Abstract
We examined the feasibility, acceptability, and therapeutic efficacy of a culturally adapted cognitive–behavior therapy (CBT) for twelve Vietnamese refugees with treatment-resistant posttraumatic stress disorder (PTSD) and panic attacks. These patients were treated in two separate cohorts of six with staggered onset of treatment. Repeated measures Group × Time ANOVAs and between-group comparisons indicated significant improvements, with large effect sizes (Cohen’s d) for all outcome measures: Harvard Trauma Questionnaire (HTQ; d = 2.5); Anxiety Sensitivity Index (ASI; d = 4.3); Hopkins Symptom Checklist-25 (HSCL-25), anxiety subscale (d = 2.2); and Hopkins Symptom Checklist-25, depression subscale (d = 2.0) scores. Likewise, the severity of (culturally related) headache-and orthostasis-cued panic attacks improved significantly across treatment
Keywords: posttraumatic stress disorder, panic attacks, cognitive, behavior therapy, Vietnamese refugees
Vietnamese refugees are a highly traumatized population, having endured years of civil war followed by multiple subsequent stressors (Mollica et al., 1998). Post-traumatic stress disorder (70–90%; Mollica et al., 1998) and panic disorder (50%; Hinton et al., 2001) are especially prevalent among Vietnamese refugees attending psychiatric clinics.
Vietnamese refugees frequently experience panic attacks cued by either headache sensations (headache-associated panic) or dizziness upon standing (orthostasis-associated panic; Hinton et al., 2001; Hinton, Pham, Chau, Tran, & Hinton, 2003). A headache often gives rise to catastrophic cognitions (e.g., that “over-stretched nerve fibers” will rip or that cerebral blood vessels may burst) as does dizziness upon standing (e.g., fears of increased blood pressure and “heart weakness”; Hinton et al., 2001, 2003). Also, headache and orthostatic symptoms may cause a Vietnamese refugee to recall memories encoded by similar sensations experienced during traumatic events such as overwork, starvation, beatings (e.g., pistol whipping), illness (e.g., malaria or typhoid), and the perilous sea crossing in a small boat from Vietnam during the escape journey (Hinton et al., 2001, 2003; on similar panic attack subtypes in Cambodian refugees produced by related mechanisms, see Hinton et al., 2004; Hinton, Ba, Peou, & Um, 2000).
A previous study by our group demonstrated the efficacy of cognitive–behavior therapy (CBT) focusing on posttraumatic stress disorder (PTSD) and comorbid panic attacks in the treatment of Cambodian refugees (Otto et al., 2003). We hypothesized that CBT focusing on PTSD and comorbid panic attacks would also be efficacious for Vietnamese refugees.
Method
Participants
Participants (all of whom were practicing Buddhists) were from two community-based outpatient clinics that provided specialized services to non-English speaking Cambodian and Vietnamese refugees. We offered CBT treatment to Vietnamese patients who were considered most treatment resistant. All 12 Vietnamese participants met PTSD criteria (as assessed by the SCID module for PTSD; First, Spitzer, & Gibbon, 1995) despite at least 1 year of an adequate dose of a selective serotonin reuptake inhibitor (SSRI) and supportive counseling. The patients were randomly assigned to two cohorts of 6 each, one being immediate (Group 1) and the other delayed CBT treatment (Group 2). Only 1 patient in each group did not have panic episodes linked to headache, and only 1 patient in each group did not have panic linked to orthostatic cues. In each of the two groups, 3 patients were men; all males were ex-political detainees. (Ex-political detainees are former Southern Vietnamese military, police, or political officials who were imprisoned by the Northern Vietnamese.) In our study, not one of the women was an ex-political detainee. All patients continued current medications (in most cases, a combination of three medications: an SSRI, a benzodiazepine, and gabapentin). Permission for use of the clinical outcome assessments for this research report was provided by the clinic’s Institutional Review Board.
