications—a discussion paper. International Journal for Integrated Care [serial online] 2002 Nov 14;2 doi: 10.5334/ijic.67. Available from: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weatherly J, Seiler R, Meyer-Lutterloh K, Schmid E, Lägel R, Amelung V. Leuchtturmprojekte Integrierter Versorgung und Medizinischer Versorgungszentren. [Flagship projects of integrated care and medical service centres]. Berlin: Schriftenreihe des Bundesverbandes Managed Care, Medizinisch Wissenschaftliche Verlagsgesellschaft; 2007. [in German] [Google Scholar]
- 7.Holman P, Devane T, Cady S, editors. The change handbook. The definitive resource on today’s best methods on engaging whole systems. 2nd edition. San Francisco: Berrett-Koehler Publishers; 2007. rev & exp. [Google Scholar]
- 8.Kerzner H. Project management—A systems approach to planning, scheduling and controlling. 9th edition updated. New York: John Wiley & Sons; 2006. [Google Scholar]
- 9.Miller GE. The assessment of clinical skills/competence/performance. Acadamic Medicine. 1990 Sep;65(9 Suppl):S63–7. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 10.Pinto JK. Project management. Upper Saddle River, NJ: Pearson Prentice Hall; 2007. [Google Scholar]
- 11.MacAdam M. Frameworks of integrated care for the elderly: a systematic review. Ontario: Canadian Policy Research Networks; 2008. [CPRN Research Report | April 2008] [Google Scholar]
- 12.Competence Center Integrierte Versorgung. Identifizierung und Priorisierung von Krankheitsbildern, die sich für integrierte Versorgung eignen. Endbericht—Prozessdokumentation, Rechercheergebnisse, Priorisierung. [Identification and prioritisation of diseases, which qualify for integrated care. Final report—Process documentation, research results, prioritisation]. Vienna: Viennese Health Insurance Fund; 2008. [in German, management summary available in English] [Google Scholar]
- 13.World Health Organization. Country Information Austria. [cited 2007 December 10, updated 2008 October 30]. Available from: http://www.who.int/countries/aut/en/
- 14.European Observatory on Health Systems and Policy. Targets for health. [webpage on the internet]. [cited 2008 October 30]. Available from: http://www.euro.who.int/observatory/Studies/20040310_2.