Abstract
This study examined the internal validity of an adapted version of the U.S. Household Food Security Survey Module administered to a sample of 241 pregnant Latinas. Single-parameter logistic (Rasch) measurement model was used to assess the psychometric properties of the adapted module. Two of 14 questions examined did not fit within the acceptable range (0.70-1.30). The severity level of 12 of the 14 questions was similar across two time periods, before pregnancy and the past month of pregnancy. These findings suggest the adapted module is valid for use among pregnant Latinas, yet some items might not be applicable during pregnancy.
Keywords: food security, psychometric properties, Latinas, pregnancy
Introduction
Ever since the 1960s, Americans have been conscious of the presence of poverty and hunger within the United States. The documentary, Hunger in America, spotlighted the plight of the poor in the United States and raised awareness that hunger exists in this wealthy country. However, conceptualizing and measuring hunger has only evolved within the past 20 years. In the late 1980s, researchers developed a conceptual framework that described the concept of hunger as a “managed process” with psychological, quality, quantity, and social components.1 In 1990, the Life Sciences Research Office (LSRO) defined the broad process of accessing food as food security and redefined the concept of hunger to a physical experience.2
Measuring food insecurity and hunger within these definitions and conceptual framework became the focus of the United States government in the early 1990's. Two scales developed by researchers in the late 1980's, the Radimer/Cornell Hunger Scale and the Community Childhood Hunger Identification Project (CCHIP) Hunger Scale, laid the groundwork for the development and implementation of a national instrument in 1995 to assess food insecurity in the United States.3
This instrument, the US Household Food Security Scale Module (US HFSSM), is comprised of 15 “stem” items and 3 frequency questions. The 15 “stem” items ask about specific household events that precipitate food insecurity and specify whether it has occurred within a specific time frame, such as the previous year. Events range from less severe events, such as worrying whether there would be enough money for food, to more severe events, such as going a whole day without eating because there wasn't enough money for food. The more items are affirmed by an individual/household, the more severe the level of food insecurity is in the household. It is expected that households that have not experienced food insecurity within the specified time period of reference, will not affirm any of the items in the US HFSSM. It is also expected that households that are experiencing more severe levels of food insecurity will affirm many of the items, especially those with events that reflect their level of food insecurity. Psychometric testing of the US HFSSM helps determine whether the severity of an item and the actual household's food security status match in the manner they should. If so, the internal validity of the instrument is considered good, indicating the items in the US HFSSM assess the underlying concept of food insecurity.
The US HFSSM has undergone rigorous psychometric testing in the past 12 years to ensure it is valid and reliable at measuring the concept of food insecurity among diverse racial/ethnic populations and age groups.4-7 Various analytical methods have been used to evaluate the internal validity of the US HFSSM. 4,7,8 One method that has been used extensively is the one-parameter item response theory model, the Rasch model.
In the case of food insecurity, the Rasch model estimates the probability that a household at a specific ability level will affirm an item at a specific difficulty level.9 Using a mathematical equation,9 the Rasch model estimates the log-odds linear function where the difference between a household's food insecurity score (S) and an item severity score (βt) determines the probability, Pt (S), of an affirmative response to item t for a household that has a food insecurity score of S:
Several assumptions must be met to use the Rasch model to evaluate the internal validity of any instrument, including the US HFSSM: a) the instrument measures a one-dimensional trait, which is food insecurity; b) the items that comprise an instrument are conditionally independent, which implies that for all households that have that same ability level, the probability that a household will affirm a response to each item is statistically independent of another household's response; 9 c) if households do not share the same ability level, the Rasch model accepts that those with higher scores (such as higher food insecurity scores) will have a higher probability of affirming an item; 9 d) the items that comprise the instrument discriminate equally and that there is equal discrimination for all populations,5 thus for the US HFSSM, all items will have the same value when calculating a food insecurity score for a household;10 e) an instrument was not administered under time-restricted conditions and that there was minimal guessing of the answers by respondents.
