Abstract
Objective
To determine special outpatient services (SOS) use, need, associated factors, and neurodevelopmental and functional outcomes among extremely preterm infants at 18 to 22 months’ corrected age.
Design
Retrospective analysis.
Setting
National Institute of Child Health and Human Development (NICHD) Neonatal Research Network.
Participants
Infants younger than 28 weeks’ gestational age who had been born weighing less than 1000 g at an NICHD Neonatal Research Network center from January 1, 1997, to December 31, 2000, and who were receiving follow-up at 18 to 22 months’ corrected age.
Interventions
Questionnaires were administered at the 18- to 22-month follow-up visit regarding SOS use since hospital discharge and the current need for SOS (social work, visiting nurse, medical specialty, early intervention, speech and language services, occupational therapy and physical therapy, and neurodevelopmental and behavioral services).
Main Outcome Measures
The use of and need for SOS were analyzed by gestational age. Logistic regression analysis identified factors independently associated with the use of more than 5 services and with the need for any services.
Results
Of 2315 infants, 54.7% used more than 3 SOS by 18 to 22 months, and 19.1% used 6 to 7 SOS. The need for any SOS was reported by approximately 37%. The following variables that were commonly associated with adverse neurodevelopmental outcomes were also associated with the use of more than 5 SOS: sepsis, birth weight, postnatal corticosteroid use, bronchopulmonary dysplasia, and cystic periventricular leukomalacia or grade 3 or 4 intraventricular hemorrhage. Male sex was associated with the need for any SOS. Although high SOS use was more likely among children with adverse neurodevelopmental outcomes, a reported need for SOS was common even among those with mild developmental impairment (39.7%) and mild cerebral palsy (42.2%).
Conclusions
High SOS use is common, has identifiable neonatal risk factors, and is associated with neurodevelopmental impairment. Extremely preterm survivors have substantial need for community supports regardless of their impairment level. Efforts to improve comprehensive delivery of family-centered community-based services are urgently needed.
Resource use among extremely preterm infants is of great concern in the present era as the survival rate among very low-birth-weight (VLBW) infants approaches 90%.1 Several studies2-4 have investigated monetary cost, services use, and risk factors associated with increased resource utilization during the initial hospitalization of extremely preterm, extremely low-birth-weight (<1000 g) (ELBW) infants. Analyses of postdischarge special outpatient services (SOS) use among former preterm infants have primarily focused on the use of educational services and on other therapies associated with functional limitations at school age.5-7 Studies8-11 of ELBW infants in later childhood have demonstrated an association between the need for services and poor neurodevelopmental outcomes. Other analyses have concentrated on the economic consequences associated with rehospitalizations after discharge12 or with early intervention service insurance claims.13
It has been estimated that 12.8% of all children younger than 18 years in the United States experience a special health care need annually.14 The range and cumulative extent of SOS use have not been thoroughly explored among extremely preterm infants after hospital discharge to early childhood, nor have the perinatal and neonatal factors that may predict high SOS use been studied, to our knowledge. Lindeke et al15 demonstrated that neonatal intensive care unit stay duration was correlated with the use of special educational services at 7 to 11 years of age, but this study was small and was not limited to extremely preterm patients. Lower birth weight and poverty-level income were associated with more emergency department visits in a 3-year follow-up study16 of the Infant Health and Development Program, but this cohort included patients of older gestational age. Other authors have noted more rehospitalizations and increased outpatient hospital visits among preterm infants, but the investigations were not limited to extremely preterm infants.17 Most important, identification by primary caregivers of unmet needs for SOS in early childhood has not been explored, to our knowledge.
An understanding of the scope of postdischarge service use among extremely preterm infants in early childhood, as well as identification of associated perinatal and neonatal risk factors, could aid in resource and fiscal planning at the local, state, and national levels. Awareness could lead to targeted referrals, better multidisciplinary coordination, and anticipatory guidance to families at initial hospital discharge. Identification of variables associated with perceived need for services could assist in recognition of low-use and high-need scenarios. Therefore, among infants born at less than 28 weeks’ estimated gestational age (EGA) at National Institute of Child Health and Human Development (NICHD) Neonatal Research Network centers, we aimed to determine the following: (1) the range and extent of outpatient special child services used from initial hospital discharge to 18 to 22 months’ corrected age, (2) the perceived need for SOS not being delivered, and (3) the associations of perinatal, neonatal, and sociodemographic factors with high SOS use and with the need for SOS. We also examined the associations of neurodevelopmental and functional outcomes with high use of and the need for SOS.
METHODS
STUDY DESIGN AND PATIENT POPULATION
This was a retrospective analysis of the NICHD Neonatal Research Network registry and the ELBW follow-up study database. Infants were included if they had survived to discharge, their birth weight had been less than 1000 g at less than 28 weeks’ EGA, they had neurodevelopmental follow-up within the 18 to 22 months’ corrected age window, and they were born at an NICHD Neonatal Research Network site between January 1, 1997, and December 31, 2000. The birth cohort was chosen to assure that the SOS questionnaire was consistent throughout the study period and that Gross Motor Function Classification System level assignment18 and severity grading for cerebral palsy (CP) were performed at the 18- to 22-month follow-up visit. Because of the confounding effects of older age at evaluation with respect to SOS used and needed, patients were included only if they were seen in follow-up within the 18- to 22-month window.
