Abstract
Background/Objective
Atrial fibrillation(AF) has been shown in numerous studies to significantly decrease patient quality of life. The Cox-Maze procedure has excellent long-term efficacy in curing AF. However, it is unknown whether this procedure improves long-term quality of life in these patients. The purpose of this study was to examine late quality of life in patients that underwent a lone Cox-Maze procedure.
Methods
Between 1987 and 2003, 163 patients underwent a Cox-Maze procedure for lone AF at our institution. Of these, 68 patients agreed and completed the Medical Outcomes Study Short Form 36 Health Survey. Scores from the age-matched general US population were normalized to a mean of 50 and standard deviation of 10 to facilitate comparison. Collected data were compared to the norm-based score for each domain using a one-sample t-test. Four patients were removed from analysis because of AF recurrence.
Results
There were 52 males(81%). Mean age was 52.6±9.5 years. Preoperatively, 37 patients(58%) had paroxysmal and 25 patients(39%) had persistent or permanent AF. The mean duration of AF before surgery was 9.8±8.2 years. There was no statistical difference in norm-based scores between the Cox-Maze procedure group and the age-matched general US population in any of the eight health domains at a mean follow-up of 8.7±3.7 years.
Conclusion
Our results suggest that the Cox-Maze procedure cures atrial fibrillation in the majority of patients, and that those patients that are cured obtain a normal quality of life as compared to the general population at late follow-up.
Keywords: atrial fibrillation, maze procedure, quality of life
INTRODUCTION
Atrial fibrillation (AF) is the most common of all sustained cardiac arrhythmias.1 The morbidity associated with atrial fibrillation includes patient discomfort and anxiety, hemodynamic compromise, thromboembolic complications, and others.2 These symptoms lead to a significant impairment in quality of life in patients with AF, comparable to patients with a recent myocardial infarction or congestive heart failure.3
Current management of atrial fibrillation includes antiarrhythmic drug therapy, cardioversion, percutaneous transcatheter ablation, and surgery. Although drugs can induce chemical cardioversion, their failure rate in some series is as high as 60% at 12-month follow-up.4 Additionally, rate and rhythm control have not improved the quality of life in AF patients to levels comparable to age-matched healthy individuals.5
First implemented in the late 1980s, the Cox-Maze procedure has become the gold standard for the surgical treatment of AF. It effectively restores both atrioventricular synchrony and a regular heartbeat, and virtually eliminates the late risk of thromboembolism and stroke.6–9 Long-term success rates have been reported in excess of 90% at our institution and by others around the world.9–14 The procedure consists of a series of maze-like incisions or ablations on both atria originally designed to prevent the macro-reentrant circuits that were felt to be responsible for AF.6, 15
After the first two iterations of the Cox-Maze procedure, the Cox-Maze III was first performed in 1988 and became the standard surgical treatment of AF for more than a decade.7, 9 Recently, various energy sources have been used to create ablation lines to replace the surgical incisions of the procedure including unipolar radiofrequency, microwave, laser, high frequency ultrasound, and cryoablation16–23. At our institution, this technology led to the development of the Cox-Maze IV, which was first performed in 2002. In this procedure many of the traditional cut and sew lesions of the traditional version are replaced with linear lines of ablation using bipolar radiofrequency energy14. This energy source was chosen due to its efficacy and speed at creating long transmural lesions. Our early experience with the simplified procedure recorded comparable success rates to the Cox-Maze III procedure with freedom from AF at last follow-up of >90%.24–26
Despite the high success rate of the Cox-Maze procedure, little information exists on the effect of the surgery on quality of life. The purpose of this study was to examine the impact on late quality of life in patients treated for AF by a lone Cox-Maze procedure.
PATIENTS AND METHODS
Between 1987 and 2003, 163 patients underwent a lone Cox-Maze procedure for the treatment of AF. The patients’ clinical profiles and postoperative outcomes were recorded prospectively in a computerized database.
