Abstract
Skeletal muscle insulin sensitivity improves with short-term reduction in calorie intake. The goal of this study was to evaluate changes in the abundance and phosphorylation of Akt1 and Akt2 as potential mechanisms for enhanced insulin action after 20 days of moderate calorie restriction [CR; 60% of ad libitum (AL) intake] in rat skeletal muscle. We also assessed changes in the abundance of SH2 domain-containing inositol phosphatase (SHIP2), a negative regulator of insulin signaling. Fisher 344 × Brown Norway rats were assigned to an AL control group or a CR treatment group for 20 days. Epitrochlearis muscles were dissected and incubated with or without insulin (500 μU/ml). Total Akt serine and threonine phosphorylation was significantly increased by 32 (P < 0.01) and 30% (P < 0.005) in insulin-stimulated muscles from CR vs. AL. Despite an increase in total Akt phosphorylation, there was no difference in Akt1 serine or Akt1 threonine phosphorylation between CR and AL insulin-treated muscles. However, there was a 30% decrease (P < 0.05) in Akt1 abundance for CR vs. AL. In contrast, there was no change in Akt2 protein abundance, and there was a 94% increase (P < 0.05) in Akt2 serine phosphorylation and an increase of 75% (P < 0.05) in Akt2 threonine phosphorylation of insulin-stimulated CR muscles compared with AL. There was no diet effect on SHIP2 abundance in skeletal muscle. These results suggest that, with brief CR, enhanced Akt2 phosphorylation may play a role in increasing insulin sensitivity in rat skeletal muscles.
Keywords: dietary restriction, insulin signaling, glucose transport, SH2 domain-containing inositol phosphatase, protein kinase B
MODERATE CALORIE RESTRICTION [CR; 25–40% reduction in food intake compared with ad libitum (AL)] improves insulin action in a variety of species, including mice, rats, rhesus monkeys, and humans (2, 22, 24, 28, 39) and leads to enhanced insulin-stimulated glucose transport in skeletal muscle (9) with 20 days of calorie restriction (10, 16, 18, 20). Skeletal muscle accounts for ~85% of insulin-stimulated blood glucose clearance (21), and glucose transport is a key rate-limiting step in muscle glucose utilization (48). Therefore, changes in skeletal muscle glucose metabolism are important for the enhanced, whole body insulin action seen with CR.
Brief CR increases translocation of the glucose transporter GLUT4 to the cell membrane in skeletal muscle after insulin stimulation (17). The CR effect on glucose transport is specific to the insulin-mediated pathway, because there is no effect of diet on basal glucose transport or hypoxia-stimulated glucose transport (17). These findings suggest that CR acts on the insulin-signaling pathway, but the specific cellular mechanism leading to the CR enhancement on insulin-stimulated GLUT4 translocation has not yet been identified. With brief CR, there is no change in insulin receptor number and binding affinity (3) nor its tyrosine kinase activity (11), indicating a postinsulin receptor mechanism. Accordingly, we first performed a series of experiments focused on phosphatidylinositol 3-kinase (PI 3-kinase), and we found no effect of brief CR on IRS-1, IRS-2, or phosphotyrosine-associated PI 3-kinase activity determined by in vitro PI 3-kinase assay (16, 17, 19). These results have led us to hypothesize that CR elicits enhanced signaling at a post-PI 3-kinase step.
In this context, Akt (also known as protein kinase B and RAC) is an attractive candidate for the CR-induced increase in insulin-stimulated glucose uptake. Akt is a pleckstrin homology (PH) domain-containing serine/threonine kinase, which can be activated by insulin and lies downstream of PI 3-kinase (6). Results from many (25, 27, 30, 40, 43-45), but not all (29), studies indicate that Akt modulates insulin-stimulated glucose transport.
Three isoforms of Akt have been identified: Akt1, Akt2, and Akt3 (47). Akt1 and Akt2 are widely expressed, including insulin target tissues liver, skeletal muscle, and adipose tissue (7, 47). In contrast, Akt3 is expressed highly in brain, heart, and kidney, with low expression in rat skeletal muscle (5, 33, 36, 47), and insulin activation in skeletal muscle is negligible (47). Activation of Akt1 and Akt2 by insulin requires membrane localization and phosphorylation on serine (Ser473 and Ser474, respectively) and threonine [Thr308 and Thr309, respectively (41)]. With insulin stimulation, PI 3-kinase-generated PI(3,4,5)triphosphate (PIP3) recruits Akt from the cytosol to the plasma membrane. Translocation to the membrane promotes serine phosphorylation by a yet-unidentified kinase (41), which in turn facilitates the threonine phosphorylation by pyruvate dehydrogenase kinase-1 (PDK-1) (1) and full activation of Akt.
Recent reports suggest that Akt1 and Akt2 have distinct functions in cellular regulation and that Akt2 may preferentially be involved in insulin-stimulated glucose metabolism. Akt2 knockout mice have impaired glucose tolerance and insulin resistance (13), whereas Akt1 knockout mice have normal glucose metabolism but are growth stunted (14). However, insulin-stimulated glucose uptake in skeletal muscle is not completely impaired in Akt2-null mice, suggesting that there may be some functional redundancy among the Akt isoforms or other compensatory mechanisms when Akt2 is absent. Using Akt isoform-specific RNA interference-mediated gene silencing in 3T3-L1 adipocytes, Katome et al. (27) found a greater attenuation of insulin-stimulated GLUT4 translocation and glucose uptake with reduced expression of Akt2 compared with Akt1.
The lack of a CR effect on PI 3-kinase, the enzyme that catalyzes PIP3 production, raises the possibility that CR acts by attenuating the degradation of PIP3. SH2 domain-containing inositol phosphatase (SHIP2), a 5′ lipid phosphatase that converts PI(3,4,5)P3 into PI(3,4)P2, is a negative regulator of insulin signaling (4, 15). Decreased SHIP2 protein expression leads to enhanced insulin sensitivity in mice heterozygous for the SHIP2 gene (15), whereas mutations in SHIP2 causing protein overexpression are associated with type 2 diabetes in rats and humans (32). In addition, changes in SHIP2 expression are inversely associated with Akt activation (4, 26).
