Physiological comparisons of cardiovascular (CV) structure/function among individuals or groups of individuals are often difficult, due to differences in body dimensions. In order to have meaningful clinical and scientific comparisons, differences in body size must be accounted for. Although there is a plethora of data demonstrating that body size is an important determinant of CV structure/function, and although most researchers recognize the need to adjust CV parameters for differences in body size, there remains considerable confusion as to the most appropriate method to account for these differences. Chirinos et al in this issue of the Journal1, highlight two important issues facing CV research: which body dimension descriptor, height, weight, body mass index (BMI), or body surface area (BSA) is optimal for scaling various CV measures; and which mathematical scaling method should be used?
Chirinos et al1 examined the relationship between measures of resting CV parameters, with height, body weight, and BSA and concluded, as have numerous previous studies, that BSA was the most appropriate descriptor, because it incorporates changes in both height and weight, which were evident between their lean vs. obese groups. It is important that the selection of the body size descriptor be based both on the accuracy of its measurement, and its physiological relevance to the CV parameter. In most circumstances BSA is not measured, but rather is estimated through formulae. BSA incorporates both low (adipose tissue) and high (skeletal and cardiac muscle) metabolically active tissues. A greater muscle mass necessitates a larger energetic requirement, and thus theoretically, the scaling of CV parameters to fat free mass (FFM) may be the most appropriate body size descriptor.
But what role does adipose tissue (AT) have on the changes in CV function, and should this be included when scaling these data? During exercise the extra weight from AT places extra burden on the CV system to respond to exercise, and blood flow to the AT increases to facilitate fatty acid metabolism. O'Connor et al.,2 have previously shown that the reserve capacity during exercise of CV parameters varied significantly with the percentage of body fat. Thus in this setting would body weight, BSA or fat mass be a more appropriate body dimension descriptor than FFM?
Perhaps more important than selecting the body dimension descriptor is the scaling technique used to adjust for differences in body size? There is a misconception that simply dividing the CV parameter to a measure of body size (i.e., ratiometric scaling) removes the effects of body size on the CV parameter. Instead, a preferred approach might be the allometric scaling method, whereby the CV function is divided by the variable of interest raised to a scalar exponent, which is derived from an equation that linearly relates the two3. The allometric method accounts for the non-linearity of the relationship between a CV parameter and body size providing a dimensionless variable. Indeed Chirinos et al1 reported that when the arterial variables were scaled allometrically to height, weight or BSA, the effects of body size on CV parameters were completely removed. However, they also reported that many of the CV parameters could be scaled ratiometrically to BSA1, producing dimensionless variables, an approach that would be more suitable for clinical research.
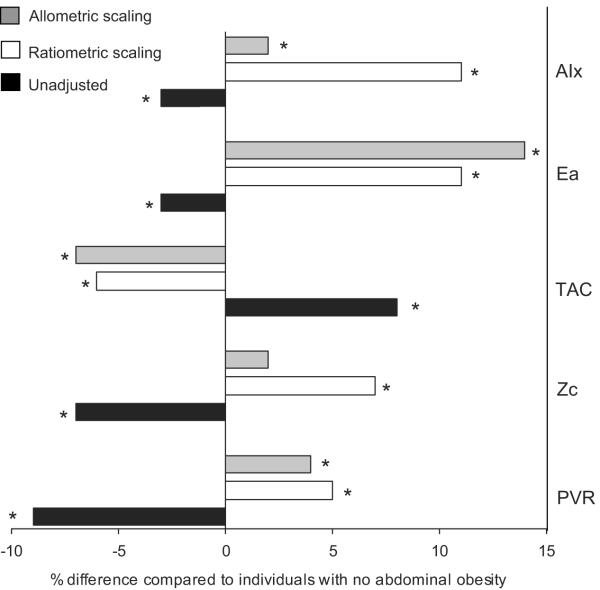
The work of Chirinos et al1 illustrates the importance of scaling for body size in order to separate the normal physiological relationship between body size and CV function from the pathologic effects of excess AT on CV function. Of note, in Chirinos et al1, with the exception of characteristic impedance (Zc), the differences in arterial function between individuals without and with abdominal obesity are evident when normalized to BSA irrespective of the scaling approach used. For example, individuals with abdominal obesity had a higher arterial elastance, resistance, augmentation index and a lower compliance compared to lean individuals when scaled ratiometrically or allometrically to BSA (Figure 1). Thus