Abstract
Objective
To assess the number of procedures required to achieve optimal competency (time required for surgery with minimal adverse events) in Rakai, Uganda, and thus facilitate the development of guidelines for training providers, as male circumcision reduces the acquisition of human immunodeficiency virus (HIV) in men and is recommended for HIV prevention.
Patients and methods
In a randomized trial, 3011 men were circumcised, using the sleeve method, by six physicians who had completed training, which included 15–20 supervised procedures. The duration of surgery from local anaesthesia to wound closure, moderate or severe surgery-related adverse events (AEs), and wound healing were assessed in relation to the number of procedures done by each physician.
Results
The median age of the patients was 24 years. The number of procedures per surgeon was 20–981. The mean time required to complete surgery was ≈40 min for the first 100 procedures and declined to 25 min for the subsequent 100 circumcisions. After controlling for the number of procedures there was no significant difference in duration of the surgery by patient HIV status or age. The rate of moderate and severe AEs was 8.8% (10/114) for the first 19 unsupervised procedures after training, 4.0% for the next 20–99 (13/328) and 2.0% for the last 100 (P for trend, 0.003). All AEs resolved with management.
Conclusion
The completion of more than 100 circumcisions was required before newly trained physicians achieved the optimum duration of surgery. AEs were higher immediately after training and additional supervision is needed for at least the first 20 procedures after completing training.
Keywords: male circumcision, Uganda, duration of surgery, adverse events
Introduction
Circumcision has been shown to reduce HIV infections in men by more than half [1–3] and has now been recommended by WHO/United Nations (UN)-AIDS for HIV prevention [4]. The development of large-scale circumcision programmes is a priority and will require training of a large cadre of surgeons, particularly in Eastern and Southern Africa, where circumcision is uncommon and HIV rates are high [5]. To plan this increase in the scale of circumcision program managers need to know the time required for surgery and how the duration of surgery varies as practitioners gain more experience. Such information is needed because surgical duration dictates the number of procedures that can be done each day. In addition, planners need to know whether newly trained personnel can safely perform circumcisions, and whether complication rates vary with the experience of practitioners. We used data from male circumcision trials in Rakai, Uganda [2,5,6] to assess the experience required to achieve optimal surgical competency as measured by the duration of surgery and rates of surgery-related adverse events (AEs), to facilitate development of guidelines for training and service programmes.
Patients and methods
The design of the trials was reported previously [1,6]. For this analysis we assessed 2321 HIV-negative and 389 HIV-positive men aged 15–49 years who were randomized to the intervention arm of the two Rakai circumcision trials. One trial, supported by the National Institutes of Health, enrolled HIV-negative men who agreed to receive their HIV results and counselling after the test; the second trial enrolled HIV-infected men with a CD4 count of > 350. Screening, enrolment and randomization were identical in both trials. In brief, participants were informed of the study procedures, risks and benefits, and provided separate written informed consent for screening, enrolment and surgery. Eligibility criteria for surgery included a haemoglobin level of ≥8 g/dL, and the absence of general or local genital contraindications. Men with treatable conditions such as anaemia, genital discharge, dysuria, ulceration or balanitis were treated and re-screened before surgery. Those with anatomical conditions that were an indication for or contraindication to surgery were referred to a urologist for care and were excluded from the trial.
Men assigned to the intervention arm were provided with detailed information on the procedure, postoperative wound care, genital hygiene and the need to abstain from sexual intercourse until complete wound healing had been certified. Information sheets were given to the men to share with their spouses or partners.
All surgeons and operating room assistants had at least 2 weeks of training by a urologist from Mulago Hospital, Kampala (S.W.), based on the WHO/UNAIDS Manual for Circumcision under Local Anaesthesia [7]. The surgeons were all physicians who had no previous experience with adult circumcision, received practical training in preoperative preparation and asepsis, local anaesthesia, the sleeve circumcision procedure, suturing, haemostasis, management of surgical emergencies and AEs. The physicians performed 15–20 supervised circumcisions during training.