When evaluating the US HFSSM, the Rasch model asserts that 1) food secure respondents are more likely not to affirm the milder food insecurity questions and 2) food insecure respondents are more likely to affirm the more severe food insecurity questions.4 The Rasch model evaluates the relationship between the severity of food insecurity and the food insecurity score by examining the severity of food insecurity at both the household level (equivalent to a respondent's ability) and at the item level. The severity of food insecurity at the household level is estimated separately from the severity of the items.11 This allows the US HFSSM to be administered to different subpopulations, such as households with children and household without children even though a different number of questions is asked.4
The Rasch model produces estimates of the severity of households and items based on the observed values. The Rasch model also estimates the degree to which an item or household “fits” the expectations of the Rasch model.12 Items “fit” if there is a greater probability that households with more severe food security will score higher than households with less severe food insecurity.11 Households “fit” if there is a greater probability that households with a certain severity of food insecurity will affirm less severe items more often than more severe items.11
The Rasch model has been found to be a method of examining the internal validity of the US HFSSM to ensure that it is measuring food insecurity among the sampled population. However, the ability of the US HFSSM to measure food insecurity among pregnant women has not been examined. The unique physiological changes and increased nutritional needs woman experience during pregnancy, influence household-level food purchasing and distribution decisions.13 Therefore, specific questions in the US HFSSM may not be applicable to pregnant women. Thus, the objective of this study was to assess the psychometric properties of the adapted US HFSSM to determine if it is a valid tool to measure household food insecurity among low-income pregnant Latinas.
Methods
Study design
Qualitative phase
The adaptation of the U.S. Food Security Scale Module is described in detail in a previous publication.14 Briefly, three focus groups were used to examine the face validity of the US HFSSM among pregnant Latinas. The results were used to adapt the US HFSSM to the target population. The adapted version is called the Hartford-HFSSM (Table 1).
Table 1.
The food security questions in the Hartford-HFSSM.a
| Item | Questionsb |
|---|---|
| 1 | Did you or other adults in your household worry whether your food would run out before you got money to buy more?b,c |
| 2 | Has the food you or other adults in your household bought just not lasted and you didn't have money to buy more? |
| 3 | Has there been a time when you or other adults in your household have not had enough money to eat healthy and varied meals? |
| 4 | Has there been a time when you or other adults in your household have relied on only a few kinds of cheap foods to feed the child(ren) to avoid running out or because you were running out of money to buy food? (by cheap we mean low cost foods that are not healthy and nutritious) |
| 5 | Has there been a time when you or other adults in your household have not been able to feed the children a healthy and varied diet, because you didn't have enough money? |
| 6 | Has there been a time when the children have not eaten enough because there wasn't enough money in your household to buy enough food? |
| 7 | Has there been a time when you or other adults in the household ever cut the size of your meals or skipped breakfast, lunch or dinner because there wasn't enough money for food? |
| 8 | Have you ever eaten less than you felt you should because there wasn't enough money to buy food? |
| 9 | Have you ever been hungry but didn't eat because you just couldn't get more food? |
| 10 | Have you lost weight because you haven't had enough money for food? |
| 11 | Have you or other adults in your household ever not eaten for a whole day because there wasn't enough money for food? |
| 12 | Have you or other adults in your household ever cut the size of the children's meals because there wasn't enough money to buy more food? |
| 13 | Have any of the children in your household ever skipped breakfast, lunch, or dinner because there wasn't enough money for food? |
| 14 | Have the children in your household ever been hungry but you just couldn't get more food? |
| 15 | Have any of the children in your household ever not eaten for a whole day because there wasn't enough money for food? |
Questions assess food insecurity across the periods of time, the year before pregnancy and the past month of pregnancy.
Participants who responded affirmatively to any Hartford-HFSSM question during the year before their pregnancy were asked: “How often did this happen?” The options were: a) every month or almost every month, b) some months but not every month, c) one month. They were then asked: “Which week or weeks of the month did this usually happen?” with the options being 1st, 2nd, 3rd, 4th week. The latter question was the only frequency question asked over the time period during pregnancy.
Quantitative phase
The Hartford-HFSSM was administered in a prenatal survey to a convenience sample of 241 pregnant Latinas. Of the 242 pregnant Latinas surveyed, 104 were surveyed from July 2004 to December 2004, while 138 were surveyed from September, 2005 to December, 2006 as part of a larger longitudinal study evaluating prenatal nutrition and pregnancy outcomes.13,15 Participants were recruited from an existing maternal and infant service program at a local community agency, community programs (such as the Special Supplemental Nutrition Program for Women, Infants, and Children), and street outreach. Participants were eligible if they were: a) self-identified as Latina, b) pregnant, c) lived in the Hartford area, d) 18 years of age or older, e) participating in WIC or eligible for WIC. Women recruited from September, 2005 to December, 2006 had additional eligibility restrictions. They had to be between 4 to 8 months pregnant, planning to deliver at one of the two city hospitals, and could not be living at a shelter at the time of the study.