The NICHD VLBW registry was developed to survey practice, assess morbidity and mortality, and provide information for the planning of clinical trials. Only data from centers that participated during the entire study period were included in the analysis. The centers’ institutional review boards reviewed and approved the data collection procedures. Research nurses collected perinatal, infant, and demographic data at each center using common definitions developed by investigators and described in previous publications.1,19 Maternal age was defined as the age of the biological mother at the time of delivery. The timing of rupture of membranes was noted. Antenatal antibiotic use was defined as the administration of any antibiotics to the mother during the admission that resulted in delivery. Antenatal corticosteroid use was defined as the administration of any corticosteroids to accelerate fetal lung maturity in the current pregnancy. The EGA was determined by best obstetric estimate using the last menstrual period, standard obstetric variables, and ultrasonography. Data were also collected pertaining to diagnoses, treatments, and in-hospital morbidities until death, discharge, or 120 days. If the infant remained in the hospital beyond 120 days, even if he or she was transferred to another facility, data were collected regarding death or date of discharge. Surfactant treatment was defined as at least 1 dose of any surfactant. Intraventricular hemorrhage was reported according to the classification by Papile et al.20 Cystic periventricular leukomalacia was defined as diagnosis by ultrasonography of the head performed after 2 weeks of age; if ultrasonography of the head was not obtained after 2 weeks of age, no report was made as to the presence or absence of cystic periventricular leukomalacia. Early sepsis was defined as culture-proven septicemia or bacteremia at 72 hours or earlier, and late sepsis was defined as culture-proven septicemia or bacteremia at later than 72 hours. Necrotizing enterocolitis was defined as modified Bell classification stage IIA or higher. The frequency of stage III or higher retinopathy of prematurity with plus disease in either eye was evaluated for this analysis. Bronchopulmonary dysplasia (BPD) was defined based on the reception of supplemental oxygen at 36 weeks’ postmenstrual age as determined by best obstetric estimate or based on the use of supplemental oxygen at hospital discharge, whichever occurred first. Postnatal corticosteroid use was defined as the administration of any corticosteroid for the prevention or treatment of BPD.
NEURODEVELOPMENTAL ASSESSMENT AND FOLLOW-UP VISIT
Neurodevelopmental and Neurologic Examination
Elements of the follow-up visit were based on the NICHD Neonatal Research Network follow-up study of ELBW infants, previously described in detail.21 All neurologic assessments were performed by certified examiners who had been trained in the assessment procedure at an annual 2-day workshop. The neurologic examination was based on techniques described by Amiel-Tison,22 Russell et al,23 and Palisano et al.18 Cerebral palsy was defined as a nonprogressive central nervous system disorder characterized by abnormal muscle tone in at least 1 extremity and by abnormal control of movement and posture that interfered with or prevented age-appropriate motor activities. Cerebral palsy was classified as moderate if the child could sit independently or with support but an assistive device was required for ambulation; CP was classified as severe if the child was unable to sit or walk with support. Certified examiners administered the Bayley Scales of Infant Development II24 Mental Developmental Index and Psychomotor Developmental Index. Scores were adjusted for prematurity. The standardized, normed mean score for both components of the Bayley Scales of Infant Development II is 100; the standard deviation is 15. Scores of 49 were assigned to infants whose extremely severe neurologic or neuro developmental impairment prevented examination. Gross motor function was classified according to the Gross Motor Function Classification System described by Palisano et al.18 Five broad levels of function are used in this system. Levels representing the greatest functional impairment are the following: level III (the subject can maintain floor sitting when the low back is supported and may roll and creep forward on his or her stomach), level IV (the subject has head control, but trunk support is required for floor sitting; he or she may roll to the supine or prone position), and level V (the subject is unable to maintain antigravity head and trunk postures in the prone and sitting positions; he or she requires assistance to roll).
Neurodevelopmental impairment (NDI) was defined as having 1 or more of the following: (1) moderate to severe CP, bilateral blindness (no useful vision in either eye) or deafness (requiring hearing aids in both ears), and Bayley Scales of Infant Development II MDI or PDI scores of less than 70. Unimpaired was defined as having none of the following: moderate to severe CP, blindness, deafness, MDI score of less than 85, and PDI score of less than 85.
Questionnaires
At the 18- to 22-month follow-up visit, research personnel administered standardized questionnaires regarding socioeconomic status, including the number of people living in the household, the highest level of education attained by the primary caregiver, the number of times the family had moved since the first hospital discharge, and other factors. The questionnaire also includes queries about receipt of any of 7 SOS at any time since the initial hospital discharge until the time of the follow-up evaluation, as well as whether the caregiver thought that the child needed but was not receiving any of these services. The caregiver was also asked whether the child was currently receiving any of these specific services. The SOS were as follows: (1) visiting nurse; (2) occupational therapy or physical therapy, described as therapy to help the child exercise muscles, play appropriately, use his or her hands, and perform whole-body movement; (3) speech or language therapy, described as therapy to improve the child’s ability to understand and use language or another communication method; (4) early intervention, described as a program to teach the child developmentally appropriate skills alone, in a center, in the home, or with other children; (5) social worker (which specifically excluded any social worker evaluation to determine the need for SOS); (6) any medical subspecialty or surgical subspecialty; and (7) neurodevelopmental or behavioral evaluations, described as services to evaluate the child’s abilities compared with those of other children (eg, walking, talking, and self-feeding). The findings of these questionnaires were not verified by review of patient medical records or other documents.
STATISTICAL ANALYSIS
Analyses were performed using χ2 test for categorical data and t test for continuous data. Independent associations of potential perinatal, neonatal, and sociodemographic risk factors for high use of (>5 SOS used) and reported need for (≥1 SOS needed) services were investigated using multivariate logistic regression analysis, and results were reported as odds ratios and 95% confidence intervals adjusted for potential confounders. Risk factors were entered into regression models, and final best-fit models were constructed by stepwise nonautomatic elimination. All final models forced inclusion of sex, EGA, birth weight, race/ethnicity, multiple gestation, and NICHD Neonatal Research Network center.
