Abstract
Primary retroperitoneal mucinous cystadenomas (RMCs) are very rare and their biological behavior and histogenesis remain speculative. An accurate preoperative diagnosis of these tumors is difficult because no effective diagnostic measures have been established. We describe a 29-year-old woman with abdominal pain and a palpable mass. Computed tomography (CT) of the abdomen revealed a retroperi-toneal cystic mass which was resected successfully at laparotomy. Histopathological examination of the resected mass confirmed the diagnosis of RMC. There was no evidence of disease 2 years after surgery.
Keywords: Retroperitoneal, Mucinous cystadenoma, Cystic mass, Clinical features
INTRODUCTION
Primary retroperitoneal mucinous cystadenomas (RMCs) are very rare, even though mucinous cystadenomas are frequent ovarian tumors[1]. Like most retroperitoneal masses, they cause symptoms when growing large enough to exert pressure or obstructive effect on adjacent organs[2]. Because of the limited number of reported cases, the biological behavior and histogenesis of such tumors remain speculative[3]. Laboratory studies and imaging methods cannot achieve an accurate preoperative diagnosis[1]. We describe here a case of a huge RMC presenting with a palpable abdominal mass and a literature review is also given together with discussion.
CASE REPORT
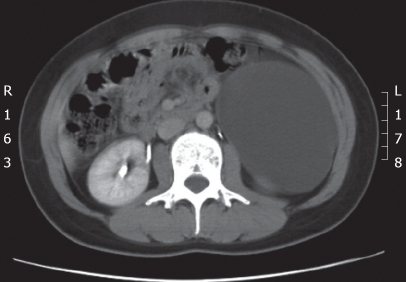
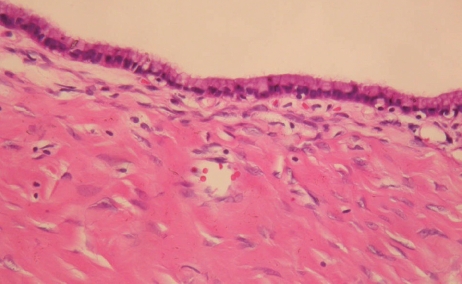
A 29-year-old woman presented at our institution with abdominal pain for 1 wk and a palpable mass on the left side of her abdomen. The abdominal pain was described as intermittently cramping and the intensity of pain was exacerbated as the palpable mass grew. She denied any systemic disease or history of drug abuse. Physical examination and pelvic examination showed no remarkable findings except for a large mobile mass which was palpable over her left flank region. The laboratory data were within reference ranges. Tumor markers, including CA199, CA125 and CEA were normal. The KUB film demonstrated a large hazy mass located over the left side of the abdomen displacing the left-side colon medially. Contrast-enhanced computed tomography (CT) of the abdomen showed a well-defined homogenous hypodense mass, which measured 12 cm × 6.5 cm in size, occupying the left retroperitoneal space with medial displacement of the descending colon (Figure 1). Because a retroperitoneal cystic mass was considered, the patient underwent surgical excision of the tumor. At laparotomy, the mass was located behind the descending colon. The white line of Toldt was divided to expose the cystic mass. A huge retroperitoneal cystic mass was resected, measuring 20 cm × 14 cm × 6 cm in size and 900 mg in weight (Figure 2). The uterus and both ovaries were normal. There was no spread of the tumor in the abdominal cavity. Histopathological assessment of the resected mass disclosed a picture of mucinous cystadenoma lined by a single layer of columnar epithelium with mucin production and surrounded by dense fibrous tissues (Figure 3). A diagnosis of primary RMC was made. The postoperative course was uneventful and she remained asymptomatic with ensuing two years of follow-up.
Figure 1.
Contrast-enhanced CT of the abdomen showing a 12 cm × 6.5 cm homogenous cystic mass in the retroperitoneal space with medial displacement of the descending colon.
Figure 2.

Photograph of the resected mass measuring 20 cm × 14 cm × 6 cm in size.
Figure 3.
Photomicrograph showing a single layer of mucin-producing columnar epithelium with underlying fibrous connective tissue (HE, × 100).