despite the allometric modeling process being theoretically and statistically superior to the ratiometric method, both methods had similar findings. Zc, however, did not differ when scaled allometrically to BSA, but was higher when scaled ratiometrically to BSA in individuals with abdominal obesity vs. no abdominal obesity (Figure 1). Could this lack of difference in Zc with ratiometric vs. allometric scaling to define the effect of obesity be attributed to the transfer of the power function exponent, which was derived from a subset of their lean cohort to the entire population? The relationship between the body descriptor and CV parameter is likely to differ in the lean vs. obese individuals, therefore, is it correct to extrapolate the b-exponent calculated from the lean to the mixed individuals? This is the conundrum that perplexes this field.
Figure 1.
The percentage difference in peripheral vascular resistance (PVR), characteristic impedance (Zc), total arterial compliance (TAC), arterial elastance (Ea) and augmentation index (AIx) in individuals with abdominal obesity compared to those without. Data obtained from Table 6 in Chirinos et al1. *P<0.05 compared to individuals without abdominal obesity. It is noticeable that the differences in arterial parameters between abdominal vs. no abdominal obesity are in the opposite direction when unadjusted vs. when scaled. Furthermore, apart from Zc, both ratiometric and allometric scaling successfully discriminated between lean and obese individuals.
But can we see the meat through the fat? While once thought of as an inert tissue, AT is now considered a complex endocrine organ that releases a variety of factors that regulate energy metabolism, cardiovascular function, reproductive status, and immune function4. Abnormal production or regulation of adipokines occurs in obese individuals and is implicated in the development of a variety of associated co-morbidities including metabolic syndrome, type 2-diabetes, atherosclerosis, and heart disease. AT expression of TNF-α and IL-6 interferes with insulin signaling5 and glucose production6. Interestingly IL-6 and TNF-α were significantly correlated with BMI, however, IL-6 levels were mostly associated with visceral adiposity, and TNF-α levels appeared to be more related to subcutaneous fat7; therefore perhaps visceral adiposity, rather than BMI, would be a better measure of obesity.
In addition, perivascular and pericardial AT have also been implicated in CV dysfunction. The secretion of adiponectin (an anti-inflammatory adipokine that modulates local vascular tone) from perivascular AT is lost with obesity leading to hypoxia, inflammation, and oxidative stress damaging the endothelial function of small-arteries8. Pericardial AT is associated with coronary artery calcification and left ventricular remodeling9. An increase in triglyceride content within the heart, which is evident in both obese and diabetic individuals10, has also been associated with ventricular diastolic dysfunction11. These data highlight the important of examining region specific effects of AT on CV structure/function and these associations are likely to go beyond this issue of appropriate scaling. Thus, future research must go beyond examining the role of total adiposity and examine the regional location of AT on CV structure/function.
In summary, Chirinos et al1 raise an important issue regarding the effects of body size on arterial function and other CV parameters, and have observed that obese individuals had a stiffer arterial system compared to lean individuals after adjusting for differences in BSA. The effects of obesity on arterial function were evident, however, with the exception of Zc, when scaled either ratiometrically or allometrically to BSA. Future research needs to move beyond examining the effects of whole (or central) adiposity and examine the regional specific effects of adipose tissue, and its interactions with the inflammatory and cytokine processes on CV structure/function.
Acknowledgments
Source of Funding This work was supported by the Intramural Research Program of the National Institutes of Health, National Institute on Aging.