RESULTS
PATIENT DISPOSITION
From January 1, 1997, to December 31, 2000, 4793 infants of less than 28 weeks’ EGA were born at an NICHD Neonatal Research Network center; 3017 survived to discharge and 56 died after discharge (Figure). Follow-up at any time occurred for 2469, but 154 of these had follow-up outside of the 18- to 22-month window. The final study group included 2315 infants.
Figure.
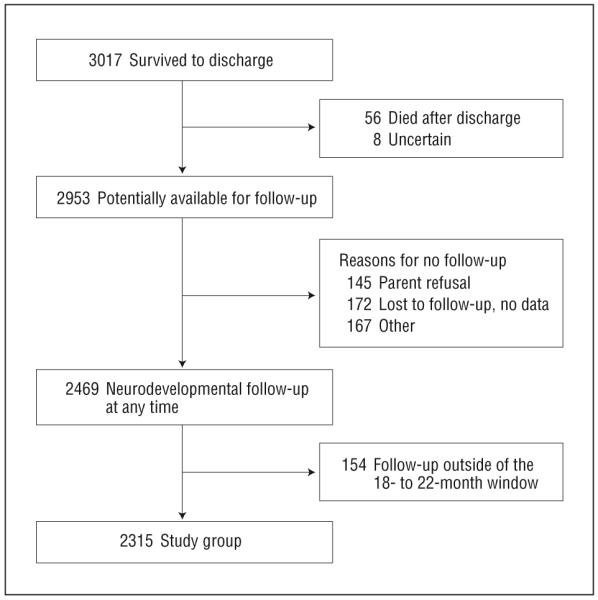
Study group disposition from hospital discharge to neurodevelopmental follow-up at 18 to 22 months of age corrected for prematurity.
SERVICE USE AND PERCEIVED NEED FOR SERVICES
The use of specific SOS and the cumulative number of services by gestational age are given in Table 1. Among the entire study group, 11.8% of primary caregivers reported using 0 to 1 SOS from the time of initial hospital discharge. Nineteen percent of the study group had used 6 to 7 SOS. Differences by EGA were noted at low-use (7.2% who were ≤24 weeks’ EGA compared with 16.7% who were 27 weeks’ EGA used 0-1 service) and high-use (25.8% who were ≤24 weeks’ EGA compared with 12.9% who were 27 weeks’ EGA used 6-7 services) extremes. Medical specialties, neurodevelopmental services, and occupational therapy and physical therapy were widely used; speech and language (33.7%) and social worker (25.6%) services were used least.
Table 1. Use of Services From Initial Hospital Discharge to 18 to 22 Months’ Corrected Age.
| Estimated Gestational Age, wk, % |
|||||
|---|---|---|---|---|---|
| Service Used | ≤24 (n=585) | 25 (n=634) | 26 (n=640) | 27 (n=456) | Total, No. (%) (N=2315) |
| Visiting nurse, % of patients | 63.9 | 57.6 | 57.8 | 53.1 | 1358 (58.7) |
| Occupational therapy or physical therapy, % of patients | 70.7 | 60.6 | 56.1 | 50.2 | 1386 (59.9) |
| Speech and language, % of patients | 41.2 | 35.8 | 30.3 | 25.6 | 779 (33.7) |
| Early intervention, % of patients | 60.5 | 56.8 | 55.2 | 48.7 | 1289 (55.7) |
| Social worker, % of patients | 30.6 | 24.4 | 23.3 | 23.9 | 592 (25.6) |
| Medical specialty, % of patients | 76.9 | 73.5 | 68.1 | 70.2 | 1666 (72.0) |
| Neurodevelopmental and behavioral, % of patients | 72.8 | 72.1 | 67.0 | 61.4 | 1592 (68.8) |
| No. of services, % of patients | |||||
| 0 | 3.1 | 3.9 | 4.1 | 5.9 | 96 (4.1) |
| 0-1 | 7.2 | 10.1 | 14.2 | 16.7 | 273 (11.8) |
| 2-3 | 27.9 | 35.5 | 33.9 | 37.7 | 777 (33.6) |
| 4-5 | 39.1 | 33.9 | 35.9 | 32.7 | 823 (35.6) |
| 6-7 | 25.8 | 20.5 | 15.9 | 12.9 | 442 (19.1) |
Primary caregivers reported current use of SOS at the time of the 18- to 22-month evaluation. Twenty-six percent (599 caregivers) reported still using 4 to 5 services, and 6.8% (157 caregivers) reported using 6 to 7 services.
The perceived need for SOS among the entire study group is summarized in Table 2. Approximately 37% reported the need for 1 or more SOS that were not being received. Of 7 services, speech and language therapy was most frequently reported as needed (24.0%).
Table 2. Reported Unmet Service Needs at 18 to 22 Months’ Corrected Age.
| Service Needed (Total No. Responding) | % Reporting Need |
|---|---|
| Visiting nurse (n=2303) | 4.1 |
| Occupational therapy or physical therapy (n=2305) | 7.9 |
| Speech and language (n=2301) | 24.0 |
| Early intervention (n=2304) | 13.7 |
| Social worker (n=2304) | 3.6 |
| Medical specialty (n=2302) | 3.8 |
| Neurodevelopmental and behavioral (n=2301) | 5.8 |
| No. of services (n=2315) | |
| 0 | 63.5 |
| 1 | 21.0 |
| 2 | 8.3 |
| 3 | 4.9 |
| 4-5 | 1.9 |
| 6-7 | 0.3 |
ASSOCIATIONS OF PERINATAL, NEONATAL, AND SOCIODEMOGRAPHIC FACTORS WITH SERVICE USE AND PERCEIVED NEED FOR SERVICES
The adjusted odds ratios and 95% confidence intervals for associations of potential risk factors with high (>5 services) SOS use by the 18- to 22-month follow-up visit are given in Table 3. Factors independently associated with increased odds for high SOS use included sepsis, BPD, multiple gestation, Medicaid as the primary insurance, cystic periventricular leukomalacia or grade 3 or 4 intraventricular hemorrhage, and postnatal corticosteroid exposure during the initial neonatal hospitalization. Factors associated with decreased odds for high SOS use included higher birth weight and aspects of the early childhood environment; each 100-g increase in birth weight was associated with a 13% odds reduction for high service use, and living with the mother at the time of follow-up was associated with an 80% odds reduction.
