Abstract
Objective
Test the efficacy of educational interventions to reduce literacy barriers and enhance health outcomes among patients with inflammatory arthritis.
Methods
The intervention consisted of plain language information materials and/or two individualized sessions with an arthritis educator. Randomization was stratified by education level. Principal outcomes included adherence to treatments, self-efficacy, satisfaction with care, and appointment keeping. Secondary outcomes included health status and mental health. Data were collected at baseline, six, and twelve months post.
Results
Of the 127 patients, half had education beyond high school and three quarters had disease duration greater than five years. There were no differences in the primary outcome measures between the groups. In mixed models controlling for baseline score and demographic factors, the intervention group showed improvement in mental health score at six and twelve months (3.0 and 3.7 points, respectively), while the control group showed diminished scores (−4.5 and −2.6 points, respectively) (p=0.03 and 0.01).
Conclusion
While the intervention appears to have had no effect on primary outcomes, further studies with continued attention to literacy are warranted. Study site and disease duration must be considered as participants in this study had higher than average health literacy and had established diagnoses for years prior to this study.
Practice Implications
The study offers insight into an application of many of the protocols currently recommended to ameliorate effects of limited literacy.
Keywords: health literacy, literacy, randomized controlled trial, patient education, inflammatory arthritis
1. Introduction
The U.S. Department of Education surveyed the literacy skills of adults in 1992 and 2003. Both surveys indicate that about half of U.S. adults have difficulty using print materials found in everyday life to accomplish mundane tasks, such as determining correct dosage by using a chart on the package of an over-the counter medicine.(1,2) An analysis based on the 1992 National Adult Literacy Survey (NALS) indicated that a clear majority of adults had difficulty using health materials to accomplish health related tasks.(3) Unfortunately, the 2003 National Assessment of Adult Literacy (NAAL) indicated little or no improvement. (4)
Health materials are complex and currently well over 800 peer-reviewed studies indicate a mismatch between the reading demands of these materials and the literacy skills of U.S. adults.(5) This mismatch between demands and skills has serious implications. (6) Poor literacy skills have been associated with unfavorable health outcomes for a number of chronic diseases such as diabetes, asthma, HIV, and heart disease. (7) Arthritis studies have contributed to this body of literature indicating, for example, that patients with rheumatoid arthritis who had not completed high school showed poorer clinical status than patients who had and that low formal education was a predictor of premature mortality for arthritis patients over a ten-year period. (8, 9) Patients with inflammatory arthritis need to be attentive to symptoms and subtle changes, engage in discussions with clinicians, differentiate among medicines, and follow recommended regimens. These activities require sophisticated literacy skills including reading, numeracy, oral presentation, and oral comprehension.
Despite the rich literature describing the burden and consequences of limited health literacy, few studies of interventions to reduce literacy related barriers to optimal care have been conducted. The Institute of Medicine Committee on Health Literacy strongly recommends that health care systems develop and support demonstration programs to establish the most effective approaches to reducing the negative effects of limited health literacy. (10)
We report on a randomized controlled trial of an educational intervention, conducted among patients with inflammatory arthritis, to reduce the literacy demand and thereby enhance health outcomes. In the design of this study, health literacy was defined as the match between the literacy skills of individuals and the expectations and demands of health systems. This definition was later reflected in the reports of the Institute of Medicine (10) and the Department of Health and Human Services. (11) We hypothesized that patients randomly assigned to an intervention designed to reduce literacy related barriers would be more adept at following treatments, have greater self-efficacy, and increased satisfaction with care than would patients managed in a customary manner.
2. Methods
We conducted a randomized controlled single blind trial of an educational intervention. From 2003–2006, Patients with rheumatoid arthritis, psoriatic arthritis and inflammatory polyarthritis (ICD-9 codes = 714.0, 696.0, 714.9) were recruited from an arthritis center in an urban teaching hospital. All participants had at least one visit with a rheumatologist who gave permission to recruit his/her patients and who also agreed to have study visits tape recorded if the patient consented to the study. Patients younger than 18 years of age, medical professionals, those with a post graduate degree, those with a visual impairment affecting reading ability, and those who reported not being comfortable with spoken and written English were excluded. Participants were initially selected based on an enrollment ratio of three participants with a high school or less education to one with a grade 13 or higher education.