DISCUSSION
Primary retroperitoneal mucinous tumors are rare. The most common type of retroperitoneal mucinous tumors is the RMC, which shares a histological similarity to ovarian mucinous cystadenomas but can arise at any location in the retroperitoneum without attachment to the ovary [4]. The histogenesis of primary RMCs remains unclear. Three main theories have been proposed to explain the histogenic origin of mucinous cystadenomas in the retroperitoneum. These tumors can arise from teratoma[5,6], heterotopic ovarian tissue[4,5], or mucinous metaplasia of the mesothelial lining cells[4,5,7-9]. Primary RMCs occur exclusively in women[1,4], although three cases of RMC in men have been reported in the literature[10]. Some authors questioned the diagnosis of these lesions as benign because all three patients died of the disease[11]. Furthermore, Subramony et al[4] reported that the estrogen receptor is positive in stromal cells of a RMC, which could explain the exclusive occurrence of these tumors in women.
In the present study, we performed a literature review using Medline starting in 1970, and found a total of 19 cases of primary RMCs in the English literature. Based on these cases, including the present one, it was found that all cases were women, with an age range of 14 to 85 years (Table 1). The size of reported tumors ranged from 7 cm to 30 cm. There was no relationship between the age of patients and the size of tumors. The symptoms were nonspecific and most of the patients complained of asymptomatic mass or abdominal discomfort. The preoperative diagnosis was mesenteric cyst in 4 cases, ovarian cyst in 3 cases, and retroperitoneal cystic tumor in one case. Interestingly, preoperative diagnosis of renal cyst was considered in 2 cases. Serum levels of tumor markers were normal in 4 cases. However, two cases demonstrated a slight elevation of CA199 and CA125 levels, respectively. There was no evidence of recurrence after surgical management in 9 patients.
Table 1.
Cases of primary RMC in the English literature since 1970
| Reference | Sex | Age | Symptom | Tumor size (cm) | Preoperative diagnosis | Tumor markers | Operation | Outcome (mo) |
| 1 | Woman | 35 | Fullness | 14 | ND | ND | Right retroperitoneal approach | ND |
| 2 | Woman | 39 | Asymptomatic mass | 10 × 9 × 5 | ND | ND | Exploratory laparoscopy | ND |
| 3 | Woman | 18 | Flatulence | 11 × 8 × 7 | ND | Elevated CA199 | Laparotomy | ND |
| Woman | 85 | Periumbilical pain | 21 × 14 × 8 | Ovarian cyst | ND | Laparotomy | ND | |
| 4 | Woman | 25 | Asymptomatic mass | 30 × 25 × 10 | Ovarian cystic mass | ND | Laparotomy | ND |
| 5 | Woman | 19 | Asymptomatic mass | 6 × 10 | Mesenteric cyst | ND | Celiotomy | NR (18) |
| 6 | Woman | 26 | Asymptomatic mass | 22 × 16 × 10 | ND | ND | Laparotomy | ND |
| 7 | Woman | 58 | Asymptomatic mass | 7 | ND | ND | Laparotomy | ND |
| 8 | Woman | 44 | Asymptomatic mass | 30 × 20 × 14 | ND | CA125:75 IU/mL | Laparotomy | ND |
| 9 | Woman | 48 | Fullness | 15 × 13 × 9 | Mesenteric cyst | ND | Laparoscopic resection | NR (8) |
| 11 | Woman | 68 | Asymptomatic mass | 8 × 8 | Renal cyst | ND | Laparotomy | ND |
| 12 | Woman | 43 | Backache | 12 × 11 × 6.5 | ND | ND | Laparotomy | NR (16) |
| Woman | 25 | Abdominal pain | 10 | ND | ND | Gastrectomy | Died 17 d postop | |
| Splenectomy, nephrectomy | ||||||||
| 14 | Woman | 45 | Asymptomatic mass | 9 × 6.5 | ND | Normal | celiotomy | NR (3) |
| 15 | Woman | 14 | Asymptomatic | 13 × 9 × 15 | Mesenteric cyst | ND | Laparotomy | NR (13) |
| Cystic teratoma | ||||||||
| 16 | Woman | 38 | Vague abdominal discomfort | 10.0 × 7.5 × 5.5 | ND | Normal | Celiotomy | NR (12) |
| 17 | Woman | 32 | Asymptomatic mass | 11 × 7 | ND | ND | Celiotomy | NR (19) |
| 18 | Woman | 21 | Abdominal discomfort | 10 × 5.5 × 6 | ND | ND | Laparotomy | ND |
| 19 | Woman | 28 | Left flank pain | 9 × 10 × 10.9 | Renal cyst | ND | ND | ND |
| Present case | Woman | 29 | Abdominal pain, mass | 20 × 14 × 6 | Retroperitoneal cystic mass | Normal | Laparotomy | NR (24) |
ND: Not described; NR: No recurrence.