Table 3. Risk Factors for High Service Use (>5 Services) From Initial Hospital Discharge to 18 to 22 Months’ Corrected Age and Independent Associations With Perinatal, Neonatal, and Sociodemographic Variables.
| Risk Factor | Odds Ratio (95% Confidence Interval) |
|---|---|
| Gestational age, per wk | 0.96 (0.85-1.08) |
| Birth weight, per 100 g | 0.87 (0.78-0.98) |
| Male sex | 1.04 (0.81-1.33) |
| Multiple gestation | 1.55 (1.16-2.07) |
| Race/ethnicity | |
| White vs black | 1.27 (0.89-1.80) |
| Hispanic vs black | 1.34 (0.83-2.17) |
| Any surfactant therapy | 1.10 (0.74-1.64) |
| Age of mother, for each year older | 1.02 (0.99-1.05) |
| Cystic periventricular leukomalacia or grade 3-4 intraventricular hemorrhage | 1.83 (1.36-2.47) |
| Bronchopulmonary dysplasia | 2.22 (1.56-2.98) |
| Necrotizing enterocolitis | 1.40 (0.93-2.10) |
| Sepsis | 1.34 (1.04-1.72) |
| Postnatal corticosteroid use | 1.46 (1.09-1.96) |
| Mother single at delivery | 0.93 (0.68-1.27) |
| Grade ≥3 retinopathy of prematurity with plus disease | 1.27 (0.91-1.76) |
| Primary caregiver educational level less than high school | 1.28 (0.93-1.77) |
| ≥6 Persons in household | 1.13 (0.82-1.55) |
| ≥3 Places lived since discharge | 1.19 (0.84-1.70) |
| Living with mother at the time of follow-up | 0.19 (0.13-0.28) |
| Primary language not English | 0.89 (0.56-1.40) |
| Medicaid insurance or Medicaid health maintenance organization | 1.50 (1.08-2.10) |
The adjusted odds ratios and 95% confidence intervals for associations of potential risk factors with perceived need for 1 or more services at 18 to 22 months are given in Table 4. Only male sex and Medicaid insurance as the primary insurance were associated with increased odds for reported need for services.
Table 4. Independent Associations of Perinatal, Neonatal, and Sociodemographic Variables With Use of More than 5 Services From Initial Hospital Discharge to 18 to 22 Months’ Corrected Age.
| Rick Factor | Adjusted Odds Ratio (95% Confidence Interval) |
|---|---|
| Gestational age, per wk | 0.98 (0.89-1.08) |
| Birth weight, per 100 g | 1.02 (0.93-1.11) |
| Male sex | 1.38 (1.14-1.68) |
| Multiple gestation | 1.05 (0.83-1.33) |
| Race/ethnicity | |
| White vs black | 0.87 (0.66-1.14) |
| Hispanic vs black | 1.12 (0.76-1.65) |
| Any surfactant therapy | 0.73 (0.56-0.97) |
| Cystic periventricular leukomalacia or grade 3-4 intraventricular hemorrhage | 0.83 (0.65-1.07) |
| Postnatal corticosteroid use | 1.10 (0.88-1.37) |
| Mother single at delivery | 1.27 (0.99-1.63) |
| Primary caregiver educational level less than high school | 1.26 (0.98-1.61) |
| ≥6 Persons in household | 1.11 (0.86-1.44) |
| ≥3 Places lived since discharge | 1.23 (0.93-1.64) |
| Living with mother at the time of follow-up | 1.07 (0.75-1.53) |
| Primary language not English | 0.75 (0.52-1.09) |
| Medicaid insurance or Medicaid health maintenance organization | 1.94 (1.50-2.52) |
SOS USE, NEURODEVELOPMENTAL OUTCOMES, AND PERCEIVED CURRENT SOS NEED
Neurodevelopmental and functional impairment levels were analyzed in the group that had used more than 5 SOS and the group that had used 5 or fewer SOS (Table 5). Compared with the lower-service use group (≤5 services), the group that had used more than 5 services had more patients with moderate or severe CP, severe cognitive delay, and high functional impairment levels. Approximately two-thirds of the group that had used more than 5 services had neurodevelopmental impairment at the 18- to 22-month examination. Conversely, only 12.8% of the group that had used more than 5 services were unimpaired.
Table 5. Neurodevelopmental and Functional Outcomes Among Those Who Used More Than 5 Services Compared With Those Who Used Fewer Services by 18 to 22 Months’ Corrected Agea.
| Services Used, No./ Total No. (%) |
|||
|---|---|---|---|
| Variable | ≤5 | >5 | P Value |
| Cerebral palsy | |||
| Moderate or severe | 102/1855 (5.5) | 91/441 (20.6) | <.001 |
| Mild | 123/1855 (6.6) | 50/441 (11.3) | .001 |
| Mental Developmental Index | |||
| <70 | 491/1749 (28.1) | 226/412 (54.9) | <.001 |
| 71-85 | 503/1749 (28.8) | 92/412 (22.3) | .01 |
| Gross Motor Function Classification System level | |||
| ≥2 | 87/1865 (4.7) | 84/441 (19.0) | <.001 |
| ≥3 | 50/1865 (2.7) | 55/441 (12.5) | <.001 |
| Neurodevelopmental impairment | 577/1724 (33.5) | 273/421 (64.8) | <.001 |
| Unimpaired | 596/1691 (35.2) | 51/399 (12.8) | <.001 |
Data were unavailable for some subjects because of missing data forms or because Bayley Scales of Infant Development II or other examinations were not performed.