To assess health-related quality of life, patients were mailed the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36).27, 28 The SF-36 measured eight quality of life health domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health. The scores may range from 0 (worst) to 100 (best). To allow comparison of the general US population with Cox-Maze procedure treated AF patients, age-matched general US population scores were normalized to a mean of 50 and a standard deviation of 10. 27, 28
Sixty-eight patients (42%) agreed and completed the SF-36 questionnaire. Data collected from the completed SF-36 questionnaires were compared to the normalized, age-matched general US population scores. Patients had follow-up visits scheduled for one, three, six, and 12 months postoperatively, and were then followed annually. At all follow-up visits, a history and physical exam and an electrocardiogram were obtained. For patients who could not return to our institution, telephone questionnaires were performed and electrocardiograms were obtained from referring physicians to document the heart rhythm. In patients with symptoms of palpitations, holter or event monitoring was obtained to assess their rhythm status. Four of the 68 patients (6%) were removed from analysis because of atrial fibrillation recurrence.
Statistical analyses were completed using QualityMetric Inc. licensed scoring software (Lincoln, RI). Comparison of the age-matched general US population to the lone Cox-Maze treated patients was made using a two-tailed one-sample t test. The null hypothesis was rejected at a P value of less than .05. Values reported in the tables and text are means ± SD (unless otherwise noted).
This study was approved by the Washington University School of Medicine/Barnes-Jewish Hospital Institutional Review Board. Informed consent and permission for the release of information were obtained from each participant.
RESULTS
Patient Demographics
Fifty-two (81%) of the patients were men, and 12 (19%) were women. Mean age was 52.6 ± 9.5 years (range, 31–73 years). There were 38 (59%) patients with paroxysmal AF and 26 (41%) with persistent or permanent AF. The mean preoperative duration of AF was 9.8 ± 8.2 years (range, 1 to 39 years; Table 1). Mean New York Heart Association (NYHA) heart failure class was 1.2 ± 0.6, while 4.7% (3/64) of patients were NYHA class III or IV.
TABLE 1.
Demographic and perioperative data
| Age, years (mean ± SD) | 52.6 ± 9.5 |
| Male gender | 52 (81.2) |
| Type of AF | |
| Paroxysmal | 37 (57.8) |
| Chronic | 25 (39.1) |
| Indication for surgery | |
| Arrhythmia intolerance | 45 (70.3) |
| Medication failure | 8 (12.5) |
| TIA | 8 (12.5) |
| CVA | 3 (4.7) |
| Duration of AF, years (mean ± SD) | 9.8 ± 8.2 |
| Cox-Maze version | |
| I | 11 (17.2) |
| II | 7 (10.9) |
| III | 43 (67.2) |
| IV | 3 (4.7) |
| Preoperative NYHA class (mean ± SD) | 1.2 ± 0.6 |
| Median length of hospital stay (range) | 10 days (4–42 days) |
Data are presented as the number of patients (%) unless otherwise specified. Type of atrial fibrillation data was not available for two patients. All operations were lone Cox-Maze procedures. AF, Atrial fibrillation; TIA, transient ischemic attack; CVA, cerebrovascular accident.
Surgical Characteristics
Indications for surgery were arrhythmia intolerance (n = 45, 70%), medication failure (n = 8, 13%), transient ischemic attack (n = 8, 13%), and cerebrovascular accident (n = 3, 5%). The versions of the Cox-Maze procedure have been previously described.13, 14 Eleven (17%) patients received the Cox-Maze I procedure, 6 (9%) the Cox-Maze II, 44 (69%) the Cox-Maze III, and 3 (5%) the Cox-Maze IV. Surgical complications included stroke (2 patients), mediastinitis (2 patients), reoperation for bleeding (3 patients), atrial tachyarrhythmia (24 patients), and pacemaker placement (14 patients). Median length of hospital stay was 10 days (range 4–42 days).