Bilingual/bicultural interviewers from the target community administered the Hartford-HFSSM in the language of choice of the participant (English or Spanish). The Hartford-HFSSM was included as part of a prenatal survey that lasted approximately three hours. The Hartford-HFSSM was asked over two time periods: before pregnancy and during pregnancy. Food security before pregnancy was assessed by asking participants to answer the Hartford-HFSSM questions over the period of time in the 12 months before they became pregnant. Food insecurity during pregnancy was assessed over the past month of pregnancy to provide a standard time frame of reference since women were enrolled in the study at various stages of pregnancy. To prevent any participant confusion between the two time periods, the Hartford-HFSSM questions assessing food insecurity before pregnancy were asked at the beginning of the prenatal survey and the Hartford-HFSSM questions assessing food insecurity during pregnancy were asked at a later time in the survey.
Prior to administration of the prenatal survey, interviewers were trained on the content and administration of each instrument in the survey, including the Hartford-HFSSM. The specialized training in the Hartford-HFSSM involved having interviewers read each question, having the purpose and content of each question explained by the study coordinator, and conducting practice interviews of the Hartford-HFSSM. To minimize interviewer bias, interviewers were instructed to read each question exactly as written and to respond to a participant's request for an explanation of the question by rereading the question rather than providing an explanation.
Written informed consent was obtained from all participants prior to administration of the survey. Approval from the Human Subjects Committee of the Institutional Review Boards from the lead institution, the University of Connecticut, and collaborating institutions, Hartford Hospital and the Hispanic Health Council, was received prior to study implementation.
Statistical analyses
Several steps were taken to prepare the pooled sample data to test the psychometric properties of the Hartford-HFSSM before and during pregnancy. The Hartford-HFSSM contained 15 items, which were adaptations of the original US HFSSM 15 ‘stem’ items. Each item in the Hartford-HFSSM was asked as a question, eliciting a yes/no response. All items were coded dichotomously with all affirmative responses being coded as a 1 and negative responses were coded as a 0. Frequencies were generated for each item to determine the prevalence of households experiencing each event (as indicated by an affirmative response to the item). Item 15, which asked whether the child has gone a whole day without eating because there wasn't any money to buy more food, was affirmed by 4 households before pregnancy and only one household during pregnancy. Thus, this item was removed from subsequent analyses evaluating the severity of the 15-items as well as of the 7 child items. Item severity scores were generated for the remaining 14-items in the Hartford-HFSSM, then separately for the 6 child items and 8 adult items using WINSTEPS version 3.64.2 software. This software fits the Rasch model to dichotomous data to assess the validity of a unidimensional scale through statistics such as item severity and infit statistics. All item severity scores were rescaled to positive values in a method similar to that used in other studies.7 Item severity scores from both time periods were compared to each other to evaluate whether the severity of the items were equivalent before pregnancy and during pregnancy. If the difference between item severity levels for an item was > 1.0, that item was not considered to be of a similar severity level across both time periods.
Item fit statistics were also generated using the Rasch model. Infit values, generated to determine whether each items fits to the expectations of the Rasch model, were used to evaluate internal validity. An item was considered to fit the model if the infit value fell within the range of 0.7 – 1.3.
The Cronbach alpha internal consistency test was run using the Statistical Package for the Social Sciences (SPSS) software version 14.0.2 to evaluate the reliability of the Hartford-HFSSM. Chi squares were also run to evaluate significant differences in the response to each of the questions by Latina subgroups (Puerto Rican Latinas and Non-Puerto Rican Latinas). Since the sample size of affirmative responses for many items was very small when broken down by ethnicity, Rasch model analyses were conducted on the pooled sample only.
Data from the Hartford-HFSSM over the time period during pregnancy were excluded from all analyses for eight participants. Two participants had unreliable data and were removed from the analyses. Four participants were excluded because we were unable to confirm that the “child” they had in their household was younger than 18 years of age. Finally, due to the unique experience of living in a shelter and the effect this has on food insecurity,16 two participants were excluded from analyses because their current residence was local area shelters. Therefore, 233 participants were included in the analyses testing the psychometric behavior of the Hartford-HFSSM during pregnancy.