Footnotes
Disclosure The authors have no disclosures to report
References
- 1.Chirinos J, Rietzschel E, De Buyzere M, De Bacquer D, Gillebert T, Gupta A, Segers P. Arterial load and ventricular-arterial coupling: physiologic relations with body size and effect of obesity. Hypertension. 2009;??:???–???. doi: 10.1161/HYPERTENSIONAHA.109.131870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Connor F, Fleg JL, Gerstenblith G, Becker LC, Goldberg AP, Hagberg JM, Lakatta L, Lakatta EG, Schulman SP. Effect of body fat on exercise hemodynamics in sedentary older men. Aging. 1994;6:257–265. doi: 10.1007/BF03324251. [DOI] [PubMed] [Google Scholar]
- 3.Batterham AM, George KP, Whyte G, Sharma S, McKenna W. Scaling cardiac structural data by body dimensions: a review of theory, practice, and problems. Int J Sports Med. 1999;20:495–502. doi: 10.1055/s-1999-8844. [DOI] [PubMed] [Google Scholar]
- 4.Rasouli N, Kern PA. Adipocytokines and the Metabolic Complications of Obesity. J Clin Endocrinol Metab. 2008;93:s64–73. doi: 10.1210/jc.2008-1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Senn JJ, Klover PJ, Nowak IA, Mooney RA. Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes. 2002;51:3391–3399. doi: 10.2337/diabetes.51.12.3391. [DOI] [PubMed] [Google Scholar]
- 6.Stouthard JM, Romijn JA, Van der Poll T, Endert E, Klein S, Bakker PJ, Veenhof CH, Sauerwein HP. Endocrinologic and metabolic effects of interleukin-6 in humans. Am J Physiol. 1995;268:E813–819. doi: 10.1152/ajpendo.1995.268.5.E813. [DOI] [PubMed] [Google Scholar]
- 7.Cartier A, Lemieux I, Almeras N, Tremblay A, Bergeron J, Despres JP. Visceral obesity and plasma glucose-insulin homeostasis: contributions of interleukin-6 and tumor necrosis factor-alpha in men. J Clin Endocrinol Metab. 2008;93:1931–1938. doi: 10.1210/jc.2007-2191. [DOI] [PubMed] [Google Scholar]
- 8.Greenstein AS, Khavandi K, Withers SB, Sonoyama K, Clancy O, Jeziorska M, Laing I, Yates AP, Pemberton PW, Malik RA, Heagerty AM. Local inflammation and hypoxia abolish the protective anticontractile properties of perivascular fat in obese patients. Circulation. 2009;119:1661–1670. doi: 10.1161/CIRCULATIONAHA.108.821181. [DOI] [PubMed] [Google Scholar]
- 9.Fox CS, Gona P, Hoffmann U, Porter SA, Salton CJ, Massaro JM, Levy D, Larson MG, D'Agostino RB, Sr., O'Donnell CJ, Manning WJ. Pericardial fat, intrathoracic fat, and measures of left ventricular structure and function: the Framingham Heart Study. Circulation. 2009;119:1586–1591. doi: 10.1161/CIRCULATIONAHA.108.828970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rijzewijk LJ, van der Meer RW, Smit JW, Diamant M, Bax JJ, Hammer S, Romijn JA, de Roos A, Lamb HJ. Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. J Am Coll Cardiol. 2008;52:1793–1799. doi: 10.1016/j.jacc.2008.07.062. [DOI] [PubMed] [Google Scholar]
- 11.van der Meer RW, Rijzewijk LJ, Diamant M, Hammer S, Schar M, Bax JJ, Smit JW, Romijn JA, de Roos A, Lamb HJ. The ageing male heart: myocardial triglyceride content as independent predictor of diastolic function. Eur Heart J. 2008;29:1516–1522. doi: 10.1093/eurheartj/ehn207. [DOI] [PubMed] [Google Scholar]