The primary aim of our study was to investigate the influence of CR on Akt in skeletal muscle. To this end, we evaluated the effect of brief CR (consuming 60% of AL intake for 20 days) on Akt1 and Akt2 by measuring abundance and serine and threonine phosphorylation of each isoform in rat skeletal muscle. To understand the mechanism mediating the CR-induced changes in Akt phosphorylation, we measured SHIP2 abundance. Our results suggest that increased insulin-stimulated phosphorylation of Akt2 may play a role in mediating the CR effect of increased insulin sensitivity in rat skeletal muscle. Furthermore, increased Akt2 phosphorylation is not attributable to a decrease in SHIP2 abundance with 20 days of CR.
MATERIALS AND METHODS
Materials
A rabbit anti-phospho-Akt(Ser473) antibody was purchased from PharMingen (San Diego, CA). Sheep anti-Akt1(residues 466–480), sheep anti-Akt2 (residues 455–469) and rabbit anti-phospho-Akt(Thr308) antibodies were purchased from Upstate Biotechnology (Lake Placid, NY). A second rabbit anti-Akt2 antibody (used to measure Akt2 abundance) was a generous gift from Morris Birnbaum, PhD (University of Pennsylvania). A goat anti-SHIP2 antibody was purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Protein G agarose beads were purchased from Upstate Biotechnology. For immunodetection, either an enhanced chemiluminescence (ECL) kit from Amersham (Piscataway, NJ) or Super Signal ECL from Pierce (Rockford, IL) was used as directed. A bicinchoninic acid (BCA) assay kit for total protein determination was purchased from Pierce. Nitrocellulose membranes and blocking milk were purchased from Bio-Rad (Hercules, CA). All other chemicals were purchased from Sigma (St. Louis, MO).
Animal treatment
Four-month-old male, Fisher 344 × Brown Norway, F1 generation rats were obtained through the National Institute on Aging from Harlan Sprague Dawley (Indianapolis, IN). Animals were individually housed in wire-bottom cages and maintained on a 12:12-h light-dark cycle with free access to food and water for a 1-wk acclimation period. Rats were fed a standard rat chow from Harlan Teklad (Teklad Rodent Diet no. 8604, Madison, WI)
After the acclimation period, rats were ranked by weight and assigned to either an AL control group or a CR treatment group such that the initial mean weight and standard error were similar for both groups. Individual baseline food intake was determined by allowing animals to eat ad libitum for 7 days and measuring food intake and spillage each day. Rats were familiarized to a meal-feeding protocol in which rats are given a portion of 100% of their individual baseline food intake in three 1.5-h periods (35% at 0600, 25% at 1500, and 40% at 2000) for 7 days. After familiarization to the meal-feeding protocol, the AL group continued receiving 100% of baseline intake for 20 days, whereas the CR group received 60% of their individual baseline intake for 20 days. Food intake was measured daily and adjusted to account for spillage. After day 20, rats were fed the 0600 meal, removed from the animal facility, and fasted with free access to water from 1500. Rats were anesthetized with an intraperitoneal injection of pentobarbital sodium (50 mg/kg) between 1300 and 1600. The epitrochlearis muscles were dissected and used for in vitro incubations. A plantaris muscle was also dissected from each rat and immediately freeze-clamped and stored at −80°C until analysis.
In vitro incubations
Dissected epitrochlearis muscles were incubated (30°C) with gentle agitation in flasks of continuously oxygenated (95% O2-5% CO2) Krebs-Henseleit (KHB) incubation buffer [0.1% BSA, 2 mM sodium pyruvate, 6 mM mannitol] with or without insulin (500 μU/ml). After 30 min of incubation, muscles were transferred to flasks containing KHB-BSA with 8 mM 3-O-[3H]methylglucose (3-MG; 0.25 mCi/mmol; New England Nuclear Life Science products, Boston, MA), 2 mM [14C]mannitol (0.1 mCi/mmol; Amersham Pharmacia) with or without insulin as in the first incubation. After 15 min, muscles were blotted, trimmed, freeze-clamped in liquid nitrogen, and stored at −80°C until analyzed. Rate of 3-MG transport was determined by use of a portion of the muscle homogenized in 0.3 N perchloric acid as previously described (8, 16).
Muscle preparation for immunoprecipitation and immunoblotting
A portion of frozen epitrochlearis was weighed, transferred to prechilled polypropylene tubes, and homogenized in ice-cold lysis buffer (50 mM HEPES, pH 7.5, 150 mM NaCl, 10 mM sodium pyrophosphate, 2 mM Na3VO4, 10 mM NaF, 2 mM EDTA, 2 nM phenylmethylsulfonyl fluoride, 5 μg/ml leupeptin, 1% Nonidet P-40, and 10% glycerol). Homogenates were solubilized for 1 h at 4°C and then centrifuged at 12,000 g for 10 min to remove insoluble material. Protein concentration was determined by the BCA method as directed.
Immunoprecipitation
To measure Akt isoform phosphorylation, 200 μg of a muscle homogenate was first incubated with anti-Akt1 or anti-Akt2 antibody for 2 h at 4°C and then immunoprecipated using protein G agarose beads. Immunoprecipitates were solubilized with 2× Laemmili SDS buffer and boiled for 5 min. The supernatant was then resolved on a 10% SDS-polyacrylamide gel and transferred to nitrocellulose paper. The immunoblots for phosphorylated Akt isoforms followed the method described in Immunoblotting, in which nitrocellulose blots were incubated with anti-phospho-Akt (Ser473/474) or anti-phospho-Akt (Thr308/309) at (1:1,000) in 1% milk in Tris-buffered saline with 0.1% Tween 20 (TBST) overnight.