SF-36 Health Survey Data
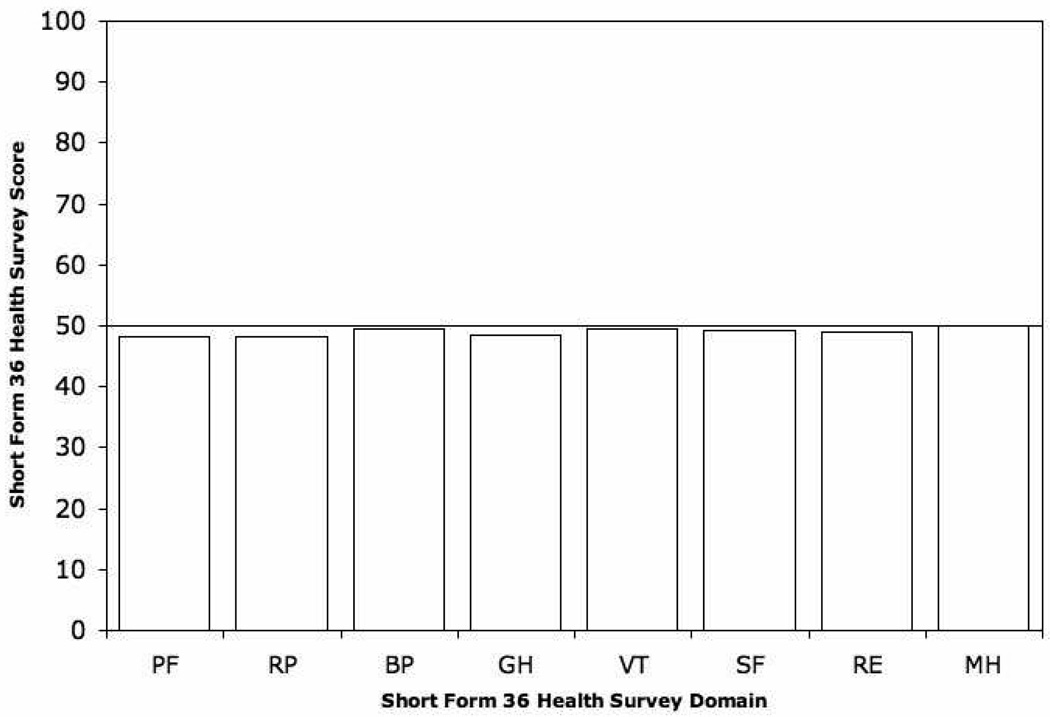
SF-36 scores of the age-matched general US population were normalized to a score of 50 with a standard deviation of 10. After a mean follow-up for the lone Cox-Maze procedure group of 8.7 ± 3.7 years (median follow-up 9.4 years, range 0.6–15.9 years), 4/64 (6%) were on anti-arrhythmia medications, and 11/64 (17%) were on Coumadin. SF-36 scores were: physical functioning 48.3 ± 9.9 (p = 0.17), role physical 48.2 ± 11.2 (P = .19), bodily pain 49.6 ± 12.5 (p = .81), general health 48.5 ± 10.8 (p = 0.26), vitality 49.6 ± 12.4 (P = 0.79), social functioning 49.2 ± 9.7 (p = .50), role emotional 49.0 ± 10.6 (P = 0.45), and mental health 50.0 ± 10.8 (p = 0.98). There was no statistical difference in norm-based scores between the Cox-Maze procedure group and the age-matched general US population in any of the eight measured health domains measured by the SF-36 survey (Table 2; Figure 1).
TABLE 2.
Short Form 36 Health Survey Data from Cox-Maze treated patients
| Measured scale | Response | p-value |
|---|---|---|
| Physical functioning | 48.3 ± 9.9 | 0.17 |
| Role – physical | 48.2 ± 11.2 | 0.19 |
| Bodily pain | 49.6 ± 12.5 | 0.81 |
| General health | 48.5 ± 10.8 | 0.26 |
| Vitality | 49.6 ± 12.4 | 0.79 |
| Social functioning | 49.2 ± 9.7 | 0.50 |
| Role – emotional | 49.0 ± 10.6 | 0.45 |
| Mental health | 50.0 ± 10.8 | 0.98 |
Patient response values compared with scores from the age-matched general US population that were normalized to 50 ± 10.
Figure 1.
Mean quality of life scores after treatment of atrial fibrillation by the Cox-Maze procedure. Patient response values compared with scores from the age-matched general US population that were normalized to 50 ± 10 (line). PF, Physical functioning; RP, role – physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role – emotional; MH, mental health.
DISCUSSION
The Cox-Maze procedure is highly effective in the long-term treatment of AF and essentially eliminates the incidence of stroke.8, 9, 11, 12 In the past, the success of this procedure and other treatments of AF have been evaluated based on late freedom from recurrent AF. However, even though the efficacy of the Cox-Maze procedure is well-documented for curing AF, the effects of the surgery on the quality of life have only been examined in a single study of 48 patients.29 In contrast, the impact of AF intervention strategies on quality of life has been examined much more extensively for the current medical treatment modalities.
