Abstract
Influenza A viruses cause recurrent outbreaks of local or global scale with potentially severe consequences for human health and the global economy. Recently, a new strain of influenza A virus was detected that causes disease in and transmits among humans, probably owing to little or no pre-existing immunity to the new strain. On June 11, 2009, the WHO declared that the infections caused by the new strain had reached pandemic proportion. Characterized as an influenza A virus of the H1N1 subtype, the genomic segments of the new strain were most closely related to swine viruses1. Most human infections with swine-origin H1N1 influenza viruses (S-OIVs) appear to be mild; however, more than 50% of hospitalized individuals do not have underlying health issues, attesting to the pathogenic potential of S-OIVs. To better assess the risk posed by the new virus, we characterized one of the first US S-OIV isolates, A/California/04/09 (H1N1; CA04), as well as several other S-OIV isolates, in vitro and in vivo. In mice and ferrets, CA04 and other S-OIV isolates tested replicate more efficiently than a currently circulating human H1N1 virus. In addition, CA04 replicates efficiently in nonhuman primates, causes more severe pathologic lesions in the lungs of infected mice, ferrets, and nonhuman primates than a currently circulating human H1N1 virus, and transmits among ferrets. In specific-pathogen free miniature pigs, CA04 replicates without clinical symptoms. The assessment of human sera from different age groups suggests that infection with human H1N1 viruses antigenically closely related to viruses circulating in 1918 confers neutralizing antibody activity to CA04. Finally, we show that CA04 is sensitive to approved and experimental antiviral drugs, suggesting these compounds as a first line of defence against the recently declared S-OIV pandemic.
Sequence analyses of recently emerged swine origin H1N1 viruses (S-OIVs) revealed the absence of markers associated with high pathogenicity in avian and/or mammalian species, such as a multibasic HA cleavage site2 or lysine at position 627 of the PB2 protein3. To characterize the new viruses in vitro and in vivo, we amplified the following S-OIVs in Madin-Darby canine kidney (MDCK) cells: A/California/04/09 (CA04); A/Wisconsin/WSLH049/09 (WSLH049); A/Wisconsin/WSLH34939/09 (WSLH34939); A/Netherlands/603/09 (Net603), and A/Osaka/164/09 (Osaka164). WSLH34939 was isolated from a patient who required hospitalization, while the remaining viruses were isolated from mild cases. These viruses represent the currently recognized NA variants among S-OIVs: CA04, NA-106V, NA-248N; Osaka164, NA-106I, NA-248N; WSLH049, NA-106I, NA-248D; WSLH34939, NA-106I, NA-248D; and Net603, NA-106V, NA-248N.
In MDCK cells and primary human airway epithelial cells, CA04 grew to titres comparable to those typically obtained for contemporary human H1N1 influenza viruses (Supplementary Fig. S1). Confocal, transmission electron, and scanning electron microscopy revealed virions of remarkably filamentous shape (Supplementary Fig. S2), in marked contrast to the spherical shape observed with negatively stained virions (http://www.cdc.gov/h1n1flu/images.htm). The biological significance of the morphology of CA04 remains unknown.
To evaluate the pathogenicity of S-OIV in mammalian models, we conducted studies in mice, ferrets, nonhuman primates, and pigs. BALB/c mice intranasally infected with a high dose (>104 plaque-forming units [PFU]) of CA04 (Supplementary Fig. S3) experienced weight loss and those infected with the highest dose of this virus were humanely euthanized, in contrast to animals infected with a recent human H1N1 virus (A/Kawasaki/UTK-4/09, KUTK-4). The 50% mouse lethal dose (MLD50) was 105.8 plaque-forming units (PFU) for CA04 and >106.6 PFU for KUTK-4. For the additional S-OIV isolates tested, the MLD50 values were >106.4 PFU for Osaka164, >106.6 PFU for WSLH049, 104.5 PFU for WSLH34939, and >105.8 PFU for Net603.
On day 3 post infection (pi) of mice, similar titres were detected in nasal turbinates of mice infected with 105 PFU of S-OIVs or KUTK-4 (Supplementary Table 1); however, S-OIVs replicated more efficiently in the lungs of infected animals, which may account for the prominent bronchitis and alveolitis with viral antigen on day 3 postinfection with CA04 (Supplementary Fig. S4a–b). On day 6 pi, virus titres followed a similar trend and the lungs of CA04-infected mice showed a bronchoaveolitis with viral antigen, although signs of regeneration were apparent (Supplementary Fig. S4c). We detected viral antigen-positive bronchial epithelial, but not alveolar, cells on day 3 pi of mice infected with KUTK-4 (Supplementary Fig. S4e). By day 6, infection in KUTK-4-inoculated mice had progressed to a bronchitis and peribronchitis; however, viral antigen was rarely detected in these lesions (Supplementary Fig. S4f).
There were marked differences in the induction of pro-inflammatory cytokines in the lungs of mice infected with CA04 versus KUTK-4 (Supplementary Fig. S5a–c). Infection with KUTK-4 resulted in limited induction of pro-inflammatory cytokines/chemokines in the lungs, in striking contrast to infection with CA04. Increased production of IL-10 (Supplementary Fig. S5a) in lungs of CA04-infected mice at day 6 pi likely reflects a host response to dampen over-exuberant pulmonary inflammation and promote tissue repair. Infection with CA04 led to strong induction of both IFNγ and IL-4 in the lungs. The selective induction of the TH2 cytokine IL-5 in CA04- but not in KUTK-4-infected mice on day 6 pi is noteworthy (Supplementary Fig. S5b), but further studies are needed to understand the relevance of this finding to viral control. IL-17 has been reported to play a role in protection against lethal influenza and also in eliciting inflammatory responses4,5. However, the enhanced viral replication and lung pathology observed in CA04-infected mice was not linked to dysregulated IL-17 production.