The recruitment letter, signed by the principal investigator and the patient’s rheumatologist, was sent approximately six weeks before the patient’s scheduled appointment. The letter was written with attention to vocabulary and sentence length, making use of everyday words and short sentences when possible. The research assistant (RA) called only those patients who expressed interest in the study or who did not return an opt-out card. Interested patients assented to complete a baseline questionnaire administered by telephone and then met the research assistant to complete the consent process just before their rheumatology appointment. The hospital’s Human Subjects Committee approved all recruitment procedures.
All research assistants and the study educator interacting with participants completed an orientation and training program related to the use of everyday speech and avoidance of jargon, scientific terms, and cumbersome sentence structure.
2.1. Randomization
The study staff members were blinded to participant’s group assignment. The recruitment logs and tracking system were kept separate from the Study Educator’s logs and appointment schedule. The participants provided baseline information, including education level. A research assistant then randomized the participants into 3 groups: Standard Care, Plain English Materials, or Individualized Care. Separate randomization schemes were used for participants with less than high school education versus participants with greater than high school education. The randomization was stratified in this way to ensure a balance of education levels across the interventions.
2.2. Description of Interventions
The Standard Care Group received standard rheumatology care from their rheumatologist and a notebook containing Arthritis Foundation (AF) pamphlets about their type of arthritis and about their arthritis medicines, examples of medicine calendars, and a map of the hospital. The AF materials had a reading level between an 11th and15th grade on the SMOG (Simple Measure of Gobbledygook). (12)
The Plain English Material Group received usual rheumatology care supplemented by a notebook containing all information materials in plain language, assessed with reading grade levels 5th to 8th grade on the SMOG and well as the examples of medicine calendars, and a map of the hospital. Plain language materials are defined as “a clear, simple, conversational style for oral and written interactions, at or below an 8th grade reading level. (13) All plain language study materials intended to reduce literacy-related barriers to self care and to health system navigation. The notebook contained information about arthritis on the following topics: What you need to know, Treatment Choices, Medicine, Therapy and Exercise, Surgery, and information sheets for each arthritis medicine the participant was taking. The notebook also contained a booklet on getting the most from a visit to the doctor, examples of medicine calendars and reminder cues, a map of the hospital and information about the hospital.
The Individualized Care Group received usual rheumatology care supplemented by the plain language materials as well as two appointments with an educator. The educator was available for an hour for participants in this group; however, meetings usually lasted about 20 minutes during which time the educator reviewed all of the materials in the notebook, highlighting information directly pertinent to the participant with specific attention to medicines that the participant was currently taking. The educator focused on the process of setting up and following the participant’s regimen using a personalized medication calendar, communication with their caregivers, and inquiry about specific challenges participants face during navigation of the health care system. Participant’s individualized concerns in these areas were addressed. After their next rheumatology appointment, participants in the Individualized Care group had a second meeting with the study educator to talk about the notebook materials, and to discuss questions and concerns they may have had or that may have come up after reviewing or using the notebook. All participants in the Individualized Care group were scheduled to complete both appointments in the study. They were also encouraged to contact her for phone discussion or for in-person appointments for further information assistance over the next six months. The educator maintained a log of all reported difficulties as well as of helpful strategies from the participants for managing arthritis and to be shared with others.
The recruitment rate in the first years of the study (2003–2004) was slow, threatening successful completion. Thus, after 42 patients had been randomized, the study was redesigned by randomizing patients to only two groups, Standard Care and Individualized Care. The 13 participants enrolled in the Plain English group were absorbed into the Individualized Care group. However, since these participants had already completed the study, they did not meet with a study educator or receive any form of tailored intervention. Because of this, subsequent analyses were performed with and without the inclusion of these participants. The analyses presented include the Plain English group as part of the Individualized Care group unless otherwise noted.