Immunoblotting
To measure Akt isoform abundance and total serine (Ser473/474) or total threonine (Thr308/309) phosphorylation of Akt, muscle homogenates were solubilized in SDS, boiled for 5 min, and subjected to 10% SDS-PAGE. For SHIP2 abundance, solubilized samples were run on a 6% SDS-PAGE. Resolved proteins were transferred to nitrocellulose paper for 2 h at constant current of 200 mA or overnight at 100 mA in electrotransfer buffer (20 mM Tris, pH 8.0, 150 mM glycine, 0.025% SDS, 20% methanol). Nitrocellulose blots were blocked with either 5% nonfat milk protein in TBST or with 3% milk protein (for Akt1) in phosphatebuffered saline with 0.05% Tween 20 (PBST) for 1 h at room temperature. Blots were washed and then incubated in milk TBST or PBST with appropriate antibody overnight at 4°C. After being washed, blots were incubated in appropriate secondary antibody (horseradish peroxidase-conjugated anti-IgG) at room temperature for 1–2 h. Excess antibody was washed off, and proteins were detected by ECL. Immunoreactive protein was quantitated by densitometry using Molecular Analyst software (Bio-Rad). The mean value for AL samples on each immunoblot, expressed in densitometry units, was adjusted to equal 1.0, and each sample value was then expressed relative to the adjusted mean value.
Statistical analysis
Student’s unpaired t-test was use to analyze differences between diet groups. A value of P < 0.05 was considered statistically significant.
RESULTS
Epitrochlearis 3-MG transport
Glucose transport results have been previously reported (16). There was no effect of CR on basal glucose transport, and there was a significant 25% increase (P < 0.05) in glucose transport for insulin-stimulated muscles from CR compared with AL rats.
Akt phosphorylation
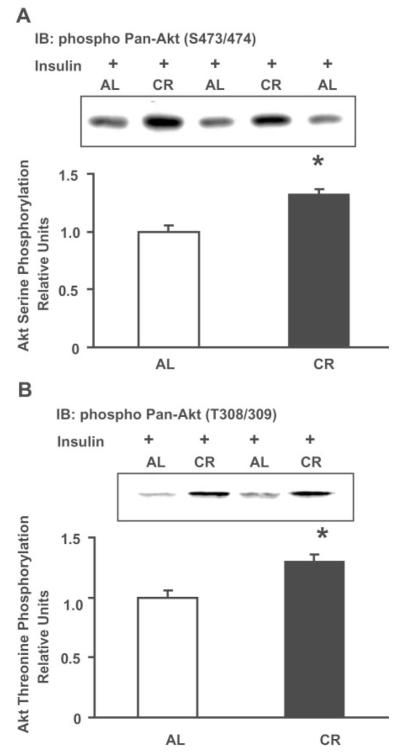
Phosphorylation of total Akt (all isoforms) at Ser473/474 or Thr308/309 was measured in epitrochlearis muscle homogenates from AL and CR rats by use of phosphoantibodies that recognize Akt1 and Akt2 (Pan-Akt Ser473/474 or Pan-Akt Thr308/309). Figure 1A shows that Akt serine phosphorylation was 32% (P < 0.05) greater in insulin-stimulated muscles from CR rats compared with muscles from AL rats. Similarly, Akt threonine phosphorylation of insulin-stimulated muscles was 30% (P < 0.05) greater for CR vs. AL (Fig. 1B). Basal Akt serine and threonine phosphorylation levels were not detectable in homogenates regardless of diet group (data not shown).
Fig. 1.
Total Akt serine and threonine phosphorylation. A: immunoblot (IB) analysis of serine phosphorylation in homogenates of insulin-stimulated epitrochlearis muscle after 20 days of ad libitum (AL) and calorie-restricted (CR) feeding (40 μg/lane). Phospho-pan-Akt (Ser473/474) antibody recognizes serine-phosphorylated Akt1 and Akt2. Data are means ± SE for 15 rats/group. B: immunoblot analysis of threonine phosphorylation in homogenates of insulin-stimulated epitrochlearis muscle (60 μg/lane). Phospho-pan-Akt (Thr308/309) antibody recognizes threonine-phosphorylated Akt1 and Akt2. Data are means ± SE for 8 rats/group. Data are relative to the average of AL values on each blot. Data were analyzed by t-test, with *P < 0.05, CR significantly different from AL. Representative immunoblots are shown.
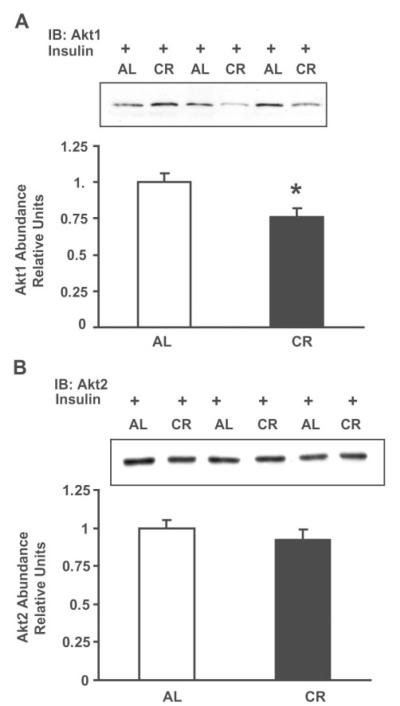
Isoform abundance
Akt1 abundance was 24% (P < 0.05) lower for CR compared with AL samples (Fig. 2A). In contrast, there was not a significant difference in Akt2 abundance for CR compared with AL samples (Fig. 2B).
Fig. 2.
Akt1 and Akt2 abundance. A: Akt1 abundance was measured by immunoblot assay using an Akt1-specific antibody in homogenates from insulin-stimulated epitrochlearis muscles (60 μg/lane). Data are means ± SE for 15 rats/group. B: Akt2 abundance was measured by immunoblot assay using an Akt2-specific antibody in homogenates from insulin-stimulated epitrochlearis muscle (25 μg/lane). Data are means ± SE for 8–9 rats/group. All data are relative to the average of AL values on each blot. Data were analyzed by t-test, with *P < 0.05, CR significantly different from AL. Representative immunoblots are shown.