The first-line treatment for patients suffering from AF is rate or rhythm control. Even the rhythm control treatment strategy offers only a limited cure rate, as the recurrence of AF at one year averages about 50%, with some antiarrhythmic drugs showing failure rates as high as 30–60%.4, 30 Few studies have found some improvement of quality of life with medical treatment,31 but several have found no improvement or even a decrease. Quality of life of this treatment option was evaluated by investigators of the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. They found that not only was quality of life decreased in both pharmacologic treatment strategies of rate and rhythm control, but also that quality of life was also similarly decreased in unsuccessfully treated patients (those that remained in AF) compared to those that reverted to sinus rhythm.5 Comparable findings were revealed in the Rate Control Versus Electrical Cardioversion (RACE) study.32 These investigators found only a minor improvement in quality of life with rate control and no significant change with rhythm control. Researchers in the double-blind, placebo-controlled Sotalol Amiodarone Atrial Fibrillation Efficacy Trial (SAFE-T) demonstrated no significant differences in the quality of life scores from baseline and at a 12 month follow-up in the sotalol, amiodarone, and placebo randomized groups except for a decrease in the mental health score in the amiodarone group.33 In contrast, this study revealed that following a successful surgical procedure patients reported health scores equivalent to a healthy age-matched population.
Recently, studies have shown that ectopic foci located in the pulmonary veins are responsible for the initiation of atrial fibrillation in a majority of patients with paroxysmal AF.34 This finding has led investigators to examine the effects of catheter-based pulmonary vein isolation as a therapeutic technique. Early data suggests that pulmonary vein ablation may be a more effective treatment of curing AF than antiarrhythmic drug therapy alone, with success rates using pulmonary vein ablation therapy still between 52–87%. Pulmonary vein ablation therapy has been shown to increase quality of life from baseline in several studies at 3–12 months of follow-up.35–37
The Cox-Maze procedure has demonstrated cures rates consistently exceeding 90% in the treatment of AF, and this high efficacy was maintained in this study population (94%). However, in the past little attention has been given to how this treatment strategy impacts quality of life. Using the SF-36 survey, the effect of the Cox-Maze procedure on postoperative quality of life was examined. This form has been used extensively in many studies, and the detailed explanation of its implementation and interpretation can be found in the literature27, 28. When quality of life was examined, scores in all eight subscales of the SF-36 were equivalent to age-matched general US population scores. Although these patients who underwent the Cox-Maze procedure did not have a baseline survey, they likely suffered from the same physical and emotional complaints as previously reviewed patients with AF.3 Swedish patients that underwent a Cox-Maze procedure had significantly lower quality of life scores before surgery on all scales, except for bodily pain, than for the age-matched general Swedish population.29 Indeed, in this population the patients may have suffered more than the general population with the disease, as they have pursued aggressive surgical treatment to seek relief of symptoms.
Our data suggests that the Cox-Maze procedure cures atrial fibrillation in the majority of patients, and it also allows them to obtain a normal quality of life at late follow-up compared to age-matched general US population. Patients who suffer from the myriad of symptoms from AF should be offered surgery for treatment, as it is efficacious in curing the disease as well as restoring patients to a normal quality of life.
Study Limitations
This study lacks baseline SF-36 scores from patients undergoing the Cox-Maze procedure, which would have been helpful for comparison. In order to associate an improvement in quality of life directly to the procedure these data should have been obtained. However, the decreased quality of life in this patient population has been well described. A randomized, prospective trial comparing quality of life between Cox-Maze, pulmonary vein ablation, and drug treated groups would be desirable to determine which intervention provided the best outcome.
A sampling bias may exist in this study, as 42% of people responded to questionnaires. A higher participation may have revealed a difference of quality of life versus controls. Finally, this study was completed for patients who had the Cox-Maze procedure for lone atrial fibrillation, and not with concomitant cardiac disease. These results may not be generalizable to patients with concomitant heart pathology.
Acknowledgments
This study was funded in part by National Institutes of Health Grants R01-HL032257 and F32 HL078136-01.