Data from the Hartford-HFSSM was not included in the analyses over the time period before pregnancy if: a) it was unreliable (n=7), b) a participant had been pregnant the year before her current pregnancy (n=2), c) a participant lived in temporary housing such as a shelter or a hotel (n=2), d) a participant lived at college the previous year before pregnancy where she was provided with 3 meals a day (n=1), d) it was not clear if there were children less than 18 years living in their household (n=11). The Hartford-HFSSM was not administered to seven participants because it was temporarily removed from the survey. Data was analyzed using the remaining 211 participants.
Results
Participants were on average 24.6 years old and had lived in the United States for an average of 11.3 years (Table 2). Over 68% of participants were born in a country or territory outside of the continental United States. More than two-thirds (67.4%) of participants were of Puerto Rican descent. The majority of participants were bilingual, but over 60% spoke predominately Spanish at home. Most participants had a high school education or less and were unemployed. Only 44.6% reported that they had a partner. Over two-thirds of participants (69.2%) reported a monthly household income of $1000 or less. On average household size was four persons, including the participant. Less than half of the participants in the study were enrolled in the Food Stamp Program (48.9%), but most were participating in the WIC program (85.0%). Upon enrollment in the study, over half (59.3%) of participants were in their second pregnancy trimester. This was the first baby for 36.5% of the study participants.
Table 2.
Prenatal survey participant characteristics.
| Mean (SD) | Na | |
|---|---|---|
| Age | 24.6 (5.50) | 233 |
| Years in the United States | 11.3 (9.16) | 233 |
| Number of people in the household (including participant) | 4.09 (1.90) | 233 |
| Percent | N | |
| Identity | ||
| Puerto Rican Latina | 67.4 | 157 |
| Non-Puerto Rican Latinab | 32.6 | 76 |
| Country of Birth | ||
| Foreign bornc | 68.1 | 158 |
| United States | 31.9 | 74 |
| Preferred Language | ||
| English | 2.6 | 6 |
| Spanish | 42.5 | 99 |
| Both | 54.9 | 128 |
| Language at home | ||
| English | 18.6 | 43 |
| Spanish | 61.5 | 142 |
| Both | 19.9 | 46 |
| Education, high school or less | 81.5 | 190 |
| Unemployed | 81.1 | 189 |
| Marital status, partner | 44.6 | 104 |
| Income | ||
| $0 - $1000 | 69.1 | 130 |
| more than $1000 | 30.9 | 58 |
| Food stamp participation, yes | 48.9 | 114 |
| WIC participation, yes | 85.0 | 198 |
| Primipara | 36.5 | 85 |
| Pregnancy Trimester | ||
| 1st d | 4.8 | 11 |
| 2nd | 59.3 | 137 |
| 3rd | 35.9 | 83 |
No more than 1% were missing for analyses for variables, except for monthly household income (n=184) because many participants did not know this information.
Includes participants who identified themselves as: Mexican (12.4%), Peruvian (6.6%), Guatemalan (2.9%), Dominican (2.5%), Honduran (2.5%), Colombian (2.1%), El Salvadorian (1.2%), Uruguayan (0.8%), Ecuadorian (0.8%), Argentinean (0.4%), Bolivian (0.4%), and Cuban (0.4%).
Includes those who were born in a country or territory outside of the United States.
An exclusion criteria for the longitudinal study.