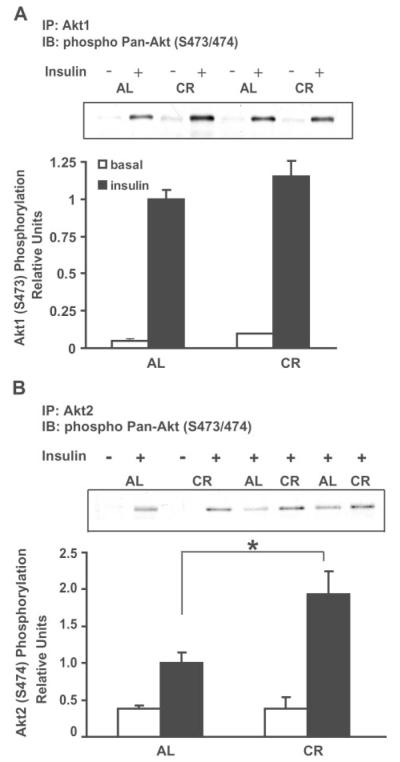
Phosphorylation of Akt1 and Akt2
There was no difference in Akt1 serine phosphorylation between AL and CR muscles for either basal or insulin-stimulated conditions (Fig. 3A). Akt2 serine phosphorylation was 90% greater (P < 0.01) in insulin-stimulated muscles of CR rats compared with AL rats (Fig. 3B). Basal Akt2 serine phosphorylation was not different between diet groups.
Fig. 3.
Serine phosphorylation of Akt1 and Akt2. Immunoprecipated (IP) Akt1 (200 μg; A) or immunoprecipated Akt2 (250 μg; B) from homogenates of epitrochlearis muscles, incubated without (open bars) or with (filled bars) 500 μU/ml insulin, was analyzed by immunoblot assay using phospho-pan-Akt (Ser473/474) antibody. Data are means ± SE for 4–6 rats/group. Data were analyzed by t-test, with *P < 0.05, CR significantly different from AL. Representative immunoblots are shown.
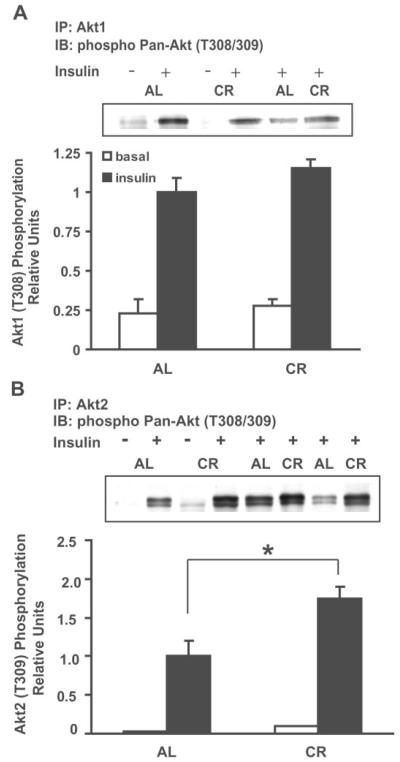
Akt1 threonine phosphorylation was not significantly different for AL compared with CR groups whether the muscles had been incubated under basal or insulin-stimulated conditions (Fig. 4A). Akt2 threonine phosphorylation was 75% greater (P < 0.05) in insulin-stimulated muscles from CR compared with AL controls. Akt2 threonine phosphorylation was not different between AL and CR groups for muscles incubated without insulin.
Fig. 4.
Threonine phosphorylation of Akt1 and Akt2. Immunoprecipated Akt1 (200 μg; A) or immunoprecipated Akt2 (250 μg; B) from homogenates of epitrochlearis muscles, incubated without (open bars) or with (filled bars) 500 μU/ml insulin, was analyzed by immunoblot assay with phospho-pan-Akt (Thr308/309) antibody. Data are means ± SE for 5–9 rats/group. Data were analyzed by t-test, with *P < 0.05, CR significantly different from AL. Representative immunoblots are shown.
It seemed possible that the decrease in Akt1 abundance with CR might have prevented a CR-induced increase in serine and threonine phosphorylation of Akt1. Therefore, we expressed the data as a ratio of Akt1 phosphorylation to Akt1 abundance for each sample to adjust for the decreased abundance with CR. Akt1 threonine phosphorylation for insulin-stimulated muscles was 50% greater with CR compared with AL (AL 1.0 ± 0.07, CR 1.5 ± 0.22; n = 8 per group; P < 0.05). We found a trend toward a similar effect on Akt1 serine phosphorylation (AL 1.0 ± 0.06, CR 1.47 ± 0.44; n = 4–5 per group; P = 0.26). Akt2 abundance was unchanged by diet; therefore, the relative difference between AL and CR groups for Akt2 phosphorylation was essentially the same whether or not it was adjusted for Akt2 abundance (data not shown).
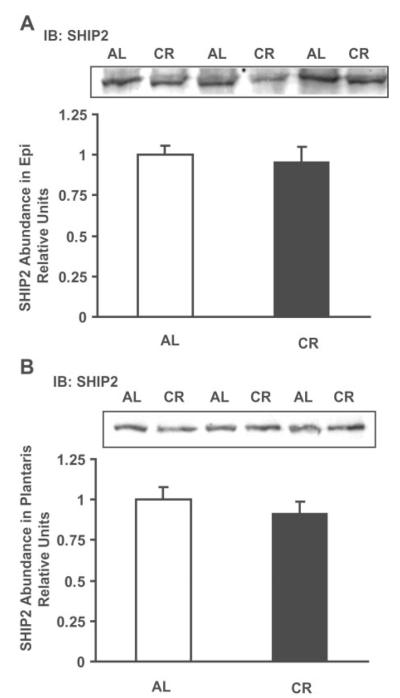
SHIP2 abundance
SHIP2 abundance was measured in homogenates from epitrochlearis muscle incubated with insulin (Fig. 5A) and from plantaris muscle frozen immediately after dissection (Fig. 5B). No difference in SHIP2 abundance was observed between AL and CR samples in either muscle.
Fig. 5.
SH2 domain-containing inositol phosphatase (SHIP2) abundance. SHIP2 abundance was measured by immunoblot assay (200 μg/lane) in homogenates from epitrochlearis (Epi) muscle (A) or plantaris muscle (B). Data are means ± SE for 8–9 rats/group. Data were analyzed by t-test, with *P < 0.05, CR significantly different from AL. Representative immunoblots are shown.