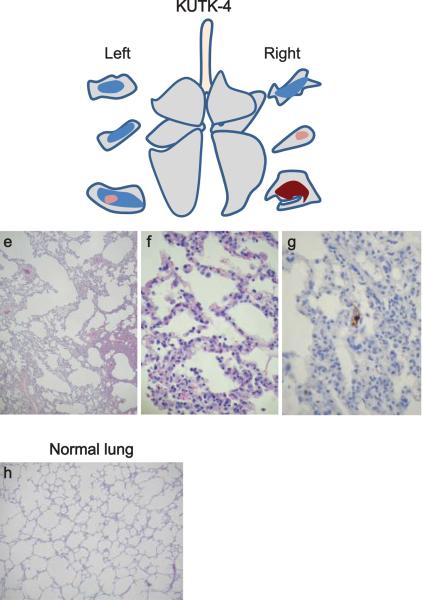
Cynomolgus macaques (Macaca fascicularis) have been used to study highly pathogenic avian H5N1 viruses6,7 and the 1918 pandemic virus8. Infection of cynomolgus macaques with CA04 (see `Methods' section for detailed procedures) resulted in a more prominent increase in body temperature than infection with KUTK-4 (Supplementary Fig. S6). This difference might originate from the observed differences in virus titres (Table 1 and Supplementary Table 2). No remarkable difference in body weight loss was found between the two groups (data not shown). CA04 replicated efficiently in the lungs and other respiratory organs of infected animals, similar to highly pathogenic influenza viruses6,8 (Table 1). By contrast, conventional human influenza viruses are typically limited in their replicative ability in the lungs of infected primates6,8 (Table 1), although a seasonal H1N1 virus was isolated from one animal on day 7 pi. Pathologic examination revealed that CA04 caused more severe lung lesions than did KUTK-4 (Fig. 1 and Supplementary Fig. S7). On day 3 pi with CA04, alveolar spaces were occupied by edematous exudate and inflammatory infiltrates (Fig. 1a); severe thickening of alveolar walls was also observed (Fig. 1b). Viral antigen-positive cells were distributed in the inflammatory lesions, and many of these cells were elongated with thin cytoplasm and hemming around the alveolar wall, indicating type I pneumocytes (Fig. 1c). In addition to type I pneumocytes, CA04 viral antigens were also detected in considerable numbers of cuboidal, cytokeratin-positive cells, hence identified as type II pneumocytes (Fig. 1d, and Supplementary Fig. S8), as has been reported for highly pathogenic avian H5N1 influenza viruses6. Upon infection with KUTK-4, large sections of infected lungs showed thickening of the alveolar wall on day 3 pi (Fig. 1e). Although the infiltration of inflammatory cells was prominent at the alveolar wall (Fig. 1f), viral antigens were sparse and detected in type I (but not type II) pneumocytes (Fig. 1g). By contrast, the lungs of noninfected animals show clear alveolar spaces (Fig. 1h).
Table 1.
Virus titres in organs of infected cynomolgus macaquesa
| A/California/04/09(H1N1) | A/Kawasaki/UTK-4/09 (H1N1) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| day 3 pi | day 7 pi | day 3 pi | day 7 pi | |||||||||
|
|
|
|||||||||||
| Animal ID | #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | #11 | #12 |
|
| ||||||||||||
| Nasal mucosa | 4.7b | 3.3 | -c | - | - | - | - | - | - | - | - | - |
| Oro/nasopharynx | 6.3 | 4.4 | 4.7 | - | 7.9 | - | - | - | 4.3 | - | - | 4.8 |
| Tonsil | 6.4 | - | - | - | 7.1 | - | - | - | 2.8 | - | - | 3.0 |
|
| ||||||||||||
| Trachea | 5.9 | 2.0 | 5.6 | - | - | - | 2.0 | 4.1 | - | 3.7 | - | 5.4 |
| Bronchus (right) | 5.7 | 2.9 | 4.3 | - | 5.1 | - | - | 2.5 | - | 3.5 | - | 3.8 |
| Bronchus (left) | 5.9 | - | 6.1 | - | 5.1 | - | - | - | - | 3.3 | - | 5.1 |
|
| ||||||||||||
| Lung (upper right) | 5.7 | 5.6 | 4.5 | - | - | - | 2.7 | - | - | - | - | - |
| Lung (middle right) | 5.6 | 6.4 | 6.9 | - | - | - | 2.3 | 2.6 | 2.5 | - | - | - |
| Lung (lower right) | 6.1 | 4.5 | 6.0 | - | - | - | 2.6 | 2.6 | - | - | - | 3.4 |
| Lung (upper left) | 4.7 | 4.3 | 6.4 | - | - | - | - | - | - | - | - | - |
| Lung (middle left) | 5.8 | 4.3 | 6.3 | - | - | - | - | - | - | - | - | - |
| Lung (lower left) | 6.7 | 4.5 | 6.6 | - | - | - | - | - | - | - | - | 2.3 |
| Conjunctiva | 3.6 | - | - | - | - | - | - | - | - | - | - | - |
Cynomolgus macaques were inoculated with 107.4 PFU of virus (6.7 ml) through multiple routes (see detailed procedure in Methods). Three macaques per group were euthanized on day 3 and 7 pi for virus titration. No virus was recovered from lymph nodes (chest), heart, spleen, kidneys, or liver of any animals.