Preoperative diagnosis of primary RMCs is reportedly very difficult due to a lack of pathognomonic clinical features. Based on the review of cases reported in the English literature (Table 1), most patients presented with asymptomatic mass and vague abdominal discomfort. Reported tumors were relatively large, which may be large enough to evoke clinical symptoms or perceived by the patients. However, no cases examined presented with severe abdominal pain. Laboratory studies, including serum tumor markers and cytology study of cystic fluid are not helpful in making diagnosis of the tumors[1,14,20]. However, Motoyama et al[21] reported that measurement of CEA level in the cystic fluid may be useful in making the diagnosis. With regard to the imaging characteristics of RMCs, these tumors usually manifest as homogenous unilocular cystic masses at CT of the abdomen[20]. Furthermore, displacement of colon, kidney or ureter may suggest the retroperitoneal location of tumors[1,20]. As for the management of primary RMCs, complete surgical excision is recommended to eliminate the risk of infection, recurrence, and malignant degeneration[1,2], although these tumors seem to behave in a benign fashion with no recurrences after surgical removal, as demonstrated in our study. Exploratory laparotomy with complete enucleation of the cyst is traditionally indicated, although successful laparoscopic excision of a primary RMC has been reported[9].
In conclusion, when confronted with a cystic mass in the retroperitoneum, a primary RMC should be included in the list of differential diagnosis. Complete surgical removal of the tumor is recommended because of high risk of infection, recurrence and malignant potential.
Footnotes
Peer reviewer: Chung-Mau Lo, Professor, Department of Surgery, The University of Hong Kong, Queen Mary Hospital, No. 102 Pokfulam Road, Hong Kong, China
S- Editor Li DL L- Editor Wang XL E- Editor Yin DH
References
- 1.Lai EC, Chung KM, Lau WY. Primary retroperitoneal mucinous cystadenoma. ANZ J Surg. 2006;76:537. doi: 10.1111/j.1445-2197.2006.03768.x. [DOI] [PubMed] [Google Scholar]
- 2.Arribas D, Cay A, Latorre A, Cordoba E, Martinez F, Lagos J. Retroperitoneal mucinous cystadenoma. Arch Gynecol Obstet. 2004;270:292–293. doi: 10.1007/s00404-003-0515-8. [DOI] [PubMed] [Google Scholar]
- 3.Isse K, Harada K, Suzuki Y, Ishiguro K, Sasaki M, Kajiura S, Nakanuma Y. Retroperitoneal mucinous cystadenoma: report of two cases and review of the literature. Pathol Int. 2004;54:132–138. doi: 10.1111/j.1440-1827.2004.01595.x. [DOI] [PubMed] [Google Scholar]
- 4.Subramony C, Habibpour S, Hashimoto LA. Retroperitoneal mucinous cystadenoma. Arch Pathol Lab Med. 2001;125:691–694. doi: 10.5858/2001-125-0691-RMC. [DOI] [PubMed] [Google Scholar]
- 5.Pennell TC, Gusdon JP Jr. Retroperitoneal mucinous cystadenoma. Am J Obstet Gynecol. 1989;160:1229–1231. doi: 10.1016/0002-9378(89)90201-9. [DOI] [PubMed] [Google Scholar]
- 6.Williams PP, Gall SA, Prem KA. Ectopic mucinous cystadenoma. A case report. Obstet Gynecol. 1971;38:831–837. [PubMed] [Google Scholar]