DISCUSSION
The most important new findings of this study are that 1) brief CR (20 days consuming 60% of AL intake) of rats increased serine and threonine phosphorylation of total Akt in insulin-stimulated skeletal muscle; 2) this increase in Akt phosphorylation is isoform specific such that Akt2 phosphorylation is markedly increased in the absence of significant change of Akt1 phosphorylation for insulin-stimulated muscles; 3) these isoform differences in phosphorylation are accompanied by reduced Akt1 protein abundance with no change in Akt2 levels; and 4) altered Akt2 phosphorylation is not attributable to reduced muscle content of inositol 5′-phosphatase SHIP2.
Brief CR leads to increased insulin sensitivity in isolated skeletal muscle (16, 18, 23), and the CR effect is mediated by increased GLUT4 translocation (17). Because enhanced glucose transport with CR is specific to the insulin-mediated pathway (17), we focused on elements of the insulin-signaling pathway. Insulin-stimulated glucose transport is dependent on PI 3-kinase activity (12, 38), but our previous results have shown no significant effect of CR on IRS-1, IRS-2, or phosphotyrosine-associated PI 3-kinase activity (16, 17, 19). These finding led us to hypothesize that CR will enhance insulin signaling by a post-PI 3-kinase mechanism, specifically through increased activation of Akt.
In support of that hypothesis, we report that, in insulin-stimulated muscles, there was an ~30% greater total Akt serine and threonine phosphorylation for CR compared with AL groups. This measurement was made on muscle homogenates with antibodies that recognize phosphorylated serine and threonine, respectively, on all Akt isoforms. The relative magnitude of the increase in total Akt phosphorylation corresponds roughly with the 25% greater glucose transport in insulin-treated muscles from CR compared with AL rats.
Recent studies provide good evidence that Akt1 and Akt2 have isoform-specific functions in cellular regulation that vary but are overlapping and that Akt2 may preferentially be involved in insulin-stimulated glucose metabolism. Akt2 has been shown to associate with GLUT4-containing vesicles (7) and appears to play a role in insulin-stimulated GLUT4 translocation (25) in adipocytes. Studies on transgenic mice lacking Akt1 or Akt2 provide compelling evidence for divergence in the roles of the Akt isoforms. Mice null for the Akt2 gene have insulin resistance measured at the intact organism and isolated skeletal muscle levels (13). Unlike Akt2-null animals, Akt1-null mice have normal glucose tolerance (14).
In this context, it is important that CR had an isoform-specific effect on insulin-stimulated Akt phosphorylation. Phosphorylation of Akt2, on both serine and threonine, was markedly enhanced in insulin-stimulated muscles from CR vs. AL rats. In contrast, Akt1 phosphorylation was not enhanced by CR. These findings suggest that Akt2 may be preferentially involved in enhancing insulin-stimulated glucose transport with CR.
How might CR-induced isoform specificity in phosphorylation be mediated? Perhaps it is related to the isoform-specific downregulation of Akt protein abundance observed: CR induced a significant reduction in Akt1 levels without any change in Akt2 abundance. If Akt1 and Akt2 compete for binding to a limited number of PIP3 sites, then the decline in Akt1 abundance could favor greater binding and phosphorylation of Akt2. Regardless of the mechanism, our observation that CR leads to enhanced Akt2 phosphorylation concomitant with improved insulin sensitivity is consistent with results from previous studies that indicate that Akt2 is important for insulin action.
Our data also provide evidence for a nonspecific isoform effect on Akt phosphorylation. Despite a 24% decrease in Akt1 abundance in CR muscle, there was no decline in Akt1 phosphorylation for CR compared with AL groups. Indeed, when Akt1 phosphorylation values are expressed relative to Akt1 abundance, there is an ~50% greater phosphorylation for CR compared with AL values in the insulin-stimulated muscles. An attractive possible mechanism that would promote Akt phosphorylation would be attenuated degradation of PIP3. The 5′ lipid phosphatase SHIP2 has been shown to negatively regulate insulin signaling and glucose transport by degradation of PI(3,4,5)P3 to PI(3,4)P2 (46). SHIP2 is abundantly expressed in insulin-sensitive cells (42), and decreased abundance of SHIP2 in mice heterozygous for a SHIP2 mutation leads to increased glucose tolerance and insulin sensitivity (15). In diabetic db/db mice, SHIP2 protein levels are elevated, and the activity of Akt is severely reduced in skeletal muscle (26). Therefore, we hypothesized that decreased SHIP2 expression might lead to the increased Akt phosphorylation observed in CR skeletal muscle. However, we found no difference in SHIP2 abundance in muscles from CR vs. AL rats. It is possible that changes in SHIP2 expression occur with longer CR or that SHIP2 activity is altered rather than expression.
Increased Akt phosphorylation in the absence enhanced PI 3-kinase activity observed in our previous studies (16, 17, 19) seems to be a paradox, but an apparent dissociation between PI 3-kinase and Akt has been observed in several studies (31, 34, 35, 37). We saw an increase in Akt phosphorylation measured in lysates from intact muscles but no measurable change in PI 3-kinase activity by conventional in vitro assay (16) in which IRS-1, IRS-2, or tyrosine-phosphorylated proteins are immunoprecipitated by the appropriate antibodies from homogenized muscle, isolating the IRS-PI 3-kinase complex from other cell components; substrate is added and accumulation of lipid product occurs. It is not unlikely that in the intact muscle the accumulation of lipid products may depend on the interaction of IRS-PI 3-kinase with the internal milieu of the intact cells. This interaction is disrupted under conditions of the assay, e.g., homogenization and immunoprecipitation would isolate IRS-PI 3-kinase from other elements in the intact cell.
Regardless of the mechanism for the enhanced Akt2 phosphorylation in insulin-stimulated muscles of CR compared with AL rats, elucidating the functional significance will be important. One approach to assessing whether Akt2 is essential for CR-induced increase in insulin sensitivity would be to study transgenic mice that are Akt2 null (13). Previous work has shown that 20 days of CR improves insulin sensitivity in mice (22); therefore, we would expect no improvement in glucose uptake in Akt2-null mice, if Akt2 is essential for the CR-mediated improvement in insulin sensitivity.