The rates of high SOS use and the need for any SOS were also evaluated within, and compared between, neurodevelopmental and functional outcome categories (Table 6). Children having severe CP, increased cognitive delay, and greater overall impairment were more likely to have used more than 5 SOS. However, many caregivers of children with mild CP, mild cognitive delay, and unimpaired status reported current SOS needs.
Table 6. High Service Use and Unmet Service Needs by 18 to 22 Months’ Corrected Age Among Neurodevelopmental and Functional Categoriesa.
| Cerebral Palsy |
Mental Developmental Index |
Gross Motor Function Classification System Level |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Moderate or Severe (n=193) |
Mild (n=173) |
P Value |
<70 (n=717) |
71-85 (n=595) |
P Value |
≥2 (n=171) |
≥3 (n=105) |
P Value |
Neurodevelopmental Impairment (n=850) |
Unimpaired (n=647) |
P Value |
| >5 Services used | 91 (47.2) | 50 (28.9) | <.001 | 226 (31.5) | 92 (15.5) | <.001 | 84 (49.1) | 55 (52.4) | .69 | 273 (32.1) | 51 (7.9) | <.001 |
| Unmet service needs | 78 (40.4) | 73 (42.2) | .82 | 343 (47.8) | 236 (39.7) | .003 | 68 (39.8) | 43 (41.0) | .94 | 388 (45.6) | 167 (25.8) | <.001 |
Data are presented as number (percentage) of subjects unless otherwise specified. Data were unavailable for some subjects because of missing data forms or because Bayley Scales of Infant Development II or other examinations were not performed.
COMMENT
Our findings underscore that significant resource use associated with extremely preterm birth is not limited to the inpatient setting and continues after initial hospitalization. Furthermore, the caregivers of more than one-third of these high-risk survivors reported unmet needs for SOS at 18 to 22 months’ corrected age. These results reinforce the necessity for proactive outpatient resource planning at the local and national levels and for more focused development of coordinated and integrated postdischarge medical care environments for these extremely high-risk, complex patients.
Previous studies have demonstrated high-resource use among extremely preterm infants after the initial neonatal hospitalization, but most authors have focused on rehospitalization12 rates or the need for later educational assistance.5-7 Preterm birth also is associated with significant long-term financial implications for hospitalization and intervention services.12,13
In our analysis, we chose to focus specifically on SOS because we believe that these encounters represent a unique and potentially underappreciated area of resource use. Few previous reports have investigated these types of SOS visits among extremely preterm infants. A recent follow-up study17 of a New Zealand preterm cohort demonstrated that virtually all preterm infants had atleast 1 outpatient hospital visit. The visits included emergency department use and a range of other specialist and medical referral services, and the cohort included infants of up to 32 weeks’ EGA and with a birth weight of less than 1500 g. In our analysis, we report SOS use by gestational age, and our study group includes only extremely preterm infants. We also chose to focus our analysis on cumulative SOS use rather than limiting it to a “snapshot” report of current service use at the time of follow-up. This approach more fully reflects the degree to which local and national systems may be affected by the service needs of extremely preterm survivors.
NICHD Neonatal Research Network Group Members (1997-2000)
Brown University Women & Infants Hospital, Providence, Rhode Island: Principal Investigator: William Oh, MD, Study Coordinator: Angelita Hensman, BSN, RNC, Follow-up Principal Investigator: Betty Vohr, MD, and Follow-up Coordinator: Lucy Noel, RN. Case Western Reserve University Rainbow Children’s Hospital, Cleveland, Ohio: Principal Investigator: Avroy A. Fanaroff, MD, Coprincipal Investigator: Michele C. Walsh, MD, Study Coordinator: Nancy Newman, BA, RN, Follow-up Principal Investigator: DeeAnne Wilson-Costello, MD, and Follow-up Coordinator: Bonnie Siner, RN. Emory University Grady Memorial Hospital and Crawford Long Hospital, Atlanta, Georgia: Principal Investigator: Barbara J. Stoll, MD, Coprincipal Investigator: Lucky Jain, MD, and Study Coordinator: Ellen Hale, RN, BS. Harvard University, Cambridge, Massachusetts: Principal Investigator: Anne R. Stark, MD, and Study Coordinator: Kerri Fournier, RN. Indiana University Riley Hospital for Children and Methodist Hospital, Indianapolis: Principal Investigator: James A. Lemons, MD, Study Coordinators: Diana Dawn Appel, RN BSN, and Lucy Miller, RN, BSN, Follow-up Principal Investigator: Anna Dusick, MD, and Follow-up Coordinator: Leslie Richard, RN. Stanford University, Stanford, California: Principal Investigator: David K. Stevenson, MD, Coprincipal Investigator: Krisa VanMeurs, MD, Study Coordinator: M. Bethany Ball, BS, CCRC, and Follow-up Principal Investigator: Susan R. Hintz, MD. University of Alabama at Birmingham University Hospital-UAB: Principal Investigator: Waldemar A. Carlo, MD, Study Coordinators: Monica Collins, RN, BSN, and Shirley Cosby, RN, BSN, Follow-up Principal Investigator: Myriam Peralta-Carcelen, MD, and Follow-up Coordinator: Vivien Phillips, RN, BSN. University of Cincinnati, The University Hospital and Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio: Principal Investigator: Edward F. Donovan, MD, Study Coordinators: Cathy Grisby, BSN, Barb Alexander, RN, Jody Shively, RN, and Holly Mincey, RN, Follow-up Principal Investigator: Jean Steichen, MD, and Follow-up Coordinator: Teresa Gratton, PA. University of Miami, Miami, Florida: Principal Investigator: Shahnaz Duara, MD, Study Coordinator: Ruth Everett, BSN, and Follow-up Principal Investigator: Charles R. Bauer, MD. University of New Mexico Hospital, Albuquerque, New Mexico: Principal Investigator: LuAnn Papile, MD, Study Coordinator: Conra Backstrom Lacy, RN, and Follow-up