Surgery was performed in well-equipped outpatient operating rooms. All instruments, drapes and other sterile materials were autoclaved and sterility was assured by the use of biological and thermal indicators. Skin preparation was by povidone-iodine and a soft brush for 3 min. Local anaesthesia was administered by a dorsal penile nerve block, with a 4–7 mL mixture of 1% lignocaine and 0.25% bupivacaine, injected in each of two positions at the dorsum close to the mons pubis, plus 0.5–3 mL at the frenulum. The prepuce was retracted and the site of the distal incision was marked at 0.5–1 cm proximal to the coronal sulcus using a sterile marking pencil. Similarly, the site of the proximal incision was marked along the outline of the coronal sulcus on the exterior surface of the unretracted prepuce. Incisions were made following the markings up to Buck’s fascia; followed by a dorsal slit between the two incisions. The foreskin (sleeve) was then dissected along Buck’s fascia. Haemostasis was achieved using bipolar cautery and sutures. Wound edges were approximated with chromic catgut 4/0 or polyglactin rapid 4/0 (Johnson and Johnson Corp, USA), starting with a simple suture at the frenulum; and four principal sutures (a horizontal mattress at the frenulum, and three vertical mattress sutures at the 3, 9 and 12 o’clock positions), with two or three simple sutures between the primary sutures. The wound was dressed using a petroleum jelly gauze impregnated with chlorhexidine, followed by an outer dry sterile gauze, followed by an elastic bandage. The time from the administration of local anaesthesia to wound closure was recorded. Patients rested for at least 30 min; vital signs were monitored and paracetamol was administered before discharge. Follow-up visits were conducted on the first day (removal of outer dressing), at 5–9 days and 4–6 weeks. At each visit, AEs and the status of wound healing were recorded. Participants were asked about symptoms suggestive of potential complications (pain, bleeding, wound dehiscence, swelling, pus discharge, etc.), resumption of sexual intercourse and condom use among those who resumed intercourse. The wound was then inspected to assess healing and to diagnose AEs.
AEs were monitored during scheduled and unscheduled visits, and graded as mild (requiring no treatment), moderate (requiring treatment), or severe (requiring surgical intervention such as wound exploration for active bleeding, repair of wound dehiscence or hospitalization). AEs were predefined and coded. AEs were reviewed by a panel consisting of medical and clinical officers, the chief urologist (S.W.), and the principal investigator (R.H.G.). Severe AEs were reported promptly to relevant institutional review boards.
The mean and 95% CI of the duration of surgery were assessed in relation to the number of procedures done by the six surgeons. The numbers of procedures were stratified into sequential groups of 20, up to 1000. Moderate and severe surgery-related AEs were estimated as a percentage of the number of procedures, and were stratified into sequential groups of 20.
Results
In all, 3011 men aged 15–49 years were circumcised, of whom 2622 (87.1%) were HIV-negative and 389 (12.9%) were HIV-positive (Table 1). The median and mean ages were 24 and 26.1 years, respectively. Six surgeons performed the circumcisions and the minimum and maximum number of procedures per surgeon were 20 and 981, respectively.