In conclusion, we have identified alterations in insulin-signaling proteins after brief CR in rat skeletal muscle that are associated with CR-enhanced insulin sensitivity. Total Akt serine and threonine phosphorylation were greater in insulin-stimulated muscles from CR compared with AL rats. These changes were due to an enhancement of Akt2 phosphorylation in CR vs. AL muscles, with no diet-related difference in Akt1 phosphorylation. Akt1 abundance was significantly lower in muscles from CR compared with AL rats. We hypothesize that this decrement in Akt1 played a role in greater membrane accessibility and phosphorylation of Akt2. The enhanced Akt phosphorylation in insulin-stimulated muscles could not be attributed to changes in SHIP2 abundance. It will be important in future studies to determine whether the substantial CR effect on Akt2 phosphorylation is essential for improved insulin sensitivity.
Acknowledgments
We thank Dr. Morris Birnbaum, at the University of Pennsylvania, for his generous gift of Akt2 antibody.
Footnotes
DISCLOSURES: This study was supported by National Institute on Aging Grant RO1 AG-10026.
REFERENCES
- 1.Andjelkovic M, Alessi DR, Meier R, Fernandez A, Lamb NJ, Frech M, Cron P, Cohen P, Lucocq JM, Hemmings BA. Role of translocation in the activation and function of protein kinase B. J Biol Chem. 1997;272:31515–31524. doi: 10.1074/jbc.272.50.31515. [DOI] [PubMed] [Google Scholar]
- 2.Arciero PJ, Vukovich MD, Holloszy JO, Racette SB, Kohrt WM. Comparison of short-term diet and exercise on insulin action in individuals with abnormal glucose tolerance. J Appl Physiol. 1999;86:1930–1935. doi: 10.1152/jappl.1999.86.6.1930. [DOI] [PubMed] [Google Scholar]
- 3.Balage M, Grizard J, Sornet C, Simon J, Dardevet D, Manin M. Insulin binding and receptor tyrosine kinase activity in rat liver and skeletal muscle: effect of starvation. Metabolism. 1990;39:366–373. doi: 10.1016/0026-0495(90)90250-g. [DOI] [PubMed] [Google Scholar]
- 4.Blero D, De Smedt F, Pesesse X, Paternotte N, Moreau C, Payrastre B, Erneux C. The SH2 domain containing inositol 5-phosphatase SHIP2 controls phosphatidylinositol 3,4,5-trisphosphate levels in CHO-IR cells stimulated by insulin. Biochem Biophys Res Commun. 2001;282:839–843. doi: 10.1006/bbrc.2001.4639. [DOI] [PubMed] [Google Scholar]
- 5.Brodbeck D, Cron P, Hemmings BA. A human protein kinase Bγ with regulatory phosphorylation sites in the activation loop and in the C-terminal hydrophobic domain. J Biol Chem. 1999;274:9133–9136. doi: 10.1074/jbc.274.14.9133. [DOI] [PubMed] [Google Scholar]
- 6.Burgering BM, Coffer PJ. Protein kinase B (c-Akt) in phosphatidylinositol-3-OH kinase signal transduction. Nature. 1995;376:599–602. doi: 10.1038/376599a0. [DOI] [PubMed] [Google Scholar]
- 7.Calera MR, Martinez C, Liu H, Jack AK, Birnbaum MJ, Pilch PF. Insulin increases the association of Akt-2 with Glut4-containing vesicles. J Biol Chem. 1998;273:7201–7204. doi: 10.1074/jbc.273.13.7201. [DOI] [PubMed] [Google Scholar]
- 8.Cartee GD, Bohn EE. Growth hormone reduces glucose transport but not GLUT-1 or GLUT-4 in adult and old rats. Am J Physiol Endocrinol Metab. 1995;268:E902–E909. doi: 10.1152/ajpendo.1995.268.5.E902. [DOI] [PubMed] [Google Scholar]
- 9.Cartee GD, Dean DJ. Glucose transport with brief dietary restriction: heterogenous responses in muscles. Am J Physiol Endocrinol Metab. 1994;266:E946–E952. doi: 10.1152/ajpendo.1994.266.6.E946. [DOI] [PubMed] [Google Scholar]
- 10.Cartee GD, Kietzke EW, Briggs-Tung C. Adaptation of muscle glucose transport with caloric restriction in adult, middle-aged, and old rats. Am J Physiol Regul Integr Comp Physiol. 1994;266:R1443–R1447. doi: 10.1152/ajpregu.1994.266.5.R1443. [DOI] [PubMed] [Google Scholar]
- 11.Cecchin F, Ittoop O, Sinha MK, Caro JF. Insulin resistance in uremia: insulin receptor kinase activity in liver and muscle from chronic uremic rats. Am J Physiol Endocrinol Metab. 1988;254:E394–E401. doi: 10.1152/ajpendo.1988.254.4.E394. [DOI] [PubMed] [Google Scholar]
- 12.Cheatham B, Vlahos CJ, Cheatham L, Wang L, Blenis J, Kahn CR. Phosphatidylinositol 3-kinase activation is required for insulin stimulation of pp70 S6 kinase, DNA synthesis, and glucose transporter translocation. Mol Cell Biol. 1994;14:4902–4911. doi: 10.1128/mcb.14.7.4902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cho H, Mu J, Kim JK, Thorvaldsen JL, Chu Q, Crenshaw EB, Kaestner KH, III, Bartolomei MS, Shulman GI, Birnbaum MJ. Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKBβ) Science. 2001;292:1728–1731. doi: 10.1126/science.292.5522.1728. [DOI] [PubMed] [Google Scholar]
- 14.Cho H, Thorvaldsen JL, Chu Q, Feng F, Birnbaum MJ. Akt1/PKBα is required for normal growth but dispensable for maintenance of glucose homeostasis in mice. J Biol Chem. 2001;276:38349–38352. doi: 10.1074/jbc.C100462200. [DOI] [PubMed] [Google Scholar]