Coordinator: Jean Lowe, PhD. University of Tennessee Hospital, Knoxville: Principal Investigator: Sheldon Korones, MD, and Follow-up Coordinators: Kim Yolton, PhD, and Marilyn Williams, LCSW. University of Texas-Houston Memorial Hermann Children’s Hospital: Principal Investigator: Jon E. Tyson, MD, MPH, Study Coordinators: Georgia McDavid, RN, Esther G. Akpa, RN, BSN, Claudia Y. Franco, RN, BNS, MSN, NNP, Patty A. Cluff, RN, and Anna E. Lis, RN, BSN, and Follow-up Principal Investigators: Brenda H. Morris, MD, and Pamela J. Bradt, MD, MPH. University of Texas Southwestern Medical Center at Dallas Parkland Hospital: Principal Investigator: Abbot R. Laptook, MD, Study Coordinators: Susie Madison, RN, Gay Hensley, RN, and Nancy Miller, RN, Follow-up Principal Investigators: Roy Heyne, MD, and Sue Broyles, MD, and Follow-up Coordinator: Jackie Hickman, RN. Wayne State University Hutzel Women’s Hospital & Children’s Hospital of Michigan, Detroit: Principal Investigator: Seetha Shankaran, MD, Study Coordinators: Rebecca Bara, RN, BSN, and Geraldine Muran, RN, BSN, Follow-up Principal Investigator: Yvette Johnson, MD, and Follow-up Coordinator: Debbie Kennedy, RN. Yale University-New Haven Children’s Hospital, New Haven, Connecticut: Principal Investigator: Richard A. Ehrenkranz, MD, Study Coordinator: Patricia Gettner, RN, and Follow-up Coordinator: Elaine Romano, RN.
NICHD Neonatal Research Steering Committee
Brown University: William Oh, MD. Case Western Reserve University: Michele Walsh, MD. Emory University: Barbara J. Stoll, MD. Harvard University: Anne R. Stark, MD. Indiana University: James Lemons, MD. Stanford University: David Stevenson, MD. University of Alabama at Birmingham: Waldemar A. Carlo, MD. University of Cincinnati: Kurt Schibler, MD, and Alan Jobe, MD, PhD (chair). University of New Mexico: LuAnn Papile, MD. University of Tennessee: Sheldon Korones, MD. University of Texas-Dallas: Abbot Laptook, MD. University of Texas-Houston: Jon E. Tyson, MD, MPH. Wayne State University: Seetha Shankaran, MD. Yale University: Richard A. Ehrenkranz, MD.
Data Coordinating Center at RTI International
Principal Investigator: Abhik Das, PhD, Coprincipal Investigator: W. Kenneth Poole, PhD, and Coordinators: Betty Hastings, MS, Kris Zaterka-Baxter, and Carolyn P. Huitema, MS.
Eunice Kennedy Shriver National Institute of Child Health and Human Development
Linda Wright, MD, Rosemary D. Higgins, MD, and Elizabeth McClure, MS.
We found that some factors commonly associated with adverse neurodevelopmental outcomes among preterm infants were also independent risk factors for high-service use. Continued efforts to address potentially modifiable factors during the neonatal period, including sepsis and postnatal corticosteroid use, are critical. Of note, BPD was most strongly associated with high-service use, with a greater than 2-fold increase in the odds of using more than 5 SOS. This is of particular concern in light of previous evidence suggesting that the rates of BPD have increased among extremely preterm and ELBW infants25,26 as mortality has decreased. The association between Medicaid as the primary insurance at the 18- to 22-month visit and high-service use may point to a link with higher social risk or may simply reflect qualification for support because of impairment already identified. We also found that a child’s living with his or her mother at the time of the follow-up visit was associated with high-service use; however, the follow-up visit questionnaire did not explore the total duration of living with mother since the initial hospital discharge.
Unlike other studies, we also examined the perceived need for services at 18 to 22 months. Although the need for 1 or more SOS was frequently reported, few factors were independently associated with the perception of unmet needs. Given that ELBW boys are at increased risk for adverse neurodevelopmental outcomes,21,27 our finding with respect to sex may demonstrate an important gap in needed services. Similarly, the finding that Medicaid as primary insurance was independently associated with high use and with a perceived need for services may delineate a much higher-risk group whose needs are not being met. Newacheck et al28 reported that publicly insured children were less likely to have a regular clinician and had greater dissatisfaction with care at their usual site; in such circumstances, children may be less likely to receive SOS referrals. We also found that even children categorized as mildly impaired apparently have substantial unmet SOS needs at 18 to 22 months. Our findings emphasize the importance of focused research into the needs, outcomes, and challenges among the families in this understudied group.
There are limitations to this study, many of which are inherent to the retrospective nature of the analysis. Although descriptions of SOS were available for questionnaire administration, each family may interpret services differently. Separate visits for SOS may not occur at some centers in which integrated comprehensive follow-up exists. Similarly, our questionnaire at the 18- to 22-month visit asked the primary caregiver to report any SOS encounters since the time of the initial hospital discharge; recall bias may have confounded this analysis. The questionnaire did not differentiate whether services were 1-time events or multiple-visit events, so our findings may overestimate the extent of SOS use. However, we sought to address this challenge by classifying high-service use as more than 5 services. In addition, perceived need for SOS was based on caregiver report only. Finally, our standardized questionnaire did not probe further as to the reasons for unmet needs or perceived barriers to service access. Given our findings in this study, additional investigation into the causes of shortfalls in SOS provision among this patient population is a critical next step to improving family-centered community-based services.