Measures
The Harvard Trauma Questionnaire (HTQ), which has been translated and validated for the Vietnamese population, assesses 16 DSM-III-R-related posttraumatic stress disorder items on 1–4 Likert-type scales (Mollica et al., 1992). A score of 2.5 or more indicates the presence of PTSD (for sensitivity and specificity data, see Mollica et al., 1992). The Hopkins Symptom Checklist-25 (HSCL-25), which has been translated and validated for the Vietnamese population, contains two scales—an anxiety scale (10 items) and a depression scale (15 items)—each item being rated on a 1–4 Likert-type scale. A score of 1.75 on either subscale suggests significant psychopathology (Mollica, et al., 1990). The 16-item Anxiety Sensitivity Index (ASI), each item being rated on a 0–4 Likert-type scale, assesses fear of anxiety symptoms (Reiss & McNally, 1985). ASI scores higher than 30 suggest a strong predisposition to panic in reaction to anxiety-related symptoms (e.g., to dizziness or palpitations). As assessed at a 1-week interval for 20 patients, the Vietnamese version of the ASI demonstrates good test–retest reliability (r = .89). The Headache Panic Attack Severity Scale (HPASS) and the Orthostatic Panic Attack Severity Scale (OPASS) rate panic severity on three dimensions (frequency, degree of distress, and duration), each of the three dimensions being rated on a 0–4 Likert-type scale. As assessed with 20 patients, the HPASS and OPASS demonstrated good interrater reliability (r = .93 and .95), and at a 2-week interval, good test–retest reliability (r = .84 and .88)
Procedure
The participants completed the HTQ, ASI, and HSCL at three time points: (a) at pretreatment (first assessment); (b) after Group 1 had undergone 11 sessions of CBT (second assessment); and (c) after Group 2 had undergone 11 sessions of CBT (third assessment). We assessed the severity of headache- and orthostasis-associated panic every 2 weeks.
Treatment
The first author led the CBT sessions. Vietnamese social workers and staff provided translation and cultural consultation. Individual CBT was offered across 11 weekly sessions. During CBT, we stressed eight core elements:
providing information about the nature of PTSD and panic disorder (Falsetti & Resnick, 2000; Resick & Schnicke, 1993) such as how trauma reminders and catastrophic cognitions generate panic attacks;
training in muscle relaxation and diaphragmatic breathing procedures, including the use of applied relaxation techniques (Öst & Westling, 1995);
instruction in a culturally appropriate visualization—a lotus bloom that spins in the wind at the end of a stem (an image encoding key Asian cultural values of flexibility)—and having the patient perform analogous rotational movements at the neck after each relaxation of the neck and head musculature (these rotational movements also serve as an introduction to dizziness interoceptive exercises; cf. Foa & Rothbaum, 1998);
framing relaxation techniques as a form of mindfulness (Borkovec, 2002), that is, as an attentive focusing upon specific sensory modalities (e.g., muscular tension and the kinesthetics of breathing);
cognitive restructuring of fear networks, especially trauma memories and catastrophic misinterpretations of somatic sensations (including culture-related fears; cf. Foa & Rothbaum, 1998; Resick & Schnicke, 1993);
conducting interoceptive exposure (including re-association to positive images) to anxiety-related sensations to treat panic attacks generated by catastrophic cognitions, trauma associations, and interoceptive conditioning to those sensations (Falsetti & Resnick, 2000; Hinton et al., 2004; Otto, Penava, Pollack, & Smoller, 1996);
providing an emotional processing protocol (Foa & Rothbaum, 1998; Rachman, 1980) to utilize during times of trauma recall (e.g., flashbacks), the protocol bringing about a shift from an attitude of pained acceptance to one of mindfulness (i.e., multisensorial awareness of the present moment); and
exploring headache and orthostatic panic, as in investigating firing sequences—e.g., the sensations, activities, and thoughts that initiate the sequence leading to panic—and associated catastrophic cognitions and trauma associations (see Hinton et al., 2001, 2004; cf. Falsetti & Resnick, 2000).