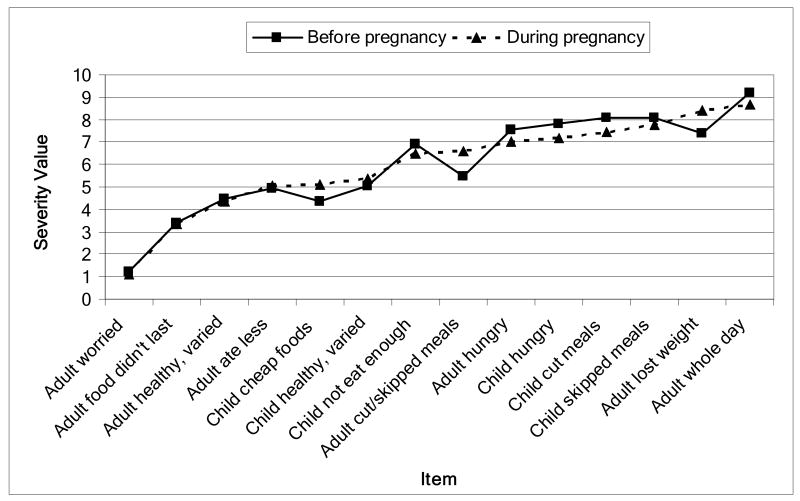
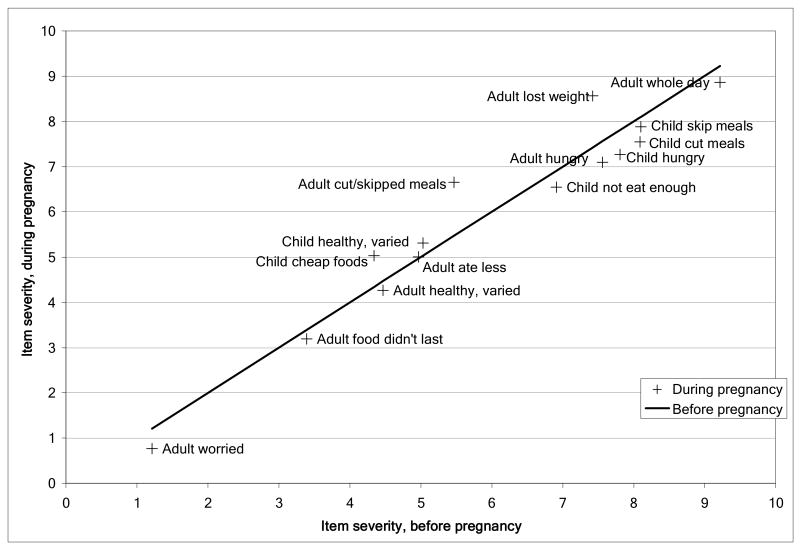
Reliability, assessed using Cronbach's alpha, was 0.91 for the Hartford-HFSSM before pregnancy and 0.88 during pregnancy. Figure 1 illustrates the relative severity of the 14 items in the Hartford-HFSSM ordered from less severe to more severe. Questions that indicated psychological worry and reduced food quality, such as did you or other adults in your household worry whether your food would run out before you got money to buy more, were less severe while questions referring to reductions in amount of food consumed among adults and children were more severe (i.e. cut or skipped meals, adult/child hunger, and not eating for a whole day). During pregnancy, adult items which indicated losing weight and not eating for a whole day were more severe than any child item. However, before pregnancy only the latter was more severe than any child item, while losing weight was less severe than the items of adult and child hunger and cutting or skipping children meals. Across both time periods, the proportion of households that affirmed each question decreased as the severity of the item increased (results not shown).
Figure 1.
Severity values for 14 items in the Hartford-HFSSM administered before and during pregnancy. a, b
a N=156 for household with children before pregnancy and N=170 for households with children during pregnancy.
b Child whole day variable was not included due to only 4 affirmative responses before pregnancy and 1 affirmative response during pregnancy.
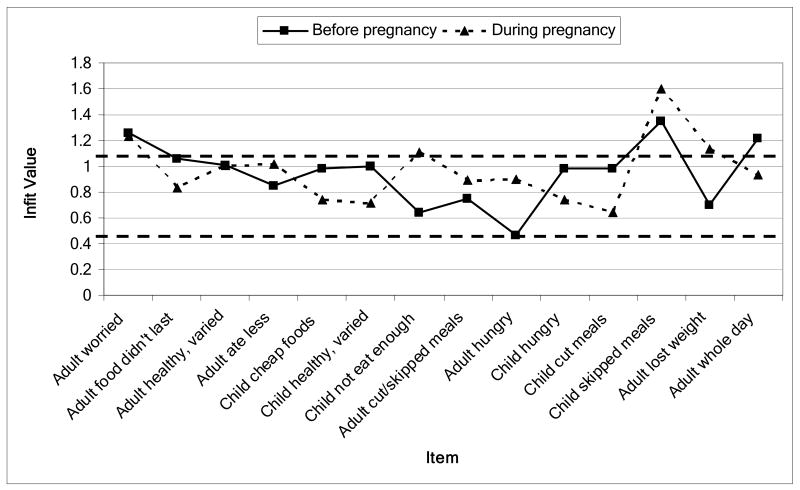
Figure 2 presents infit values for the 14 items in the Hartford-HFFM scale. Before pregnancy, three items, child not eat enough, child skipped meals, and adult hungry, had infit values that were not within the expected range (0.64, 1.35, and 0.47, respectively). During pregnancy, two child items, child cut meals and child skipped meals, had infit values outside the expected range (0.7-1.3) at 0.64 and 1.60, respectively.