Virus titre (mean log10 PFU/g).
-, virus not detected (detection limit: 2 log10 PFU/g).
Figure 1. Pathologic examination of the lungs of infected cynomolgus macaques.
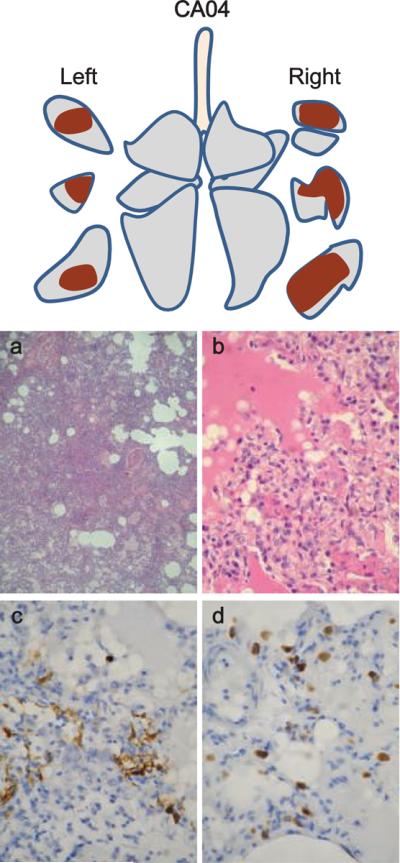
Representative pathologic images of CA04- (macaque #1, a-d), KUTK-4- (macaque #7, e-g), and mock- (h) infected lungs on day 3 pi. One or two sections per lung lobe were examined; representative findings are shown to depict the distribution of lesions in the sections (shown as cross sections placed next to illustrations of each lung lobe), with or without viral antigen, as follows: brown, severe lung lesion containing moderate to many viral antigen-positive cells; pink, mild lung lesions containing a few viral antigen-positive cells; blue, lung lesions with alveolar wall thickening, with remaining air spaces unaffected.
On day 7 pi, lung pathology remained more severe for CA04- than for KUTK-4-infected lungs (Supplementary Fig. S7), although regenerative changes were seen for CA04. Nonetheless, considerable numbers of antigen-positive cells were still detectable (Supplementary Fig. S7c). Collectively, these findings demonstrate that CA04 causes more severe lung lesions in nonhuman primates than does a contemporary human influenza virus.
Induction of pro-inflammatory cytokines/chemokines in the lungs of CA04-infected macaques was variable at day 3 pi (Supplementary Fig. S9). However, consistent with persisting lung pathology and inflammation on day 7 pi, the levels of MCP-1, MIP-1α, IL-6, and IL-18 were markedly higher in the lungs of 2 of 3 CA04-infected macaques.
Ferrets are widely accepted as a suitable small-animal model for influenza virus pathogenicity and transmissibility studies. Infection of ferrets with S-OIVs or KUTK-4 did not cause marked changes in body temperature or weight in any group (data not shown). Although all test viruses were detected in nasal turbinates at similar titres on day 3 pi (Supplementary Table 3), S-OIVs replicated to higher titres in trachea and lungs.
Pathological examination detected similar levels of viral antigen in the nasal mucosa of both CA04- and KUTK-4-infected ferrets (Supplementary Fig. S10a and e). However, the lungs of CA04-infected ferrets showed more severe bronchopneumonia with prominent viral antigen expression in the peribronchial glands and a few alveolar cells (Supplementary Fig. S10b-d) on day 3 pi. By contrast, most of the lung appeared normal following infection with KUTK-4 (Supplementary Fig. S10f and g). Thus, in all three mammalian models tested, CA04 appeared to be more pathogenic than a contemporary human H1N1 virus, KUTK-4.
Efficient human-to-human transmission is a critical feature of pandemic influenza viruses. To assess the transmissibility of CA04, naïve ferrets in perforated cages were placed next to ferrets inoculated with 106 PFU of CA04 (see `Methods' section for detailed procedures). This experimental setting allows for aerosol transmission, i.e., the exchange of respiratory droplets between the inoculated and non-inoculated ferrets, but prevents transmission by direct and indirect contact. All three contact ferrets were positive for CA04 virus on days 3 and 5 pi (Supplementary Table 4). This transmission pattern is comparable to those of two human control influenza viruses that are known to transmit among ferrets, KUTK-4 and A/Victoria/3/75 (H3N2)9. By contrast, an avian influenza virus (A/duck/Alberta/35/76; H1N1) did not transmit (Supplementary Table 4).
Genetic analysis suggests that S-OIV originated in pigs1. However, there were no confirmed influenza virus outbreaks in Central American pigs prior to the reported S-OIV infections in humans. To assess S-OIV replication in pigs, we inoculated specific-pathogen free miniature pigs, which are easier to manage, with CA04 or a classical swine influenza virus (A/swine/Hokkaido/2/81, H1N1). No signs of disease were observed (data not shown), although both viruses replicated efficiently in the respiratory organs of these animals (Supplementary Tables 5 and 6). Slightly higher titres of CA04 were detected in lungs on day 3 pi, which is supported by pathological findings that show more apparent bronchitis and bronchiolitis in pigs infected with CA04 (Supplementary Fig. S11). The asymptomatic infection of CA04, despite efficient virus replication, might explain the lack of reports of S-OIV outbreaks in pigs prior to virus transmission to humans.