Results
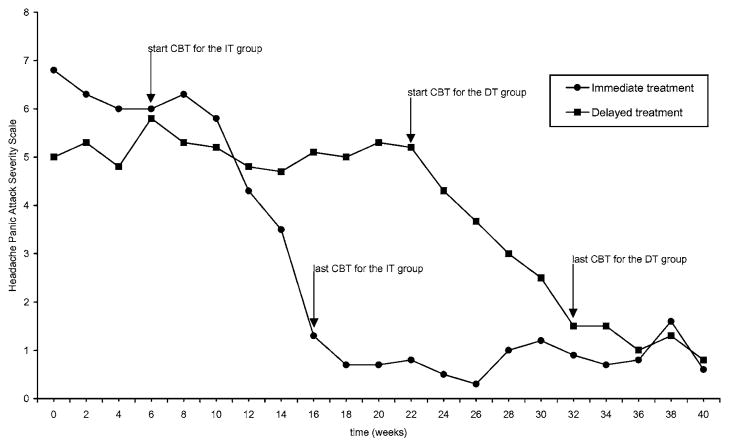
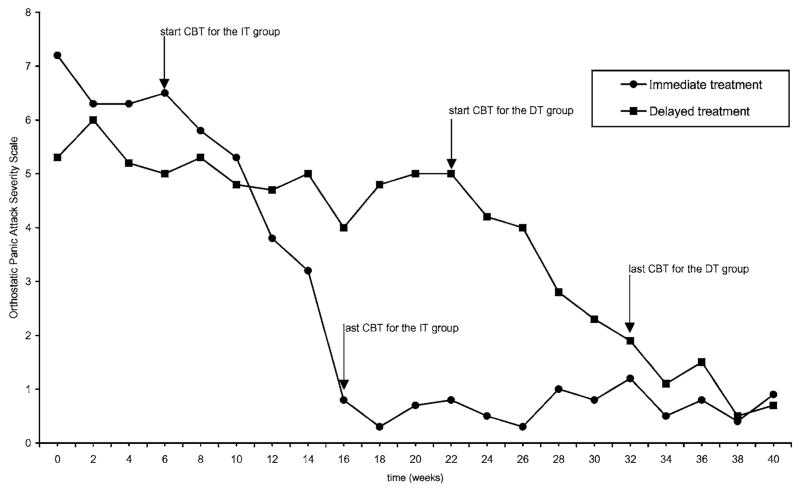
Table 1 provides symptom scores for the three assessments. Figures 1 and 2 give the HPASS and OPASS as assessed every 2 weeks. We computed between-group effect sizes (d = Meanwaitlist − MeanCBT/SDpooled) to illustrate the magnitude of treatment benefits relative to other studies (Otto et al., 1996). We also conducted 2 (initial waitlist vs. initial treatment) × 3 (first, second, and third assessments) analyses of variance on each of the outcome variables.
Table 1.