2.3. Measures
The principal outcomes were fourfold: (1) adherence to treatments using a 4-item measure based on a questionnaire by Levine; (2) Lorig’s self-efficacy scale; (3) satisfaction with medical care based on the 8-item subscale of the Medical Interview Satisfaction Scale; and (4) appointment keeping by a question on the self-efficacy scale. (15–17) Secondary outcomes included self-reported health status assessed with the Health Assessment Questionnaire (HAQ) (18) and mental health assessed with the 5-item Mental Health Index from the SF-36. (19) In addition, the A-REALM, an arthritis-specific word recognition test based on and correlated with the REALM (Rapid Assessment of Adult Literacy in Medicine), a validated, reliable measure of health literacy, was used to measure health literacy skills as part of the baseline interview. (20) Participants were asked to read aloud a list of 66 arthritis-specific words and were given a point for each word they read correctly. The target sample size of 100 participants randomized to the two groups (Standard Care and Individualized Care) afforded 80% power to detect a statistically significant difference in outcomes for the medication adherence score and self-efficacy.
2.4. Study procedures
Self-efficacy for arthritis management, adherence to medication regimen, health status and satisfaction were assessed at baseline. Immediately after the clinical encounter which was recorded, the patient and physician completed independent reports on the quality of their encounter and described their current regimen. The RA collected these data along with the patient’s understanding of regimen medication schedule and purpose. These data is being analyzed separately. The patient was randomized to one of the interventions immediately after this visit.
Participants were followed at their next scheduled visit occurring at least six weeks later. This visit was also tape-recorded. Physicians completed written reports on the quality of their communication and description of current regimen; patients were interviewed for the same information. At six and twelve months post-intervention, self-efficacy for arthritis management, adherence to the medication regimen, health status, and usefulness of the material were assessed.
2.5. Statistical analysis
Baseline variables were compared between the two groups (data from participants in the Plain English group were included with data from participants in the Individualized Care group). Means were compared using two independent sample t-tests for continuous variables. Proportions were compared using the Chi-square test of independence or Fisher’s exact test for all categorical variables. Longitudinal data were analyzed as percent change between baseline and six months and between baseline and one year. These data were also analyzed using multivariate models where the baseline value was subtracted from subsequent values. Models were run with and without adjustment for covariates that differed at baseline between the groups. Models were run with and without inclusion of the Plain English group with the Individualized Care group. The physician pool was small and was not analyzed for differences. All statistical analyses were performed at a 5% level of significance using SAS statistical software version 9.1 (SAS Institute, Cary, NC).
3. Results
3.1. Recruitment
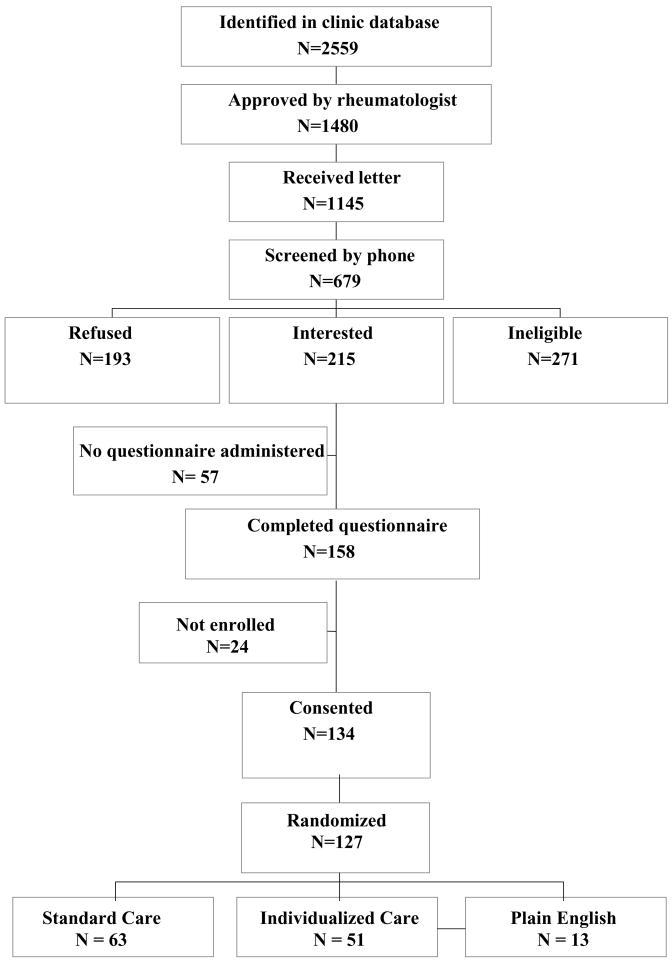
Detailed recruitment protocol and analysis of this multi-stage recruitment effort are published elsewhere.(21) As is illustrated in Figure 1, of 1145 patients sent a recruitment letter, 679 were reached by phone for the initial screening. Of those contacted by phone, about a third (N= 271) were ineligible, the modal reason being too high a level of education, and another third (N = 193) refused to participate, many of whom stated they were not interested or didn’t give a reason. We found no evidence of refusal to participate due to educational attainment, insurance status, or gender. Older patients were more likely to refuse participation.(21) One hundred fifty-eight patients went on to complete the baseline questionnaire, 134 of whom consented to the study, and ultimately 127 were randomized.