- 7.Banerjee R, Gough J. Cystic mucinous tumours of the mesentery and retroperitoneum: report of three cases. Histopathology. 1988;12:527–532. doi: 10.1111/j.1365-2559.1988.tb01972.x. [DOI] [PubMed] [Google Scholar]
- 8.Balat O, Aydin A, Sirikci A, Kutlar I, Aksoy F. Huge primary mucinous cystadenoma of the retroperitoneum mimicking a left ovarian tumor. Eur J Gynaecol Oncol. 2001;22:454–455. [PubMed] [Google Scholar]
- 9.Chen JS, Lee WJ, Chang YJ, Wu MZ, Chiu KM. Laparoscopic resection of a primary retroperitoneal mucinous cystadenoma: report of a case. Surg Today. 1998;28:343–345. doi: 10.1007/s005950050137. [DOI] [PubMed] [Google Scholar]
- 10.Hansmann G, Budd J. Massive Unattached Retroperitoneal Tumors: An Explanation of Unattached Retroperitonel Tumors Based on Remnants of the Embryonic Urogenital Apparatus. Am J Pathol. 1931;7:631–674. [PMC free article] [PubMed] [Google Scholar]
- 11.de Peralta MN, Delahoussaye PM, Tornos CS, Silva EG. Benign retroperitoneal cysts of mullerian type: a clinicopathologic study of three cases and review of the literature. Int J Gynecol Pathol. 1994;13:273–278. doi: 10.1097/00004347-199407000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Rothacker D, Knolle J, Stiller D, Borchard F. Primary retroperitoneal mucinous cystadenomas with gastric epithelial differentiation. Pathol Res Pract. 1993;189:1195–1204. doi: 10.1016/S0344-0338(11)80844-7. [DOI] [PubMed] [Google Scholar]
- 13.Bortolozzi G, Grasso A, Zasso B. Mucinous cystadenoma of the retroperitoneum. A case report and review. Eur J Gynaecol Oncol. 1995;16:65–68. [PubMed] [Google Scholar]
- 14.Yunoki Y, Oshima Y, Murakami I, Takeuchi H, Yasui Y, Tanakaya K, Konaga E. Primary retroperitoneal mucinous cystadenoma. Acta Obstet Gynecol Scand. 1998;77:357–358. [PubMed] [Google Scholar]
- 15.Tamura T, Yamataka A, Murakami T, Okada Y, Kobayashi H, Ohshiro K, Lane GJ, Miyano T. Primary mucinous cystadenoma arising from behind the posterior peritoneum of the descending colon in a child: a case report. Asian J Surg. 2003;26:237–239. doi: 10.1016/S1015-9584(09)60313-4. [DOI] [PubMed] [Google Scholar]
- 16.Min BW, Kim JM, Um JW, Lee ES, Son GS, Kim SJ, Moon HY. The first case of primary retroperitoneal mucinous cystadenoma in Korea: a case report. Korean J Intern Med. 2004;19:282–284. doi: 10.3904/kjim.2004.19.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheen-Chen SM, Eng HL. Retroperitoneal mucinous cystadenoma. Dig Dis Sci. 2006;51:752–753. doi: 10.1007/s10620-006-3202-3. [DOI] [PubMed] [Google Scholar]
- 18.Kehagias DT, Karvounis EE, Fotopoulos A, Gouliamos AD. Retroperitoneal mucinous cystadenoma. Eur J Obstet Gynecol Reprod Biol. 1999;82:213–215. doi: 10.1016/s0301-2115(98)00254-1. [DOI] [PubMed] [Google Scholar]
- 19.Ginsburg G, Fraser J, Saltzman B. Retroperitoneal mucinous cystadenoma presenting as a renal cyst. J Urol. 1997;158:2232. doi: 10.1016/s0022-5347(01)68209-0. [DOI] [PubMed] [Google Scholar]
- 20.Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353–1365. doi: 10.1148/rg.245045017. [DOI] [PubMed] [Google Scholar]
- 21.Motoyama T, Chida T, Fujiwara T, Watanabe H. Mucinous cystic tumor of the retroperitoneum. A report of two cases. Acta Cytol. 1994;38:261–266. [PubMed] [Google Scholar]