Psychiatric Symptoms As a Function of Treatment and Time of Assessment
| First assessment M (SD) | Second assessment M (SD) | Third assessment M (SD) | Between-group effect size, first vs. second assessment, Cohen’s d | |
|---|---|---|---|---|
| HTQ | ||||
| Immediate treatment | 3.3(0.4) | 1.7(0.5) | 1.8(0.7) | 2.5 |
| Delayed treatment | 3.1(0.7) | 3.3(0.8) | 2.0(0.6) | |
| ASI | ||||
| Immediate treatment | 43.5(9.1) | 18.5(6.4) | 21.0(8.0) | 4.3 |
| Delayed treatment | 38.0(7.4) | 47.6(7.2) | 20.2(4.9) | |
| HSCL-anxiety | ||||
| Immediate treatment | 3.5(0.5) | 2.2(0.5) | 1.8(0.6) | 2.2 |
| Delayed treatment | 3.3(0.6) | 3.2(0.4) | 2.1(0.4) | |
| HSCL-depression | ||||
| Immediate treatment | 3.1(0.7) | 2.1(0.5) | 1.6(0.6) | 2.0 |
| Delayed treatment | 3.3(0.9) | 3.2(0.6) | 1.9(0.4) | |
| HPASS | ||||
| Immediate treatment | 6.0(3.3) | 0.9(0.8) | 0.7(0.9) | 2.3 |
| Delayed treatment | 5.4(2.9) | 5.3(3.1) | 1.3(1.4) | |
| OPASS | ||||
| Immediate treatment | 6.4(3.4) | 0.8(0.7) | 0.6(0.8) | 2.2 |
| Delayed treatment | 5.1(2.7) | 5.0(3.1) | 1.2(1.5) | |
Note. N = 12. To obtain a headache and an orthostatic panic score, for the first assessment, we totaled and then averaged the panic attack severity scale score for Weeks 4 and 6; for the second assessment, Weeks 18 and 20; and for the third assessment Weeks 34 and 36. HTQ = Harvard Trauma Questionnaire; ASI = Anxiety Sensitivity Index; HSCL = Hopkins Symptom Checklist; HPASS = Headache Panic Attack Severity Scale; OPASS = Orthostatic Panic Attack Severity Scale.
Fig. 1.
Improvement of headache-associated panic in the immediate treatment (IT) group and the delayed treatment (DT) group as a function of cognitive–behavior therapy (CBT) and time.
Fig. 2.
Improvement of orthostatic-associated panic in the immediate treatment (IT) group and the delayed treatment (DT) group as a function of cognitive–behavior therapy (CBT) and time.
The overall interaction was significant for each of the outcome variables: PTSD, F (2, 10) = 8.0, p < .01; ASI, F (2, 10) = 34.9, p < .001; HSCL-anxiety, F (2, 10) = 7.3, p < .001; HSCL-depression, F (2, 10) = 5.7, p < .05; HPASS, F (2, 10) = 8.2, p < .01; and OPASS, F (2, 10) = 8.7, p < .01. As post hoc tests, we broke down the 2 × 3 interactions into separate 2 (intervention condition) × 2 (time point) interactions. First, we compared the first and second assessment points by condition. The interaction term for all of the outcome measures was significant, demonstrating greater improvement from Assessment 1 to Assessment 2 in the initial CBT group (Group 1) as compared to the delayed CBT group (Group 2): PTSD, F (1, 11) = 12.9, p < .01; ASI, F (1, 11) = 34.0, p < .001; HSCL-anxiety, F (1, 11) = 12.6, p < .01; HSCL-depression, F (1, 11) = 12.3, p < .01; HPASS, F (1, 11) = 14.7, p < .01; and OPASS, F (1, 11) = 14.7, p < .01. To examine whether the delayed CBT group (Group 2) had similar improvements across treatment after both groups received treatment, we performed 2 × 2 ANOVAs to compare Assessment 1 to Assessment 3. For all outcome measures, the interaction term was not significant (p > .05). However, from Assessment 1 to Assessment 3, significant main effects for time occurred for all outcome measures.
Discussion
In this small study of traumatized Vietnamese refugees, a culturally adapted CBT treatment focusing on PTSD and comorbid panic attacks was well accepted and efficacious. Several limitations of this study should be mentioned. The same individual provided all treatment; therefore, a “therapist effect” rather than a “treatment effect” may account for the observed improvements. Larger and better powered studies should investigate the use of this approach with different therapists. We cannot determine whether this combined treatment (and our culture-related modifications of CBT) would be more efficacious than other current treatment components that have been evaluated. Other packages of CBT (e.g., Cognitive-Processing Therapy; Resick, Nishith, Weaver, Astin, & Feuer, 2002; Multiple Channel Exposure Therapy; Falsetti & Resnick, 2000; or Prolonged Exposure; Foa et al., 1999) may have resulted in a similar degree of benefit. All patients in the present study were taking medication. Future studies should consider medication dosage both as an outcome measure and as a possible confounding variable.