Figure 1.
Overview of patient recruitment and randomization
3.2. Baseline
The randomized patients (N=127) were predominantly female (N=101, 79%) and Caucasian (N=117, 92%), with an average of 13.0 ± 2.1 years of education. The mean age was 58.5 ± 13.8 years and mean disease duration was 16.6 ± 14.3 years. Forty-three percent of the sample was working full or part-time. Thirty percent had an annual family income below $30,000. Only 18% of the population scored at high school reading level or less on the A-REALM.
The study cohort was balanced on most variables. However, in the Standard Care group, significantly more patients were 65 year of age or older (43% vs. 25%; Chi-Square=4.5, p=.03) and significantly more patients reported an annual family income < $30,000 (39% vs. 20%; Chi-Square=5.4, p=.02) than in the combined Individualized Care and Plain English groups (Table 1). Of the outcome variables, only satisfaction with care differed significantly between the two groups at baseline, with the standard care group reporting greater satisfaction (3.9 vs. 3.7; T=−2.6, p= 0.01).
Table 1.
Baseline demographic and clinical characteristics
| Variable | Standard Care (N=63) | Individualized Care & Plain English (N=64) | p-valuea |
|---|---|---|---|
| Age, mean (SD) | 59.5 (13.9) | 57.6 (13.8) | .43 |
| N (%) | N (%) | ||
| Age >=65 years | 27 (43%) | 16 (25%) | .03 |
| Female | 49 (78%) | 52 (81%) | .63 |
| Caucasian | 59 (94%) | 58 (91%) | .53 |
| Education<= high school | 33 (52%) | 31 (48%) | .66 |
| Working full/part-time | 23 (36%) | 32 (50%) | .12 |
| Disease duration <5 yrs | 16 (25%) | 17 (27%) | .88 |
| Annual income <30K | 24 (39%) | 12 (20%) | .02 |
| A-REALMb <h=high school level | 12 (21%) | 10 (16%) | .44 |
| mean (SD) | Mean (SD) | ||
| HAQ score (0–3, 0=best) | 0.91 (0.66) | 0.93 (0.63) | .86 |
| Satisfaction score (1–4, 4=best) | 3.9 (0.29) | 3.7 (0.42) | .01 |
| Self-efficacy (1–4, 4=best) | 2.9 (0.48) | 2.8 (0.53) | .40 |
| SF 36 mental health subscale (0–100, higher is better) | 75.0 (18.4) | 74.5 (15.1) | .86 |
Chi-Square test for categorical variables; Student’s T-test for continuous variables
A-REALM: Arthritis modification to the REALM (rapid estimate of adult literacy in medicine
Analyses excluding the Plain English Group (N=114) showed the same magnitude of differences in age, annual family income and satisfaction score between the Standard Care and Individualized Care groups. However, the Individualized Care group had significantly more people working full or part-time (55% vs. 36%; Chi-Square=3.9, p=.05) than the Standard Care group.
3.3. Differences in Outcomes
Mean baseline and follow up scores at six and twelve months are shown in Table 2. Mean scores changed little over time. When percent change was examined, the intervention group showed improvement from baseline to six and twelve months in Mental Health Score (4.6 and 4.8 % change), while the standard care group had decreased scores (−4.3 and −0.8 % change) (Table 3). For self-efficacy, the intervention group improved more from baseline to twelve months (1.5 and 3.6% change) than the standard care group (−3.2 and −2.0% change). The differences between the Individualized Care and the Standard Care groups were statistically significant at six and twelve months at the p=0.05 level, with the exception of the percent change in mental health score at twelve months (p=0.11).
Table 2.