Table 1.
The population characteristics and procedures
| Characteristics | N (%) |
|---|---|
| Total (observations) | 3011 (100) |
| Age, years | |
| 15–19 | 724 (24.05) |
| 20–29 | 1363 (69.31) |
| 30–39 | 712 (23.65) |
| 40–49 | 212 (7.04) |
| HIV status | |
| positive | 389 (12.92) |
| negative | 2622 (87.08) |
| Surgeon | |
| 1 | 220 (7.31) |
| 2 | 910 (30.22) |
| 3 | 20 (0.66) |
| 4 | 854 (28.36) |
| 5 | 981 (32.58) |
| 6 | 26 (0.86) |
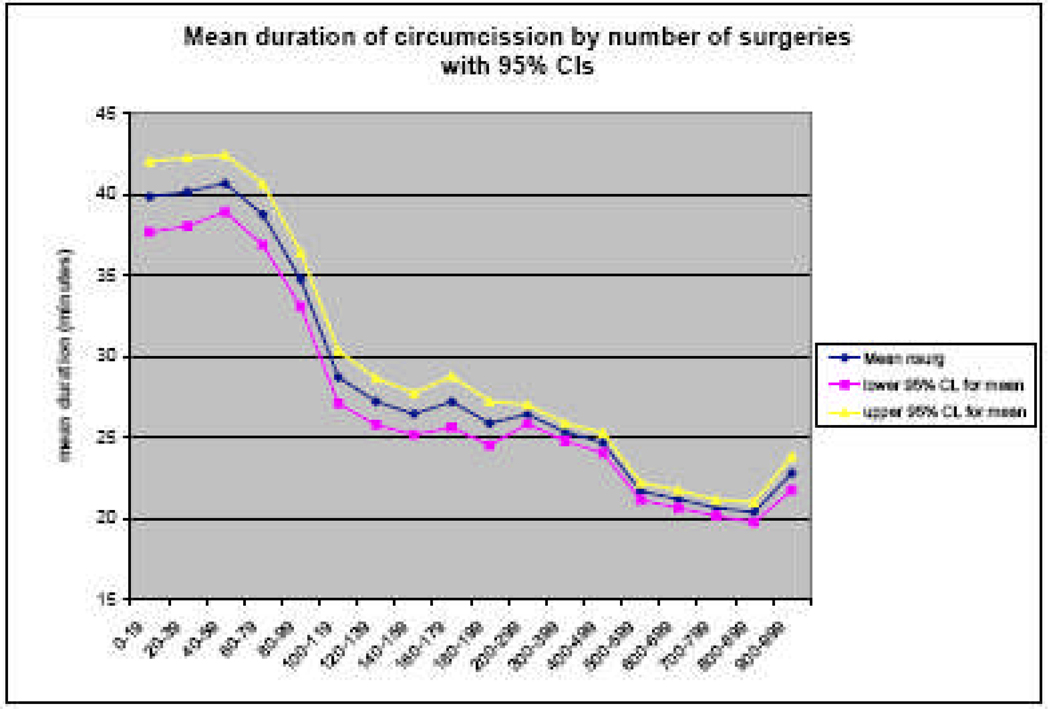
Figure 1 shows the mean (95% CI) of the time required for surgery by number of procedures. The mean duration of surgery was ≈40 min for the first 80–100 procedures, and then declined to 27.1 min for the second 100 (P < 0.001). Ultimately the duration of surgery declined to ≈20 min per procedure after completing ≈600 circumcisions. The median duration of surgery was similar to the mean. The duration of surgery initially differed between surgeons but converged to ≈25 min for all surgeons after ≈100 procedures. There were no statistically significant differences in the duration of surgery between HIV-infected and uninfected men (P = 0.15). Younger patients aged 15–19 years required a shorter duration than the older groups, but this was not statistically significant.
Fig. 1.
Mean and 95% CI of the duration of surgery by the number of circumcisions.
Table 2 shows the rate of surgery-related moderate and severe AEs requiring treatment. During the first 20 unsupervised procedures after training, the AE rate was 8.8% (10/114) and then declined to 4.0% (13/328) for the next 20–99 procedures, stabilizing at ≈2% for the next 100 (8/400 procedures). This trend was statistically significant (P = 0.003). All AEs resolved with management. There were five (0.17%) severe AEs, which included one wound infection, two haematomas that required exploration and ligation of bleeding vessels, one wound disruption (due to an external cause), and a case of herpetic ulceration that did not involve the surgical site but required hospitalization for management.
Table 2.
Moderate and severe AEs by number of circumcisions performed
| No. of procedures |
No. of circumcisions |
N (%) moderate/severe AEs |
|---|---|---|
| 0–19 | 114 | 10 (8.8) |
| 20–39 | 88 | 3 (3.4) |
| 40–59 | 80 | 2 (2.5) |
| 60–79 | 80 | 4 (5.0) |
| 80–99 | 80 | 4 (5.0) |
| 100–199 | 400 | 8 (2.0) |
| 200–299 | 321 | 8 (2.5) |
| 300–399 | 300 | 12 (4.0) |
| 400–499 | 300 | 7 (2.3) |
| 500–599 | 300 | 14 (2.5) |
| 600–699 | 300 | 3 (1.0) |
| 700–799 | 300 | 7 (2.3) |
| 800–899 | 255 | 11 (4.3) |
| 900–999 | 93 | 2 (2.2) |
| Total | 3011 | 95 |
Discussion
Newly trained surgeons required ≈40 min to perform circumcision for their first 80–100 cases, and the duration of surgery declined thereafter to ≈25 min. This suggests that programmes should plan to schedule fewer circumcisions per day until newly trained practitioners can accumulate substantial experience. The rates of AEs were significantly greater (8.8%) during the first 20 unsupervised procedures after training, and then declined with greater experience. This suggests that newly trained physicians require at least 20 supervised procedures after training to minimize the risk of AEs.