References
- Borkovec TD. Life in the future versus life in the present. Clinical Psychology: Science and Practice. 2002;9:76–80. [Google Scholar]
- Falsetti SA, Resnick HS. Cognitive–behavioral treatment for PTSD with panic attacks. Journal of Contemporary Psychotherapy. 2000;30:163–179. [Google Scholar]
- First MB, Spitzer RL, Gibbon M. Structured clinical interview for DSM-IVAxis I disorders. New York: New York State Psychiatric Institute; 1995. [Google Scholar]
- Foa EB, Dancu CV, Hembree E, Jaycox HH, Meadows EA, Street P. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape. New York: Guilford; 1998. [Google Scholar]
- Hinton DE, Ba P, Peou S, Um K. Panic disorder among Cambodian refugees attending a psychiatric clinic: Prevalence and subtypes. General Hospital Psychiatry. 2000;22:437–444. doi: 10.1016/s0163-8343(00)00102-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton DE, Chau H, Nguyen L, Nguyen M, Pham T, Quinn S, et al. Panic disorder among Vietnamese refugees attending a psychiatric clinic: Prevalence and subtypes. General Hospital Psychiatry. 2001;23:337–344. doi: 10.1016/s0163-8343(01)00163-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton DE, Pham T, Chau H, Tran M, Hinton SD. “Hit by the wind” and temperature-shift panic among Vietnamese refugees. Transcultural Psychiatry. 2003;40:342–376. doi: 10.1177/13634615030403003. [DOI] [PubMed] [Google Scholar]
- Hinton DE, Pich V, So V, Pollack MH, Pitman RK, Orr SP. The psychophysiology of orthostatic panic in Cambodian refugees attending a psychiatric clinic. Journal of Psychopathology and Behavioral Assessement. 2004;26:1–13. [Google Scholar]
- Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire. Journal of Nervous and Mental Disease. 1992;180:111–116. [PubMed] [Google Scholar]
- Mollica RF, Grace W, Lavelle J, Truong T, Svang T, Yang T. Assessing symptom change in Southeast Asian refugee survivors of mass violence and torture. American Journal of Psychiatry. 1990;147:83–88. doi: 10.1176/ajp.147.1.83. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Mcinnes K, Pham T, Smith F, Mary C, Murphy E, et al. The dose–effect relationship between torture and psychiatric symptoms in Vietnamese ex-political detainees and a comparison group. Journal of Nervous and Mental Disease. 1998;186:543–553. doi: 10.1097/00005053-199809000-00005. [DOI] [PubMed] [Google Scholar]
- Öst LG, Westling BE. Applied relaxation vs. cognitive behavior therapy in the treatment of panic disorder. Behaviour Research and Therapy. 1995;33:145–158. doi: 10.1016/0005-7967(94)e0026-f. [DOI] [PubMed] [Google Scholar]
- Otto MW, Hinton DE, Korbly NB, Chea A, Ba P, Gershuny BS, et al. Treatment of pharmacotherapy-refractory post-traumatic stress disorder among Cambodian refugees: A pilot study of combination treatment with cognitive–behavior therapy vs. sertraline alone. Behaviour Research and Therapy. 2003;41:1271–1276. doi: 10.1016/s0005-7967(03)00032-9. [DOI] [PubMed] [Google Scholar]
- Otto MW, Penava SJ, Pollack RA, Smoller JW. Cognitive–behavioral and pharmacologic perspectives on the treatment of post-traumatic stress disorder. In: Pollack M, Otto M, Rosenbaum J, editors. Challenges in clinical practice: Pharmacologic and psychosocial strategies. New York: Guilford; 1996. pp. 219–260. [Google Scholar]
- Rachman S. Emotional processing. Behaviour Research and Therapy. 1980;24:685–688. doi: 10.1016/0005-7967(80)90069-8. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. The expectancy model of fear. In: Reiss S, Bootzin R, editors. Theoretical issues in behavior therapy. NewYork: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims. Newbury Park, CA: Sage; 1993. [DOI] [PubMed] [Google Scholar]