Figure 2.
Infit values for each item in the Hartford-HFSSM administered before and during pregnancy a, b
a N=156 for household with children before pregnancy and N=170 for households with children during pregnancy.
b Child whole day variable was not included due to only 4 affirmative responses before pregnancy and 1 affirmative response during pregnancy.
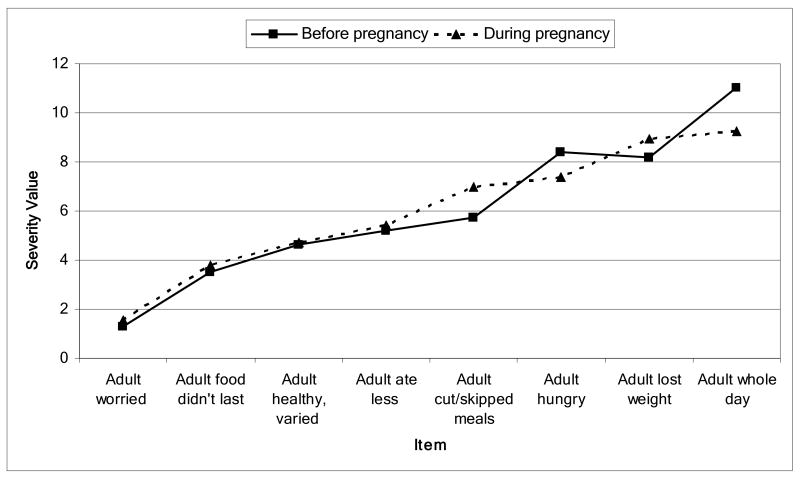
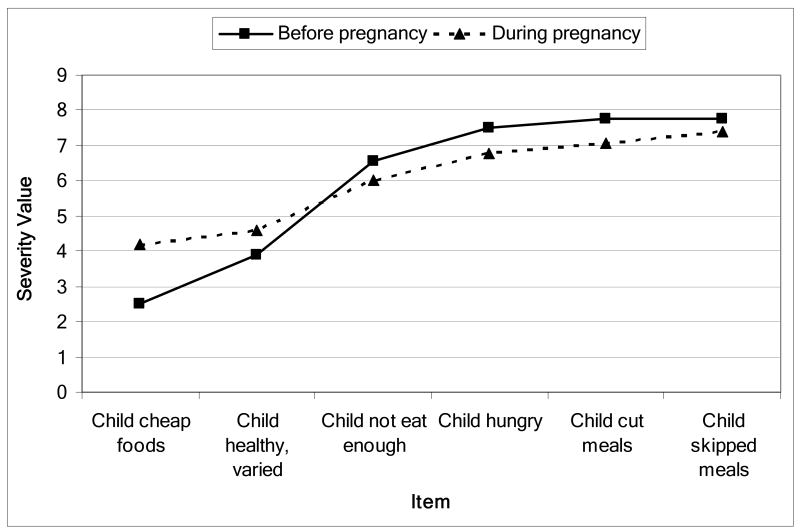
Figures 3 and 4 reflect the relative severity scores of the adult/household items and child items, respectively. Over both time periods, the severity of the adult/household items and child items showed that the less severe items were those that identified psychological or reduced food quality, while more severe items were those that evaluated reduced food consumption.
Figure 3.
Item severity values for the 8 adult items in the Hartford-HFSSM administered before and during pregnancy. a, b
a N=156 for household with children before pregnancy and N=170 for households with children during pregnancy.
b Child whole day variable was not included due to only 4 affirmative responses before pregnancy and 1 affirmative response during pregnancy.
Figure 4.
Item severity values for child items in the Hartford-HFSSM before and during pregnancy. a, b
a N=170 for households with children during pregnancy and N=156 for those before pregnancy.
b Child whole day variable was not included due to only 1 affirmative response.
When the infit values for the 8 adult/household items were examined, all items assessed during pregnancy had values that fell within the range of 0.7-1.3 (figure not shown). Before pregnancy, two adult items evaluating adult hunger and adult cutting/skipping meals had infit values lower than the acceptable range (0.54 and 0.67, respectively). Assessing the infit values of the 6 child items during pregnancy, two child items, child cut meals and child skipped meals, had infit values outside the expected range at 0.64 and 1.60, respectively, (figure not shown). Before pregnancy, the item child not eat enough had a low infit value at 0.56. These reflect similar findings as seen with the infit values of the 14 items of the Hartford-HFSSM.