Mean and Standard deviation of measures at three time points for the two groups.
| Standard Care | Individualized Carea | |||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | 1 year | Baseline | 6 months | 1 year | |
| N | 63 | 57 | 57 | 51 | 49 | 48 |
| SF36 mental subscale (0–100, higher is better) | 75.0 (18.4) | 71.3 (23.9) | 73.0 (19.2) | 74.8 (12.6) | 77.7 (14.1) | 78.6 (15.3) |
| Satisfaction (1–4, 4 = best) | 3.89 (0.29) | 3.92 (0.18) | 3.86 (0.35) | 3.72 (0.41) | 3.77 (0.39) | 3.78 (0.36) |
| HAQ score (0–3, 0 = best) | 0.91 (0.66) | 0.92 (0.60) | 0.89 (0.67) | 0.92 (0.62) | 0.85 (0.65) | 0.84 (0.62) |
| Self-efficacy (1–4, 4 = best) | 2.87 (0.48) | 2.73 (0.59) | 2.78 (0.59) | 2.78 (0.49) | 2.83 (0.54) | 2.91 (0.63) |
| Medication adherenceb | 0.30 (0.37) | 0.24 (0.32) | 0.18 (0.30) | 0.40 (0.40) | 0.23 (0.28) | 0.17 (0.25) |
| Appointment keeping (0–3, 0 = best) | 0.56 (0.72) | 0.44 (0.60) | 0.63 (0.75) | 0.39 (0.60) | 0.29 (0.54) | 0.50 (0.82) |
Individualized Care group includes Plain English group (N = 13)
mean adherence of 4 questions on a 0–3 scale over all medications (0=best)
Table 3.
Percent change at 6 months and 12 months in outcome variables*
| % change (baseline to 6 months) | % change (baseline to 1 year) | |||||
|---|---|---|---|---|---|---|
| Outcome Measure | Standard Care | Individualized Carea | p-valueb | Standard Care | Individualized Carea | p-valueb |
| SF36 mental subscalec | −4.32 | 4.56 | .04 | −0.78 | 4.79 | .11 |
| Satisfactionc | 0.83 | 1.29 | .71 | −0.43 | 1.38 | .21 |
| HAQ scored | 3.30 | −0.30 | .45 | 1.33 | −0.79 | .64 |
| Self-efficacyc | −3.18 | 1.53 | .05 | −2.04 | 3.57 | .04 |
| Medication adherenced | 0.25 | −4.76 | .33 | −3.12 | −12.21 | .10 |
| Appointment keepingd | 0.89 | 0.00 | .91 | 13.39 | 13.19 | .98 |
Individualized Care group includes Plain English group (N= 13)
Student’s T-test
Scales show improvement with increased scores
Scales shows improvement with decreased scores
Note that the mean percent changes in Table 3 do not exactly correspond to the mean values in Table 2. The percent changes in Table 3 are calculated in patients that have both base line and follow-up values.
Sets of multivariate models adjusting for age, work status, literacy level, annual family income, and baseline value of outcome measure showed significantly better SF-36 mental status scores in the Individualized Care group as compared to the Standard Care group (adjusted mean difference between groups = 7.5 points, p=0.003). Analysis of the difference in least squared means for these models at six and twelve months showed that there was an intervention effect at both time periods, but the improvement in SF36 mental status was greater at six months (7.5 points, p=.01) than at twelve months (6.3 points, p=.03). While the intervention had a significant effect on self-efficacy in univariate analyses, this effect was no longer significant in multivariate models (p=0.12). No significant difference between groups was seen for the other primary and secondary outcomes.
4. Discussion and Conclusion
No differences between intervention groups were observed in the primary outcomes, including adherence to treatment and appointment keeping. However, the Individualized Care group did demonstrate greater improvement in mental health.
4.1. Discussion
The demonstration program undertaken here involved a well-known rheumatology practice in a large teaching hospital, which may draw on a patient population with stronger than average literacy and system navigation skills. The relatively high level of literacy among patients in our hospital made recruitment more challenging than we had anticipated, necessitating a change in design from a comparison of three groups to two groups. The Plain English Materials group we dropped would have helped us to interpret a benefit if the intervention had been substantially better than standard care. Given that these two groups did not differ on the primary endpoints, the loss of the Plain English Materials group had little effect on interpretation of the trial.