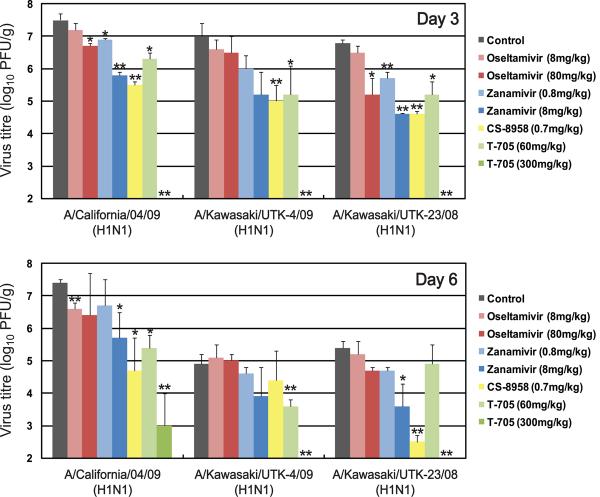
Antiviral compounds are the first line of defence against pandemic influenza viruses. Sequence analysis suggests that S-OIVs are resistant to ion channel inhibitors such as amantadine and rimantadine1. We, therefore, tested the licensed neuraminidase inhibitors oseltamivir and zanamivir, the experimental neuraminidase inhibitor R-125489 (the active form of CS-895810), and the experimental compound T-705 (a broad-spectrum viral RNA polymerase inhibitor11) for their efficacy against CA04. In cell culture, CA04 was highly susceptible to all compounds tested (Supplementary Table 7), as were the human H1N1 control viruses A/Kawasaki/UTK-23/08 and KUTK-4, with the exception of the known oseltamivir resistance of KUTK-4. Comparable sensitivities were also found in an enzymatic neuraminidase inhibition assay12 (Supplementary Table 8) and in mice (Fig. 2), consistent with observations in clinical settings.
Figure 2. CA04 sensitivity to antiviral compounds in mice.
Mice were intranasally inoculated with 104 PFU (50 μl) of CA04, KUTK-4, or A/Kawasaki/UTK-23/08 (H1N1). At 1 h pi, mice were administered oseltamivir phosphate, zanamivir, CS-8958, T-705, or distilled water and PBS (control). Three mice per group were euthanized on days 3 and 6 pi and the virus titres in lungs were determined by plaque assays in MDCK cells. *, p<0.05, **, p<0.01.
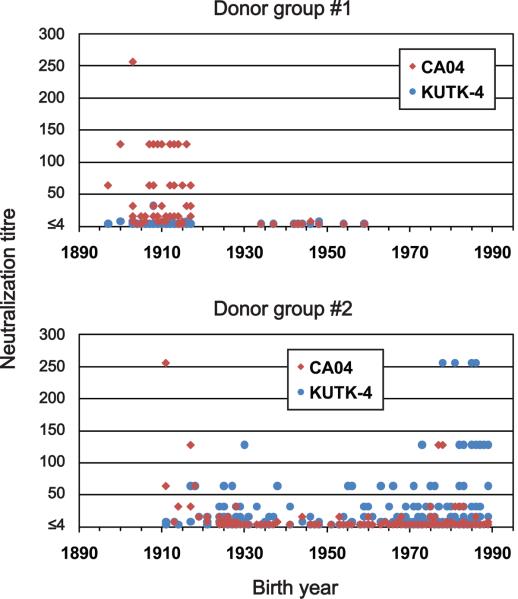
A recent report suggested that 33% of individuals over 60 years of age had neutralizing antibodies to CA04 (http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5819a1.htm:MMWR), likely due to previous exposure to antigenically similar H1N1 viruses. In fact, both the human H1N1 viruses that circulated until 1957 and the classical swine virus HA gene of S-OIVs are descendants of the 1918 pandemic virus, possibly explaining their antigenic relatedness. In 1977, H1N1 viruses re-emerged that were genetically and antigenically very closely related to viruses circulating in the 1950s13 and should thus have elicited neutralizing antibodies to CA04 among younger age groups; however, this does not appear to be the case, according to the above described report. To resolve this puzzling finding, we assessed the neutralizing activities of sera collected from a broad range of age groups against CA04 and KUTK-4. We used two sets of donor sera, collected in 1999 from residents and workers in a nursing home (donor set #1), and in April of 2009 from workers and patients in a hospital (donor set #2). High neutralizing activity against KUTK-4 was detected for many sera in donor set #2 (Fig. 3), but not for sera in donor set #1, likely because these sera were collected prior to the emergence of the current human H1N1 viruses. Interestingly, with few exceptions, no appreciable neutralizing antibodies against CA04 were found for individuals born after 1920; however, many of those born before 1918 had high neutralizing antibody titres (individual neutralizing antibody titres are shown in Supplementary Table 9). These data indicate that infection with the 1918 pandemic virus or closely related human H1N1 viruses, but not infection with antigenically divergent human H1N1 viruses circulating in the 1920s to 1950s, and again since 1977, elicited neutralizing antibodies to S-OIVs.
Figure 3. Neutralization activities in human sera against viruses.
Human sera of donor groups #1 (collected in 1999) and #2 (collected in April and May of 2009) were subjected to neutralization assays with CA04 and KUTK-4. Since the sera of donor group #1 were collected in 1999, little neutralization activity was expected against KUTK-4, which was isolated in 2009.