- 15.Clement S, Krause U, Desmedt F, Tanti JF, Behrends J, Pesesse X, Sasaki T, Penninger J, Doherty M, Malaisse W, Dumont JE, Marchand-Brustel Y, Erneux C, Hue L, Schurmans S. The lipid phosphatase SHIP2 controls insulin sensitivity. Nature. 2001;409:92–97. doi: 10.1038/35051094. [DOI] [PubMed] [Google Scholar]
- 16.Davidson RT, Arias EB, Cartee GD. Calorie restriction increases muscle insulin action but not IRS-1-, IRS- 2-, or phosphotyrosine-PI 3-kinase. Am J Physiol Endocrinol Metab. 2002;282:E270–E276. doi: 10.1152/ajpendo.00232.2001. [DOI] [PubMed] [Google Scholar]
- 17.Dean DJ, Brozinick JT, Jr, Cushman SW, Cartee GD. Calorie restriction increases cell surface GLUT-4 in insulin-stimulated skeletal muscle. Am J Physiol Endocrinol Metab. 1998;275:E957–E964. doi: 10.1152/ajpendo.1998.275.6.E957. [DOI] [PubMed] [Google Scholar]
- 18.Dean DJ, Cartee GD. Brief dietary restriction increases skeletal muscle glucose transport in old Fischer 344 rats. J Gerontol A Biol Sci Med Sci. 1996;51:B208–B213. doi: 10.1093/gerona/51a.3.b208. [DOI] [PubMed] [Google Scholar]
- 19.Dean DJ, Cartee GD. Calorie restriction increases insulin-stimulated tyrosine phosphorylation of insulin receptor and insulin receptor substrate-1 in rat skeletal muscle. Acta Physiol Scand. 2000;169:133–139. doi: 10.1046/j.1365-201x.2000.00723.x. [DOI] [PubMed] [Google Scholar]
- 20.Dean DJ, Gazdag AC, Wetter TJ, Cartee GD. Comparison of the effects of 20 days and 15 months of calorie restriction on male Fischer 344 rats. Aging (Milano) 1998;10:303–307. doi: 10.1007/BF03339792. [DOI] [PubMed] [Google Scholar]
- 21.DeFronzo RA, Binder C, Wahren J, Felig P, Ferrannini E, Faber OK. Sensitivity of insulin secretion to feedback inhibition by hyperinsulinaemia. Acta Endocrinol(Copenh) 1981;98:81–86. doi: 10.1530/acta.0.0980081. [DOI] [PubMed] [Google Scholar]
- 22.Gazdag AC, Dumke CL, Kahn CR, Cartee GD. Calorie restriction increases insulin-stimulated glucose transport in skeletal muscle from IRS-1 knockout mice. Diabetes. 1999;48:1930–1936. doi: 10.2337/diabetes.48.10.1930. [DOI] [PubMed] [Google Scholar]
- 23.Gazdag AC, Tucker MZ, Turcotte LP, Dean DJ, Cartee GD. Effect of extracellular palmitate on 2-deoxy-D-glucose uptake in muscle from ad libitum fed and calorie restricted rats. Biochem Biophys Res Commun. 1998;252:733–737. doi: 10.1006/bbrc.1998.9713. [DOI] [PubMed] [Google Scholar]
- 24.Harris SB, Gunion MW, Rosenthal MJ, Walford RL. Serum glucose, glucose tolerance, corticosterone and free fatty acids during aging in energy restricted mice. Mech Ageing Dev. 1994;73:209–221. doi: 10.1016/0047-6374(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 25.Hill MM, Clark SF, Tucker DF, Birnbaum MJ, James DE, Macaulay SL. A role for protein kinase Bβ/Akt2 in insulin-stimulated GLUT4 translocation in adipocytes. Mol Cell Biol. 1999;19:7771–7781. doi: 10.1128/mcb.19.11.7771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hori H, Sasaoka T, Ishihara H, Wada T, Murakami S, Ishiki M, Kobayashi M. Association of SH2-containing inositol phosphatase 2 with the insulin resistance of diabetic db/db mice. Diabetes. 2002;51:2387–2394. doi: 10.2337/diabetes.51.8.2387. [DOI] [PubMed] [Google Scholar]
- 27.Katome T, Obata T, Matsushima R, Masuyama N, Cantley LC, Gotoh Y, Kishi K, Shiota H, Ebina Y. Use of RNA-interference-mediated gene silencing and adenoviral overexpression to elucidate the roles of AKT/PKB-isoforms in insulin actions. J Biol Chem. 2003 May 6; doi: 10.1074/jbc.M302094200. [E pub ahead of print] 10.1074/jbc.M302094200. [DOI] [PubMed] [Google Scholar]
- 28.Kemnitz JW, Roecker EB, Weindruch R, Elson DF, Baum ST, Bergman RN. Dietary restriction increases insulin sensitivity and lowers blood glucose in rhesus monkeys. Am J Physiol Endocrinol Metab. 1994;266:E540–E547. doi: 10.1152/ajpendo.1994.266.4.E540. [DOI] [PubMed] [Google Scholar]
- 29.Kitamura T, Ogawa W, Sakaue H, Hino Y, Kuroda S, Takata M, Matsumoto M, Maeda T, Konishi H, Kikkawa U, Kasuga M. Requirement for activation of the serine-threonine kinase Akt (protein kinase B) in insulin stimulation of protein synthesis but not of glucose transport. Mol Cell Biol. 1998;18:3708–3717. doi: 10.1128/mcb.18.7.3708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kohn AD, Summers SA, Birnbaum MJ, Roth RA. Expression of a constitutively active Akt Ser/Thr kinase in 3T3—L1 adipocytes stimulates glucose uptake and glucose transporter 4 translocation. J Biol Chem. 1996;271:31372–31378. doi: 10.1074/jbc.271.49.31372. [DOI] [PubMed] [Google Scholar]
- 31.Kurowski TG, Lin Y, Luo Z, Tsichlis PN, Buse MG, Heydrick SJ, Ruderman NB. Hyperglycemia inhibits insulin activation of Akt/protein kinase B but not phosphatidylinositol 3-kinase in rat skeletal muscle. Diabetes. 1999;48:658–663. doi: 10.2337/diabetes.48.3.658. [DOI] [PubMed] [Google Scholar]