The study design was based on evidence that at least 20% of the hospital patient population had less than a high school education. Furthermore, we used recruitment strategies that reduced literacy related barriers to participation including plain language oral and written protocols and interview techniques. Strategies used in the recruitment protocol designed to remove literacy-related barriers to recruitment may be responsible for the observation that participants with lower education did not have higher refusal rates. Although these strategies were in place, recruitment proved problematic most likely because the clinic population did not include sufficient numbers of people with limited education not because of selection bias at our site. Consequently, the study was limited by drawing from a population with relatively strong literacy skills and higher educational attainment than might be found ordinarily in public hospital and community based settings. Participants also had relatively high levels of baseline satisfaction, adherence, and attendance; thus, a ceiling effect may have contributed to our inability to detect significant changes.
In addition, disease duration may well have influenced study outcomes. The average disease duration of the study population was 17 years. Clinicians generally seek to establish rapport and trust during their early encounters with patients. This sets the tone and expectations for future visits. Over time, the exchange and interactive patterns between a clinician and a patient may be firmly established. Furthermore, patients’ experience with arthritis, with arthritis information and sources of information, and with arthritis care increase over time as well. Thus, an educational intervention and informational materials may have less of an effect among experienced patients than among those with new diagnoses. A community based setting might have drawn more newly diagnosed patients.
4.2. Conclusion
We conclude that the intervention we developed did not have significant effects on the primary outcomes in this study. The modest improvement in mental health in the intervention group suggests the intervention may have relieved anxiety among participants. The improvements in mental health may reflect subtle benefits of the intervention that require confirmation in further study.
4.3. Practice Implications
We applied many of the protocols recommended to ameliorate effects of limited literacy – recruitment protocols designed to reduce literacy barriers, an emphasis on plain language in written and spoken communication, and expanded opportunities for tailored education.(22) It is possible that interventions such as ours would be shown to be beneficial in trials of patients with early arthritis and relatively low literacy skills.
Few studies to date have examined education programs designed for audiences with low literacy skills. Additional studies focused on mechanisms for minimizing effects of limited health literacy and providing a cost-benefit analysis comparing the use of plain language materials with time spent with an educator are called for.
Acknowledgments
Role of Funding: This work was supported in part by grants: NIH P60 AR 47782; NIH K24 AR 02123. The funding source had no involvement in data collection, analysis, or the preparation of this manuscript.
We honor the memory of Dr. Lawren Daltroy who designed this study but did not live to see its completion. We are grateful to Simha Ravven, Marsha Lynch and Kaleena Scamman for their recruitment efforts, interview and data entry skills, and assistance with materials design.
Footnotes
Conflict of Interest: All authors declare that they have no actual or potential conflict of interest including any financial, personal or other relationship with other people or organizations within three years of beginning the work submitted that could inappropriately influence (bias).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rima E. Rudd, Harvard School of Public Health, Department of Society, Human Development and Health, Boston, MA
Danielle C. Blanch, Department of Psychology, Northeastern University, Boston, MA
Victoria Gall, Brigham and Women’s Hospital, Division of Rheumatology, Immunology and Allergy, Boston, MA.
Lori B. Chibnik, Brigham and Women’s Hospital, Division of Rheumatology, Immunology and Allergy, Boston, MA
Elizabeth A. Wright, Brigham and Women’s Hospital, Division of Rheumatology, Immunology and Allergy/Department of Orthopaedic Surgery, Boston, MA
William Reichmann, Brigham and Women’s Hospital, Division of Rheumatology, Immunology and Allergy, Boston, MA.