Our findings indicate that S-OIVs are more pathogenic in mammalian models than seasonal H1N1 influenza viruses. In fact, the ability of CA04 to replicate in the lungs of mice, ferrets, and nonhuman primates, and to cause appreciable pathology in this organ is reminiscent of infections with highly pathogenic H5N1 influenza viruses14, as acknowledged in a recent report by WHO (http://www.who.int/wer/2009/wer8421/en/index.html). We therefore speculate that the high replicative ability of S-OIVs might contribute to a viral pneumonia characterized by diffuse alveolar damage that contributes to hospitalizations and fatal cases where no other underlying health issues exist (http://www.who.int/wer/2009/wer8421/en/index.html). In addition, sustained person-to-person transmission might result in the emergence of more pathogenic variants, as observed with the 1918 pandemic virus (reviewed in Ref. 15). Furthermore, S-OIVs may acquire resistance to oseltamivir through mutations in their NA gene (as recently witnessed with human H1N1 viruses16), or through reassortment with co-circulating, oseltamivir-resistant seasonal human H1N1 viruses. Collectively, our findings are a firm reminder that S-OIVs have not yet garnered a place in history, but may still do so, as the pandemic caused by these viruses has the potential to produce significant impact on human health and the global economy.
Methods Summary
Viruses and cells
All swine-origin H1N1 viruses were isolated and passaged in MDCK cells to produce viral stocks. The viruses and their passage histories are described in the `Methods' section. All experiments with S-OIVs were performed in approved enhanced biosafety level 3 (BSL3) containment laboratories.
Madin-Darby canine kidney (MDCK) cells and MDCK cells overexpressing the β-galactoside α2,6-sialyltransferase I gene17 were maintained in Eagle's minimal essential medium (MEM) containing 5% newborn calf serum. Human airway epithelial (HAE) cells were obtained from residual surgical tissue trimmed from lungs during the process of transplantation. The bronchial specimens were dissected and enzymatically digested, and monolayers of HAE cells were isolated, cultured and differentiated as previously described18.
Animals
Five- and six-week-old female BALB/c mice (Jackson Laboratory, Bar Harbor, ME, and Japan SLC Inc., Shizuoka, Japan), approximately three-to-four-year-old cynomolgus macaques (Ina Research Inc., Ina, Japan), five-to-eight-month-old male ferrets (Marshall Farms, Wolcott, NY and Triple F Farms, Sayre, PA), and two-month-old female specific-pathogen free miniature pigs (Nippon Institute for Biological Science, Yamanashi, Japan) were used according to approved protocols for the care and use of animals. Detailed procedures are provided in the `Methods' section.
Antiviral sensitivity of viruses in mice
Five-week-old female BALB/c mice (Japan SLC Inc., Shizuoka, Japan; groups of six) were anesthetized with sevoflurane and intranasally inoculated with 104 plaque-forming units (volume: 50 μl) of CA04, KUTK-4, or A/Kawasaki/UTK-23/08 (H1N1). At 1 h pi, mice were administered antiviral compounds as described in detail in the `Methods' section. Three mice per group were euthanized on days 3 or 6 pi and the virus titres in lungs were determined by plaque assays in MDCK cells.
Methods
Viruses
A/California/04/09 (H1N1; CA04) was kindly provided by the Centers for Disease Control (CDC). A/Wisconsin/WSLH049/09 (H1N1) was isolated from a patient with mild symptoms, while A/Wisconsin/WSLH34939/09 (H1N1) was isolated from a hospitalized patient. A/Netherlands/603/09 (H1N1) was isolated from a patient with mild symptoms and was kindly provided by Ron Fouchier (Erasmus University, Rotterdam, The Netherlands). A/Osaka/164/09 (H1N1) was also isolated from a patient with mild symptoms.
The following influenza viruses served as controls: A/Kawasaki/UTK-4/09 (H1N1; KUTK-4; passaged twice in MDCK cells), an oseltamivir-resistant seasonal human virus; A/WSN/33 (H1N1; generated by reverse genetics and passaged twice in MDCK cells), a typical spherical influenza virus19; A/Kawasaki/UTK-23/08 (H1N1; passaged twice in MDCK cells), an oseltamivir-sensitive seasonal human virus; A/Victoria/3/75 (H3N2; passaged several times in eggs after it was obtained from the CDC), a human virus; A/swine/Hokkaido/2/81 (H1N1; passaged several times in eggs), a classical swine virus; and A/duck/Alberta/35/76 (H1N1; passaged several times in eggs), an avian virus. All experiments with S-OIV viruses were performed in enhanced biosafety level 3 (BSL3) containment laboratories at the University of Wisconsin-Madison, which are approved for such use by the CDC and the U.S. Department of Agriculture, or in BSL3 containment laboratories at the University of Tokyo (Tokyo, Japan), the Shiga University of Medical Science (Shiga, Japan), or the Hokkaido University (Sapporo, Japan), all of which are approved for such use by the Ministry of Agriculture, Forestry and Fisheries, Japan.
Viral pathogenesis in mice
Six-week-old female BALB/c mice (Jackson Laboratory, Bar Harbor, ME) were used in this study. Baseline body weights were measured prior to infection. Three mice per group were anesthetized with isoflurane and intranasally inoculated with 102, 103, 104, or 105 PFU (50 μl) of CA04 and KUTK-4, or undiluted virus from virus stocks (CA04; 106.5 PFU, KUTK-4; 106.6 PFU). Body weight and survival were monitored daily for 14 days and mice with body weight loss of more than 25% of pre-infection values were euthanized. For virologic and pathologic examinations, 6 mice per group were intranasally infected with 105 PFU of S-OIVs and KUTK-4 and 3 mice per group were euthanized on days 3 and 6 pi. The virus titres in various organs were determined by plaque assays in MDCK cells.