REFERENCES
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 3.Dorian P, Jung W, Newman D, Paquette M, Wood K, Ayers GM, Camm J, Akhtar M, Luderitz B. The impairment of health-related quality of life in patients with intermittent atrial fibrillation: implications for the assessment of investigational therapy. J Am Coll Cardiol. 2000;36:1303–1309. doi: 10.1016/s0735-1097(00)00886-x. [DOI] [PubMed] [Google Scholar]
- 4.Naccarelli GV, Wolbrette DL, Khan M, Bhatta L, Hynes J, Samii S, Luck J. Old and new antiarrhythmic drugs for converting and maintaining sinus rhythm in atrial fibrillation: comparative efficacy and results of trials. Am J Cardiol. 2003;91:15D–26D. doi: 10.1016/s0002-9149(02)03375-1. [DOI] [PubMed] [Google Scholar]
- 5.Jenkins LS, Brodsky M, Schron E, Chung M, Rocco T, Jr, Lader E, Constantine M, Sheppard R, Holmes D, Mateski D, Floden L, Prasun M, Greene HL, Shemanski L. Quality of life in atrial fibrillation: the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. Am Heart J. 2005;149:112–120. doi: 10.1016/j.ahj.2004.03.065. [DOI] [PubMed] [Google Scholar]
- 6.Cox JL, Schuessler RB, D'Agostino HJ, Jr, Stone CM, Chang BC, Cain ME, Corr PB, Boineau JP. The surgical treatment of atrial fibrillation. III. Development of a definitive surgical procedure. J Thorac Cardiovasc Surg. 1991;101:569–583. [PubMed] [Google Scholar]
- 7.Cox JL, Boineau JP, Schuessler RB, Jaquiss RD, Lappas DG. Modification of the maze procedure for atrial flutter and atrial fibrillation. I. Rationale and surgical results. Journal of Thoracic & Cardiovascular Surgery. 1995;110:473–484. doi: 10.1016/S0022-5223(95)70244-X. [DOI] [PubMed] [Google Scholar]
- 8.Cox JL, Ad N, Palazzo T. Impact of the maze procedure on the stroke rate in patients with atrial fibrillation. J Thorac Cardiovasc Surg. 1999;118:833–840. doi: 10.1016/s0022-5223(99)70052-8. [DOI] [PubMed] [Google Scholar]
- 9.Prasad SM, Maniar HS, Camillo CJ, Schuessler RB, Boineau JP, Sundt TM, 3rd, Cox JL, Damiano RJ., Jr The Cox maze III procedure for atrial fibrillation: long-term efficacy in patients undergoing lone versus concomitant procedures. J Thorac Cardiovasc Surg. 2003;126:1822–1828. doi: 10.1016/s0022-5223(03)01287-x. [DOI] [PubMed] [Google Scholar]
- 10.Raman J, Ishikawa S, Storer MM, Power JM. Surgical radiofrequency ablation of both atria for atrial fibrillation: results of a multicenter trial. J Thorac Cardiovasc Surg. 2003;126:1357–1366. doi: 10.1016/s0022-5223(03)01185-1. [DOI] [PubMed] [Google Scholar]
- 11.McCarthy PM, Gillinov AM, Castle L, Chung M, Cosgrove D., 3rd The Cox-Maze procedure: the Cleveland Clinic experience. Semin Thorac Cardiovasc Surg. 2000;12:25–29. doi: 10.1016/s1043-0679(00)70013-x. [DOI] [PubMed] [Google Scholar]
- 12.Schaff HV, Dearani JA, Daly RC, Orszulak TA, Danielson GK. Cox-Maze procedure for atrial fibrillation: Mayo Clinic experience. Semin Thorac Cardiovasc Surg. 2000;12:30–37. doi: 10.1016/s1043-0679(00)70014-1. [DOI] [PubMed] [Google Scholar]
- 13.Cox JL, Schuessler RB, Lappas DG, Boineau JP. An 8 1/2-year clinical experience with surgery for atrial fibrillation. Ann Surg. 1996;224:267–273. doi: 10.1097/00000658-199609000-00003. discussion 273–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaynor SL, Diodato MD, Prasad SM, Ishii Y, Schuessler RB, Bailey MS, Damiano NR, Bloch JB, Moon MR, Damiano RJ., Jr A prospective, single-center clinical trial of a modified Cox maze procedure with bipolar radiofrequency ablation. J Thorac Cardiovasc Surg. 2004;128:535–542. doi: 10.1016/j.jtcvs.2004.02.044. [DOI] [PubMed] [Google Scholar]