- 32.Marion E, Kaisaki PJ, Pouillon V, Gueydan C, Levy JC, Bodson A, Krzentowski G, Daubresse JC, Mockel J, Behrends J, Servais G, Szpirer C, Kruys V, Gauguier D, Schurmans S. The gene INPPL1, encoding the lipid phosphatase SHIP2, is a candidate for type 2 diabetes in rat and man. Diabetes. 2002;51:2012–2017. doi: 10.2337/diabetes.51.7.2012. [DOI] [PubMed] [Google Scholar]
- 33.Masure S, Haefner B, Wesselink JJ, Hoefnagel E, Mortier E, Verhasselt P, Tuytelaars A, Gordon R, Richardson A. Molecular cloning, expression and characterization of the human serine/threonine kinase Akt-3. Eur J Biochem. 1999;265:353–360. doi: 10.1046/j.1432-1327.1999.00774.x. [DOI] [PubMed] [Google Scholar]
- 34.Mauvais-Jarvis F, Ueki K, Fruman DA, Hirshman MF, Sakamoto K, Goodyear LJ, Iannacone M, Accili D, Cantley LC, Kahn CR. Reduced expression of the murine p85α subunit of phosphoinositide 3-kinase improves insulin signaling and ameliorates diabetes. J Clin Invest. 2002;109:141–149. doi: 10.1172/JCI13305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nadler ST, Stoehr JP, Rabaglia ME, Schueler KL, Birnbaum MJ, Attie AD. Normal Akt/PKB with reduced PI3K activation in insulin-resistant mice. Am J Physiol Endocrinol Metab. 2001;281:E1249–E1254. doi: 10.1152/ajpendo.2001.281.6.E1249. [DOI] [PubMed] [Google Scholar]
- 36.Nakatani K, Sakaue H, Thompson DA, Weigel RJ, Roth RA. Identification of a human Akt3 (protein kinase B γ) which contains the regulatory serine phosphorylation site. Biochem Biophys Res Commun. 1999;257:906–910. doi: 10.1006/bbrc.1999.0559. [DOI] [PubMed] [Google Scholar]
- 37.Nelson BA, Robinson KA, Buse MG. Defective Akt activation is associated with glucose- but not glucosamine-induced insulin resistance. Am J Physiol Endocrinol Metab. 2002;282:E497–E506. doi: 10.1152/ajpendo.00438.2001. [DOI] [PubMed] [Google Scholar]
- 38.Pessin JE, Saltiel AR. Signaling pathways in insulin action: molecular targets of insulin resistance. J Clin Invest. 2000;106:165–169. doi: 10.1172/JCI10582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reaven E, Wright D, Mondon CE, Solomon R, Ho H, Reaven GM. Effect of age and diet on insulin secretion and insulin action in the rat. Diabetes. 1983;32:175–180. doi: 10.2337/diab.32.2.175. [DOI] [PubMed] [Google Scholar]
- 40.Sano H, Kane S, Sano E, Miinea CP, Asara JM, Lane WS, Garner CW, Lienhard GE. Insulin-stimulated phosphorylation of a Rab GTPase-activating protein regulates GLUT4 translocation. J Biol Chem. 2003;278:14599–14602. doi: 10.1074/jbc.C300063200. [DOI] [PubMed] [Google Scholar]
- 41.Scheid MP, Marignani PA, Woodgett JR. Multiple phosphoinositide 3-kinase-dependent steps in activation of protein kinase B. Mol Cell Biol. 2002;22:6247–6260. doi: 10.1128/MCB.22.17.6247-6260.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schurmans S, Carrio R, Behrends J, Pouillon V, Merino J, Clement S. The mouse SHIP2 (Inppl1) gene: complementary DNA, genomic structure, promoter analysis, and gene expression in the embryo and adult mouse. Genomics. 1999;62:260–271. doi: 10.1006/geno.1999.5995. [DOI] [PubMed] [Google Scholar]
- 43.Shepherd PR, Withers DJ, Siddle K. Phosphoinositide 3-kinase: the key switch mechanism in insulin signalling. Biochem J. 1998;333:471–490. doi: 10.1042/bj3330471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ueki K, Yamamoto-Honda R, Kaburagi Y, Yamauchi T, Tobe K, Burgering BM, Coffer PJ, Komuro I, Akanuma Y, Yazaki Y, Kadowaki T. Potential role of protein kinase B in insulin-induced glucose transport, glycogen synthesis, and protein synthesis. J Biol Chem. 1998;273:5315–5322. doi: 10.1074/jbc.273.9.5315. [DOI] [PubMed] [Google Scholar]
- 45.Vanhaesebroeck B, Alessi DR. The PI3K-PDK1 connection: more than just a road to PKB. Biochem J. 2000;346:561–576. [PMC free article] [PubMed] [Google Scholar]
- 46.Vollenweider P, Clodi M, Martin SS, Imamura T, Kavanaugh WM, Olefsky JM. An SH2 domain-containing 5′ inositolphosphatase inhibits insulin-induced GLUT4 translocation and growth factor-induced actin filament rearrangement. Mol Cell Biol. 1999;19:1081–1091. doi: 10.1128/mcb.19.2.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Walker KS, Deak M, Paterson A, Hudson K, Cohen P, Alessi DR. Activation of protein kinase Bβ and γ isoforms by insulin in vivo and by 3-phosphoinositide-dependent protein kinase-1 in vitro: comparison with protein kinase Bα. Biochem J. 1998;331:299–308. doi: 10.1042/bj3310299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ziel FH, Venkatesan N, Davidson MB. Glucose transport is rate limiting for skeletal muscle glucose metabolism in normal and STZ-induced diabetic rats. Diabetes. 1988;37:885–890. doi: 10.2337/diab.37.7.885. [DOI] [PubMed] [Google Scholar]