Growth kinetics of virus in human airway epithelial (HAE) cells
Cultures of differentiated HAE cells were washed extensively with PBS to remove accumulated mucus and infected with virus at a multiplicity of infection (MOI) of 0.001 from the apical surface. The inoculum was removed after 1 h of incubation at 35°C, and cells were further incubated at 35°C. Samples were collected at 12, 24, 48, 72 and 96 h post infection from the apical surface. Apical harvesting was performed by adding 500 μl of medium to the apical surface, followed by incubation for 30 min at 35°C, and removal of the medium from the apical surface. The titres of viruses released into the cell culture supernatant were determined by plaque assay in MDCK cells.
Experimental infection of cynomolgus macaques
Approximately three-to-four-year-old cynomolgus macaques (Macaca fascicularis) from the Philippines (obtained from Ina Research Inc., Ina, Japan), weighing 2.1–3.0 kg and serologically negative by AniGen AIV Ab ELISA, which detects all influenza A virus subtypes (Animal Genetics Inc., Kyonggi-do, Korea), were used in this study. Baseline body weights were established by two or three measurements prior to infection. Under anesthesia, telemetry probes (TA10CTA-D70, Data Sciences International, St. Paul, MN) were implanted in the peritoneal cavities of animals to monitor body temperature. Six macaques per group were intramuscularly anesthetized with ketamine (5 mg per kg) and xylazine (1 mg per kg) and inoculated with a suspension containing 106.5 PFU/ml of CA04 or KUTK-4 virus through a combination of intratracheal (4.5 ml), intranasal (0.5 ml per nostril), ocular (0.1 ml per eye) and oral (1 ml) routes (resulting in a total infectious dose of 107.4 PFU). Macaques were monitored every 15 minutes for changes in body temperature. On days, 1, 3, 5, and 7 pi, nasal and tracheal swabs and bronchial brush samples were collected. On days 3 and 7 pi, 3 macaques per group were euthanized for virologic and pathologic examinations. The virus titres in various organs and swabs were determined by plaque assays in MDCK cells. Experiments were carried out in accordance with the Guidelines for the Husbandry and Management of Laboratory Animals of the Research Center for Animal Life Science at Shiga University of Medical Science, Shiga, Japan, and approved by the Shiga University of Medical Science Animal Experiment Committee and Biosafety Committee.
Experimental infection of ferrets
We used five-to-eight-month-old male ferrets (Marshall Farms, Wolcott, NY and Triple F Farms, Sayre, PA), which were serologically negative by hemagglutination inhibition (HI) assay for currently circulating human influenza viruses. Baseline body temperatures and body weights were established by one or two measurements prior to infection. Six ferrets per group were intramuscularly anesthetized with ketamine and xylazine (5 mg and 0.5 mg per kg of body weight, respectively) and intranasally inoculated with 106 PFU (500 μl) of S-OIVs or KUTK-4. On days 3 and 6 pi, 3 ferrets per group were euthanized for virologic and pathologic examinations. The virus titres in nasal washes and various organs were determined by plaque assays in MDCK cells.
Experimental infection of miniature pigs
Two-month-old female specific-pathogen free miniature pigs (Nippon Institute for Biological Science, Yamanashi, Japan), which were serologically negative by AniGen AIV Ab ELISA for currently circulating influenza viruses, were used in this study. Baseline body temperatures were measured once prior to infection. Four pigs per group were intranasally inoculated with 106.2 PFU (1 ml) of viruses. Nasal swabs were collected daily. On day 3 pi, two pigs per group were euthanized and their tissues collected for examination. On day 14 pi, the remaining two pigs per group were euthanized for virologic and pathologic examinations. Virus titres in various organs and swabs were determined by plaque assays in MDCK cells. The miniature pigs used in this study were housed in self-contained isolator units (Tokiwa Kagaku, Tokyo, Japan) at a BSL3 facility and experiments were conducted in accordance with guidelines established by the Animal Experiment Committee of the Graduate School of Veterinary Medicine, Hokkaido University, Japan.
Pathologic examination
Excised tissues of the nasal turbinates, trachea and/or lungs of euthanized mice, macaques, ferrets, and pigs were preserved in 10% phosphate-buffered formalin. Tissues were then processed for paraffin embedding and cut into 5-μm-thick sections. One section from each tissue sample was stained using a standard hematoxylin-and-eosin procedure, while another one was processed for immunohistological staining with an anti-influenza virus rabbit antibody (R309; prepared in our laboratory) that reacts comparably with CA04 and KUTK-4. Specific antigen-antibody reactions were visualized by 3, 3' diaminobenzidine tetrahydrochloride staining using a Dako EnVision system (Dako Co. Ltd., Tokyo, Japan).