- 15.Cox JL, Canavan TE, Schuessler RB, Cain ME, Lindsay BD, Stone C, Smith PK, Corr PB, Boineau JP. The surgical treatment of atrial fibrillation. II. Intraoperative electrophysiologic mapping and description of the electrophysiologic basis of atrial flutter and atrial fibrillation. J Thorac Cardiovasc Surg. 1991;101:406–426. [PubMed] [Google Scholar]
- 16.Damiano RJ., Jr Alternative energy sources for atrial ablation: judging the new technology. Ann Thorac Surg. 2003;75:329–330. doi: 10.1016/s0003-4975(02)04844-0. [DOI] [PubMed] [Google Scholar]
- 17.Gillinov AM, Smedira NG, Cosgrove DM., 3rd Microwave ablation of atrial fibrillation during mitral valve operations. Ann Thorac Surg. 2002;74:1259–1261. doi: 10.1016/s0003-4975(02)03760-8. [DOI] [PubMed] [Google Scholar]
- 18.Knaut M, Spitzer SG, Karolyi L, Ebert HH, Richter P, Tugtekin SM, Schuler S. Intraoperative microwave ablation for curative treatment of atrial fibrillation in open heart surgery--the MICRO-STAF and MICRO-PASS pilot trial. MICROwave Application in Surgical treatment of Atrial Fibrillation. MICROwave Application for the Treatment of Atrial Fibrillation in Bypass-Surgery. Thorac Cardiovasc Surg. 1999;47 Suppl 3:379–384. doi: 10.1055/s-2007-1013205. [DOI] [PubMed] [Google Scholar]
- 19.Venturini A, Polesel E, Cutaia V, Asta A, Mangino D, Moretti R, Terrini A, Zussa C. Intraoperative microwave ablation in patients undergoing valvular surgery: midterm results. Heart Surg Forum. 2003;6:409–411. [PubMed] [Google Scholar]
- 20.Knaut M, Tugtekin SM, Spitzer S, Gulielmos V. Combined atrial fibrillation and mitral valve surgery using microwave technology. Semin Thorac Cardiovasc Surg. 2002;14:226–231. doi: 10.1053/stcs.2002.33754. [DOI] [PubMed] [Google Scholar]
- 21.Mokadam NA, McCarthy PM, Gillinov AM, Ryan WH, Moon MR, Mack MJ, Gaynor SL, Prasad SM, Wickline SA, Bailey MS, Damiano NR, Ishii Y, Schuessler RB, Damiano RJ., Jr A prospective multicenter trial of bipolar radiofrequency ablation for atrial fibrillation: early results. Ann Thorac Surg. 2005;78:1665–1670. doi: 10.1016/j.athoracsur.2004.05.066. [DOI] [PubMed] [Google Scholar]
- 22.Banerjee A, Singh S, Tempe DK. Intraoperative endocardial ablation of chronic atrial fibrillation along with mitral valve surgery using high frequency ultrasound with a ball-tipped harmonic scalpel probe. Indian Heart J. 2004;56:178–180. [PubMed] [Google Scholar]
- 23.Reddy VY, Houghtaling C, Fallon J, Fischer G, Farr N, Clarke J, McIntyre J, Sinofsky E, Ruskin JN, Keane D. Use of a diode laser balloon ablation catheter to generate circumferential pulmonary venous lesions in an open-thoracotomy caprine model. Pacing Clin Electrophysiol. 2004;27:52–57. doi: 10.1111/j.1540-8159.2004.00385.x. [DOI] [PubMed] [Google Scholar]
- 24.Prasad SM, Maniar HS, Diodato MD, Schuessler RB, Damiano RJ., Jr Physiological consequences of bipolar radiofrequency energy on the atria and pulmonary veins: a chronic animal study. Ann Thorac Surg. 2003;76:836–841. doi: 10.1016/s0003-4975(03)00716-1. [DOI] [PubMed] [Google Scholar]