We did not undertake a fiscal analysis of the extraordinary SOS use in the first 18 to 22 months, but it is clear that our findings add to the long-term economic consequences of prematurity that have already been identified in the literature.29 There are unmeasured family costs associated with the need for frequent SOS visits, including care arrangement for other children, the need for caregivers to take time off from work, and transportation-associated costs to reach specialty regional providers.14 Such burdens may contribute to long-term negative outcomes for families with VLBW and premature infants.30
Given our findings, we speculate that improved survival of extremely preterm infants is likely to have an effect on community and regional SOS use. The reauthorized Individuals With Disabilities Education Act of 2004,31 including Part C amendments, was intended to require that states enhance opportunities for early intervention to at-risk infant and toddler populations and to those with developmental delays, as well as to ensure appropriate transitional services for later childhood. However, the increasing numbers of children with ever more complex multidisciplinary care needs will continue to result in substantial coordination responsibilities for the primary care physician and for the caregiver. Recent policy statements have recommended a “medical home” to promote optimal coordinated care for children with special needs,32,33 but the barriers to provision of such an environment are numerous. Analyses such as ours can help to inform regarding the immense requirements for and potential predictors of these services. However, the time, effort, organization, and dedication to communication and collaboration needed to provide comprehensive care for these patients are substantial and are growing. Proper implementation of the medical home concept will require true societal commitment to enhanced educational emphasis on service facilitation skills, the needs of patients and families, and appropriate reimbursement for the expanding role of care coordinators.
Acknowledgments
Funding/Support: The study was supported by grants U10 HD34216, U10 HD27853, U10 HD27871, U10 HD40461, U10 HD40689, U10 HD27856, U10 HD27904, U10 HD40498, U10 HD40521, U01 HD36790, U10 HD21385, U10 HD27880, U10 HD27851, U10 HD 21373, U10 HD21415, and U10 HD27881 from the NICHD and by General Clinical Research Center grants M01 RR08084, M01 RR00125, M01 RR00750, M01 RR00070, M01RR0039-43, M01 RR00039, M01 RR00044, and M01 RR00997 from the National Center for Research Resources.
Footnotes
Financial Disclosure: None reported.
REFERENCES
- 1.Fanaroff AA, Stoll BJ, Wright LL, et al. NICHD Neonatal Research Network Trends in morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196(2):147.e1–147.e8. doi: 10.1016/j.ajog.2006.09.014. doi:10.1016/j.ajog.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Kilpatrick SJ, Schlueter MA, Piecuch R, Leonard CH, Rogido M, Sola A. Outcome of infants born at 24-26 weeks’ gestation, I: survival and cost. Obstet Gynecol. 1997;90(5):803–808. doi: 10.1016/S0029-7844(97)00483-3. [DOI] [PubMed] [Google Scholar]
- 3.Chan K, Ohlsson A, Synnes A, Lee DS, Chien LY, Lee SK, Canadian Neonatal Network Survival, morbidity, and resource use of infants of 25 weeks’ gestational age or less. Am J Obstet Gynecol. 2001;185(1):220–226. doi: 10.1067/mob.2001.115280. [DOI] [PubMed] [Google Scholar]
- 4.Tyson JE, Younes N, Verter J, Wright LL, National Institute of Child Health and Human Development Neonatal Research Network Viability, morbidity, and resource use among newborns of 501-800-g birth weight. JAMA. 1996;276(20):1645–1651. [PubMed] [Google Scholar]
- 5.Saigal S, Hoult LA, Streiner DL, Stoskopf BL, Rosenbaum PL. School difficulties at adolescence in a regional cohort of children who were extremely low birth weight. Pediatrics. 2000;105(2):325–331. doi: 10.1542/peds.105.2.325. [DOI] [PubMed] [Google Scholar]
- 6.D’Angio CT, Sinkin RA, Stevens TP, et al. Longitudinal, 15-year follow-up of children born at less than 29 weeks’ gestation after introduction of surfactant therapy into a region: neurologic, cognitive, and educational outcomes. Pediatrics. 2002;110(6):1094–1102. doi: 10.1542/peds.110.6.1094. [DOI] [PubMed] [Google Scholar]
- 7.Hack M, Taylor HG, Drotar D, et al. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA. 2005;294(3):318–325. doi: 10.1001/jama.294.3.318. [DOI] [PubMed] [Google Scholar]
- 8.Buck GM, Msall ME, Schisterman EF, Lyon NR, Rogers BT. Extreme prematurity and school outcomes. Paediatr Perinat Epidemiol. 2000;14(4):324–331. doi: 10.1046/j.1365-3016.2000.00276.x. [DOI] [PubMed] [Google Scholar]
- 9.Halsey CL, Collin MF, Anderson CL. Extremely low-birth-weight children and their peers: a comparison of school-age outcomes. Arch Pediatr Adolesc Med. 1996;150(8):790–794. doi: 10.1001/archpedi.1996.02170330016003. [DOI] [PubMed] [Google Scholar]
- 10.Bowen JR, Gibson FL, Hand PJ. Educational outcome at 8 years for children who were born extremely prematurely: a controlled study. J Paediatr Child Health. 2002;38(5):438–444. doi: 10.1046/j.1440-1754.2002.00039.x. [DOI] [PubMed] [Google Scholar]