Ferret transmission study
For transmission studies in ferrets, animals were housed in adjacent transmission cages that prevent direct and indirect contact between animals but allow spread of influenza virus through the air. Three or two 5-to-8-month-old ferrets were intranasally inoculated with 106 PFU (500 μl) of CA04, KUTK-4, A/Victoria/3/75 (H3N2), or A/duck/Alberta/35/76 (H1N1) (= inoculated ferrets). One day after infection, three or two naïve ferrets were each placed in a cage adjacent to an inoculated ferret (= contact ferrets). All ferrets were monitored daily for changes in body temperature and weight, and the presence of clinical signs. To assess viral replication in the upper respiratory tract, viral titres were determined in nasal washes collected from virus-inoculated and contact ferrets on day 1 after inoculation or co-housing, respectively, and then every other day (up to 9 days).
Cytokine and chemokine measurement
For cytokine and chemokine measurement, homogenates of mouse lungs were processed with the Bio-Plex Mouse Cytokine 23-Plex and 9-Plex panels (Bio-Rad Laboratories, Hercules, CA), whereas macaque lung homogenates were measured with the MILLIPLEX MAP Non-human Primate Cytokine/Chemokine Panel - Premixed 23-Plex (Millipore, Bedford, MA). Array analysis was performed by Bio-Plex Protein Array system (Bio-Rad Laboratories).
Antiviral sensitivity of viruses in mice
To test the antiviral sensitivity of viruses in mice, animals were infected as described in the `Method Summary' section and one hour later administered the following antiviral compounds: (i) oseltamivir phosphate: 8 or 80 mg/kg/400 μl (divided into two oral administrations per day) for 5 days; (ii) zanamivir: 0.8 or 8 mg/kg/50 μl in one daily intranasal administration for 5 days; (iii) CS-8958: 0.7 mg/kg/50 μl in one intranasal administration; (iv) T-705: 60 or 300 mg/kg/400 μl (divided into two oral administrations per day) for 5 days; (v) or distilled water orally (200 μl) and PBS intranasally (50 μl). Three mice per group were euthanized on days 3 or 6 pi and the virus titres in lungs were determined by plaque assays in MDCK cells.
Sensitivity to antiviral compounds in tissue culture
MDCK cells overexpressing the β-galactoside α2,6-sialyltransferase I gene (or, for studies with T-705, regular MDCK cells) were infected with CA04, KUTK-4, or A/Kawasaki/UTK-23/08 (H1N1) at a multiplicity of infection of 0.001. After incubation for 1 h at 37°C, growth medium containing various concentrations of oseltamivir carboxylate (the active form of oseltamivir), zanamivir, R-125489 (the active form of CS-8958), or T-705 was added to the cells. Twenty-four hours later, the culture supernatants were harvested and the 50% tissue-culture infectious dose (TCID50) in MDCK cells determined. Based on the TCID50 value, the 90% inhibitory concentration (IC90) was calculated.
Neuraminidase inhibition assay
To assess the sensitivity of viruses to neuraminidase inhibitors (i.e., oseltamivir, zanamivir, and CS-8958), neuraminidase inhibition assays were performed as described previously20. Briefly, diluted viruses were mixed with various concentrations of oseltamivir carboxylate, zanamivir, or R-125489 in 2-(N- morpholino)ethanesulfonic acid containing calcium chloride, and incubated for 30 min at 37°C. Then, we added methylumbelliferyl-N-acetylneuraminic acid (Sigma, St Louis, MO) as a fluorescent substrate to this mixture. After incubation for one hour at 37°C, sodium hydroxide in 80% ethanol was added to the mixture to stop the reaction. The fluorescence of the solution was measured at an excitation wavelength of 360 nm and an emission wavelength of 465 nm and the 50% inhibitory concentration (IC50) was calculated.
Neutralization assay with human sera
Human sera were collected in 1999 or 2009 from donor group #1 (age range: 50 to 112 years as of 2009, mean = 92.7 ± 15.0 years) or #2 (age range: 20 to 68 years as of 2009, mean = 48.2 ± 23.7 years), respectively. These sera were treated with receptor-destroying enzyme (DENKA SEIKEN CO., LTD, Tokyo, Japan) to remove inhibitors of influenza virus replication. One hundred TCID50 (50% tissue culture infectious dose) of CA04 and KUTK-4 were pre-incubated with twofold serial dilutions of treated sera, incubated for 30 min on MDCK cells, which were then observed for cytopathic effects to determine the neutralizing activity of the test sera. Our research protocol was approved by the Research Ethics Review Committee of the Institute of Medical Science, the University of Tokyo (approval numbers; 21-6-0428 for donor group #1, 21-7-0529 for donor group #2).
Immunofluorescence microscopy
MDCK cells were infected with CA04, KUTK-4, or WSN and fixed with 4% paraformaldehyde 16–24 hours later. Infected cells were incubated with the following primary antibodies: mouse anti-HA (7B1b), anti-HA (IVC102), or mouse anti-HA (WS3-54) antibody against CA04, KUTK-4, or WSN, respectively. Cells were then incubated with Alexa Fluor 488 goat anti-mouse immunoglobulin G (Invitrogen, Carlsbad, CA), and examined with a confocal laser- scanning microscope (LSM510META; Carl Zeiss, Jena, Germany).
Electron microscopy
MDCK cells were infected with CA04, KUTK-4, or WSN at a multiplicity of infection of 10. At 16–24 hours pi, cells were processed for ultrathin section electron microscopy and scanning electron microscopy as described previously19,21.