Matthew H. Liang, Massachusetts Veterans Epidemiology Research and Information Center/Brigham and Women’s Hospital, Division of Rheumatology, Immunology and Allergy, Boston, MA
Jeffrey N. Katz, Brigham and Women’s Hospital, Division of Rheumatology, Immunology and Allergy/Department of Orthopaedic Surgery, Boston, MA
References
- 1.Kirsh IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America. Washington, DC: US Department of Education; 1993. [Google Scholar]
- 2.Kutner M, Greenberg E, Baer J. US Department of Education. Washington, DC: National Center for Education Statistics; 2005. A First Look at the Literacy of America’s adults in the 21st Century (NCES 2006-470) [Google Scholar]
- 3.Rudd RE. Health Literacy Skills of U.S. Adults. Journal of Health Behavior. 2007;31:S8–18. doi: 10.5555/ajhb.2007.31.supp.S8. [DOI] [PubMed] [Google Scholar]
- 4.Kutner M, Greenberg E, Jin Y, Paulsen C. US Department of Education. Washington, DC: National Center for Education Statistics; 2006. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. [Google Scholar]
- 5.Rudd RE, Anderson JE, Oppenheimer S, Nath C. Health Literacy: An Update of Public Health and Medical Literature. In: Comings JP, Garner B, Smith C, editors. Review of Adult Learning and Literacy. Vol. 7. Mahway NJ: Lawrence Erlbaum Associates; 2007. pp. 175–204. [Google Scholar]
- 6.The Joint Commission. Improving health literacy to protect patient safety. The Joint Commission; Oakbrook Terrace, IL: 2007. What did the doctor say? [Google Scholar]
- 7.Berkman N, DeWalt D, Pignone M, Sheridan S, Lohr K, Lux L, et al. Literacy and Health Outcomes. Evidence Report/Technology Assessment No. 87. Quality Agency for Healthcare Research and Quality. 2004 [PMC free article] [PubMed] [Google Scholar]
- 8.Rudd RE, Rosenfeld L, Gall V. Health literacy and arthritis research and practice. Current Opinion in Rheumatology. 2007;19:97–100. doi: 10.1097/BOR.0b013e328032782e. [DOI] [PubMed] [Google Scholar]
- 9.Pincus T, Keysor J, Sokka T, Krishnan E, Callahan LF. Patient questionnaires and formal education level as prospective predictors of mortality over 10 years in 97% of 1416 patients with rheumatoid arthritis from 15 United States private practices. J Rheumatol. 2004;31:229–34. [PubMed] [Google Scholar]
- 10.Institute of Medicine Committee on Health Literacy. Recommendation 6-1. National Academies Press; 2004. Health Literacy: A prescription to end confusion. [PubMed] [Google Scholar]
- 11.Rudd RE. Office of the Surgeon General. Washington DC; HHS: 2002. Health Literacy Action Plan, in Communicating Health. [Google Scholar]
- 12.McLaughlin G. SMOG grading: A new readability formula. Journal of Reading. 1969;12:639–46. [Google Scholar]
- 13.Brus H, VanDeLaar M, Rasker J, Weigman O. Compliance in rheumatoid arthritis and the role of formal patient education. Seminars Arthritis Rheum. 1997;26:702–10. doi: 10.1016/s0049-0172(97)80006-6. [DOI] [PubMed] [Google Scholar]
- 14.National Cancer Institute. Making Health Communications Work: A Planner’s Guide. Bethesda, MD: National Cancer Institute, USDHHS; 1989. NIH Pub. No. 89-1493. [Google Scholar]
- 15.Levine DM, Green LW, Deeds SG. Health education for hypertensive patients. J Amer Med Assoc. 1979;241:1700–3. [PubMed] [Google Scholar]
- 16.Lorig K, Chastain R, Ung E, Shoor S, Holman H. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32:37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 17.Wolf MH, Putnam SM, James SA, Stiles WB. The Medical Interview Satisfaction Scale: Development of a scale to measure patient perceptions of physician behavior. J Behav Med. 1978;1:391–401. doi: 10.1007/BF00846695. [DOI] [PubMed] [Google Scholar]
- 18.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23:137–45. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 19.Ware JEJ, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston: The Health Institute; 1993. [Google Scholar]
- 20.Davis TC, Michielutte R, Askov EN, Williams MV, Weiss BD. Practical assessment of adult literacy in health care. Health Educ Behav. 1998;25:613–24. doi: 10.1177/109019819802500508. [DOI] [PubMed] [Google Scholar]
- 21.Blanch DC, Rudd R, Wright E, Gall V, Katz JN. Predictors of refusal during a multistep recruitment process for a randomized controlled trial of arthritis education. Pat Educ Couns. 2008;73:280–5. doi: 10.1016/j.pec.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rudd RE. The importance of literacy in research and in practice. Nature Clinical Practice Rheumatology. 2007;3:479. doi: 10.1038/ncprheum0576. [DOI] [PubMed] [Google Scholar]