Figure 5 compares the item severity values from the Hartford-HFSSM administered during pregnancy with item severity values from the same scale examining food insecurity over the 12 months before pregnancy. The figure shows that overall the severity values for the items administered during pregnancy were similar to the severity values for the items administered over the period of time before pregnancy. Two items, adult lost weight and adult cut/skipped meals, had much higher severity values during pregnancy than before pregnancy indicating they were interpreted as more severe events during pregnancy. Thus, women were less likely to answer “yes” to these questions during pregnancy than before pregnancy.
Figure 5.
Comparison of item severity values between the Hartford-HFSSM administered during pregnancy and the Hartford-HFSSM administered over the time period of the 12 months before pregnancy.
When the Rasch model was rerun without these two items, the severity values for the 12 items were similar between the two scales (before and during pregnancy).
Discussion
This study fills a gap in the literature by testing the psychometric behavior of an adapted version of the U.S. HFSSM for pregnant Latinas. The findings from this study indicate that the Hartford-HFSSM is a valid, reliable instrument for measuring food insecurity among pregnant Latinas. Our findings showed good reliability (Cronbach's alpha > 0.80) of the Hartford-HFSSM across both time frames. For both time periods, the great majority of the items in the Hartford-HFSSM fit within the expectations of the Rasch model, indicating that these items capture the food insecurity construct. Two items assessed before pregnancy, child not eat enough and adult hungry, and one item assessed during pregnancy, child cut meals, had infit values below the expected range, suggesting a degree of redundancy of these questions in the scale. Our previous qualitative findings indicated that Latinas felt that questions in the scale sounded repetitive.13 If our modifications did not improve the repetitive quality of these two items, it is possible participants may have felt they were being asked the same question and their answers would have also been the same. The item child skipped meals, had infit values above the expected range both before and during pregnancy, suggesting that this question is producing erratic responses. One possible explanation is that it is common for children to skip meals due to other reasons. Therefore, this question might not be sensitive enough to be used to assess food insecurity within this low-income population.
The findings from this study suggest that some food insecurity events are more severe during pregnancy than before pregnancy. Comparison of the Hartford-HFSSM before pregnancy and during pregnancy indicated that two adult items, losing weight and cut/skipping meals, were less severe before pregnancy than during pregnancy. This suggests that these events are experienced differently during pregnancy than before pregnancy. One reason for this may be the uniqueness of pregnancy. The physiological changes that occur during pregnancy favor weight gain rather than weight loss during pregnancy. If a woman loses weight as a result of not having enough food to eat, it is reasonable to expect that this event indicates a level of food insecurity that is more severe for a women who is pregnant than one who is not pregnant. In addition, our previous research conducted in this population indicated that moderately food insecure women within the Latina community might be more likely to gain excessive weight rather than to lose weight during pregnancy.13 Therefore, this question may not be as applicable to pregnant women as it would be to non-pregnant populations. Pregnant women also experience a dilemma over whether to feed themselves and their unborn child or their children when food is limited in a household.13 This may make an event, such as cutting or skipping meals, a more difficult choice during pregnancy than it would be if the woman was not pregnant.
In conclusion, the Hartford-HFSSM was found to be a valid, reliable measure to assess household food insecurity during pregnancy among Latinas. Since valid scales are vital to obtaining quality data, having an adapted food security scale that can be used for pregnant Latinas is likely to motivate researchers to conduct more studies evaluating food insecurity among Latinas during pregnancy.
Acknowledgments
The authors would like to thank the staff from the Center for Community Nutrition as well as the Comadrona Program at the Hispanic Health Council for their unwavering assistance in implementing this study. We would also like to thank Dr. Donna Chapman and Dr. Maria Luz-Fernandez for their thoughtful review and comments on the Ph.D. dissertation that served as the foundation for this manuscript. This study was funded through the University of Connecticut Research Foundation, the University of Connecticut USDA Food Stamp Nutrition Education Program, Connecticut NIH EXPORT Center of Excellence for Eliminating Health Disparities among Latinos (NIH-NCMHD P20MD001765), and a USDA National Needs pre-doctoral fellowship.