Supplementary Material
Acknowledgements
We thank the Centers for Disease Control (CDC) for A/California/04/09 virus and Ron Fouchier (Erasmus University, Rotterdam, The Netherlands) for A/Netherlands/603/09 virus. We thank Krisna Wells for editing the manuscript, Martha McGregor, Rebecca Moritz, Anthony Hanson, Hideaki Ishida, Hideaki Tsuchiya, Ryuzo Torii, Naoki Yamamoto, Kosuke Soda, Naoki Nomura, and Hiromi Yoshida for excellent technical assistance. We also thank Takashi Umemura, Yuji Sunden, and Tomohisa Tanaka for pathological analyses of virus-infected pigs. This work was supported by National Institute of Allergy and Infectious Diseases Public Health Service research grants; by an NIAID-funded Center for Research on Influenza Pathogenesis (CRIP, HHSN266200700010C), by Grant-in-Aid for Specially Promoted Research, by a contract research fund for the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases from the Ministry of Education, Culture, Sports, Science, and Technology, and by grants-in-aid from the Ministry of Health and by ERATO (Japan Science and Technology Agency). G.N. is named as co-inventor on several patents about influenza virus reverse genetics and/or the development of influenza virus vaccines or antivirals. Y.K. is named as inventor/co-inventor on several patents about influenza virus reverse genetics and/or the development of influenza virus vaccines or antivirals.
Footnotes
Supplementary Information is linked to the online version of the paper at www.nature.com/nature.
Reference List
- 1.Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team Emergence of a Novel Swine-Origin Influenza A (H1N1) Virus in Humans. N. Engl. J Med. 2009 doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 2.Kawaoka Y, Webster RG. Sequence requirements for cleavage activation of influenza virus hemagglutinin expressed in mammalian cells. Proc Natl Acad Sci U S A. 1988;85:324–8. doi: 10.1073/pnas.85.2.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular Basis for High Virulence of Hong Kong H5N1 Influenza A Viruses. Science. 2001;293:1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 4.Iwakura Y, Nakae S, Saijo S, Ishigame H. The roles of IL-17A in inflammatory immune responses and host defense against pathogens. Immunol Rev. 2008;226:57–79. doi: 10.1111/j.1600-065X.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 5.Hamada H, et al. Tc17, a unique subset of CD8 T cells that can protect against lethal influenza challenge. J Immunol. 2009;182:3469–3481. doi: 10.4049/jimmunol.0801814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baskin CR, et al. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc. Natl. Acad. Sci U. S. A. 2009;106:3455–3460. doi: 10.1073/pnas.0813234106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rimmelzwaan GF, et al. Pathogenesis of influenza A (H5N1) virus infection in a primate model. J Virol. 2001;75:6687–91. doi: 10.1128/JVI.75.14.6687-6691.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kobasa D, et al. Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature. 2007;445:319–323. doi: 10.1038/nature05495. [DOI] [PubMed] [Google Scholar]
- 9.Maines TR, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc. Natl. Acad. Sci U. S. A. 2006;103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamashita M, et al. CS-8958, a prodrug of the new neuraminidase inhibitor R-125489, shows long-acting anti-influenza virus activity. Antimicrob. Agents Chemother. 2009;53:186–192. doi: 10.1128/AAC.00333-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Furuta Y, et al. In vitro and in vivo activities of anti-influenza virus compound T-705. Antimicrob. Agents Chemother. 2002;46:977–981. doi: 10.1128/AAC.46.4.977-981.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayden FG, et al. Inhaled zanamivir for the prevention of influenza in families. Zanamivir Family Study Group. N. Engl. J Med. 2000;343:1282–1289. doi: 10.1056/NEJM200011023431801. [DOI] [PubMed] [Google Scholar]
- 13.Nakajima K, Desselberger U, Palese P. Recent human influenza A (H1N1) viruses are closely related genetically to strains isolated in 1950. Nature. 1978;274:334–339. doi: 10.1038/274334a0. [DOI] [PubMed] [Google Scholar]
- 14.Peiris JS, et al. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet. 2004;363:617–619. doi: 10.1016/S0140-6736(04)15595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright PF, Neumann G, Kawaoka Y. In: Fields Virology. Knipe DM, et al., editors. Wolters Kluwer, Lippincott Willams & Wilkins; Philadelphia: 2007. pp. 1691–1740. [Google Scholar]
- 16.Moscona A. Global transmission of oseltamivir-resistant influenza. N. Engl. J Med. 2009;360:953–956. doi: 10.1056/NEJMp0900648. [DOI] [PubMed] [Google Scholar]
- 17.Hatakeyama S, et al. Enhanced expression of an alpha2,6-linked sialic acid on MDCK cells improves isolation of human influenza viruses and evaluation of their sensitivity to a neuraminidase inhibitor. J Clin Microbiol. 2005;43:4139–4146. doi: 10.1128/JCM.43.8.4139-4146.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jakiela B, Brockman-Schneider R, Amineva S, Lee WM, Gern JE. Basal cells of differentiated bronchial epithelium are more susceptible to rhinovirus infection. Am J Respir. Cell Mol. Biol. 2008;38:517–523. doi: 10.1165/rcmb.2007-0050OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noda T, et al. Architecture of ribonucleoprotein complexes in influenza A virus particles. Nature. 2006;439:490–492. doi: 10.1038/nature04378. [DOI] [PubMed] [Google Scholar]
- 20.Kiso M, et al. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet. 2004;364:759–765. doi: 10.1016/S0140-6736(04)16934-1. [DOI] [PubMed] [Google Scholar]
- 21.Neumann G, et al. Ebola virus VP40 late domains are not essential for viral replication in cell culture. J Virol. 2005;79:10300–10307. doi: 10.1128/JVI.79.16.10300-10307.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.