- 25.Prasad SM, Maniar HS, Schuessler RB, Damiano RJ., Jr Chronic transmural atrial ablation by using bipolar radiofrequency energy on the beating heart. J Thorac Cardiovasc Surg. 2002;124:708–713. doi: 10.1067/mtc.2002.125057. [DOI] [PubMed] [Google Scholar]
- 26.Mokadam NA, McCarthy PM, Gillinov AM, Ryan WH, Moon MR, Mack MJ, Gaynor SL, Prasad SM, Wickline SA, Bailey MS, Damiano NR, Ishii Y, Schuessler RB, Damiano RJ., Jr A prospective multicenter trial of bipolar radiofrequency ablation for atrial fibrillation: early results. Ann Thorac Surg. 2004;78:1665–1670. doi: 10.1016/j.athoracsur.2004.05.066. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 28.Ware JE, Jr, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and interpretation guide. The Health Institue, New England Medical Center; 1993. [Google Scholar]
- 29.Lonnerholm S, Blomstrom P, Nilsson L, Oxelbark S, Jideus L, Blomstrom-Lundqvist C. Effects of the Maze Operation on Health-Related Quality of Life in Patients With Atrial Fibrillation. Circulation. 2000;101:2607. doi: 10.1161/01.cir.101.22.2607. [DOI] [PubMed] [Google Scholar]
- 30.Alboni P, Botto GL, Baldi N, Luzi M, Russo V, Gianfranchi L, Marchi P, Calzolari M, Solano A, Baroffio R, Gaggioli G. Outpatient Treatment of Recent-Onset Atrial Fibrillation with the "Pill-in-the-Pocket" Approach. The New England Journal of Medicine. 2004;351:2384. doi: 10.1056/NEJMoa041233. [DOI] [PubMed] [Google Scholar]
- 31.Dorian P, Paquette M, Newman D, Green M, Connolly SJ, Talajic M, Roy D. Quality of life improves with treatment in the Canadian Trial of Atrial Fibrillation. Am Heart J. 2002;143:984–990. doi: 10.1067/mhj.2002.122518. [DOI] [PubMed] [Google Scholar]
- 32.Hagens VE, Ranchor AV, Van Sonderen E, Bosker HA, Kamp O, Tijssen JG, Kingma JH, Crijns HJ, Van Gelder IC. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241–247. doi: 10.1016/j.jacc.2003.08.037. [DOI] [PubMed] [Google Scholar]
- 33.Singh BN, Singh SN, Reda DJ, Tang XC, Lopez B, Harris CL, Fletcher RD, Sharma SC, Atwood JE, Jacobson AK, Lewis HD, Jr, Raisch DW, Ezekowitz MD. Amiodarone versus sotalol for atrial fibrillation. N Engl J Med. 2005;352:1861–1872. doi: 10.1056/NEJMoa041705. [DOI] [PubMed] [Google Scholar]
- 34.Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Metayer P, Clementy J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–666. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 35.Wazni OM, Marrouche NF, Martin DO, Verma A, Bhargava M, Saliba W, Bash D, Schweikert R, Brachmann J, Gunther J, Gutleben K, Pisano E, Potenza D, Fanelli R, Raviele A, Themistoclakis S, Rossillo A, Bonso A, Natale A. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA. 2005;293:2634–2640. doi: 10.1001/jama.293.21.2634. [DOI] [PubMed] [Google Scholar]
- 36.Purerfellner H, Martinek M, Aichinger J, Nesser HJ, Kempen K, Janssen JP. Quality of life restored to normal in patients with atrial fibrillation after pulmonary vein ostial isolation. Am Heart J. 2004;148:318–325. doi: 10.1016/j.ahj.2004.03.036. [DOI] [PubMed] [Google Scholar]
- 37.Tse HF, Sin PY, Siu CW, Tsang V, Lam CL, Lau CP. Successful pulmonary vein isolation using transvenous catheter cryoablation improves quality-of-life in patients with atrial fibrillation. Pacing Clin Electrophysiol. 2005;28:421–424. doi: 10.1111/j.1540-8159.2005.50001.x. [DOI] [PubMed] [Google Scholar]