References
- 1.Radimer KL, Olson CM, Greene JC, Campbell CC, Habicht JP. Understanding hunger and developing indicators to assess it in women and children. Journal of Nutrition Education. 1992;24:36S–44S. [Google Scholar]
- 2.Anderson SA, editor. Journal of Nutrition. 1990. Core indicators of nutritional state for difficult-to-sample populations; pp. 1557–1600. [DOI] [PubMed] [Google Scholar]; A report prepared by the Life Sciences Research Office, Federation of American Societies for Experimental Biology for the American Institution of Nutrition.
- 3.Carlson SJ, Andrews MS, Bickel GW. Measuring food insecurity and hunger in the United States: development of a national benchmark measure and prevalence estimates. Journal of Nutrition. 1999;129:510S–516S. doi: 10.1093/jn/129.2.510S. [DOI] [PubMed] [Google Scholar]
- 4.Derrickson JP, Fisher AG, Anderson JE. The core food security module scale measure is valid and reliable when used with Asians and Pacific Islanders. Journal of Nutrition. 2000;130:2666–2674. doi: 10.1093/jn/130.11.2666. [DOI] [PubMed] [Google Scholar]
- 5.Nord M. Measuring the food security of elderly persons. Family Economics and Nutrition Review. 2003 Winter; Available at: http://www.findarticles.com/p/articles/mi_m0EUB/is_1_15/ai_112167032. February 25, 2008.
- 6.Connell CL, Nord M, Lofton KL, Yadrick K. Food security of older children can be assessed using a standardized survey instrument. Journal of Nutrition. 2004;134:2566–2572. doi: 10.1093/jn/134.10.2566. [DOI] [PubMed] [Google Scholar]
- 7.Melgar-Quinonez H, Nord M, Perez-Escamilla P, Segall-Correa AM. Psychometric properties of a modified U.S. Household Food Security Survey Module in Campinas, Brazil. [February 25, 2008];European Journal of Clinical Nutrition. 2007 April; doi: 10.1038/sj.ejcn.1602760. Available at: http://www.nature.com/ejcn/journal/vaop/ncurrent/pdf/1602760a.pdf. [DOI] [PubMed]
- 8.Opsomer JD, Jensen HH, Pan S. An evaluation of the U.S. Department of Agriculture food security measure with generalized linear mixed models. Journal of Nutrition. 2003;133:421–427. doi: 10.1093/jn/133.2.421. [DOI] [PubMed] [Google Scholar]
- 9.Wilde PE. Differential response patterns affect food-security prevalence estimates for households with and without children. Journal of Nutrition. 2004;134:1910–1915. doi: 10.1093/jn/134.8.1910. [DOI] [PubMed] [Google Scholar]
- 10.Johnson MS. Item response models and their use in measuring food insecurity and hunger. Department of Statistics and Computer Information, (Baruch College, University of New York) [February 25, 2008];2004 July; Available at: http://www7.nationalacademies.org/cnstat/Item_Response_Models_and_Measuring_Food_Security_Paper.pdf.
- 11.Smith EV, Conrad KM, Chang K, Piazza J. An introduction to Rasch measurement for scale development and person assessment. Journal of Nursing Measurement. 2002;10:189–206. doi: 10.1891/jnum.10.3.189.52562. [DOI] [PubMed] [Google Scholar]
- 12.Bond TG, Fox CM. Applying the Rasch model: Fundamental measurement in the human sciences. Lawrence Erlbaum Associates Inc; 2001. [Google Scholar]
- 13.Hromi-Fiedler A. Doctoral Dissertation. Department of Nutritional Sciences, University of Connecticut; Storrs, CT: 2007. Nutrient Intakes, Food Insecurity, Pregnancy Weight Gain and Birth Outcomes among Connecticut Latinas. [Google Scholar]
- 14.Hromi-Fiedler A, Bermúdez-Millán A, Segura-Pérez S, Pérez-Escamilla R. Adaptation of the U.S. Food Security Scale Module for low-income pregnant Latinas: Qualitative Phase 1. Midwifery. doi: 10.1080/19320240802706841. Submitted 8 February 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bermúdez-Millán A. Doctoral Dissertation. Department of Nutritional Sciences, University of Connecticut; Storrs, CT: 2007. Egg Contribution to Nutrient Intakes, Pregnancy Weight Gain and Birth Outcomes among Connecticut Latinas. [Google Scholar]
- 16.Tarasuk VS, Beaton GH. Household food insecurity and hunger among families using food banks. Canadian Journal of Public Health. 1999;90:109–13. doi: 10.1007/BF03404112. [DOI] [PMC free article] [PubMed] [Google Scholar]