- 11.Hille ET, den Ouden AL, Bauer L, van den Oudenrijn C, Brand R, Verloove-Vanhorick SP. School performance at nine years of age in very premature and very low birth weight infants: perinatal risk factors and predictors at five years of age. J Pediatr. 1994;125(3):426–434. doi: 10.1016/s0022-3476(05)83290-1. [DOI] [PubMed] [Google Scholar]
- 12.Petrou S. The economic consequences of preterm birth during the first 10 years of life. BJOG. 2005;112(suppl 1):10–15. doi: 10.1111/j.1471-0528.2005.00577.x. [DOI] [PubMed] [Google Scholar]
- 13.Clements KM, Barfield WD, Ayadi MF, Wilber N. Preterm birth-associated cost of early intervention service: an analysis by gestational age. Pediatrics. 2007;119(4):e866–e874. doi: 10.1542/peds.2006-1729. [DOI] [PubMed] [Google Scholar]
- 14.van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004;158(9):884–890. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- 15.Lindeke LL, Stanley JR, Else BS, Mills MM. Neonatal predictors of school-based services used by NICU graduates at school age. MCN Am J Matern Child Nurs. 2002;27(1):41–46. doi: 10.1097/00005721-200201000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Brooks-Gunn J, McCormick MC, Klebanov PK, McCarton C. Health care use of 3-year-old low birth weight premature children: effects of family and neighborhood poverty. J Pediatr. 1998;132(6):971–975. doi: 10.1016/s0022-3476(98)70393-2. [DOI] [PubMed] [Google Scholar]
- 17.Gray D, Woodward LJ, Spencer C, Inder TE, Austin NC. Health service utilisation of a regional cohort of very preterm infants over the first 2 years of life. J Paediatr Child Health. 2006;42(6):377–383. doi: 10.1111/j.1440-1754.2006.00876.x. [DOI] [PubMed] [Google Scholar]
- 18.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 19.Lemons JA, Bauer CR, Oh W, et al. NICHD Neonatal Research Network Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. [Accessed April 30, 2008];Pediatrics. 2001 107(1):e1. doi: 10.1542/peds.107.1.e1. http://pediatrics.aappublications.org/cgi/content/full/107/1/e1. [DOI] [PubMed] [Google Scholar]
- 20.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a case study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529–534. doi: 10.1016/s0022-3476(78)80282-0. [DOI] [PubMed] [Google Scholar]
- 21.Vohr BR, Wright LL, Poole WK, McDonald SA. Neurodevelopmental outcomes of extremely low birth weight infants <32 weeks’ gestation between 1993 and 1998. Pediatrics. 2005;116(3):635–643. doi: 10.1542/peds.2004-2247. [DOI] [PubMed] [Google Scholar]
- 22.Amiel-Tison C. Neuromotor status. In: Taeusch HW, Yogman MW, editors. Follow-up Management of the High-Risk Infant. Little Brown & Co; Boston, MA: 1987. pp. 115–126. [Google Scholar]
- 23.Russell DJ, Rosenbaum PL, Cadman DT, Gowland C, Hardy S, Jarvis S. The gross motor function measure: a means to evaluate the effects of physical therapy. Dev Med Child Neurol. 1989;31(3):341–352. doi: 10.1111/j.1469-8749.1989.tb04003.x. [DOI] [PubMed] [Google Scholar]
- 24.Bayley N. Bayley Scales of Infant Development-II. Psychological Corp; San Antonio, TX: 1993. [Google Scholar]
- 25.Hintz SR, Poole WK, Wright LL, et al. NICHD Neonatal Research Network Changes in mortality and morbidities among infants born at less than 25 weeks during the post-surfactant era. Arch Dis Child Fetal Neonatal Ed. 2005;90(2):F128–F133. doi: 10.1136/adc.2003.046268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hack M, Fanaroff AA. Outcomes of children of extremely low birthweight and gestational age in the 1990s. Semin Neonatol. 2000;5(2):89–106. doi: 10.1053/siny.1999.0001. [DOI] [PubMed] [Google Scholar]
- 27.Hintz SR, Kendrick DE, Vohr BR, Poole WK, Higgins R, NICHD Neonatal Research Network Gender differences in neurodevelopmental outcomes among extremely preterm, extremely-low-birthweight infants. Acta Paediatr. 2006;95(10):1239–1248. doi: 10.1080/08035250600599727. [DOI] [PubMed] [Google Scholar]
- 28.Newacheck PW, McManus M, Fox HB, Hung YY, Halfon N. Access to health care for children with special health care needs. Pediatrics. 2000;105(4 pt 1):760–766. doi: 10.1542/peds.105.4.760. [DOI] [PubMed] [Google Scholar]
- 29.Petrou S, Sach T, Davidson L. The long-term costs of preterm birth and low birth weight: results of a systematic review. Child Care Health Dev. 2001;27(2):97–115. doi: 10.1046/j.1365-2214.2001.00203.x. [DOI] [PubMed] [Google Scholar]
- 30.Taylor HG, Klein N, Minich NM, Hack M. Long-term family outcomes for children with very low birth weights. Arch Pediatr Adolesc Med. 2001;155(2):155–161. doi: 10.1001/archpedi.155.2.155. [DOI] [PubMed] [Google Scholar]
- 31.IDEA-Reauthorized Statute. [Accessed April 30, 2008];Part C amendments in IDEA 2004. http://www.ed.gov/policy/speced/guid/idea/tb-partc-ammend.pdf.
- 32.Medical Home Initiatives for Children With Special Needs Project Advisory Committee. American Academy of Pediatrics The medical home. Pediatrics. 2002;110(1 pt 1):184–186. [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics Council on Children With Disabilities Care coordination in the medical home: integrating health and related systems of care for children with special health care needs. Pediatrics. 2005;116(5):1238–1244. doi: 10.1542/peds.2005-2070. [DOI] [PubMed] [Google Scholar]