There are limitations to this study that might affect its general applicability. First, all surgeons were medical practitioners, and we do not know whether those who are not physicians can achieve comparable surgical times and AE rates. Studies of traditional circumcisions or surgery performed by medical personnel in less optimal circumstances are associated with substantially higher complication rates [8,9]. Our findings also do not apply to industrialized countries, where adult circumcision would most likely be done by trained surgeons who would almost certainly learn more quickly and have fewer AEs. Second, the trial had strict eligibility criteria and excluded men with penile pathology and current genital infections. Such criteria might not always be adhered to in large service programmes. Third, the physicians in the trial carried out up to 11 circumcisions per day, and had no other clinical or surgical responsibilities during the trial. They thus had a level of experience and focus which is unlikely to be replicated in many service settings. We also do not know how their skills would be maintained should they stop doing circumcisions for some protracted period and then resume surgery. Finally, we only assessed the sleeve circumcision procedure and cannot determine whether the forceps-guided or dorsal-slit methods might differ in surgical duration or complications. A Kenyan study [10,11] reported a median duration of surgery of ≈37 min for the first 100 procedures and subsequent declines in the duration of surgery, which is similar to patterns reported here. We found no statistically significant difference in the mean duration of surgery for HIV-positive and -negative men, and a previous Rakai study found that AEs were comparable in these two groups [6]. However, HIV-infected men in this trial had CD4 counts of > 350, and surgical outcomes might be different in men with lower CD4 counts.
In conclusion, programmes should consider the longer surgical times required for the first 100 circumcisions after training, so they do not overburden newly trained surgeons. Also, it would be advisable to provide supervision for at least 20 circumcisions after training, to reduce the risk of surgery-related AEs. As training in this study required 15–20 supervised procedures, this finding suggests that training programmes should plan for 35–40 supervised circumcisions to minimize complications.
Acknowledgements
The trials were funded by the National Institutes of Health (#U1AI51171), the Bill and Melinda Gates Foundation (#22006.02) and the Fogarty International Center (#5D43TW001508 and #D43TW00015). The trials are registered with ClinicalTrials.gov numbers NCT00425984 for HIV-negative men and NCT00124878 for HIV-positive men.
Abbreviations
- UN
United Nations
- AE
adverse event
Footnotes
Conflict of Interest
None declared.
Contributor Information
Valerian Kiggundu, Rakai Health Sciences Program, Entebbe.
Stephen Watya, Department of Surgery, Urology unit, Mulago Hospital.
Godfrey Kigozi, Rakai Health Sciences Program, Entebbe.
David Serwadda, School of Public Health, Makerere University, Kampala.
Fred Nalugoda, Rakai Health Sciences Program, Entebbe.
Denis Buwembo, Rakai Health Sciences Program, Entebbe.
Adrian Settuba, Rakai Health Sciences Program, Entebbe.
Margaret Anyokorit, Rakai Health Sciences Program, Entebbe.
James Nkale, Rakai Health Sciences Program, Entebbe.
Noah Kighoma, Rakai Health Sciences Program, Entebbe.
Victor Sempiija, Rakai Health Sciences Program, Entebbe.
Maria Wawer, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA.
Ronald H. Gray, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA
References
- 1.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. Plos Med. 2005;2:1112–1122. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 3.Bailey RSM, CBP, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 4.WHO/UNAIDS. Male Circumcision and HIV Prevention: Research Implications for Policy and Programming. Montreux: 2007. Mar 6–8, [DOI] [PubMed] [Google Scholar]
- 5.Wawer M, Kigozi G, Serwadda D, et al. Trial of male circumcision in HIV+ men, Rakai, Uganda: Effects in HIV+ men and in women partners. 15th Conference on Retroviruses and Opportunistic Infections; February 3–6 2008; Boston. p. 33LB. [Google Scholar]
- 6.Kigozi G, Gray RH, Wawer MJ, Serwadda D, et al. The safety of adult male circumcision in HIV-infected and uninfected men in Rakai, Uganda. PLos Medicine. 2008;5:e116. doi: 10.1371/journal.pmed.0050116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO/UNAIDS, JHPIEGO. Manual for Male Circumcision under Local Anaesthesia. Geneva: 2008. Jan, Version 2.5C. [Google Scholar]
- 8.Bailey RC, Egesah O. Special Report. Washington, DC: USAID, PSI Aidsmark; 2006. Assessment of clinical and traditional male circumcision services in Bungoma District, Kenya. Complication rates and operational needs; pp. 1–39. [Google Scholar]
- 9.Okeke LI, Asinobi AA, Ikuerowo OS. Epidemiology of complications of male circumcision in Ibadan, Nigeria. BMC Urology. 2006:6. doi: 10.1186/1471-2490-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krieger JN, Bailey RC, Opeya J, et al. Adult male circumcision. Results a standardized procedure in Kisumu District, Kenya. BJU Int. 2005;96:1109–1113. doi: 10.1111/j.1464-410X.2005.05810.x. [DOI] [PubMed] [Google Scholar]
- 11.Krieger JN, Bailey RC, Opeya JC, et al. Adult male circumcision outcomes: experience in a developing country setting. Urologia Intis. 2007;78:235–240. doi: 10.1159/000099344. [DOI] [PubMed] [Google Scholar]